Summary
Scars are a consequence of the natural way of wound healing and replacement of the damaged part of the skin. Hypertrophic scars and keloids are formed as a result of the process of abnormal wound healing, causing aesthetic and functional deformities, discomfort, and disturbance of children's normal growth. The prophylaxis and treatment of these scars, i.e. burns sequelae, are a significant moment in the treatment of children with burns. The objectives of the present study are methods for the prophylaxis and non-operative treatment of hypertrophic scars and keloids in children with burns. Altogether, 547 children with 485 burns sequelae - fresh scars in the period of healing and old hypertrophic scars (377) and keloids (108) - were treated in our Clinic of Children's Burns for a period of five years. The age of the patients varied between 0 and 18 years. Non-operative treatment was applied in 276 children. The patients were divided into two groups according to the treatment applied. Compression, intralesional application of triamcinolone acetonide, and silicone sheets were employed in the first group (84.06%), while only silicone sheets were applied to children in the second group (15.94%). Unaffected areas and areas adjacent to the scar were used as control areas. The sequelae monitored in both groups were assessed using the Vancouver Scar Scale. The children were monitored in an out-patient department. The results obtained are regardless of age, anatomical location, and scar aetiology. In old scars, and especially in keloids, the treatment proved to have variable results, according to the assessment parameters. We were satisfied with the improvement of the parameters during the course of treatment and with the good final results, which we consider a therapeutic success. Analysis of the results shows that the parameters improved slowly during the course of treatment, the process being most active during the first few weeks. The use of compressive therapy, the intralesional application of triamcinolone acetonide, and silicone sheets may prevent and minimize the formation of hypertrophic scars and keloids. The methods of non-operative treatment of these abnormal scars continue to be discussed and developed.
Keywords: non-operative, treatment, hypertrophic, scars, keloids, burns, children
Abstract
Les cicatrices sont une conséquence du mode naturel de la guérison des lésions et du remplacement des portions endommagées de la peau. Les cicatrices hypertrophiques et les chéloïdes se forment comme résultat du processus de la guérison anormale des lésions, ce qui provoque des difformités esthétiques et fonctionnelles, des malaises et des troubles de la croissance normale de l'enfant. La prophylaxie et le traitement de ces cicatrices, c'est-à-dire des séquelles des brûlures, constituent un moment significatif dans le traitement des enfants brûlés. Les Auteurs de cette étude se sont proposés d'examiner les méthodes de la prophylaxie et du traitement non-opératoire des cicatrices hypertrophiques et des chéloïdes chez les enfants brûlés. Ils ont traité 547 patients atteints de séquelles de 485 brûlures - de nouvelles cicatrices en voie de guérison et de vieilles cicatrices hypertrophiques (377) et des chéloïdes (108) - dans leur Clinique des Brûlures de l'Enfance pendant une période de cinq ans. L'âge des patients oscillait entre 0 et 18 ans. Le traitement non-opératoire a été appliqué dans 276 patients. Les enfants ont été divisés en deux groupes selon le type de traitement qu'ils ont reçu. Les patients du premier groupe (84,06%) ont été traités avec la compression, l'application intralésionale d'acétonide de triamcinolone et des feuilles de silicone, tandis que les enfants du deuxième groupe (15,94%) ont reçu seulement des feuilles de silicone. Des zones non touchées et d'autres zones adjacentes à la cicatrice ont été utilisées comme zones témoins. Les séquelles contrôlées dans tous les deux groupes ont été évaluées moyennant l'Echelle des Cicatrices de Vancouver. Les enfants ont été observés dans un service ambulatoire. Les résultats obtenu ne prennent pas en considération l'âge, le site anatomique ou l'étiologie cicatricielle. Pour ce qui concerne les cicatrices vieilles, et particulièrement les chéloïdes, le traitement appliqué produisait, selon les paramètres d'évaluation, des effets variables. Les Auteurs se sont convaincus de l'amélioration des paramètres au cours du traitement et des bons résultats finaux, ce qu'ils considèrent un succès thérapeutique. L'analyse des résultats démontre que les paramètres amélioraient lentement au cours du traitement, avec l'activité majeure du processus pendant les premières semaines. L'emploi de la thérapie compressive, l'application intralésionale d'acétonide de triamcinolone et les feuilles de silicone peuvent prévenir ou minimiser la formation des cicatrices hypertrophiques et des chéloïdes. Les méthodes du traitement non-opératoire de ces cicatrices anormales continuent â être discutées et développées.
