Summary
The present review of the literature aims at analysing the challenges facing burn management in low- and middleincome countries (LMICs) and exploring probable modalities to optimize burn management in these countries. In Part 1, the epidemiology of burn injuries and the formidable challenges for proper management due to limited resources and inaccessibility to sophisticated skills and technologies in LMICs were presented. Part II will discuss the actual state of burn injuries management in LMICs.
Keywords: OPTIMIZING, BURN, TREATMENT, COUNTRIES, DEVELOPING, LOW, MIDDLE-INCOME, HEALTH CARE, RESOURCES
Abstract
Les Auteurs de cette revue de la littérature se sont proposés d'analyser les problèmes majeurs que les pays à revenu faible ou intermédiaire (PRFI) doivent affronter dans la gestion des brûlures et d'explorer les modalités possibles pour optimiser la gestion des brûlures dans ces pays. Dans la première partie ils ont considéré l'épidémiologie des brûlures et les énormes problèmes pour garantir leur gestion adéquate en raison des ressources limitées et de l'inaccessibilité des compétences et des technologies sophistiquées dans les PFRI. La deuxième partie s'occupera de l'état actuel de la gestion des brûlures dans les PRFI.
Management of burn injuries in lowand middle-income countries
Burn management in developing countries encounters huge problems at any stage. 26Inadequate access to burn care facilities and a poorly-equipped health care system hinder optimal treatment. 1With no formal infection control policy in most low- and middle-income country (LMIC) burn units and limited aseptic techniques for wound care management, due to nursing constraints and inadequate limited facilities, high rates of burn-related mortality and morbidity are still seen in developing countries. 27, 28This is further complicated by the patients' parents having to apply some of the dressings unsupervised, in less than ideal circumstances, 27and by superstition, 29religious rituals,30 and faith in alternative medicine. 1, 5, 31
Service provision for burns in most LMICs is mainly through the western system of care,1 considered to be the ultimate in patient care. The approach to burn management, however, has to be radically different from that in western countries. 5Certain well-tested, cost-effective treatment procedures need to be adopted to conserve resources5 and make the best of what it is realistically available. Overall poor conditions and lack of resources make excisional surgery impossible for a large percentage of patients. 26, 32, 33
Unfortunately, only a handful of studies evaluating burn interventions in LMICs have been reported, possibly due to lack of the funding necessary to conduct such studies and partly due to lack of expertise in many of these LMICs. 3
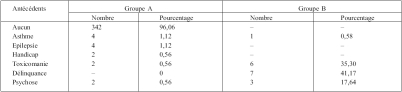
Tableau I. Antécédents pathologiques des patients.
Tous les patients du groupe B proviennent du milieu urbain, dont 64,7% habitent dans des bidonvilles.
First aid, emergency care, and resuscitation
The severity of the burn wound and its clinical manifestation depends not only on the treatment regime at the burn centre but also on first aid and initial management at the burn site, at the emergency department, and during transfer to the burn centre. 32, 33, 34, 35, 36Few population-based studies have been conducted in LMICs about the first aid to be provided and the subsequent healthcare-seeking for burns, along with methods of burn treatment at home. 3, 37, 38, 39
Obviously, traditional values may determine the treatment of burn injuries in the home setting. 40, 41Adequate immediate first aid following a burn appreciably determines outcome and limits tissue damage and subsequent morbidity, including the need for surgery. 42, 43Cool running water at a temperature of between 10 and 15 °C for 20-30 min is considered adequate burn first-aid treatment. 32, , 33, 40, 42, 44, 45In one study about burn treatment in LMICs, including all countries in sub-Saharan Africa, Latin America, and the Caribbean, the Middle East, India, and China, as well as other countries in Asia and adjoining islands, cool water was applied to the burned area as a first-aid therapy in a third of the cases, 3a ratio comparable to that observed in some high-income countries (HICs). 42Naturally, the availability of running water at the appropriate temperature, not universally readily available, in addition to proper education and knowledge, is an obvious limiting factor. Subsequently, since burn wounds are sterile immediately after injury but liable to rapid bacterial colonization, 40, 46the wounds should be covered with a clean sterile sheet until they are dressed. 5, 32, 33
