Summary
Background. Burn trauma is a major public health concern, with increased risk for burns in children. Objectives. To characterize the profile of injured burn patients and to identify patients who are prone to burn injury. Methods. This is a cross-sectional study including all patients who were admitted to the Burns and Plastic Surgery Department, Soroka University Medical Center, Israel, between 1 January 2001 and 31 December 2002. Results. Five hundred and fifty-eight patients with a mean age of 15.4 yr (SD, 19.5 yr) were included in the study. There were 348 male patients (62.4%). The cause of the burns was scalding in 314 patients (56.3%), flame in 177 (31.7%), chemicals in 31 (5.6%), explosion in 20 (3.6%), and electricity in four (0.7%). There were 325 Bedouin patients (58.2%) and 221 Jewish patients (39.6%). In Bedouins, 235 patients (72.3%) were children below 5 yr, compared to 59 Jewish patients (26.7%) (p < 0.001). Eighteen burn patients (3.2%) expired. A multivariate analysis demonstrated that age and percentage of body surface area involved in the burn were significantly associated with mortality. Conclusions. The epidemiological characteristics of the burned population in Soroka University Medical Center are described. Burn injury has become a principal public health problem, particularly in Bedouin children.
Keywords: BURNS, SOROKA, UNIVERSITY, MEDICAL, CENTER, EXPERIENCE
Abstract
Données de base. Les traumatismes causés par les brûlures constituent un important problème de santé publique, avec des risques encore plus graves pour les enfants. Buts. Caractériser le profil des patients brûlés et identifier ceux qui sont exposés à ce type de risque. Méthodes. Cette étude transversale comprenait tous les patients hospitalisés dans le Département de Brûlures et Chirurgie Plastique du Centre Médical de l’Université de Soroka, Israël, entre 1/1/01 et 31/12/02. Résultats. L’étude intéressait 558 patients (âge moyen, 15,4 ans; déviation standard, 19,5 ans), dont 348 du sexe masculin (62.4%). La cause des brûlures était l’ébouillantement chez 314 patients (56,3%), les flammes chez 1717 (31,7%), les produits chimiques chez 31 (5,6%), les explosions chez 20 (3,6%) et l’électricité chez quatre (0,7%). Il y avait 325 patients bédouins (58,2%) et 221 patients juifs (39,6%). Chez les Bédouins, 235 patients (72,3%) étaient des enfants âgés de moins de 5 ans par comparaison avec 59 patients juifs (26.7%) (p < 0.001). Dix-huit patients brûlés (3,2%) sont décédés. Une analyse multivariée a démontré que l’âge et pourcentage de la surface corporelle brûlée étaient associés en manière significative avec la mortalité. Conclusions. Les Auteurs décrivent les caractéristiques épidémiologiques de la population brûlée au Centre Médical Universitaire de Soroka. Les brûlures sont devenues un problème prédominant de la santé publique, particulièrement chez les enfants bédouins.
Introduction
Burn injuries range from minor to severe events and present a major public health concern. Deep, extensive (severe) burns are often fatal, especially when the burns are associated with smoke inhalation or additional trauma. Treatment of burns that requires specialized personnel and medical technologies is expensive and consumes considerable medical resources. Burn patients may suffer long-term sequelae such as disfiguring, disabling scars and contractures. Affected patients often experience psychological complications. Children are in particularly prone to burns. Risk factors include low socioeconomic conditions, poor living conditions, illiteracy, overcrowding, and floor level cooking. 1, 2, 3, 4, 5
In the present study, we describe the burn-injured patient population in Israel’s southern region who were hospitalized during the years 2001-02 in the Burns and Plastic Surgery Department of Soroka University Medical Center, aiming to identify patient subsets that may be especially burn-prone.
Materials and method
The study included the complete medical files of all 558 burn-injured patients who were hospitalized during the years 2001-02 in the Burn Unit of the Plastic Surgery Department in Soroka University Medical Center, Beer-Sheva. After preparation of the study protocol and data-collecting forms, all files were reviewed and clinical parameters were extracted. Data concerning burn depth, extent, causes, complications, risk factors, and overall mortality were analysed retrospectively.
Statistical analysis was performed using SPSS software. Results of continuous variables are shown as means ± SD. Results of categorical variables are described as frequencies. Chi-square tests were used to analyse statistically significant differences of categorical variables. T-tests or one-way ANOVA were used to compare continuous parameters between groups. Logistic regression models were used for multivariate analyses. P values ≤ 0.05 were considered statistically significant.
