Summary
Hand burns in children, whether isolated or part of massive burns, require special attention. A crucial element in this respect is the preservation and full restoration of hand function. Most cases of severe sequelae after burns are associated with hand burns. From January 2002 to November 2004, 125 children with hand burns and other body burns were treated at the Centre of Burns and Plastic Surgery in Sofia, Bulgaria. This review presents our experience with 71 children with 89 burned hands in the region of the dorsal surface of the hand. Forty-nine hands had isolated dorsal surface burns, and 40 had combined burns, i.e. both dorsal and volar. Of all the hands treated, 69 had superficial burns, which epithelialized spontaneously. Twenty hands with deep dermal and full-thickness burns were subjected to sheet autografting. The review includes many details of the systematic approach to this type of burns. Optimal recovery of hand function can be achieved by accurate planning of treatment. Tracking of long-term results is also included in the general plan of behaviour in this type of burn. Our approach is conservative for superficial burns and active - with early excision and prompt closure with sheet autograft or, in extensive burns, allografting followed by covering with an autograft.
Keywords: ACUTE, DORSAL, HAND, BURNS, CHILDREN
Abstract
Les brûlures de la main, soit isolées soit faisant part de brûlures massives, nécessitent une attention particulière. A cet égard la conservation et la restauration complète de la fonction de la main constituent un élément décisif. La plupart des séquelles sévères à la suite des brûlures sont associées aux brûlures de la main. Dans la période janvier 2002/novembre 2004, 125 enfants atteints de brûlures de la main et d'autres brûlures corporelles ont été traités au Centre des Brûlés et de Chirurgie Plastique à Sofia, Bulgarie. Cet article présente l'expérience des Auteurs avec 71 enfants et 89 mains brûlées dans la région dorsale de la main. Quarante-neuf mains présentaient des brûlures isolées dans la surface dorsale, et 40 présentaient des brûlures associées, c'està dire à la fois dorsales et palmaires. De toutes les mains traitées, 69 étaient atteintes de brûlures superficielles, qui se sont épithélialisées spontanément. Vingt mains atteintes de brûlures profondes dermiques et à toute épaisseur ont été traitées moyennant l'autogreffe à feuillet. L'article décrit beaucoup des détails de l'approche systématique à ce type de brûlures. Il est possible, avec une planification précise du traitement, d'obtenir la récupération optimale de la fonction de la main. Aussi l'observation des résultats à long terme est incluse dans le plan général du comportement pour ce type de brûlure. L'approche décrite est conservatrice pour les brûlures superficielles et active - avec l'excision précoce et la couverture rapide moyennant l'autogreffe à feuillet ou, dans les grandes brûlures, l'allogreffe suivie par la couverture avec une autogreffe.
Introduction
As a result of increased post-burn survival, the main goal of treatment is not only survival itself but also, in hand burns, maximum functional restoration and aesthetic recovery of the hands. Along with the general treatment, special attention has to be paid to the quality of healing of burned hands. Our retrospective analysis considers the incidence and mechanisms of this type of burn as well as the methods of treatment of superficial and deep burns.We also include methods for rehabilitation and monitoring of long-term results in the whole treatment process.
Materials and method
From January 2002 to November 2004, a total of 125 children with hand burns and other body burns were treated at the Centre of Burns and Plastic Surgery in Sofia,Bulgaria. Of these children, 71 (56.8%) presented 89 hands burned in the region of the dorsal surface: 49 hands had isolated dorsal surface burns and 40 had combined burns, i.e. both dorsal and volar burns. The 89 hands treated presented burn injuries of all degrees of severity. All the children were actively monitored for up to one year after discharge. The analysis was based on age, burn size and depth, mechanism of burns, palmar involvement, surgical course, sequelae and the necessity of reconstructive surgery, rehabilitation, and the degree of hand function restoration.
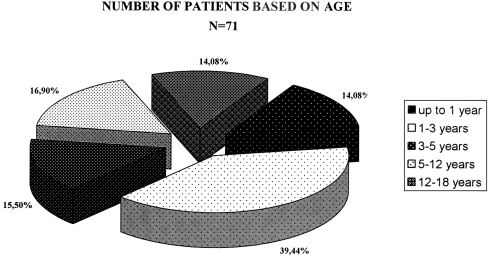
The incidence of injury in relation to the number of patients and age range was as follows ( Fig. 1 ):
Fig. 1. Number of patients based on age.
