Summary
This paper deals with specific aspects of paediatric burns in the acute phase and considers how the treatment of burned children differs from that of burned adults. The epidemiology of paediatric burns is reviewed. Particular aspects of the treatment of burned children are presented, with regard to treatment at the site of the accident, first aid, resuscitation, and local treatment. The importance of the accurate assessment of paediatric burns is stressed.
Keywords: PAEDIATRIC, BURNS, ACUTE, PHASE, SPECIFIC, ASPECTS
Abstract
Les Auteurs discutent les aspects spécifiques des brûlures en âge pédiatrique dans la phase aiguë et considèrent comme le traitement des enfants brûlés est différent de celui des adultes brûlés. Après avoir décrit l'épidémiologie des brûlures chez les enfants, ils présentent les aspects particuliers du traitement des enfants brûlés, en particulier pour ce qui concerne le traitement au site de l'accident, les premiers soins, la réanimation et le traitement local. L'importance de l'évaluation précise des brûlures des enfants est soulignée.
Introduction
In both children and adults burns, constitute a very complex pathology which, if severe, affects the entire organism, often endangering the patient's life.1
This form of trauma is one of the commonest causes of hospitalization due to accidents among paediatric patients, especially in very young children.
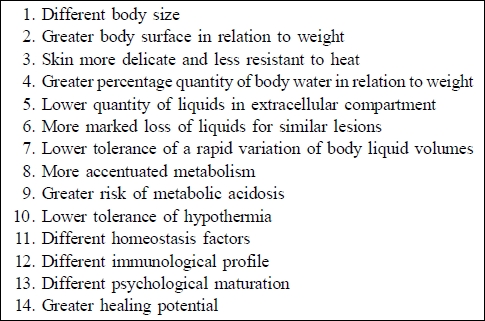
The treatment of paediatric burns (i.e. in patients aged 0 to 12-15 yr - the age definition varies) requires special skills in the paediatric field and dedicated facilities guaranteeing modern, complete, and effective therapy.2 The treatment of burned children differs substantially from that of adults not only because of the smaller body surface areas and the different anatomical structures but also - and more importantly - because of the metabolic processes involved, homeostasis factors, hormonal responses, the immunological profile, the degree of psychological maturation, and healing potential. All these combined factors make children very special patients - the younger they are the more special they become (Table I).1-3
Table I. Important differences in children compared with adults as regards burns.
Epidemiology
According to the most recent international collections of case histories,1-7 paediatric burns account for about 40% of all burn-related hospitalizations. They are frequent worldwide, and from country to country have the same features in common, with some differences related to local customs. The epidemiology of children's burns is different from that of adults.
In Italy paediatric burns are very frequent, especially in the first four years of life, peaking in the second year. They occur most frequently in the home, caused by the spilling of boiling liquids. They rarely cover more than 30% of total body surface area; when caused by flame the lesions have a worse prognosis. Except in a few cases they are not associated with lesions of the airways, concomitant serious traumas, or important previous diseases.
The fact that they are mainly caused by boiling liquids, with predominantly second-degree burns, has a particularly positive affect on prognosis and treatment.
The difference between paediatric burns and those sustained at other ages is not only epidemiological but also clinical because of the basic differences between adults and children, as listed above, differences that determine in children a response to the heat trauma that is quite specific and imposes different treatment from the moment of the burn.
Particular details of treatment of burned children in the first 48-72 hours
The characteristic features of treatment of the burned child in the first 48-72 hours concern: A. treatment at the site of the accident; B. first aid; C. resuscitation; D. local treatment.
A. Particular problems to be tackled at the site of the accident
different assessment of gravity
more rapid onset of hydroelectrolyte imbalance
more difficult venous cannulation
more rapid appearance of breathing complications
more difficult intubation of airways
greater risk of onset of hypothermia
different criteria in the choice of hospital centre
1. Different assessment of gravity
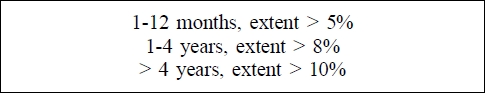
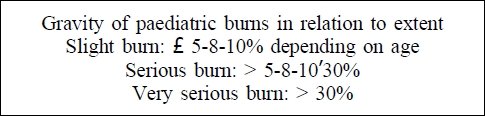
The guidelines are the age and the extent of the wounds, which must necessarily be a rough calculation. It is however important that this calculation should be as accurate as possible as in children the margin between a slight burn and a serious one is minimal. This limit also varies in relation to the patient's age.1
In this phase the depth of the burn is less important in the assessment of its gravity; other parameters (site of burn, concomitant traumas, previous diseases, etc.) have the same importance as in adults.