Results
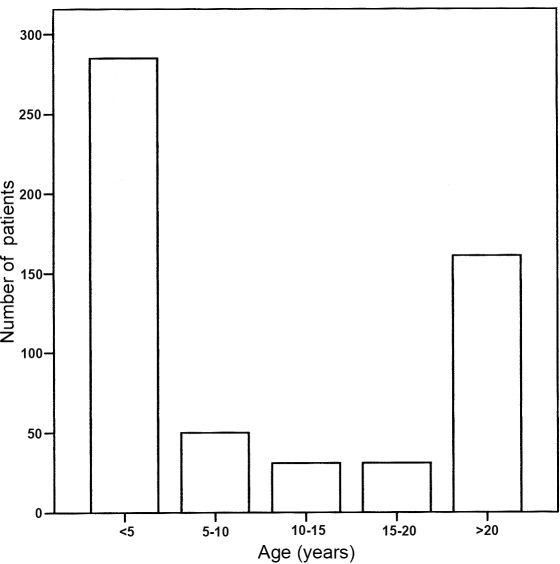
Five hundred and fifty-eight patients with a mean age of 15.4 yrears (SD, 19.5 yr) were included in the study. There were 348 male patients (62.4%). The detailed age distribution of the patients appears in Fig. 1 .
Fig. 1. Age distribution of 558 patients hospitalized for burns.
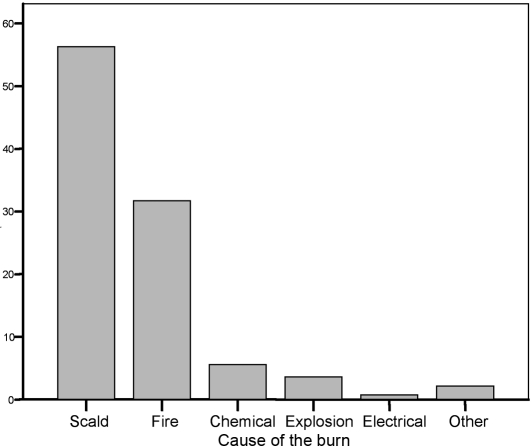
Four hundred and eighty-two patients (86.4%) had burns involving less than 20% of the body surface area (BSA), 53 patients (9.5%) had burns involving 20-40% BSA, 13 patients (2.3%) had burns involving 40-60% BSA, and 10 patients (1.8%) had burns involving more than 60% BSA. Thirteen patients (2.3%) had first-degree burns, 398 patients (71.3%) had superficial second-degree burns, 94 patients (16.8%) had deep second-degree burns, and 53 patients (9.5%) had third-degree full-thickness burns. Scalding was the commonest cause of burn injury, followed by flame. The causes are represented in Fig. 2 .
Fig. 2. Cause of the burns in 558 patients hospitalized for burns.
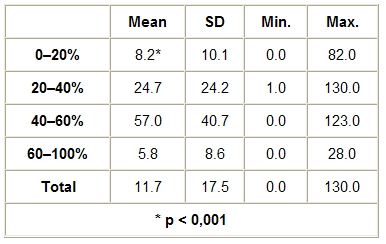
The patients were hospitalized for a mean period of 11.6 days; the length of hospitalization was significantly associated with the extent of the burns (p < 0.001) ( Table I ).
Table I. Days of hospitalization of burn-injured patients, stratified according to extent of burns.
There were 325 Bedouin patients (58.2%), 221 Jewish patients (39.6%), and 12 patients (2.2%) of other ethnic origins. In Bedouins, the majority of burns occurred in young children; in Jewish patients, the majority of burns occurred in adults. The age distribution stratified according to origin appears in Table II .
Table II. Age distribution of burn-injured patients, stratified according to origin.

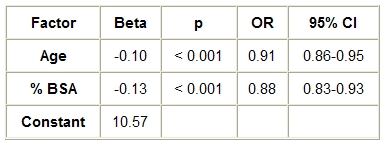
Thirty-four patients (6.1%) had smoke inhalation in addition to burns. Eighteen patients (3.2%) died: nine Jewish patients, six Bedouin patients, and three patients of other origin. The cause of death was septic shock in nine patients, multi-organ failure in five, extensive burns in three, and underlying diseases in one. A multivariate analysis demonstrated that age and extent (% BSA) of the burns were significantly associated with mortality ( Table III ).
Table III. Multivariate analysis for factors associated with mortality in burn-injured patients.
Discussion and conclusion
Burn injury is a considerable public health concern. Severe burns may be fatal and survivors frequently suffer from severe sequelae (i.e., disabling scars and psychological consequences). The care of burn patients is a complex team endeavour consuming substantial medical and human resources. Almost all children who sustain a severe burn injury will have some sequel of the accident persisting into adulthood.