- up to 1 yr - 10 children (14.08%)
- 1 to 3 yr - 28 children (39.44%)
- 3 to 5 yr - 11 children (15.50%)
- 5 to 12 yr - 12 children (16.90%)
- 12 to 18 yr - 10 children (14.08%)
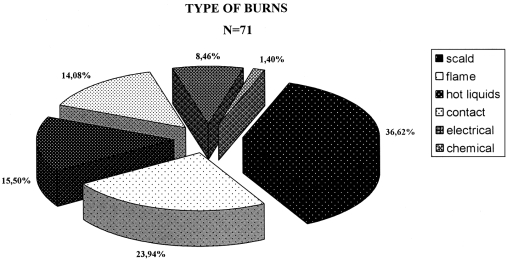
Fig. 2. Type of burn.
The incidence in relation to the type of burn was as follows (Fig. 2):
- scald burns - 26 children (36.62%)
- flame burns - 17 children (23.94%)
- hot liquids - 11 children (15.50%)
- contact burns - 10 children (14.08%)
- electrical burns - 6 children (8.46%)
- chemical burns - 1 child (1.40%)
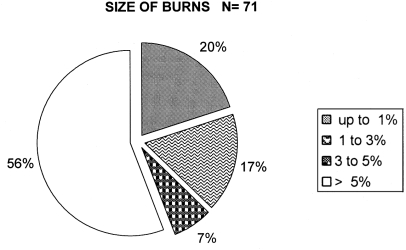
The incidence on the basis of burn size was as follows ( Fig. 3 ):
Fig. 3. Size of burn.
- 20% of the children presented burns in up to 1% TBSA
- 17.14% presented burns in 1-3% TBSA
- 7.14% presented burns in 3-5% TBSA
- 55.72% presented burns in more than 5% TBSA
There were 40 hands with dorsal and volar surface burns. Twenty hands required surgery, which represented 22.47% of all 89 hands. Four children with six burned hands required necrotomy and fasciotomy. Amputation of the distal phalanges was required in four fingers of the right hand in one child.
The injured hands were treated according to our routine practice in the following way. A detailed initial evaluation of both the patient and the burned hands was performed, paying particular attention to digital perfusion. Superficial burns were locally managed with silver sulphadiazine and splinting. Full-thickness and deep dermal burns underwent tangential or total excision and sheet autografting.Surgery was performed as soon as it was practical, usually within 72 h of the injury. Hands not requiring surgery were bandaged twice a day and maintained in functional position with the metacarpophalangeal joints at 70-90° flexion, the interphalangeal joints in extension, the first web space open, and the wrist at approximately 25° of extension. This position was maintained by a thermoplastic splint. The upper extremities were elevated to minimize oedema. The hands that underwent surgery were maintained and immobilized in the same functional position for 7 days, followed by passive and active rehabilitation with maximum stimulation of natural hand motion.
Results
Of the children with superficial hand burns not requiring surgical intervention, five (7.24%) developed sequelae requiring reconstructive procedures during the first year post-burn. These procedures consisted of three Z-plasties in the region of the second and third commissures and two flexion contractures of the fingers. Of the 20 hands subjected to surgery, three developed sequelae and required reconstructive surgery. In these three cases, reconstruction involved the region of the second and third commissures, plus wrist and finger extension contracture corrections. In 92.76% of the hands not requiring surgery and 85% of the hands requiring it, the functional results showed normal function. Abnormal function, but the ability to perform usual everyday activities, was seen in 7.24% of hands not subjected to surgery and in 15% of those subjected to surgery. In the second group, normal function was achieved after reconstructive operation and rehabilitation.
We present one case, patient N.G.H., 8 years old, with 25% TBSA burns after a fire accident (Figs. 4 , 5 , 6 , 7 ).
Fig. 4. Patient N.G.H., 8 years old, immediately after accident.
Fig. 5. Necrotomy performed during admission.
Fig. 6. Early surgical excision day 2 post-burn.
Fig 7a, Final result before discharge.
Discussion
The initial evaluation of a burned hand is extremely significant and determines the future course of surgery. 1, 2Important basic points in this respect are the mechanism of the injury, the character of the burning agent, the possibility of other injuries to the hand, the temperature and contact time when burns are caused by hot liquids, and previous hand diseases. Another significant assessment includes verification of the presence of adequate perfusion of the burned hand. Accurate estimation of burn depth is difficult immediately after injury.