Introduction
Burn injury (whether limited or widespread) frequently leads to long-lasting physical, aesthetic, functional, psychological, and social consequences. Scars, especially those following deep burns, may cause emotional disorders, a variety of psychopathological conditions, and disturbances in a child's normal growth. The prophylaxis and treatment of hypertrophic scars and keloids are a significant period in the care of children with burns and constitute a challenging task for surgeons and rehabilitators.
Keloids and hypertrophic scars are an atypical process of wound healing that develops after skin injury healing. These scars consist of excessive dense fibrous tissue growing in all directions and elevated above the level of the skin. Keloids were first described in an Egyptian papyrus 3000 years ago and later defined in detail by Alibert in 1806, who suggested the use of this term. 1
An appropriate classification of scars is a significant element because the differences in their clinical types determine the therapeutic approach. The existence of a variety of classification schemes is based on the need of optimal clinical reliability. 1, 2Post-trauma wound healing leads to different types of scars: 1. normal scar; 2. wide-stretched scar; 3. atrophic scar; 4. scar contracture; 5. hypertrophic scar; 6. keloid. Scars that are difficult to categorize are defined as transient - if a growing scar continues to grow after a year, the probable diagnosis would be a keloid, while a hypertrophic scar shows signs of regression within such time. 3Another commonly used classification defines scars as follows:
mature scar - a completely developed scar
immature scar
linear hypertrophic scar
wide-stretched scar
small keloid - this does not grow back within a year after the injury and does not extend beyond the borders of the original wound
big keloid - this is wide (> 0.5 cm) and still continues to grow after a year
The objectives of our study are hypertrophic scars and keloids, their prophylaxis, and conservative treatment. These scars are similar in appearance and are considered by some researchers to be relatively indistinguishable despite considerable differences in their histomorphology and behaviour. The two types of scar can be described as variations of typical wound healing and are characterized by an excessive synthesis of collagen due to increasing activity of various types of fibroblasts and especially of myofibroblasts. In spite of some similarities in their biology, they have some distinctive differences. 3The clinical differences between hypertrophic scars and keloids are especially significant. Hypertrophic scars appear at an earlier stage after the trauma, while keloids develop several months or years later. The former may regress spontaneously within 12-18 months, whereas the latter persist and may grow over time. Hypertrophic scars are more frequently localized in the flexor areas than in the extensor areas in contrast to keloids, whose most frequent locations are the earlobes, breast, shoulders, neck, upper extremities, and face. Hypertrophic scars remain limited to the area of the initial trauma, while keloids extend beyond this area. The complications in hypertrophic scars are contractures, possible functional impairment, and motion limitation if the location is over a joint. Tenderness, pain, a burning sensation, and itching (the commonest symptom) may be observed in keloids. Histologically, both hypertrophic scars and keloids are characterized by a high density of fibroblasts and collagen fibrils, a rich vasculature, a thickened epidermal cell layer, and high mesenchymal cell density. 3
The process of post-burn wound healing and the level of functional impairment vary according to the severity of the tissue injury. In superficial burns, in which the epithelium and part of the dermis are damaged, the wound heals more rapidly and restoration is complete, followed only by changes of pigmentation. Only a limited number of cases develop scars. Owing to the longer treatment period, deep dermal and full-thickness burns are always suspicious because they may cause hypertrophic scars and keloids. Many factors influence the formation and severity of post-burn hypertrophic scars and keloids. 1, 4Genetic predisposition, race, anatomical location, age, and burn depth are defined as unmanageable factors, while infection (general and local), the manner of wound healing (operative or non-operative), and wound closure tension are manageable factors. Scarring is a dynamic process with a marked activity within the first 18 months. Knowing the factors influencing this process, prevention of the formation of hypertrophic scars and keloids is more effective than their subsequent treatment. In this sense, the whole treatment of post-burn wounds is subjected to a single goal, i.e. reducing the risk of the development of problem-causing scars, while at the same time prevention in the transitional period, before diagnosis of an immature scar, needs to be included in the treatment plan.
