Summary
The aim of this trial was to measure the pH value of the skin of burn patients using a non-invasive method, from the acute phase through to complete re-epithelialization. The research was then completed by treating the patients with new materials and innovative methods to verify whether this had an effect on the skin pH and on re-epithelialization time. In this clinical trial, the patients were medicated repeatedly with hydrogel (Burnshield®) kept in place by a transparent, semipermeable adhesive film with a moisture vapour transmission rate equivalent to 1600 until day 5 or 6 post-burn. In one patient, treated silk (DermaSilk®) was applied several times until re-epithelialization; in another patient, synthetic hyaluronic acid (Hyalomatrix®) was applied. Various studies using Dermasilk® have confirmed that the fibroin in silk stimulates re-epithelialization, in addition to keeping the burned skin disinfected, thanks to the antimicrobial agent contained in the treated silk. Hyalomatrix® was used on the other patient, as in other studies, as a temporary substitute for the skin in deep burns. Late complications (keloids and hypertrophic scars) can give rise, even after prolonged periods of time, to Marjolin's ulcer (carcinoma but also melanoma and sarcoma), which can develop in the course of a year. A recent Danish trial affirms that appropriate burn treatment facilitates re-epithelialization and decreases the incidence of Marjolin's ulcer. For the trial, we used a centimetre-wide strip of reactive paper sensitive to pH variations and an acid test (Duotest® kit) as a reference, applied for more than one minute on the patient's burned and slightly damp skin. We performed control procedures on the patient's normal skin, away from the wound site. The pH was measured from day 1 post-burn and every other day thereafter until complete re-epithelialization. We found alkaline pH values for the burned skin from the day of the burn until day 12, with an alkaline pH peak on day 4 (10.5 in the first patient, 9.5 in the second). The values then gradually returned to normal (pH, 5.5) from day 13 onwards. The mean re-epithelialization time was similar in the two patients, equivalent to 24.5 days (25 days in the first patient, 24 in the second), with a mean follow-up of 21 months (33 months in the first case, 9 in the second). No early or late complications were observed.
Keywords: SKIN, VARIATIONS, RE-EPITHELIALIZATION, PATIENTS, MATERIALS, SEMIPERMEABLE, ADHESIVE, NON-INVASIVE, EXPERIMENTAL, CLINICAL
Abstract
L'Auteur de cette étude s'est proposé de mesurer la valeur du pH de la peau des patients brûlés moyennant l'emploi d'une méthode non invasive, depuis la phase aiguë jusqu'à la réépithélialisation complète. L'étude a été complétée en traitant les patients avec des matériaux nouveaux et des méthodes innovatives pour vérifier si cela exerçait un effet sur le pH de la peau et sur les temps de la réépithélialisation. Dans cette épreuve clinique les patients ont été traités à maintes reprises avec l'hydrogel (Burnshield®), maintenu en place avec une pellicule transparente, semiperméable adhésive qui avait un taux de transmission de la vapeur d'eau équivalente à 1600, jusqu'au cinquième ou sixième jour après la brûlure. Chez un patient, de la soie traitée (DermaSilk®) a été appliquée diverses fois jusqu'à la réépithélialisation; chez un autre patient, l'acide hyaluronique synthétique (Hyalomatrix®) a été appliqué. Plusieurs études qui ont considéré le DermaSilk® ont confirmé que la fibroïne dans la soie stimule la réépithélialisation et maintient la désinfection de la peau brûlée, grâce à l'agent antimicrobien contenu dans la soie traitée. L'Hyalomatrix® a été employé chez l'autre patient, comme dans d'autres études, comme substitut temporaire de la peau atteinte de brûlures profondes. Les complications tardives (chéloïdes et cicatrices hypertrophiques) peuvent provoquer, même après de longues périodes de temps, l'ulcère de Marjolin (carcinome, mais aussi mélanome et sarcome), qui peut se manifester au cours d'un an. Un essai récent danois a trouvé que le traitement approprié des brûlures facilite la réépithélialisation et réduit la fréquence de l'ulcère de Marjolin. Dans cette étude nous avons utilisé une bande de carte réactive, large un centimètre, sensible aux variations du pH, et un test d'acide (Duotest® kit) comme référence, appliquée pour plus d'une minute sur la peau brûlée et légèrement humide du patient. Nous avons effectué les procédures de contrôle sur la peau normale du patient à une certaine distance de la lésion. Le pH a été mesuré le premier jour après la brûlure et puis tous les deux jours jusqu'à la réépithélialisation complète. Nous avons trouvé des valeurs alcalines du pH dans la peau brûlée depuis le jour de la brûlure jusqu'au douzième jour, avec une valeur maximum du pH alcalin au quatrième jour (10,5 chez le premier patient, 9,5 chez le deuxième). Ensuite les valeurs sont retournées aux niveaux normaux (pH, 5,5) du 13ème jour en avant. Le temps moyen de la réépithélialisation était similaire chez les deux patients, équivalent à 24,5 jours (25 jours pour le premier patient et 24 pour le deuxième), avec un suivi moyen di 21 mois (33 mois dans le premier cas, 9 dans le deuxième). Aucune complication précoce ou tardive n'a été observée.