One-half to two-thirds of burned persons in LMICs are reported to be taken to a health care facility for treatment and a significant relationship is found between the size of the burn sustained and subsequent healthcare seeking. 3
Those who seek healthcare have significantly deeper burns covering a wider TBSA or an infected burn previously treated at home. 3In the remaining cases that receive home treatment, non-tested household remedies are commonly used as a first-aid measure in developing countries. 34, 47, 48A traditional preparation is usually applied in the form of concoctions made of urine and mud, cow dung, beaten eggs, or mud and leaves. 3A significant relationship is also found between the size of burn sustained and the type of home-based treatment. Superficial burns and those covering a small body surface area are treated with gentian violet, while more extensive burns are paradoxically treated with a traditional preparation. 3, 38In a report from Turkey, after cold water and ice, raw egg white was most commonly used as first-aid treatment in addition to yogurt, toothpaste, tomato paste, or sliced potato. Most of these substances are harmful, seriously compounding the injury. 40
Unfortunately, most people in Turkey as well as in other LMICs still believe that this kind of medicine is safer and less expensive than western medications and ointments. 40
Early presentation and active resuscitation are the key to successful management of severe burns. Among the components of initial management, fluid resuscitation has a crucial role in preventing complications and reducing the death rate.32-34,49 Initial care is in the line of the ABC of resuscitation.
An adequate airway and respiration must be ensured. All patients except those with minor burns must receive fluid resuscitation based on a simple formula using the Parkland or Carvajal formulas for resuscitation. 5, 26
In some situations, intravenous fluid replacement must be established prior to transfer to a burn centre - however, time should not be wasted to set up an intravenous infusion in the case of a short journey that is expected to take no more than 1 h. 32, 33, 34Unfortunately, such conditions may not be possible to achieve in developing countries. 34First, a first-aid health care provider may not be available at the scene of a burn accident; second, adequate resuscitation at the scene may not be possible due to the considerable ignorance of health care providers about the correct and safe initial management of burns; and third, early transfer of patients may not be possible because of the lack of an available ambulance or other means of transport. 32, 33, 34, 35A long journey during the shock period is in any case challenging and risky, and delay for immediate urgent resuscitation or the treatment of life-threatening problems is the rule in most remote and rural areas and LMICs.
In fire disasters involving a large number of victims, good triage is the cornerstone of effective burn disaster management and should be performed at the disaster site by staff with knowledge of burn treatment, 32, 33largely lacking in most LMICs. Adequate triage must take into consideration the total number of patients, bed availability, and transportation capacity. Increased mortality rates associated with fire disasters in LMICs are due - in addition to limited resources and adequate facilities - to the lack of a proper burn disaster and rescue organization plan. 32
Topical care and dressings
Local burn wound management is one of the most important aspects of burn therapy after the shock phase. Several methods of burn wound management are available today. 50Conventional dressings necessitate, however, topical antimicrobial ointments and creams that may be expensive or not available, and require frequent dressing changes. 50
The cost of these topical agents may even be prohibitive. 51
Economics and logistics dictate that alternatives to the relatively expensive burns dressings available in the developed world are required. 27In a developing country with a fairly large incidence of burns and with financial constraints and limited budgets where all medical resources are stretched beyond practical limits, a major factor that must be considered is how to reduce the cost of therapy and reach a cost-effective management. 50, 52In LMICs an extremely simple, convenient, economical but effective dressing with a long shelf life is required. In addition treatment should be on an outpatient basis as much as possible so that the load on hospital beds is reduced. 5, 52Pursuing conservative burn wound management and using amnion as a biological dressing 5, 53seem to be an appropriate burn management in developing countries.
