Summary
Perineal or genital burns are mostly part of large body surface injuries, and isolated burns to the genitalia are not common. Nevertheless, they are of major concern to the patient and clinician. Highly concentrated solutions of sulphuric acid are available to unclog drains. We have noted a substantial number of both accidental and intentional cutaneous burns caused by these agents and we therefore conducted a study on the incidence and treatment of isolated chemical burns in the genitalia. The study was performed in the Burns Unit, King Saud Hospital, Al-Qassim, Kingdom Saudi Arabia, from April 2001 to December 2004. During this period we received 12 patients with isolated chemical burns in the genitalia, representing 3.4% of all cases of burns treated between 2001 and 2004 (350 patients with different causes and variable percentages of burns). Of these 12 patients, 11 were males and one female. The patients' ages ranged from 9 to 75 yr. The mean burn size was 2% of the total body surface area. The cause of the burn injury was sulphuric acid, which is famous in this area for water closet cleaning. Eight patients (66.7%) required skin grafting, one healed with minimal scarring, and three (25%) healed with minimal contractures treated with multiple Z-plasty. We concluded that conservative management of perineal and genital chemical burns was recommended until the demarcation zone became clear. Split-thickness skin grafts were durable, safe, and technically easy, with satisfactory cosmetic and functional results.
Keywords: isolated, chemical, burns, genitalia
Abstract
Généralement, les brûlures périnéales et génitales sont associées à des lésions qui touchent d'autres surfaces corporelles plus étendues: les brûlures isolées des organes génitaux sont rares. Elles constituent néanmoins un important problème pour le médecin et le clinicien car il n'est pas difficile d'obtenir des solutions d'acide sulfurique à haute concentration pour débloquer les canalisations sanitaires. Les Auteurs ont noté un nombre considérable de brûlures accidentelles et intentionnelles causées par ces agents et ils ont effectué une étude sur la fréquence et le traitement des cas de brûlures chimiques isolées des organes génitaux. L'étude a été réalisée chez l'Unité des Brûlures, Hôpital Roi Saud, Al-Qassim, Royaume d'Arabie Saoudite, pendant la période avril 2001/décembre 2004. Les Auteurs, pendant cette période, ont traité 12 patients atteints de brûlures chimiques isolées des organes génitaux, ce qui constituait 3,4% de tous les cas de brûlures qu'ils ont traités entre 2001 et 2004 (350 patients atteints de brûlures ayant des causes diverses et des pourcentages variables). Tous les 12 patients, avec une seule exception, étaient du sexe masculin. L'âge des patients variait entre 9 et 75 ans. L'extension moyenne des brûlures était 2% de la surface totale corporelle. La cause des brûlures était l'acide sulfurique, qui est communément utilisé dans ce pays pour nettoyer les waters. Huit patients (66,7%) nécessitaient des greffes cutanées, un a guéri avec des cicatrices minimales, et trois (25%) ont guéri avec des contractures minimales traitées moyennant des Z-plasties multiples. Les Auteurs concluent que la gestion conservatrice des brûlures chimiques périnéales et génitales est recommandée jusqu'à la nette définition de la zone de démarcation. Les greffes cutanées à épaisseur variable se sont démontrées durables, sûres et techniquement faciles, avec des résultats cosmétiques et fonctionnels satisfaisants.
Introduction
Compared with other natural disasters, burns exert a catastrophic influence on people in terms of human life, suffering, disability, and financial loss. People of all ages are susceptible to minor burn injury. Chemical burns account for relatively few admissions to a burns unit. These injuries, however, deserve separate consideration owing to their ability to cause continuing tissue destruction, to their potential for systemic toxicity, and to the value of early treatment with copious lavage. 1Although chemical burns account for only 3% of all burns, they cause more than 30% of burn deaths. Most chemical burns are work-related, and occur because of accidental contact with a chemical agent. Chemical burns usually occur in exposed areas of the body such as the hands and face. 1, 2, 3A genital perineal acid burn caused by a chemical agent is very rare. Such injuries may lead to fatal results but they may also heal and leave serious sequelae. 4, 5, 6All burn wounds, whether chemical or thermal, result in the denaturation of proteins. 2Sulphuric acid and its precursor, sulphur trioxide, are strong acids and desiccants with many industrial applications. It is a very oily liquid and can cause coagulation necrosis.Mixing with water leads to heat production. 3Sulphuric acid is highly corrosive to all parts of the body.