Both in theory and in practice, prevention and nonoperative treatment may be similar. 4The main goals of the prophylaxis and treatment of hypertrophic scars and keloids are restoration of the injured anatomical area's functional activity, relief of symptoms, and prevention of their appearance or recurrence. The best therapeutic option is the complex approach, which includes operative and nonoperative treatment. In the present study, we consider noninvasive methods, i.e. additional tools, applied initially for the management of hypertrophic scarring, as well as the effectiveness of the related treatment. There is no confirmed standard method for the treatment of hypertrophic scars and keloids. Here rises the question as to what criteria to use for the assessment of scars and their monitoring during the treatment process. There is no common agreement regarding the most appropriate tool or tools for the assessment of the lesion and its evolution. The Vancouver Scar Scale (VSS), described by Sullivan et al. in 1990, 5is commonly used and is considered the most reliable. It allows assessment of the pigmentation, vascularity, pliability, and height of the scar monitored. The fact that there are some practical problems in the application of the scale imposed the development of new, modified assessment methods. Itching in the damaged areas during the period of scar formation is a frequent complaint but is not included in the scale. The estimation of pliability is carried out by testing the scar pleat using a six-degree scale: normal, supple, yielding, firm, banding, and contracture type of tissue. The scar's functional mobility, which is associated with pliability and contracture, is included in these parameters. Another drawback of this scale is the difficult separation, in some cases, of the two parameters associated with colour, i.e. vascularity and pigmentation. Photos (taken regularly) and biopsy analyses (where possible) are included in the assessment made by the scale.
Materials and methods
For the prophylaxis and treatment of hypertrophic scars and keloids we apply (separately or in combination) the following non-invasive methods: compressive treatment and, if necessary, splinting (temporary or permanent), intralesional application of corticosteroids, and silicone sheets stuck to the skin. All these methods are accompanied by hydrotherapy and a variety of hydrating lotions and creams.
A total number of 547 children with 485 burns sequelae - fresh scars in the period of healing and old hypertrophic scars (377) and keloids (108) localized in different anatomical areas - were examined in our Clinic of Children's Burns for a period of five years. The age of the patients varied between 0 and 18 yr. The most frequently treated and monitored children were in the age range of 1 to 11 yr. In 308 children (56.31%), treatment started within one year of the burn. Non-operative treatment according to the method described was applied in 276 children.Depending on the type of burn, the most frequently treated burns sequelae were due to hot water, followed by flame burns. The highest (and comparatively equal) incidence of anatomical location was in the area of the body and the upper and lower extremities.
The children were placed in groups according to the local treatment applied. The group treated with compression, intralesional application of triamcinolone acetonide, and silicone sheets was the largest group - 232 (84.06%), followed by that in which only silicone sheets were applied - 44 (15.94%). Unaffected areas and those adjacent to the scar were used as control areas. The sequelae monitored in both groups were assessed using the VSS criteria. The cases were photo-documented and a biopsy was carried out when possible. Demographic data, together with scar analysis data (burn depth in the injured area, spontaneous healing, operated or donor site), were documented. Current treatment of the scars was also recorded. The presence or lack of itchy sensation in the scar area was added to the VSS criteria. Calorie-metric, profile-metric and planometric methods for assessment of the mechanical parameters (tonometry, goniometry) were used.
We applied compressive treatment (compression garments) for the prophylaxis and maintaining of hypertrophic scarring in fresh scars. This was applied continuously 24 h a day starting from the moment of epithelialization or operative closure of the wound for a period of one year, at a mean pressure of 24 mm Hg. Application of triamcinolone acetonide (10-40 mg/ml) is one of the principal methods of non-operative treatment of hypertrophic scars and keloids. It is applied in combination with silicone sheets and compression. Application began when the initial signs of hypertrophic scars, i.e. already formed ones and keloids, were observed. This method is used as an intralesional application in order to avoid reduction or atrophy of the surrounding skin. It is applied three or four times a month. Another method used was the application of silicone sheets (Sica Care) and elastomers as a single approach (44 children) or in combination with the other methods. The treatment started immediately after wound closure (operative or spontaneous). During the first week the silicone sheet was placed for 8 h, after which it was kept permanently until the end of treatment. Depending on the results obtained, the application period can last from three to eight months.