Human amniotic membranes, used for many years in the treatment of burns, 54are cost effective and on the whole ideal as a burn wound cover. 50, 53They remarkably reduce the cost of dressing changes and the period of stay in hospital for the patient. They also significantly reduce nursing time and hence nursing costs. 50, 55
The procurement and storage of amniotic membrane is easy. 50Amnion stored in glycerol is reliable and effective for a long period of time. 55
It may not be possible for a developing country to afford the kind of "skin banks" that European countries have. But certainly all hospitals in all developing countries can have "amnion banks" providing sufficient and indeed unlimited quantities of an easily available extremely economical biological dressing which can be preserved for a long period of time and which has almost all the qualities of an ideal dressing. 52, 55The rate of wound infection is also significantly low in membrane-treated patients, whether it is fresh or preserved in glycerol. 50Moreover, preserved membranes are relatively free from transmitting bacterial or viral infections, especially HIV and HbSAg. 55Human amnion as a temporary biological wound dressing is certainly inferior to allogenic skin but remains a beneficial and cost-effective means of treating burns in developing countries. 55, 56, 57
Due to the limited resources, traditional medicine still plays a role in the management of a wide range of medical and surgical conditions, including burns. 27, 57, 58In the absence of medical care, in rural Kenya burn wounds are treated with plants and plant juices and covered with large tropical banana leaves. 59In other parts of Africa, traditional first aid may also involve the application of gentian violet, honey, Mentholatum, starch, and a variety of plants and herbs. Particularly favoured by traditional healers are plants such as bitter orange, coriander, grapefruit, lantana, and blue tansy to soothe, treat, and bandage. 59In West Africa more than 25plants have been described specifically for the treatment of burns. 27Papaya paste, readily available and inexpensive, spread on gauze and then applied to the burn wound is a simple topical burn treatment method and seems to be effective. Papaya applied by this method is sufficient for the dressing to stick to the wound and has the advantage of avoiding circumferential dressings, which are uncomfortable in a tropical environment. 27, 59
Typically, the papaya paste is applied once a day, but occasionally twice daily dressings for infected wounds may be necessary. With limited theatre time and blood, and inherent risks to the patient, a major advantage is that topical papaya obviates the need to debride burn wounds surgically.
Papaya appears to be effective in debriding necrotic tissue, preventing burn wound infection, and providing a granulating wound suitable for application of a splitthickness skin graft. Possible mechanisms of action include the activity of the proteolytic enzymes chymopapain, leukopapain, and papain. Papaya also contains carpaine and aglycones, which have a broad spectrum of antimicrobial activity. 27
Boiled potato peels and gauze bandages, onto which they can be affixed and then applied over a thin layer of 5% silver sulphadiazine, have also been proposed as a simple low-cost easy-to-sterilize dressing for superficial partial thickness burn wound coverage in developing countries. 60, 61, 62The application of potato peel dressing was shown to reduce or eliminate desiccation, permit the survival of superficial skin cells, and hasten epithelial regeneration. 60, 61, 62
Boiled potato peel bandages (BPPB) may cause discomfort for some patients, however, and their preparation is time-consuming. 63An even cheaper alternative is banana leaf dressing (BLD). 63, 64Its preparation is very simple and can be easily taught to previously treated patients, relatives of patients, and literate as well as illiterate individuals. 63Banana leaves are readily available in most cities, towns, and villages in LMICs. It is even not difficult to have a patch of land with a banana plantation within the hospital premises in a busy burn unit. Banana leaf dressing, being totally non-adherent, tends to slip. It thus needs careful, firm bandaging. 63BLD is 11 times cheaper than BPPB, 160 times cheaper than Sofratulle (Soframycin impregnated gauze), 1750 times cheaper than Kollagen (collagen sheet), and 5200 times cheaper than Skintemp (biosynthetic dressing). 63
The medicinal properties of honey and other hive products, e.g. pollen, royal jelly, propolis, and bee larvae, have been well described for a variety of medicinal and nutritional purposes, including treatment of burn wounds. 65The beneficial effects of honey include the cleansing of wounds, absorption of oedema fluids, antimicrobial activity, promotion of granulation tissue, epithelialization, and the improvement of nutrition. 66, 67In one study, honey dressing was found to be superior to boiled potato peel dressings as a cover for fresh partial-thickness burns regarding infection control and healing time. 68, 69, 70, 71More recently, MEBO (moist exposed burn ointment) (Julphar Gulf Pharmaceutical Industries, UAE), a traditional Chinese burn ointment, was reported to provide adequate moist environment for optimal healing without the need of a cumbersome and expensive overlying protective dressing. Its main active component is ß-sitosterol in a base of beeswax and sesame oil. 72, 73MEBO has been found to be a useful alternative in the treatment of partial-thickness burns because of its convenient method of application 72, 74and could be a valuable treatment modality in LMICs.