Introduction
Under normal conditions, the skin has a mean pH of 5.5, kept constant by the skin's pH regulating barrier function. Variations tending towards higher or lower values are rapidly brought into line with the base value. This barrier function is efficacious at the age intervals between early infancy (6 months to 1 year) and advancing age (65-70 years). Prior to this interval and subsequent to it, the barrier function does not work rapidly: in newborn infants it is not yet mature and in the elderly it is related to the degree of skin atrophy in course.
A pH of 5.5 enables individuals to protect themselves from the multiplication of the germs harboured by humans - the majority of pathogenic and saprophytic bacteria survive at a pH that varies between 7.2 and 7.6. The skin's barrier function consists of cholesterol, ceramids, and free fatty acids. 2It is common knowledge that first- and second-degree skin burns re-epithelialize in the course of 14 days without leaving scars, while deep second- and third-degree burns take 30 days to re-epithelialize, often leaving hypertrophic scars and keloids.
There are no clinical trials currently available in the literature describing non-invasive methods for measuring the pH of burned skin from the acute phase to complete re-epithelialization. We thus studied new materials (DermaSilk®, semipermeable adhesive film, Hyalomatrix®, Burnshield® hydrogel) and innovative methods (medications without cotton gauze, with active ingredients and semipermeable adhesive film ([SAF]) with a view to treating skin burn patients better and more efficaciously. 4, 5, 6, 7Patients with deep second- and third-degree burns affecting a limited percentage of the body surface (TBSA < 10-12% in adults, < 7-8% in children) first underwent cooling treatment in the Casualty Unit (cooling for 15 min with physiological solution at 23 °C), after which hydrogel was applied (Burnshield®), kept in place by SAF. Subsequent to this, DermaSilk® was applied to one patient and synthetic hyaluronic acid (Hyalomatrix®) to the other, until complete re-epithelialization.
Materials and methods
The clinical trial was conducted from 26 March to 19 April 2004 (patient 1) and from 14 March to 10 April 2006 (patient 2) at the Casualty Unit of the Emergency Department of San Donà di Piave, Venice. The study involved two patients with deep second-degree burns in the lower limbs - the left leg and foot in the first patient, the left leg in the second patient - affecting approximately 4% TBSA in both cases. The patients, both male, aged respectively 61 and 42 yr, had both been burned by steam during their working activities. The time period between the injury and first-aid treatment was 15 min. The patients immediately had their skin pH measured at the site of the injury (8.5 in patient 1, 8 in patient 2) and again immediately after cooling for 15 min with physiological solution at 23 °C. Surgical toilette of the necrotic skin edges was then performed, after which hydrogel was applied by transparent, semipermeable adhesive film.