Results
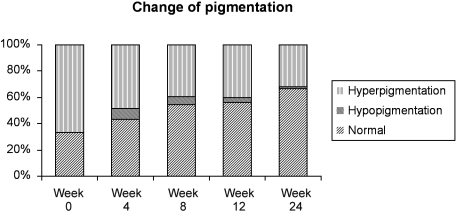
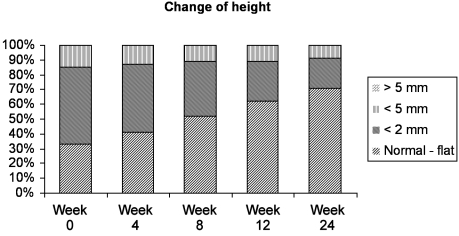
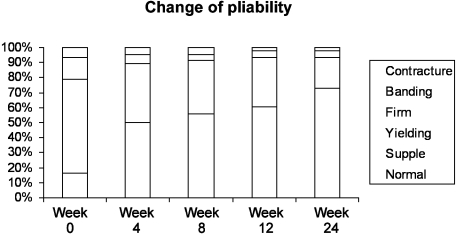
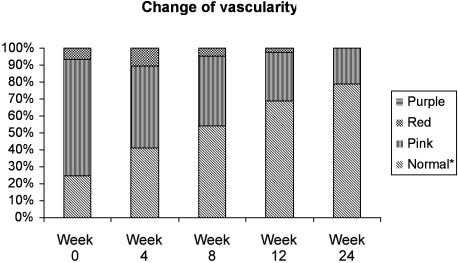
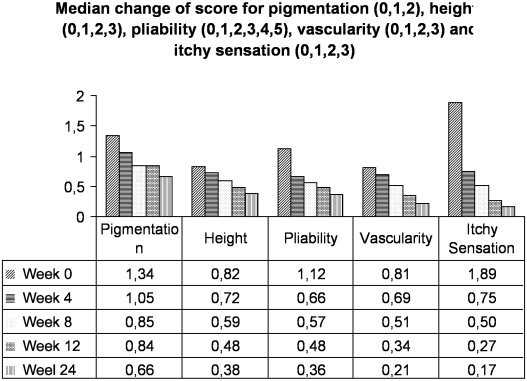
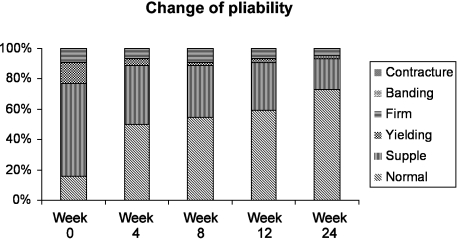
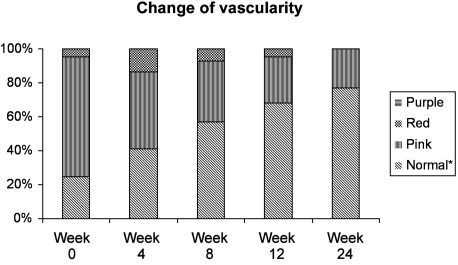
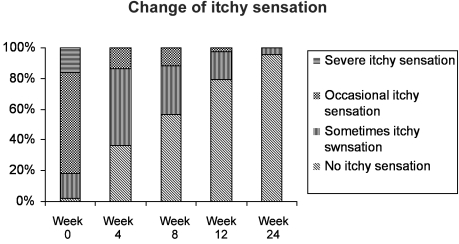
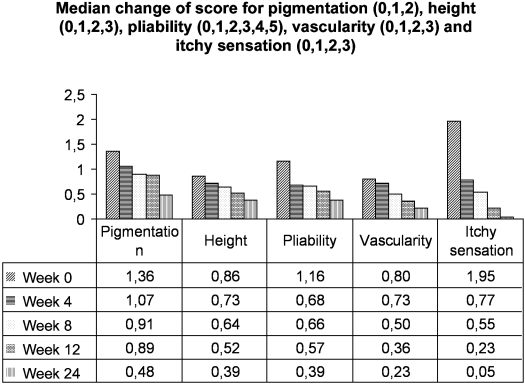
The patients were monitored in an out-patient department. The assessment of the results of treatment was documented. The results were not related to the child's age, the anatomical location of the scar, or its aetiology. In old scars, and especially in keloids, the treatment yielded variable results in the assessment parameters. For example, the itchy sensation and vascularity showed clearer improvement than the other parameters (Figs. 1 , 2 , 3 , 4 5 6 , 7 8 , 9 10 , 11 , 12 ).