Exposure therapy is often the method of choice as gauze dressings are considered to be expensive. The exposure method is particularly suitable for the treatment of paediatric burn injuries, especially in a tropical climate where patients are nursed under mosquito nets to keep flies and other insects away from open burn wounds. 59
Surgical excision and grafting
Increasingly aggressive surgical approaches with early tangential excision and wound closure are nowadays standard practice in burn units and probably represent the most significant change in recent years, leading to improvement in mortality rates of burn victims at a substantially lower cost. 75, 76, 77, 78, 79, 80, 81Early excision of burned skin was first advocated for small to moderate burns. 51Subsequently, tangential excision in repeated but frequent interventions and immediate skin cover with skin auto- or homografts were recommended for large burns. 51By shortening hospital stay, early burn wound closure reduces infective complications.
Faster healing decreases the severity of hypertrophic scarring, joint contractures, and stiffness and promotes quicker rehabilitation. 75, 76
However, lack of education in general and of health education in particular amongst the common people in the developing countries can hinder acceptance of this procedure and a lack of well-trained and motivated burns surgeons can worsen the situation as well. 81
If proper facilities are lacking, if blood and other resources such as dressings are not available, and if health care providers are inadequately trained and prepared, such aggressive therapy in burn victims can induce further trauma and result in a less than optimal outcome. 27, 75Moreover, without adequate skin cover by autografts, homografts, or other substitutes, the early excision of burned tissue is of no value. 27, 51"Delayed primary" is the second best alternative to "early" burn wound excision and closure, with similar advantages of reducing the risk of septicaemia, mortality, morbidity, hospital stay, and cost of treatment. It should be preferred to "secondary" skin-grafting of granulating wounds. Thus, in the developing countries, indications of delayed primary burn surgery could be: unstable patients or those unfit for surgery during the first post-burn week; 5delay in transfer; 25delay in getting patient's consent for surgery; 8major burns with no available skin substitutes; 3and lack of operating time. 7Contraindications for delayed primary surgery are any sign of invasive sepsis or organ failure. 60
Autografts from uninjured skin remain the mainstay of treatment. Severe burn patients, however, invariably lack adequate skin donor sites 75and not infrequently a temporary coverage needs to be applied following early tangential excision. While in HICs it is possible to collect homografts from cadavers, and skin banks have been created, in most LMICs this is not possible not only because of lack of expertise and facilities but most commonly because of social, cultural, and religious objections and certainly because of cost. In India, for example, harvesting cadaver skin is even forbidden by law. 51Pig skin has been recommended instead, but in Muslim countries or in countries with a large Muslim population the use of porcine products is a sensitive issue, if not completely forbidden as well. 51Synthetic skin replacement products are far too expensive to be of any value for management of severe burns in LMICs. 51BPPB have been developed as a substitute and though they are useful they are not comparable to allografts. Amnion or collagen sheets may be used instead. 51Another alternative would be harvesting skin from live donors - relatives in general. Though the idea seems appealing in some situations, one must not forget that the living donor will be another patient with partial-skin loss requiring treatment, further taxing already stretched and limited resources.