Following previous epidemiological studies conducted in Israel, 6, 7, 8, 9, 10, 11, 12, 13a national prevention programme for burn- and house-related accidents was instituted in Israel 15 years ago. This programme has contributed to increased patient awareness of risks and to promote injury control. 12
In the present study of 558 burn-injured hospitalized patients, the overall mortality was 3.2%, which is within the range of similar studies described in the literature. 10, 11, 14 15 16 17 18 19 20 21 22
The mortality rate described in the literature may reflect the level of clinical care, burn severity, and possibly some population characteristics that influence their general health condition. A multivariate analysis demonstrated that mortality predicting factors are the age of the patients and the percentage of body surface area involved. The increased mortality rate in Jewish patients observed in the current study is attributed to the older age mix of the Jewish population than that of the younger Bedouin population.
The length of hospitalization was significantly associated with the extent of the burns, reflecting the high cost of care of burn injuries. It should be noted that in burns affecting > 60% BSA, hospitalization length was shorter, probably owing to the higher mortality rate.
The development of the burn centre in the Soroka University Medical Center has proved to be of considerable benefit to the patients. A distinct advantage is the availability of multidisciplinary team care. Psychiatrists, dieticians, social workers, neurologists, paediatricians, anaesthetists, neurosurgeons, ophthalmologists, physicians, physiotherapists, and occupational therapists are available under one roof. In addition, our skin bank provides bilayered skin substitutes and keratinocyte cultures for the treatment of burn patients.
A most important observation in this study is the fact that the majority of the burns occurred in young Bedouin children (72.3% of the Bedouin patients were less than five years old), whereas in Jewish patients the majority of burns occurred in adults. The Bedouin population in the Negev comprises about 130,000 people. The Bedouins are an ethnic, religious, and cultural minority with various social and economic problems. The religion of the Bedouins is Islam, the spoken language is usually Arabic, and the men are more frequently able to speak Hebrew. Approximately half of the population lives in urban settlements and the other half lives in rural settlements. Unemployment rates are high and many families live on social security income. The Bedouins are a population in transition from a nomadic to a more settled and urban form of life. The transition from a traditional to a western lifestyle, characterized by changes in dietary habits and a reduction in physical activity, is associated with considerable changes in morbidity patterns, such as a considerable increase in diabetes prevalence 23and a high rate of home-related injuries. 24The medical services offered by the health authorities are not fully used, owing to geographical scattering and distance, as well as language, cultural, and economic difficulties.
Burn hazards are present daily in Bedouin life, but epidemiological studies on childhood injuries in the Bedouin population in Israel are limited11 and the exact magnitude and causes of burn injuries have not been well documented. In this study, there were 325 burns in Bedouins, in a population base of 130,000 (0.25%), as compared to 221 burns in Jewish patients, in a population base of 415,000 (0.05%). As our study was conducted retrospectively, we cannot estimate exact incidence rates. However, a crude estimate shows that burns appear five times more frequently in the Bedouin population than in the Jewish population.
In this study, scalding, a typical home-related accident, was the most frequent cause of burn injuries (56.3%), as observed elsewhere. 10, 11, 14 15 17 18 19 20 21 22Cooking in hot water and a lifestyle that is based on sitting and placing cooked foods on the floor are widespread in Bedouin culture. Accidental scald burns in small children who come into contact with hot foods and liquids are common, reflecting overcrowding with young children playing on the floor in the vicinity of the cooking area and cooked foods. The second most common cause of burns in this study was flame (31.7%), which indicates the continued use of open fire in daily life in the Bedouin population.
Since scalding and fire are the prevalent causes of burns among Bedouin children, preventive steps should be taken to prevent these specific causes of injury. Focused preventive interventions and education measures for the control of paediatric burns and injury in the Bedouin population are currently performed by Clalit Health Services and by the “Play it safe” prevention programme initiated in the Department of Plastic Surgery and Burn Unit in Soroka. 12We recommend that sufficient resources should be allocated to burn injury control in the Bedouin population.