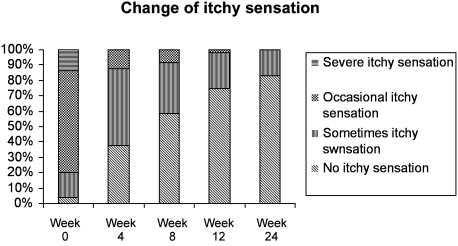
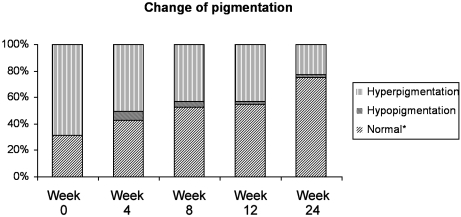
Fig. 1. Change of pigmentation for the group treated with compression, intralesional application of triamcinolone acetonide, and silicone sheets.
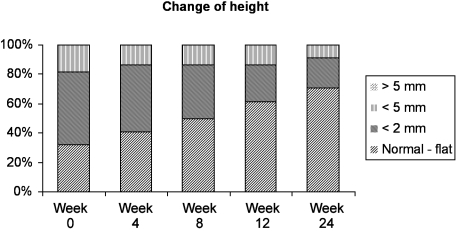
Fig. 2. Change of scar height for group treated with compression, intralesional application of triamcinolone acetonide, and silicone sheets.
Fig. 3. Change of pliability for the group treated with compression, intralesion application of triamcinolone acetonide, and silicone sheets.
Fig. 4. Change of vascularity for group treated with compression, intralesional application of triamcinolone acetonide, and silicone sheets.
Fig. 5. Change of itchy sensation for group treated with compression, intralesional application of triamcinolone acetonide, and silicone sheets.
Fig. 6. Median change of cores for pigmentation, height, pliability, vascularity, and itchy sensation for group treated with compression, intralesional application of triamcinolone acetonidel, and silicone sheets.
Fig. 7. Change of pigmentation for group treated with silicone sheets.
Fig. 8. Change of height for group treated with silicone sheets.
Fig. 9. Change of pliability for group treated with silicone sheets.
Fig. 10. Change of vascularity for group treated with silicone sheets.
Fig. 11. Change of itchy sensation for group treated with silicone sheets.
Fig. 12. Median change of scores for pigmentation, height, pliability, vascularity, and itchy sensation for group treated with silicone sheets.
Scars, regardless of their aetiology, cannot disappear completely, for which reason unrealistic results were not expected.
The improvement of the parameters during the course of treatment and the good results obtained were in our opinion satisfactory and we consider them a therapeutic success. Analysis of the results shows that the parameters improved slowly during the course of treatment, this process being most active during the first few weeks. With regard to the aesthetic outcome, we rated the optimal result to be a pale, non-pigmented, pliable, painless, nonbulgy scar that did not prevent growth.
Side effects were seen in both groups. In the first group these were associated with the application of triamcinolone acetonide, i.e. atrophy in 10 children, which disappeared within a year of termination of treatment, when the tissue occupied the architectonics normal for the particular area. After the use of silicone sheets, we observed petechial rash and mild maceration in 17 children from both groups. These effects disappeared after an interval of several days.
Discussion
The prophylaxis of hypertrophic scar and keloid formation is more effective than its subsequent treatment. The prophylaxis involves the application of treatment that reduces the risk of the development of problem-causing scars. nalysis of the results of our study indicates clearly that preventive and treatment methods are similar. Knowing the factors that influence the development of hypertrophic scars and keloids, we have to pay special attention to children, who are exposed to an increased risk. The application of strong antiseptics, early wound closure, and good surgical technique are the principal methods for preventing the development of hypertrophic scars and keloids.
The treatment of hypertrophic scars resulting from burns is difficult and often requires a combination of invasive and non-invasive methods. Non-invasive methods (alone or in combination with other methods) include individual compressive treatment, splinting, application of triamcinolone acetonide, silicone sheets, and gels, as well as a great variety of additional means such as hydrating creams, antihistamine drugs, radiation therapy, cryosurgery, laser therapy, treatment with interferon, and intralesional application of Verapamil (a calcium antagonist). None of these methods gives completely satisfactory results.
Compressive treatment was first devised by Dr Silverstein and popularized by Linares at al. (Galveston Shriners Burns Institute) in the early 1970s. 4, 5, 6It is the cheapest and most widespread method for the prevention and treatment of hypertrophic scars and keloids. The pressure needs to be maintained within a range of 24-30 mm Hg for the method to be effective. The compression garment has to be worn permanently for up to 6-12 months. The exact mechanism of compressive action is not fully understood. Mechanical compression controls the release of cytokines in a hypertrophic scar and reduces the binding of collagen fibres. 6, 7, 8It can be combined with silicone elastomers, especially in concave surface areas of the body. The method was discovered and studied by Van den Kerckhove et al. in 1991.