It must be stressed that xenografts, allografts, and other synthetic or tissue-engineered replacements are only a temporary means of burn wound cover. True closure of deep and full-thickness burn wounds is achieved only with living autografts 75, 82provided for coverage of extensive burn injuries by keratinocyte cultures (cultured epithelial autograft [CEA]), largely unavailable in most LMICs for obvious reasons. CEA is expensive to use and very sensitive to infection. It requires meticulous wound care and more professional time and effort than procedures with conventional autografts. 83, 84Needless to say, even if the use of confluent sheets of CEA for the treatment of extensive third-degree burn wounds is considered to be definitely a life-saving procedure, long-term results have been disappointing and at present the true value of CEA is being questioned in most HIC burn centres. Better long-term coverage requires dermal replacement as well as epidermal replacement, which entails even more complex and expensive technologies. 83Early excisional surgery in most LMICs is thus impossible for a large percentage of extensive burn patients. 5
Anaesthesia for burn patients and pain management
The major improvements in quality and safety in anaesthesia over the last 30 years have resulted from advances in technology, refinements in anaesthesia equipment and drugs, and a focus on education and training. These all require significant resources,85 lacking in most LMICs. The financial resources allocated to health are meagre and access to even the most basic of facilities such as clean drinking water remains a serious issue in these countries. 85Electricity supplies are unreliable and many hospitals have neither a mains electricity supply nor a generator always available. 85
Local healthcare resources and international aid are consumed by conditions such as HIV, malaria, and malnutrition. 85
A study conducted in Uganda demonstrated that 23% of anaesthetists had the facilities to deliver safe anaesthesia to an adult, 13% to deliver safe anaesthesia to a child, and 6% to deliver safe anaesthesia for a Caesarean section. 86The critical shortage of manpower is a further barrier to progress. 8, 87In many African and Asian countries the doctor/patient ratio is so low that the ideal of employing a physician specifically to provide routine anaesthesia is invariably out of the question. 87Even though children constitute more than half the population in many countries of the developing world, a paediatric anaesthesiologist per se is a luxury. 87
Anaesthesia does not enjoy a high profile in developing countries and anaesthesia services are not considered a major healthcare issue in LMICs. 87Most anaesthesia is provided by non-physicians and nurses under the direction of a surgeon or unqualified personnel 'trained on the job' with little medical background. 87The morbidity or mortality associated with different methods of anaesthesia in developing countries is not known, and the optimum equipment and drugs for providing a service have not been defined: these will vary according to the facilities available locally. 85
Facilities considered mandatory for the surgical care of children, such as the provision of adequate analgesia, a recovery area for immediate post-operative observation, ventilatory support, and high-level care following surgery, are inadequate or nonexistent in many parts of the developing world. 87
Despite poor conditions, life-saving anaesthesia may be provided. 87In many areas anaesthesia remains largely ketamine based, particularly for children even when halothane or ether is available. 86, 87This is dictated by its ease of use, lack of airway equipment (e.g. tracheal tubes, facemasks, or breathing circuits), and the perception that intravenous access is not necessary or that intravenous cannulae are simply not available. 86, 87Other drugs considered basic to anaesthesia are seldom available in the developing world.