2. More rapid onset of hydroelectrolyte imbalance
Owing to the different distribution of body fluids, the hydroelectrolyte distribution alters more seriously and more rapidly, especially in very young, seriously burned children.
3. More difficult venous cannulation
In children it is usually difficult to cannulate a useful venous pathway,2 and this is especially true in very small children. Everything is even more complicated in burned children, who also need rapid hydroelectrolyte reanimation. As the minutes go by, it becomes more and more difficult to perform an "open sky" manoeuvre, for which reason it is necessary to use an intraosseous route,9 using the special equipment that rescue workers are provided with.
4. More rapid appearance of breathing complications2,3
This event occurs in children not only when the airways are directly damaged but also when there are deep burns of the face and/or neck owing to the consequent considerable oedema of the soft parts, which becomes progressively more severe and may last hours and even days
5. More difficult intubation of airways3
This manoeuvre, owing to the anatomical structure and the dimension of the upper airways and the child's neck, especially in the case of a very small child, becomes very difficult and sometimes impossible after a burn, with the result that an emergency tracheotomy may have to be performed.
6. Greater risk of onset of hypothermia
Hypothermia occurs owing to the insufficiency of a small child's thermoregulatory system, with the result that the action of cooling burn surfaces, which is a basic form of treatment, must be limited in time in such a patient.
7. Different criteria in the choice of hospital centre
Children require hospitalization more often than adults. Experienced rescue workers have to decide whether young patients have to be transported to the nearest emergency department or directly to a local burns centre, after confirmation that the patient has been accepted.
What care should be given to a burned child at the site of the accident?
Pay special attention to the cooling time of burns in small children with extensive burns (reduce the time!).
Perform analgesia immediately,1,2 as appropriate to the child's age (correct drug and dosage) and to the gravity of the lesions, without any prejudices regarding the use of opioids which at the recommended doses do not create any problems even for small children.
Commence hydroelectrolyte rehydration with an emergency solution and formula (valid for the first 2 h): - 20 ml/kg/h of Ringer's lactate, cannulating an appropriate vessel.1,3
Administer oxygen if airways involvement is suspected.
Insert a bladder catheter only if a lengthy transfer to hospital is expected. Any attempt to catheterise a small child takes up precious time, unless the child presents burns in the perineum, which will cause local oedema.
B. Particular problems to be tackled in the emergency room
Precise assessment according to standard paediatric criteria2
Different criteria for hospitalization
Different criteria for sending patients to the nearest burns centre
1. Precise assessment according to standard paediatric criteria
The hospital doctor must be very precise in the calculation of the extent of burns,1,2 using paediatric maps and thoroughly examining the entire patient, paying special attention to the scalp, which may have extensive burn areas beneath the hair. At this point it is also important to establish the depth of the burns in addition to their site. All observations must be made taking into account the patient's age.