The intralesional application of 10-40 mg/ml of triamcinolone acetonide is an old and well-tried method for treating hypertrophic scars and keloids. It can be applied separately or in combination. 4The treatment does not start immediately after burn wound closure but during the process of scar evolution, when the initial signs of hypertrophic scars are observed, i.e. usually 1-2 months later.
The earlier the placement of corticosteroids in the lesion (when the scar is supple), the better the results. The applications are performed three or four times at one-month intervals. The application in old scars and keloids softens, flattens, and smoothes them. The formation of teleangiectasia, changes of pigmentation, and skin atrophy in the surrounding tissue are considered a disadvantage of the treatment. These complications disappear within several months or a year of termination of treatment, whereas the fading of pigmentation changes takes longer. 4, 9
The mechanism of action of silicone gel and sheets is not altogether understood, despite numerous investigations in this field. 10The outcome of this treatment is very good, whatever the child's age, the manner of attachment, or the anatomical location of the hypertrophic scar and keloid. It can be applied as a single method or in combination with other treatment methods. Silicones are completely synthetic polymers, usually based on dimethyl siloxane monomer. They contain a repeated structural unit, SiO(CH3) 2, and therefore have a silica-derived backbone and organic groups as SiOC chains attached directly to a silicon atom via silicon carbon bonds. Three types of silicone are used in the treatment of scars, namely fluids, gels, and elastomers. The application of silicone sheets in post-burn scars was described by Perkins et al. and later by Davey et al. Silicone elastomers and sheets are applied directly on the scar without exerting any pressure or without increasing it, giving similar good clinical results at the same time. The exact mechanism of action has not been clarified and its clinical investigation continues.
The investigations include analysis of a variety of factors - pressure, oxygen tension, hydration, silicone leakage, changes of microcirculation in the scar, increases in the local temperature, and electrostatic influence. Occlusion and increased hydration of the scar are considered the most likely factors of the mechanism of action. 11, 12
The advantages of silicone sheets and gels are as follows: 1. comfort in application; 2. no hindrance to joint movements; 3. easy to use; 4. ideal solution to concavity problems; 5. they are especially useful in children who cannot tolerate the pain of other management procedures.The method is simple, safe, and effective for the treatment of hypertrophic scars and keloids. After application, an improvement of the clinical parameters (colour, pliability, vascularity) and relaxation of the patient's itching and pain are observed within some weeks. This therapy can give rise to slight complications, such as rash, maceration, and redness of the intact skin, especially when combined with compression garments. These effects disappear when treatment is withdrawn or the wearing time of the sheets reduced. Our experience in using silicone gels, sheets, and elastomers shows that they are extremely effective and convenient tools for prophylaxis and management of post-burn hypertrophic scars and keloids. Precise observation of the application procedures and good hygiene are the key to the success of this method. In cases of single application, the process starts after a hydroprocedure with an application for 8 h during the first week, after which it is worn continuously 24 h a day with some breaks for hygiene procedures. In cases of combined application with compressive therapy in a warm climate, application time can be 12 h a day. The treatment period is 6-12 months. 10, 12
The regular monitoring of the evolution of hypertrophic scars and keloids is of special importance. Assessment methods for the outcome of treatment have been widely discussed in the literature, the most favoured being the VSS. This scale is one the most commonly used for the assessment of scars. 5, 13, 14Scar assessment is more reliable when estimated by more than two examiners (the optimal number is three), which may be an impediment in clinical environment. In our clinical practice, for assessment of the treatment applied, we used these scale parameters, photographs (Figs. 13 a , 13 b , 13 c , 13 d , 13 e , 14 a , 14 b , 14 c , 15 a , 15 b , 15 c , 16 a , 16 b , 16 c ), and histological analyses (where possible). 14
Fig. 13 a. Thirty-month-old child after operative treatment for hot liquid burn in the areas of neck, breast, and shoulder.
Fig. 13 b. Application of triamcinolone acetonide to hypertrophic scar in same child.
Fig. 13 c. Application of silicone sheets on epithelialized operated areas.
Fig. 13 d. Pressure garments over a silicone sheet.
Fig. 13 e. Final outcome.
Fig. 14 a. Hypertrophic scars on 3-yr-old child after operative treatment in the breast and abdomen.