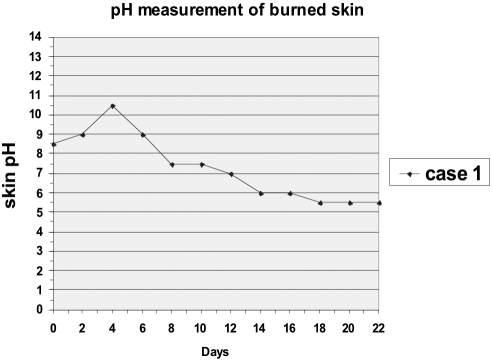
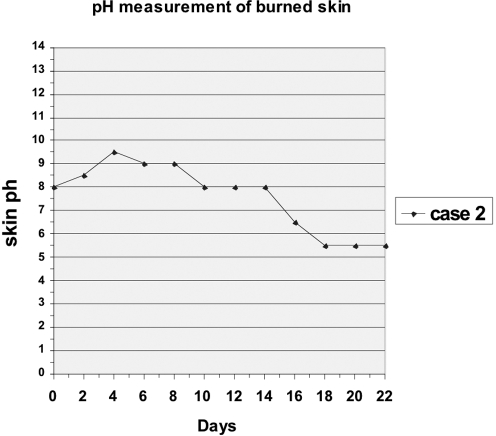
The permeability of a semipermeable film to water vapour when in contact with liquids is measured in grams per square metre over a 24-h period at 37 °C and is defined in terms of the quantity of water vapour that can pass through the film within a given unit of time (moisture vapour transmission rate [MVTR]). In this trial, we used a transparent, semipermeable film with an MVTR equivalent to 1600 g/m2 in the 24-h period at 37 °C. Patient 1 was medicated with hydrogel three times (for a total of 5 days), after which Hyalomatrix was applied once (for a total of 10 days). Patient 2 was medicated with hydrogel four times (for a total of 8 days), after which DermaSilk was applied nine times (for a total of 19 days) until re-epithelialization took place. The pH change curves relative to the days from the beginning of the treatment until re-epithelialization in patients 1 and 2 are shown in Figs. 1 and 2 respectively. For the measuring of skin pH we used a kit (Duotest®, manufactured by Macherey-Nagel) containing a strip of reactive paper sensitive to pH variations in a slightly damp environment, together with litmus paper. This method is used in the chemical textile industry to stimulate a chemical reaction in the reagents contained in pH sensitive paper in a slightly damp environment. The application of the sensitive strip lasted for more than 1 min on the burned skin and for the same length of time for control purposes on the healthy skin of the same patient. The pH measurement was repeated in this way every other day until re-epithelialization took place.
Fig. 1. Day-to-day variations in skin pH value of patient 1 from acute phase to re-epithelialization (patient treated with Hydrogel (Burnshield) and Hyalomatrix).
Fig. 2. Day-to-day variations in skin pH value of patient 2 from the acute phase to re-epithelialization (patient treated with Hydrogel (Burnshield) and Dermasilk).
For the immediate treatment of the burns of both patients, we used hydrogel and SAF with MVTR equivalent to 1600 g/m2. 4For re-epithelialization, we medicated one patient with DermaSilk and the other with Hyalomatrix. The silk consists of 70-78% fibroin, 20-28% sericin, 2-3% ceramids, fats, and minerals. Sericin can bring about allergic reactions. Pure silk consists solely of fibroin with a content very similar to that of human hair. Dermasilk is pure silk, and contains a non-releasable, permanent, odourless, colourless antimicrobial (AEGIS, AEM 5772/5) with a wide spectrum of action that maintains its efficacy intact for the entire life of the substrate. The antimicrobial is a water-based solution of 3-(trimethoxysilyl) propyl-dimethyoctadecyl ammonium chloride which binds through a silane (silicone derivative that permanently alters the properties of a surface) to the fibroin which, in direct contact with the micro-organism, destroys the cell membrane and maintains its efficacy until the silk is soaked with organic substances. However, it resumes its activity once it has been separated from the polluting substance. 7DermaSilk, and pure silk in general, absorbs a quantity of water equivalent to 30% of its dry weight. 3, 6In the other burn patient, synthetic hyaluronic acid (Hyalomatrix) was applied to the cleansed injury site for a period of 10 days. Hyalomatrix has an internal layer, the matrix, consisting of a benzyl ester of biocompatible hyaluronic acid, which is long-lasting because it is particularly resistant to enzymatic degradation, and an external layer consisting of a fine, transparent, semipermeable silicone lamina. The silicone layer acts as a semipermeable barrier against external germs and safeguards against excessive loss of fluids. The lamina is transparent and facilitates monitoring of the wound bed. It is easy to remove after the formation of granulation tissue. When in contact with the serum and/or exudate, hyaluronic acid promotes active healing of the wound by stimulating angiogenesis, cell migration, and proliferation, creating a micro-environment that is favourable to the deposition of dermal constituents for the orderly construction of new skin.
Results
During the first routine phase of burn treatment with hydrogel (Burnshield), the transparent, semipermeable adhesive film guaranteed an extensive and continuous view of the wound, normal personal hygiene and washing practices, and hence a better quality of life for the patient. The semipermeable film (MVTR of 1600) kept the skin well hydrated without allowing micro-organisms to penetrate - during medication with hydrogel and semipermeable film, we observed that the patient’s skin presented a totally normal state of hydration. The same hydration was maintained in a different way by DermaSilk, for while the semipermeable film regulated the transpiration of the water vapour produced by the skin, the pure silk absorbed the water vapour produced by the skin; as it possesses hygroscopic properties, it has the capacity to absorb a quantity of water equivalent to 30% of its dry weight. At the same time, pure silk stimulates re-epithelialization, and DermaSilk also safeguards against microbial contamination. The outer side of Hyalomatrix contains a semipermeable film which is breathable and well tolerated by the patient, also guaranteeing a complete and continuous view of the wound. The mean time for the cessation of pain after application of hydrogel was 2 min, and this was maintained also after application of Hyalomatrix (patient 1) and DermaSilk (patient 2). The mean re-epithelialization time was 24.5 days, i.e. 25 days for the first patient and 24 for the second, with a mean follow-up of 21 months (33 months in the first case and 9 in the second). No complications were observed, whether early (infections) or late (hypertrophic scars).