2. Different criteria for hospitalization
The emergency room doctor must always order the hospitalization of burned children:
who present, or are suspected of presenting, inhalation of boiling vapours or caustic substances
who present superficial or deep skin burns (second degree) greater than 5% up to one year, greater than 8% up to four years, and greater than 10% after four years of age
who have third-degree burns (as electrical burns always are and, very often, also chemical burns)> than 2%
who have burns in critical locations, i.e. the face, hands, perineum, or feet
who have deep circumferential burns
who present concomitant lesions in other organs or systems
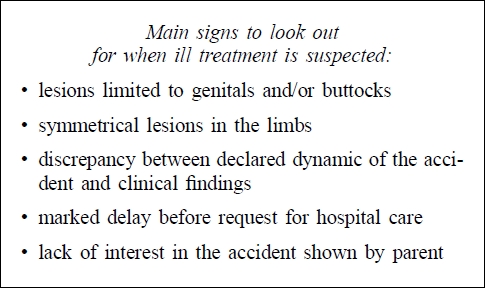
who have suspected or confirmed lesions due to ill treatment2 (see below the main signs to look out for)
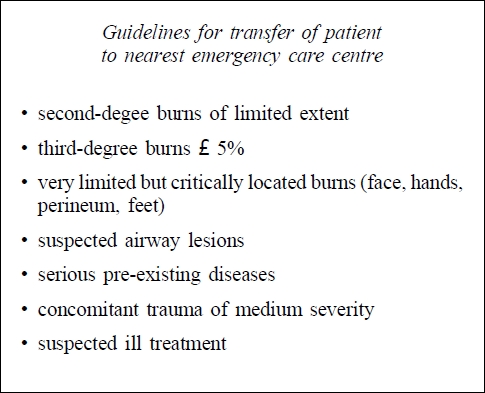
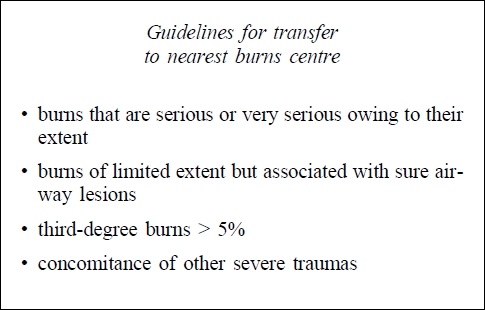
3. Different criteria for sending patients to the nearest burns centre
The emergency room doctor has to base the decision of whether to transfer a patient on an assessment of particular gravity of the patient's condition, necessitating more specialized treatment.
Burned children require hospitalization in a burns centre more frequently than adults. This is because a seriously traumatized child always presents problems requiring special treatment, and this is all the more true if the trauma is a burn, which needs care by medical personnel with particular experience in this pathology.
Burned children must be transferred to a local burns centre if they present:
burns that are serious or very serious owing to their extent
third-degree burns > 5%
burns of slight extent but associated with airway lesions, concomitant serious trauma, or important illnesses
C. Particular problems to be tackled during hydroelectrolyte resuscitation
Owing to the anatomical and physiological differences in the paediatric patient, hydroelectrolyte resuscitation cannot be the same as that of the adult.1,2
A number of precise guidelines govern hydroelectrolyte resuscitation of burned children:1,2
special formulas for children have to be used that allow an exact calculation of the amount of fluid in order to avoid dangerous hypo- and hyperhydration because such patients run a high risk of lung oedema and hypovolaemic shock. For this reason it is preferable to use formulas based on body surface and not on body weight;2
the solution used must have a low sodium concentration in children aged less than one year because complete renal function has not been achieved;10
colloids should be administered after the first 24 h, and in no case until at least 8 h after the trauma. This is to prevent leakage of a greater quantity of fluids from the intravascular compartment that are drawn towards the tissues by proteins which in a state of infusion do not remain in circulation;1,3
it must be possible to administer the maintenance fluids, at least in part, by mouth or using a feeding tube; this can be achieved if after the first hours the child is given fluids by mouth or using a tube in order to avoid post-traumatic intestinal gastroplegia and paresis.12
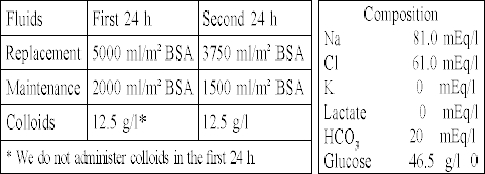
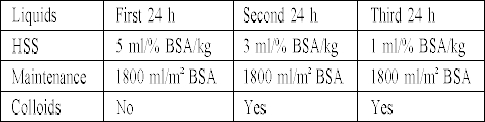
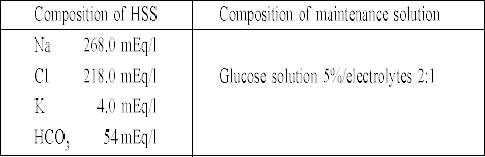
In our centre we use two formulas for hydroelectrolyte resuscitation of severely burned children:
1. Carvajal's formula (as modified by ourselves) for children less than one year old; this provides an amount of sodium that is appropriate for the renal immaturity of such patients.1,10 A particular feature of this formula is that it uses the same quality of fluids for replacement as for maintenance; also, it is based on the patient's body surface, not body weight.