These include induction agents (propofol), neuromuscular blocking agents, analgesics (morphine, pethidine), reversal agents (neostigmine, naloxone), and long-acting local anaesthetics (bupivacaine, ropivacaine). Moreover, the ability to deal with complications such as malignant hyperthermia is virtually impossible. 87Ketamine and ether have many positive features, and any recommendations for changes in existing drugs, techniques, and equipment must take account of all features of running a service in the local environment. 85
The availability of safe blood is a major factor dividing the developed from the developing world. Fewer than 30% of developing countries have a nationally coordinated blood transfusion service, and storage of blood is difficult considering the unreliable and unpredictable electricity supply in many of the poorer countries. Many of these do not even perform the most rudimentary tests for diseases such as HIV or hepatitis B and C, because of financial constraints. 80Patients, particularly children, in developing countries face the greatest risks from unsafe blood and blood products. 87Voluntary unpaid donors are hard to come by in developing countries not only because of the lack of resources but also because of traditional or religious beliefs. In traditional Chinese culture, for example, blood loss is detrimental to health and donation shows disloyalty to one's ancestors. In Africa blood donation is thought to lead to impotency. 87Many countries still rely on paid donors or a family member to donate blood prior to surgery. 87
Pain management, particularly in children, is another factor that divides the developed from the developing world. Provision of pain relief in the face of limited resources and, if available, a limited spectrum of analgesics, as well as inadequately trained staff, is a challenge. Any attempt to apply similar standards to those used in sophisticated units is fraught with difficulty. Illiteracy, malnutrition, poor cognitive development, differing coping strategies, and pharmacogenetic, cultural, and language differences all add to the complexity of the problem. 87Complex techniques that offer the most benefit are seldom available to children in the developing world as they require a minimum standard of monitoring and regular reassessment to allow individualized titration of analgesia, the final choice of which is unfortunately dictated by economic pressure or by the facilities available rather than what would be considered best for a burned child. 87
References
- 1.Lau Y.S. An insight into burns in a developing country: A Sri Lankan experience. Public Health. 2006:958–65. doi: 10.1016/j.puhe.2006.05.016. [DOI] [PubMed] [Google Scholar]
- 2.Kalayi G.D. Mortality from burns in Zaria: An experience in a developing economy. East Afr. Med. J. 2006;83:461–4. doi: 10.4314/eamj.v83i8.9459. [DOI] [PubMed] [Google Scholar]
- 3.Forjuoh S.N. Burns in low- and middle-income countries A review of available literature on descriptive epidemiology, risk factors, treatment, and prevention. Burns. 2006;32:529–37. doi: 10.1016/j.burns.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 4.Forjuoh S.N. Injury control in developing nations What can we learn from industrialized countries? Inj. Prev. 1996;2:90–1. doi: 10.1136/ip.2.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahuja R.B., Bhattacharya S. Burns in the developing world and burn disasters. BMJ. 2004;329:447–9. doi: 10.1136/bmj.329.7463.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Geneva: 2002. The Injury Chart Book :A Graphical Overview of the Global Burden of Injuries, Dept of Injuries and Violence Prevention + Noncommunicable Diseases and Mental Health Cluster. [Google Scholar]
- 7.Murray C.J.L., Lopez A.D., editors. "The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors In 1990 and Projected To 2020". World Health Organization. 1996;1 [Google Scholar]
- 8.Dongo A.E., Irekpita E.E., Oseghale L.O., Ogbebor C.E., Iyamu C.E., Onuminya J.E. A five-year review of burn injuries in Irrua. BMC Health Serv. Res. 2007;7:171. doi: 10.1186/1472-6963-7-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diop-Ndoye M., Bodjona J.P., Diouf E., Beye M.D., Ngom G., Fall I., Ndoye M., Ka-Sall B. Management of thermal severe burns in children in Le Dantec University Teaching Hospital. Dakar Med. 2005;50:194–7. [PubMed] [Google Scholar]