Analysis of the curves
The skin pH of the first and second patient approximately 30 min post-burn was found to be 8.5 and 8 respectively, continuing to rise in the two days that followed, reaching a peak of 10.5 and 9.5 respectively on day 4, irrespective of the type of therapy administered. We do not know why the pH continued to rise until day 4, notwithstanding the treatment. Further in-depth studies on the pathophysiology of this particular period of the burn will have to be conducted in order to ascertain whether reducing the pH during this phase could bring about more rapid re-epithelialization of the wound. The progressive return of the pH to its normal initial value as the burn zone gradually re-epithelializes is, on the other hand, most probably explained by the progressive production of skin barrier substances by the new cells. It is also important to bear in mind that during the re-epithelialization phase (respectively days 7 and 10 in patients 1 and 2), when the epidermis had not yet appeared at the centre of the wound, the pH value was 8; the pH value at the edges of the same wound was around 6.5. On day 18, the pH returned to normal values, but re-epithelialization was not yet macroscopically complete - it was complete by day 22. As shown by the analysis of the patients’ skin pH curves, different therapies and methods did not lead to substantial differences in the curves or the re-epithelialization times of the two patients. Figs. 1 and 2 present the pH curves of the burned skin, with reference to time, of patient 1 and patient 2 from the day of the burn until the moment of complete re-epithelialization.
Discussion
There are no clinical trials in the literature on skin pH values during the course of burns and on their variations during the re-epithelialization phase, measured with non-invasive methods. The only studies to have measured subcutaneous variations in pH in the course of burns used invasive methods. We conducted this study in order to record the variations in skin pH from the acute phase of the burn through to complete re-epithelialization, and also to assess whether changes in pH can safeguard against damage due to deepening of the wound and keep pain under control, e.g. by modifying or neutralizing the wound’s initial alkalinity. We treated the burns with new materials and innovative methods in order to promote more rapid re-epithelialization, with a view to preventing the onset of late neoplastic complications in deep burns. 10Researchers have demonstrated and emphasized, as we have also done in our study, the importance of cooling in the Casualty Unit and in Emergency Departments during acute phase burns treatment, with a view to reducing the depth of skin wounds. 11, 12It has been observed experimentally in vivo that a locally positioned ACE inhibitor orientates the deposition and direction of hyaluronic acid fibrils in horizontal lines, leading to a marked reduction of scarring. 13This line of research on materials for topical use, with a view to obtaining more rapid re-epithelialization with a more orderly deposition of the skin’s fundamental cells, should undoubtedly be pursued. Also, it has long been known that local compression in a second- or third-degree burn (at risk for keloids and hypertrophic scars) produces hypoxia, which reduces the conversion of fibroblasts to myofibroblasts and mitigates the stoppage of the local production of collagen; compression makes the collagen fibres arrange themselves in parallel fashion, thereby preventing the formation of vorticose collagen structures. 3In contrast, it has also been demonstrated experimentally that local use at the burn site of vasoconstrictors induces progression of the wound. 14It is known that when the skin pH value is more acidic than normal, this produces a burning sensation and that when it is alkaline, there is an itching sensation. An experimental study has confirmed that pure silk not treated with an antimicrobial is, in fact, a biocompatible material that acts as a framework for the regrowth of collagen fibres, to the extent that it actually becomes embedded in the repair tissue. 15An analysis of the pH curves of the burn patients treated in this trial shows that irrespective of the method or the materials used, the trends of the patients’ pH curves were very similar. In actual fact, during the acute phase (day 1 to day 4) the pH values of the patients’ burned skin were decidedly alkaline (pH = 9.5-10.5). This may be due to the skin’s failure to produce barrier substances - as the skin starts to re-epithelialize, pH gradually decreases from day 5 onwards. Further research needs to be carried out on the local application of ACE inhibitor-type materials, using for example graduated local compression or - even better - genetic engineering, in which a sample is taken of a patient’s healthy epidermis, the number of cells is increased in the laboratory, and the cells are re-implanted at the wound site, thereby avoiding potential adverse reactions.