Widespread inexperience in the treatment of chemical burns highlights the potential for greater levels of general awareness and knowledge. 4
The prompt recognition and management of chemical burns in general and specifically of the genitalia can prevent injury to the deep structures of the penis and scrotum, making the difference between satisfactory rehabilitation and crippling deformities. Immediate irrigation with water is the single most important treatment that can be carried out, and should be continued for at least an hour and even for several hours, depending on the severity of the injury. Precious time should not be wasted hunting for a specific neutralizing agent. 5The majority of cases present deep full-thickness burn involving less than 10% of the total body surface area (TBSA). Chemical burns may be accidental or due to criminal assault. Strong acids, mainly sulphuric acid, nitric acid, and hydrochloric acid, and alkalis, mainly lime and sodium hydroxide, are common causative agents.
The management of the injuries consists of either surgical or conservative treatment. The former includes debridement and split-thickness skin grafting or primary closure, and the latter topical treatment with 1% silver sulphadiazine cream and appropriate dressings.
The purpose of this article is to report our experience with the uncommon site of chemical burns to the genitalia, of which we cannot find a similar number of cases in the literature, and to present our management guidelines for such burns, which include excision and skin grafting. The cosmetic and functional results are also presented.
Materials and methods
Twelve patients were identified as having isolated burns due to sulphuric acid in the genitalia during the study period from 2001 to 2004 for a total of 350 patients presenting different causes and variable percentages of burns
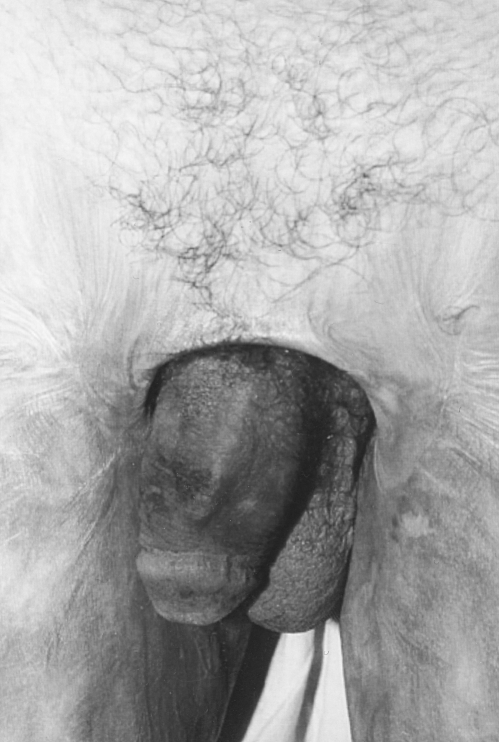
admitted to the Burns Unit in the King Saud Hospital, Al Qassim, Kingdom of Saudi Arabia. There were 11 males and one female. The ages of the patients ranged from 9 to 75 yr. The median burn size was 2% TBSA (range, 0.5 4%). The cause of the burn injury was sulphuric acid, which is famous in this area for water closet cleaning, and is applied accidentally during washing of the genital organs as an initial step of making Wodoa before praying in Islam. Most commonly the upper thighs and left hand were involved, together with the external genitalia ( Fig 1 ).
Fig 1. Patient with accidental chemical burn to the penis, scrotum, and medial aspect of left thigh. There are demarcated necrotic areas in the burn region.