References
- 1.Meuli M., Lochbuhler H. Current concepts in pediatric burn care: General management of severe burns. Eur. J. Pediatr. Surg. 1992;2:195–200. doi: 10.1055/s-2008-1063439. [DOI] [PubMed] [Google Scholar]
- 2.Stuart J.D., Kenney J.G., Morgan R.F. Pediatric burns. Am. Fam. Physician. 1987;36:139–46. [PubMed] [Google Scholar]
- 3.Zeitlin R. Late outcome of paediatric burns - scarred for life. Ann. Chir. Gynaecol. 1998;87:80. [PubMed] [Google Scholar]
- 4.Zeitlin R.E., Jarnberg J., Somppi E.J., Sundell B. Long-term functional sequelae after paediatric burns. Burns. 1998;24:3–6. doi: 10.1016/s0305-4179(97)00052-1. [DOI] [PubMed] [Google Scholar]
- 5.Zeitlin R.E. Long-term psychosocial sequelae of paediatric burns. Burns. 1997;23:467–72. doi: 10.1016/s0305-4179(97)00045-4. [DOI] [PubMed] [Google Scholar]
- 6.Eldad A., Israeli A. The treatment of burns in Israel. Harefuah. 1999;116:583–5. [PubMed] [Google Scholar]
- 7.Eldad A. Burns in children in Israel - epidemiology, prevention, and treatment. Harefuah. 1999;137:177–9. [PubMed] [Google Scholar]
- 8.Gofin R., Palti H., Adler B., Edet E. Childhood injuries: A population-based study of emergency room visits in Jerusalem. Paediatr. Perinat. Epidemiol. 1989;3:174–88. doi: 10.1111/j.1365-3016.1989.tb00511.x. [DOI] [PubMed] [Google Scholar]
- 9.Gofin R., Israeli I., Palti H. The incidence of childhood and adolescent injuries and their outcome: A population-based study. Isr. J. Med. Sci. 1991;27:566–71. [PubMed] [Google Scholar]
- 10.Milo Y., Robinpour M., Glicksman A., Tamir G., Burvin R., Hauben D.J. Epidemiology of burns in the Tel Aviv area. Burns. 1993;19:352–7. doi: 10.1016/0305-4179(93)90127-t. [DOI] [PubMed] [Google Scholar]
- 11.Morad M., Hemmo-Lotem M., Kandel I., Hyam E., Merrick J. Burn injuries and adolescents in Israel. Int. J. Adolesc. Med. Health. 2004;16:201–5. doi: 10.1515/ijamh.2004.16.3.201. [DOI] [PubMed] [Google Scholar]
- 12.Shani E., Rosenberg L. Are we making an impact? A review of a burn prevention program in Israeli schools. J. Burn Care Rehabil. 1998;19:82–6. doi: 10.1097/00004630-199801000-00018. [DOI] [PubMed] [Google Scholar]
- 13.Silfen R., Chemo-Lotan M., Amir A., Hauben D.J. Profile of the pediatric burn patient at the Schneider Children’s Medical Center of Israel. Isr. Med. Assoc. J. 2000;2:138–41. [PubMed] [Google Scholar]
- 14.Cronin K.J., Butler P.E., McHugh M., Edwards G. A one-year prospective study of burns in an Irish paediatric burns unit. Burns. 1996;22:221–4. doi: 10.1016/0305-4179(95)00109-3. [DOI] [PubMed] [Google Scholar]
- 15.Davies J.W. The problems of burns in India. Burns. 1990;(1):S1–24. [PubMed] [Google Scholar]
- 16.Forjuoh S.N., Guyer B., Ireys H.T. Burn-related physical impairments and disabilities in Ghanaian children: Prevalence and risk factors. Am. J. Public Health. 1996;86:81–3. doi: 10.2105/ajph.86.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forjuoh S.N., Keyl P.M., Diener-West M., Smith G.S., Guyer B. Prevalence and age-specific incidence of burns in Ghanaian children. J. Trop. Pediatr. 1995;41:273–7. doi: 10.1093/tropej/41.5.273. [DOI] [PubMed] [Google Scholar]
- 18.Forjuoh S.N., Guyer B., Strobino D.M., Keyl P.M., Diener-West M., Smith G.S. Risk factors for childhood burns: A case-control study of Ghanaian children. J. Epidemiol. Community Health. 1995;49:189–93. doi: 10.1136/jech.49.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Forjuoh S.N., Guyer B., Smith G.S. Childhood burns in Ghana: Epidemiological characteristics and home-based treatment. Burns. 1995;21:24–8. doi: 10.1016/0305-4179(95)90776-v. [DOI] [PubMed] [Google Scholar]
- 20.Kumar P., Chirayil P.T., Chittoria R. Ten years’ epidemiological study of paediatric burns in Manipal, India. Burns. 2000;26:261–4. doi: 10.1016/s0305-4179(99)00109-6. [DOI] [PubMed] [Google Scholar]
- 21.Passaretti D., Billmire D.A. Management of pediatric burns. J. Craniofac. Surg. 2003;14:713–8. doi: 10.1097/00001665-200309000-00021. [DOI] [PubMed] [Google Scholar]
- 22.van Rijn O.J., Grol M.E., Bouter L.M., Mulder S., Kester A.D. Incidence of medically treated burns in The Netherlands. Burns. 1991;17:357–62. doi: 10.1016/s0305-4179(05)80067-1. [DOI] [PubMed] [Google Scholar]
- 23.Cohen A.D., Gefen K., Ozer A., Bagola N., Milrad V., Cohen L., et al. Diabetes control in the Bedouin population in Southern Israel. Med. Sci. Monit. 2005;11:CR376–80. [PubMed] [Google Scholar]
- 24.Broides A., Assaf M. Home accidents in Arab Bedouin children in Southern Israel. J. Child Health Care. 2003;7:207–14. doi: 10.1177/13674935030073006. [DOI] [PubMed] [Google Scholar]