- 10.Aldemir M., Kara I.H., Girgin S., Güloglu C. Factors affecting mortality and epidemiological data in patients hospitalised with burns in Diyarbakir, Turkey. S. Afr. J. Surg. 2005;43:159–62. [PubMed] [Google Scholar]
- 11.Adamo C., Esposito G., Lissia M., Vonella M., Zagaria N., Scuderi N. Epidemiological data on burn injuries in Angola A retrospective study of 7230 patients. Burns. 1995;21:536–8. doi: 10.1016/0305-4179(95)00038-d. [DOI] [PubMed] [Google Scholar]
- 12.Laloë V., Ganesan M. Self-immolation: A common suicidal behaviour in eastern Sri Lanka. Burns. 2002;28:475–80. doi: 10.1016/s0305-4179(02)00047-5. [DOI] [PubMed] [Google Scholar]
- 13.Atiyeh B.S., Saba M. Cost/benefit value of a burn unit at AUBMC. Ann. Burns and Fire Disasters. 1995;8:164–8. [Google Scholar]
- 14.Ferrara M.M., Masellis M., Conte F. "The Management of Mass Burns Casualties and Fire Disasters". Kluwer Academic Publishers; 1992. The philosophy of a burns prevention campaign; pp. 314–6. [Google Scholar]
- 15.Sawhney C.P. Flame burns involving kerosene pressure stoves in India. Burns. 1989;15:362–4. doi: 10.1016/0305-4179(89)90099-5. [DOI] [PubMed] [Google Scholar]
- 16.Gupta R.K., Srivastava A.K. Study of fatal burns cases in Kanpur (India). Forensic Sci. Int. 1988;37:81–9. doi: 10.1016/0379-0738(88)90096-5. [DOI] [PubMed] [Google Scholar]
- 17.Paraffin Safety Association of Southern Africa. www.pasasa.org SABS Stove Test Report. 2005 [Google Scholar]
- 18.Pelaez Mata D.J., Medina Villanueva A., Garcia Saavedra S., Prieto Espunes S., Concha Torre J.A., Menendez Cuervo S., et al. Importance of initial management in severe pediatric trauma. Cir. Pediatr. 2005;18:17–21. [PubMed] [Google Scholar]
- 19.Keswani M.H. Burns in India 1974-1999. Burns. 2000;26:63–4. doi: 10.1016/s0305-4179(99)00152-7. [DOI] [PubMed] [Google Scholar]
- 20.Delagado J., Ramirez-Cardich E.M., Gilamn R.H., et al. Risk factors for burns in children:Crowding, poverty, and poor maternal education. Inj. Prev. 2002;8:38–41. doi: 10.1136/ip.8.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daisy S., Mostaque A.K., Bari T.S., Khan A.R., Karim S., Quamruzzaman Q. Socioeconomic and cultural influence in the causation of burns in the urban children of Bangladesh. J. Burn Care Rehab. 2001;22:269–73. doi: 10.1097/00004630-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Mabrouk A., Maher A., Nasser S. An epidemiology study of elderly burn patients in Ain Shams University Burn Unit, Cairo, Egypt. Burns. 2003;29:687–90. doi: 10.1016/s0305-4179(03)00071-8. [DOI] [PubMed] [Google Scholar]
- 23.Olaitan P.B., Olaitan J.O. Burns and scalds - Epidemiology and prevention in a developing country. Niger. J. Med. 2005;14:9–16. doi: 10.4314/njm.v14i1.37128. [DOI] [PubMed] [Google Scholar]
- 24.Buor D., Bream K. An analysis of the determinants of maternal mortality in sub-Saharan Africa. J. Women's Health. 2004;13:926–38. doi: 10.1089/jwh.2004.13.926. [DOI] [PubMed] [Google Scholar]
- 25.Opaluwa A.S., Orkar S.K. Emphasize burns prevention in developing countries. BMJ. 2004;329:801. doi: 10.1136/bmj.329.7469.801-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rajabian M.H., Aghaei S., Fouladi V. Analysis of survival and hospitalization time for 2057 burn patients in Shiraz, south-western Iran. Med. Sci. Monit. 2007;13:CR353–5. [PubMed] [Google Scholar]
- 27.Prasanna M., Mishra P., Thomas C. Delayed primary closure of the burn wounds. Burns. 2004;30:169–75. doi: 10.1016/j.burns.2003.09.028. [DOI] [PubMed] [Google Scholar]
- 28.Branski L.K., Herndon D.N., Celisa M.M., Norbur W.B., Masters O.E., Jeschke M.G. Amnion in the treatment of pediatric partialthickness facial burns. Burns. 2008 doi: 10.1016/j.burns.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 29.Nordstrom C.R. Exploring pluralism - The many faces of Ayurveda. Soc. Sci. Med. 1988;27:479–89. doi: 10.1016/0277-9536(88)90371-1. [DOI] [PubMed] [Google Scholar]