The burns were third-degree in eight patients (66.7%) and deep second-degree in four (33.3%). All patients required an indwelling silicone catheter placed immediately after the injury as part of resuscitation, which remained indwelling for 7 to 22 days (mean, 11 days) without complications. Genital and perineal burns were treated with physiological dressings and topical antimicrobials. The five burn patients who presented immediately were managed in an as aseptic an environment as possible to prevent infection. They were washed with water and chlorhexidine three times a day. Silver sulphadiazine cream was used as a topical antimicrobial, and occlusive dressing was applied over the agent in male patients. Healing with minimal scarring after 17 days was seen in the one female patient, whose injury was diagnosed as a mixed second-degree burn because the acid concentration was low and the patient used water to relieve pain immediately after the accident.
In three other patients, healing was completed after 25 days with minimal contractures, subsequently released with multiple Z-plasties. Out of eight patients requiring a surgical procedure, seven were referred to us two weeks postburn when the burn site was covered with black eschar with a clear demarcation zone (Figs. 2 a , b ). In these patients culture swabs were taken from the burn site and tangential excision of the adherent eschar was performed down to a healthy bleeding surface, which was covered immediately with non-meshed thick split-thickness skin graft to the penis and meshed skin graft to the scrotum. In all grafted cases the grafts were wrapped around the penile shaft, making the suture line in the under surface of the penis. Another meshed skin graft was applied over the scrotal fasciae (mostly cremasteric fasciae) in seven cases or directly over the testes and cords in one patient.
Fig 2 a. Healed chemical burn to penis with minor contractures.
Fig 2 b. After release of contractures with multiple Z-plasties.
In another patient who came directly to our hospital, tangential excision and an immediate thick split-thickness skin graft from the thigh were performed before reconstruction of the defect seven days post-burn.
Compressive dressings with immobilization of the area were an important step, using a plastic water cup and a scrotal sling.
An antibiotic was given according to results of culture swabs taken before the operation, and the first dressing was mostly done on the fifth post-operative day. Patients were discharged after their first dressing and followed up in the plastic surgery out-patients department for dressing and stitch removal.
Results
Twelve patients were identified as having isolated chemical burns, mainly in the perineal and genital area due to sulphuric acid during the study period (2001 to 2004) among 350 patients admitted with different causes and variable percentages of burns to the Burns Unit, King Saud Hospital, Al-Qassem, Kingdom of Saudi Arabia. There were 11 males and one female. The ages of the patients ranged from 9 to 75 yr (mean age, 42 yr). The median burn size was 2% TBSA (range, 0.5-4%). The cause of
the burn injuries was sulphuric acid, which is famous in this area for water closet cleaning - it is applied accidentally during washing of the genital organs as an initial step of making Wodoa before praying in Islam. The upper thighs were involved most commonly, together with the external genitalia ( Fig 1 ). The burns were third-degree in eight patients (66.7%) and deep second-degree in four (33.3%). All patients required an indwelling silicone catheter placed immediately after the injury as part of resuscitation, which remained indwelling for 7 to 22 days without complications. Healing with minimal scarring after 17 days was seen in one female patient who sustained mixed seconddegrees burn as the acid concentration was low and she used water to relieve pain immediately after the accident. In three other patients, healing was completed after 25 days with minimal contractures that were subsequently released with multiple Z-plasties (Figs. 2 a , b , 3 a , b ). Eight patients required a surgical procedure involving tangential excision, and an immediate thick split-thickness skin graft from the thigh was used to reconstruct the defect (Figs. 4 , 5 ).
Fig 3 a. Child with contracture of prepuce to the thigh one year after chemical burn.
Fig 3 b. After circumcision and release of contractures.
Fig 4. Same patient as in Fig. 1 five months after skin grafting of penis and scrotum with good cosmetic results.
Fig 5. Lateral view of same case.
Post-operative follow-up ran smoothly with adequate healing. The cosmetic results were good, and functionally the patients and their partners were satisfied concerning erection and sensation (they were advised to start the act after six months but erection was allowed 10 days post-operatively to give the chance for graft expansion and to prevent contracture). There was no urethral stenosis or penile contracture and the patients continued their normal daily life; one patient even got married six months postgrafting with a good durable graft not affected by repeated intercourse.