The widely known diagnostic methods are of some help to the surgeon but they are not sufficient. Differentiation should usually be made between superficial, deep dermal, or full-thickness burns and burns involving tendons and joint capsules. 3, 4, 5, 6
The condition of the hand is examined very often during the first 24 h and, in case of need (clinical evidence of progressively diminished hand perfusion), necrotomy and fasciotomy with electrocautery are performed by axially oriented medial and lateral incisions through the eschar. 7The restoration of perfusion is examined before performing digital necrotomy.
In the presence of large surface area burns, in which resuscitation and initial stabilization play a leading role, the hands should be elevated higher than the horizontal line and splinted in functional position. This optimal position includes the interphalangeal joints in extension, the metacarpophalangeal joints at 70-90° of flexion, and the wrist at 20-30° of extension. The thumb is kept in neutral position with the first web space open. A splint is always placed to maintain this position.
Fig 7b. Final result before discharge.
Most children with superficial hand burns achieve excellent functional and cosmetic results with topical wound care using silver sulphadiazine and epithelializing agents, and hand therapy. 8, 9, 10Deep dermal and full-thickness burns require excision of non-vital tissue, as soon as it is practical, and closure with sheet autografts without meshing. Sheet autografts have to be used except in cases of large surface area burns, where allografts can be initially applied. The grafted hand is covered with compressive gauze wrap and splinted. After the stabilization of autografts (after 7 days), the hands are left open. The rehabilitation programme starts in this period - apart from splinting, this includes hydro-procedures, massage in the region of the small joints, and the encouragement of active hand motion.
Conclusion
In conclusion, it can be said that this organized approach to hand dorsal surface burns provides excellent functional and cosmetic results.
References
- 1.Tancheva D., Gioreva E., Novkov H. Intensive care of life-threatening shock in children with major burns. First International Symposium on Cardiovascular Prevention and Paediatric Cardiology Sofia Bulgaria September. 1995:260–73.
- 2.Sheridan R.L., Hurley J., Smith M.A., et al. The acutely burned hand: Management and outcome based on a ten-year experience with 1047 acute hand burns. Trauma. 1995;38:406–11. doi: 10.1097/00005373-199503000-00022. [DOI] [PubMed] [Google Scholar]
- 3.Sheridan R.L., Schomaker K.T., Lucchina L.C., et al. Burn depth estimation by use of indocyanine green fluorescence: Initial human trial. J. Burn Care Rehabil. 1995;16:602–4. doi: 10.1097/00004630-199511000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Burke J.F., Quinby W.C., Bondoc C.C. Primary excision and prompt grafting as routine therapy for the treatment of thermal burns in children. Hand Clin. 1990;6:305–17. [PubMed] [Google Scholar]
- 5.Burke J.F. Efficacy of tangential excision and immediate autografting to deep second-degree burns to the hand. J. Trauma. 1997;19:673. doi: 10.1097/00005373-197909000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Cryer G., Anigian G., Miller F., et al. Effects of early tangential excision and grafting on survival after burn injury. Surg. Gyn. Obstetr. 1991;173:449–53. [PubMed] [Google Scholar]
- 7.Robotti E.B. The treatment of burns: An historical perspective with emphasis on the hand. Hand Clinics. 1990;6:163–90. [PubMed] [Google Scholar]
- 8.Covey M.H., Dutcher K., Marvin J.A., Heimbach D..M. Efficacy of continuous passive motion (CPM) devices with hand burns. J. Burn Care Rehabil. 1988;9:397–400. [PubMed] [Google Scholar]
- 9.Dutton R. Rehabilitation frame of reference. In: Hopkins H.L., editor; Smith H.D., editor. Willard and Sparkman's Occupational Therapy. J.B. Lippincott; Philadelphia: 1993. pp. 79–81. [Google Scholar]
- 10.Barillo D.J., Harvey K.D., Hobbs C.L., et al. Prospective outcome analysis of a protocol for the surgical and rehabilitative management of burns to the hands. Plast. Reconstr. Surg. 1997;100:1442–9. doi: 10.1097/00006534-199711000-00010. [DOI] [PubMed] [Google Scholar]