2. HSS, the hypertonic formula suggested by the European Club for Paediatric Burns (ECPB), is based on Monafo's original formula as modified.1,3
D. Particular problems to be tackled in local treatment
In children, who frequently present second-degree superficial and deep burns, the treatment we perform is especially indicated, if possible in the first 24 hours, associating dermoabrasion of the burn surfaces11,12 with the subsequent application, when the burns are covered, with a skin substitute - we use Biobrane.1,14
Dermoabrasion makes it possible:
to perform early superficial necrectomy;
to obtain optimal cleaning of the burn surface;
to assess the depth of the lesions on the basis of the speed of bleeding of the lesions caused by the dermoabrasor;
to obtain a suitable bed for the application of skin substitutes.
When skin substitutes are used in children they present the following advantages:
they reduce local pain;
they make subsequent wound dressing easier and less painful;
they stimulate and promote spontaneous re-epithelialization of second-degree superficial and deep burns.
Conclusions
The treatment of burned children in the first 48-72 h requires a particular approach as regards rapidity of action, accuracy of clinical tests, and careful monitoring since the margins of error are extremely limited and the danger of the onset of important complications is ever present. Any carelessness on the part of the doctors and nurses can have serious repercussions in terms of duration of hospitalization, therapeutic means employed, risk to life, and the quality of future existence.
References
- 1.Grisolia G.A. Le ustioni in età pediatrica. S.E.E. Florence. 1999 [Google Scholar]
- 2.Deich E.A., Rutan R.L. The challenger of children: The first 48 hours". J. Burn Care Rehabil. 2000;21:424–442. [PubMed] [Google Scholar]
- 3.Meuli M., Lochbuhler H. Current concepts in pediatric burn care: General management of severe burns. Eur. J. Pediatric Surg. 1992;2:195–200. doi: 10.1055/s-2008-1063439. [DOI] [PubMed] [Google Scholar]
- 4.Green R.A. et al. Epidemiology of burns in childhood. Burns. 1984;10:368–371. doi: 10.1016/s0305-4179(84)80011-x. [DOI] [PubMed] [Google Scholar]
- 5.Smith R.W., O'Neill T.J. An analysis into childhood burns. Burns. 1985;11:117–124. doi: 10.1016/0305-4179(84)90134-7. [DOI] [PubMed] [Google Scholar]
- 6.Alaghehbandan R., Rossignol A.M., Rastegar Lari A. Pediatric burn injuries in Tehran, Iran. Burns. 2001;27:115–118. doi: 10.1016/s0305-4179(00)00083-8. [DOI] [PubMed] [Google Scholar]
- 7.Ying S.Y., Ho W.S. An analysis of 550 hospitalized pediatric burn patients in Hong Kong. J. Burn Care Rehabil. 2001;22:228–231. doi: 10.1097/00004630-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Rajpura A. The epidemiology of burns and smoke inhalation in secondary care: A population-based study covering Lancashire and South Cumbria. Burns. 2002;28:121–130. doi: 10.1016/s0305-4179(01)00087-0. [DOI] [PubMed] [Google Scholar]
- 9.Evans R.J., Jewkes F., Owen G., McCabe M., Palmer D. Intraosseous infusion - a technique available for intravascular administration of drugs and fluids in the child with burns. Burns. 1995;21:552–553. doi: 10.1016/0305-4179(95)00039-e. [DOI] [PubMed] [Google Scholar]
- 10.Carvajal H.F., Parks D.H. "Burns in Children - Pediatric Burn Management". Year Book Medical Publisher Inc.; Chicago-London-Boca Raton: 1988. [Google Scholar]
- 11.Hansbrough W.B., Hansbrough J.F. Success of immediate intragastric feeding of patients with burns. J. Burn Care Rehabil. 1993;14:512–516. doi: 10.1097/00004630-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Lorthioir J. "Traitement des Brûlures par Ponçage. Physiopathologie et Traitement des Brûlures". Presses Acad. Europ.; Bruxelles: 1964. [Google Scholar]
- 13.Montagnani C.A., Poccianti F. "Emergency dermoabrasion in the treatment of burns in children". Kinderchirurgie. 1969:165–176. [Google Scholar]
- 14.Grisolia G.A., Pelli P., Pinzauti E., Panozzo G., Stuto A., Danti D.A., Billi G., Pampaloni A. Skin substitutes in the treatment of deep partial-skin thickness burns in children: Clinical experience and long-term results. Burns. 1991;17:52–55. doi: 10.1016/0305-4179(91)90012-6. [DOI] [PubMed] [Google Scholar]