Discussion
Perineal or genital burns are usually part of large total body surface injuries, and death is usually the result of the extent of the injury and not of the perineal or genital burn per se. The literature on this topic is scarce. 1 2Mc Dougal et al. 1reported a series of 197 military patients with perineal burns from 1971 to 1976, which represented 13% of hospital admissions for burns. Peck et al. 2treated 103 civilians with genital and perineal burns in five years, which represented 5% of all hospital admissions for burns. Our hospital admission rate of isolated chemical burns in the genitalia was 3.4%, with an average injury size of 2% and no mortality, which is comparable to the results of Peck et al. 3and to those of the military study, indicating the severity of such injuries in the latter group.
Flame and scald burns account for the majority of injuries in most of the literature. 7Isolated chemical burns in the genitalia are rare. Hosokawa et al. 7presented a 27-yrold man who was attacked at his place of work. He received chemical burns to the penis induced by hydrochloric acid and developed severe phimosis. He complained of pain on erection and ballooning during urination. The foreskin was partially resected with foreskin grafting for the stricture. The post-operative outcome was favourable and his symptoms were relieved. Demir et al. 5presented an interesting case of chemical burn injury of the genital perianal region caused by accidental hydrochloric acid exposure during washing of the genitalia. Conservative treatment was initiated for one week, and after the demarcation zone had become defined they excised the devitalized tissues and applied a split-thickness skin graft, achieving a satisfactory outcome without complications. Ricketts and Kimble 8managed 31 patients presenting chemical injuries - the upper and lower extremities were involved in all cases and the perineum also in four patients, the mean TBSA affected being 3.4%. Their management included debridement and split-thickness skin grafting or primary closure and conservative treatment in the form of topical treatment with 1% silver sulphadiazine cream and appropriate dressings. Bond et al. 9conducted a retrospective review of patients who sustained sulphuric acid burns over a 13-yr period: 21 patients (13 children, 8 adults) sustained cutaneous burns caused by concentrated sulphuric acid solutions.In eight instances, the burn was accidental, while in the other 13 cases sulphuric acid was used as a weapon.The median TBSA burned was 5% (range, 1-25%). Approximately 50% of the burns involved the face and neck.Skin grafting was required in 14 patients (66%). It is estimated that nationwide approximately 3,000 injuries per year are related to drain cleaners and that one-third of these involve cutaneous burns.
In our study chemical burns with concentrated sulphuric acid solutions were the main cause of isolated genital and perineal burns, owing to the frequent occurrence of this type of injury in rural Bedouin areas where they use water bottles to wash the genitalia as an important step in making Wodoa before praying in Islam, by mistake using acid which is available in bottles and employed for WC cleaning. Burn depth is one of the most important factors in management but it may be difficult to determine.Traditionally, chemical burns are classified as third-degree burns with involvement of the epidermis, dermis, fat, and underlying tissue. The affected part may be brown, dark red, or black in colour. The diagnostic signs of full-thickness burns are lack of sensation in the burned skin, lack of capillary refilling, and a leathery texture that is unlike that of normal skin. Sometimes, when the acid is diluted with rapid copious irrigation with water, the resulting burn will be more superficial. Pitkanen and Al-Qattan,10 reviewing the domestic chemical injury experience in two major government hospitals in Saudi Arabia, found that alkali drain cleaners were the major cause of chemical burns in the series, seen in 75% of the total study population.The remaining 25% of cases resulted from concentrated sulphuric acid. Skin grafting was required in most of their patients.
Treatment of genital or perineal burns is primarily conservative, which is the preferred method for chemical burns in the genital area. 1 5 8 9After the daily dressing change, if the demarcation zone of the necrotic areas has become defined, necrotic areas are debrided and skin defects are grafted. 3 5 8 9 10 11
Topical antimicrobials, sulphadiazine silver with cerium nitrate, and physiological dressings resulted in excellent healing in 87 cases in the series reported by Michielsen et al. 2Another four children had excellent healing after the use of allografts enhanced epithelialization. Indeed, longterm results showed that hypertrophic scar formation in superficial and deep dermal burns was reduced when allografts were used (same series). Radical debridement should be avoided, since apparently nonviable structures often recover, and skin grafts are recommended in cases of delayed healing.