Conclusions
The innovative methods and the various materials used in this trial produced identical re-epithelialization values, which were, however, more rapid than the norm. The development of new materials and of new methods of burn therapy is useful for the treatment of pain, for the ensuring of more rapid re-epithelialization and a better quality of life, and, last but not least, for the reduction of the patient’s medical and social security costs. Patients presenting with late complications such as keloids and hypertrophic scars often have to be subjected to numerous surgical operations in an attempt to prevent deformities and serious physical disabilities, even in young persons.
References
- 1.Panin G. Principi di cosmesi pediatrica. 2002:24. [Google Scholar]
- 2.Bouwsta J.A., Gooris G.S., Dubbelaar F.E., Ponec M. Phase behaviour of skin barrier model membranes at pH 7.4. Cell Mol. Biol. 2000;46:979–92. [PubMed] [Google Scholar]
- 3.Elsner P., Hatch K., Wigger-Alberti W., editors. Textiles and the Skin. Curr. Probl. Dermatol. 2003;31:108–13. doi: 10.1159/000072242. [DOI] [PubMed] [Google Scholar]
- 4.Osti E. Cutaneous burns treated with hydrogel (Burnshield) and a semipermeable adhesive film. Arch. Surg. 2006;141:39–42. doi: 10.1001/archsurg.141.1.39. [DOI] [PubMed] [Google Scholar]
- 5.Sugihara A., Sugiura K., Morita H., Ninagawa T., Tubouchi K., Tobe R., Izumiya M., Horio T., Abraham N.G., Ikehara S. Promotive effects of a silk film on epidermal recovery from full-thickness skin wounds. Exp. Biol. Med. 2000;225:58–64. doi: 10.1046/j.1525-1373.2000.22507.x. [DOI] [PubMed] [Google Scholar]
- 6.Gettings R.L., Triplett B.L. A new durable antimicrobial finish for textiles. AATCC. Book of Papers. 1978:259–61. [Google Scholar]
- 7.Ricci G., Patrizi A., Bendandi B., Menna G., Varotti E., Masi M. Clinical effectiveness of a silk fabric in the treatment of atopic dermatitis. Brit. J. Dermatol. 2004;150:127–31. doi: 10.1111/j.1365-2133.2004.05705.x. [DOI] [PubMed] [Google Scholar]
- 8.Esposito E., Travia G. Impiego del sostituto dermico Hyalomatrix® nelle ustioni pediatriche. XV Meeting Invernale di Chirurgia Plastica. 2003:33–4. [Google Scholar]
- 9.Melandri D., Neri R., Landi G. Hyalomatrix®: un nuovo sostituto dermico in ustioni profonde di 2° e 3° grado. XV Meeting Invernale di Chirurgia plastica. 2003:38–39. [Google Scholar]
- 10.Mellemkjeaer L., Holmich L.R., Gridley G., Rabkin C., Olsen J.H. Risks for skin and other cancers up to 25 years after burn injuries. Epidemiology. 2006;17:668–773. doi: 10.1097/01.ede.0000239651.06579.a4. [DOI] [PubMed] [Google Scholar]
- 11.Nguyen N.L., Gun R.T., Spanon A.L., Ryan P. The importance of immediate cooling - a case series of childhood burns in Vietnam. Burns. 2002;28:173–6. doi: 10.1016/s0305-4179(01)00094-8. [DOI] [PubMed] [Google Scholar]
- 12.Siamanga H. Burn injuries - treatment of burn patients prior to admission to the emergency department. Annals of Burns and Fire Disasters. 2002;15:53–8. [Google Scholar]
- 13.Morihara K., Takai S., Takenaka H., Sakaguchi M., Okamoto Y., Morihara T., Miyazaki M., Kishimoto S. Cutaneous tissue angiotensin-converting enzyme may participate in pathologic scar formation in human skin. J. Am. Acad. Dermat. 2006;54:251–7. doi: 10.1016/j.jaad.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 14.Knabl J.S., Bauer W., Andel H., Schwendenwein I., Dado P.F., Mittlböck M., Römer W., Choi M.S.S., Horvat R., Meissl G., Frey M. Progression of burn wound depth by systemical application of a vasoconstrictor: An experimental study with a new rabbit model. Burns. 1999;25:715–21. doi: 10.1016/s0305-4179(99)00086-8. [DOI] [PubMed] [Google Scholar]
- 15.Armato U., Dal Pra I., Chiarini A., Freddi G. Silk fibroin-structured nonwovens used as scaffolds to engineer reticular connective tissues. Sixth International Meeting Health & Textiles. 2006 [Google Scholar]