Fig. 14 b. Compressive therapy.
Fig. 14 c. Final outcome.
Fig. 15 a. Twenty-four-month-old child after scalding.
Fig. 15 b. Application of silicone sheets over epithelialized areas.
Fig. 15 c. Final outcome.
Fig. 16 a. Four-yr-old child after scalding in abdomen and lower extremities.
Fig. 16 b. Application of triamcinolone acetonide to fresh hypertrophic scars.
Fig. 16 c. Final outcome.
Conclusion
The prophylaxis and treatment of post-burn hypertrophic scars and keloids is a difficult process and often requires the application of a combination of techniques, the development of individual programmes of treatment, and regular monitoring in an out-patient department. Unlike other types of injuries, burns cause permanent sequelae. Deep-dermal, full-thickness, limited, and superficial burns may lead to the formation of hypertrophic scars and keloids, which apart from their unsightly aesthetic appearance frequently cause functional impairment and disturb a child's normal growth. Timely wound closure and the development of an individual programme for prophylaxis and the possible treatment of hypertrophic scars and keloids are crucial for excellent outcomes in children with burns.
References
- 1.Berman B., Kapoor S. Keloid and hypertrophic scar. eMedicine. 2001;2:1–12. [Google Scholar]
- 2.Berman B., Bieley H.C. Keloids. J. Am. Acad. Dermatol. 1995;33:117. doi: 10.1016/0190-9622(95)90035-7. [DOI] [PubMed] [Google Scholar]
- 3.Shaffer J.J., Taylor S.C., Cook-Bolden F. Keloidal scars: A review, with a critical look at therapeutic options. J. Am. Acad. Dermatol. 2002;46:S63. doi: 10.1067/mjd.2002.120788. [DOI] [PubMed] [Google Scholar]
- 4.Alster T.S., West T.B. Treatment of scars: A review. Ann. Plast. Surg. 1997;39:418. doi: 10.1097/00000637-199710000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan T., Smith J., Kermode J., McIver E., Courtemanche D.J. Rating the burn scar. J. Burn Care Rehabil. 1990;11:256. doi: 10.1097/00004630-199005000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Young A., Tan P., Berman B., Villa A., Poochareon V. Topical application of semi-permeable, semi-occlusive, non-silicone-based dressing for keloid treatment. Cosmet. Dermatol. in press. [Google Scholar]
- 7.Bieley H.C., Berman B. Keloids. Effects of a water-impermeable, non-silicone-based occlusive dressing on keloids. J. Am. Acad. Dermatol. 1996;35:113. doi: 10.1016/S0190-9622(96)90521-6. [DOI] [PubMed] [Google Scholar]
- 8.Rayner K. The use of pressure therapy to treat hypertrophic scarring. J. Wound Care. 2000;9:151. [PubMed] [Google Scholar]
- 9.Tang Y.W. Intra- and post-operative steroid injections for keloids and hypertrophic scars. Br. J. Plast. Surg. 1992;45:371. doi: 10.1016/0007-1226(92)90007-k. [DOI] [PubMed] [Google Scholar]
- 10.Perkins K., Davey R.B., Wallis K. Silicone gel: A new treatment for burn scars and contractures. Burns. 1983;9:201–4. doi: 10.1016/0305-4179(83)90039-6. [DOI] [PubMed] [Google Scholar]
- 11.Sawada Y., Sone K. Treatment of scars and keloids with a cream containing silicone oil. Brit. J. Plast. Surg. 1990;43:683–8. doi: 10.1016/0007-1226(90)90189-7. [DOI] [PubMed] [Google Scholar]
- 12.Sawada Y., Sone K. Hydration and occlusion treatment for hypertrophic scars and keloids. Brit. J. Plast. Surg. 1992;45:599–603. doi: 10.1016/0007-1226(92)90027-u. [DOI] [PubMed] [Google Scholar]
- 13.Flores J., Berman B., Burdick A., Jonusas A.M. The effectiveness of a new method for assessing induration. J. Am. Acad. Dermatol. 1998;39:1021. doi: 10.1016/s0190-9622(98)70283-x. [DOI] [PubMed] [Google Scholar]
- 14.Bariza M.J., Baryza G.A. The Vancouver Scar Scale: An administration tool and its interrater reliability. J. Burn Care Rehabil. 1995;16:535. doi: 10.1097/00004630-199509000-00013. [DOI] [PubMed] [Google Scholar]