In our series, surgical intervention was required after the demarcation zone became clear. One patient came direct to our unit 7-10 days post-burn; in the other seven patients, as they presented with a clear demarcation zone, we performed tangential excision of the adherent eschar down to a healthy bleeding surface, which was covered immediately with nonmeshed thick split-thickness skin graft to the penis and meshed skin graft to the scrotum. In four patients with conservative management, delayed healing resulted in minor contractures of the external genitalia, which occurred in three patients. The scars were left alone to mature. Reconstruction with multiple Z-plasties was performed for contracture of the penile shaft, and scar formation of the prepuce was treated successfully with circumcision.
Chemical burns in the genitalia represented 3.4% of all cases of burns admitted to our unit. Even though the series was small, certain aspects of our chemical burns require emphasis. All our cases reflected negligence by cleaners, the victims' ignorance, and the poor experience of physicians in rural areas. The focus of our education efforts should be directed toward the public, emphasizing the safe use of household chemicals. In order to reduce morbidity following chemical burns, we re-emphasize the importance of early continuous water irrigation of burn wounds. As regards preventive measures, we suggest the imposition of legal restrictions on the sale of potentially injurious chemicals, as well as measures to prevent the sale of such chemicals without warning labels in special colours to arouse the attention of persons of limited education.
References
- 1.McDougal W.S., Peterson H.D., Pruitt B.A., Persky L. The thermally injured perineum. J. Urol. 1979;121:320. doi: 10.1016/s0022-5347(17)56770-1. [DOI] [PubMed] [Google Scholar]
- 2.Michielsen D., Van Hee R., Neetens C., Lafaire C., Peeters R. Burns to the genitalia and the perineum. J. Urol. 1998;159:418–9. doi: 10.1016/s0022-5347(01)63937-5. [DOI] [PubMed] [Google Scholar]
- 3.Peck M.D., Boileau M.A., Grube B.J., Heimbach D.M. The management of burns to the perineum and genitals. J. Burn Care Rehab. 1990;11:54. doi: 10.1097/00004630-199001000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Penner G.E. Acid ingestion: Toxicology and treatment. Ann. Emerg. Med. 1980;97:374–9. doi: 10.1016/s0196-0644(80)80116-8. [DOI] [PubMed] [Google Scholar]
- 5.Demir Z., Eroclu A., Çelebiocluan S. Interesting case of chemical burn injury of the genital perianal region caused by hydrochloric acid exposure. Burns. 2003;29:175–7. doi: 10.1016/s0305-4179(02)00241-3. [DOI] [PubMed] [Google Scholar]
- 6.Givens M.L., Rivera W. Genital burns from home use of podophyllin. Burns. 2005;31 3:394–5. doi: 10.1016/j.burns.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 7.Hosokawa Y., Kishino T., Ono T., Oyama N., Joko M., Momose H. A case of acid burn of the penis. Hinyokika Kiyo. 2002;48:615–6. [PubMed] [Google Scholar]
- 8.Ricketts S., Kimble F.W. Chemical injuries: The Tasmanian Burns Unit experience. ANZ J. Surg. 2003;73:45–8. doi: 10.1046/j.1445-2197.2003.02617.x. [DOI] [PubMed] [Google Scholar]
- 9.Bond S.J., Schnier G.C., Sundine M.J., Maniscalco S.P., Groff D.B. Cutaneous burns caused by sulphuric acid drain cleaner. J. Trauma. 1998;44:523–6. doi: 10.1097/00005373-199803000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Pitkanen J., Al-Qattan M.M. Epidemiology of domestic chemical burns in Saudi Arabia. Burns. 2001;27:376–8. doi: 10.1016/s0305-4179(00)00126-1. [DOI] [PubMed] [Google Scholar]
- 11.Alghanem A.A, McCautey R.L., Robson M.C., Rutan R.L., Herndon D.N. Management of paediatric perineal and genital burns: Twenty years' review. J. Burn Care Rehabil. 1990;11:308–11. doi: 10.1097/00004630-199007000-00007. [DOI] [PubMed] [Google Scholar]