- 30.Kalantri S.P. Temple healing. Healing temples may breed superstitions. BMJ. 2002;325:968. [PMC free article] [PubMed] [Google Scholar]
- 31.Laloë V. Epidemiology and mortality of burns in a general hospital of Eastern Sri Lanka. Burns. 2002;28:778–81. doi: 10.1016/s0305-4179(02)00202-4. [DOI] [PubMed] [Google Scholar]
- 32.Masellis M., Gunn S.W.A. The Management of Mass Burns Casualties and Fire Disasters. Kluwer Academic Publishers; 1992. Thermal agent disaster and burn disaster: Definition, damage, assessment and relief operation. pp. 7–12. [Google Scholar]
- 33.Masellis M., Ferrara M.M., Gunn S.W.A. Fire disaster and burn disaster:Planning and management. Ann. Burns and Fire Disasters. 1999;12:67–76. [Google Scholar]
- 34.Olaitan P.B., Iyidobi E.C., Olaitan J.O., Ogbonnaya I.S. Burns and scalds: First-aid home treatment and implications at Enugu, Nigeria. Ann. Burns and Fire Disasters. 2004;17:61–3. [Google Scholar]
- 35.Nguyen N.L., Nguyen T.D. First aid and initial management for childhood burns in Vietnam - An appeal for public and continuing medical education. Burns. 2008;34:67–70. doi: 10.1016/j.burns.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 36.Nguyen N.L., Gun R.T., Sparnon A.L., Ryan P. The importance of immediate cooling - A case series of childhood burns in Vietnam. Burns. 2002;28:173–6. doi: 10.1016/s0305-4179(01)00094-8. [DOI] [PubMed] [Google Scholar]
- 37.Guilbaud J. Problems created by the use of cultured epithelia. Ann. Medit. Burns Club. 1993;6:176–8. [Google Scholar]
- 38.Courtright P., Haile D., Kohls E. The epidemiology of burns in rural Ethiopia. J. Epidemiol. Community Health. 1993;47:19–22. doi: 10.1136/jech.47.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Forjuoh S.N., Guyer B., Smith G.S. Childhood burns in Ghana: Epidemiological characteristics and home-based treatment. Burns. 1995;21:24–8. doi: 10.1016/0305-4179(95)90776-v. [DOI] [PubMed] [Google Scholar]
- 40.van de, Velde S., Broosa P., van Bouwelena M., De Wina R., Sermona A., et al. European first-aid guidelines. Resuscitation. 2007;72:240–51. doi: 10.1016/j.resuscitation.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 41.Karaoz B., Kucuk M. Substances used as first-aid home treatment of burns among young children at Milas, Turkey. Burns. 2008;34:294. doi: 10.1016/j.burns.2007.06.015. [DOI] [PubMed] [Google Scholar]
- 42.Forjuoh S.N., Guyer B., Strobino D.M. Determinants of modern health care use by families after a childhood burn in Ghana. Inj. Prev. 1995;1:31–4. doi: 10.1136/ip.1.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rea S., Kuthubutheen J., Fowler B., Wood F. Burn first aid in Western Australia - Do healthcare workers have the knowledge? Burns. 2005;31:1029–34. doi: 10.1016/j.burns.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 44.Skinner A., Peat B. Burns treatment for children and adults: A study of initial burns first aid and hospital care. N. Z. Med. J. 2002;115:199. [PubMed] [Google Scholar]
- 45.Haberal M., Moray G., Kut A. The current status of burn centers and burn care in Turkey. In: Haberal M., Moray G., Kut A., editors. Burn Care Facilities At Baskent University. Vol. 8. Baskent University Publications; 2004. [Google Scholar]
- 46.Hudspith J., Rayatt S. First aid and treatment of minor burns. BMJ. 2004;328:1487–9. doi: 10.1136/bmj.328.7454.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nguyen N.L., Gun R.T., Sparnon A.L., Ryan P. The importance of initial management:A case series of childhood burns in Vietnam. Burns. 2002;28:167–72. doi: 10.1016/s0305-4179(01)00079-1. [DOI] [PubMed] [Google Scholar]
- 48.Kumar P., Chirayil P.T., Chittoria R. Ten years' epidemiological study of pediatric burns in Manipal, India. Burns. 2000;26:261–4. doi: 10.1016/s0305-4179(99)00109-6. [DOI] [PubMed] [Google Scholar]
- 49.Johnson D., Coleman D.J. Ink used as first-aid treatment of a scald. Burns. 2000;26:507–8. doi: 10.1016/s0305-4179(00)00012-7. [DOI] [PubMed] [Google Scholar]
- 50.Shahin A., Shadata G., Franka M.R., Abusetta A., Brogouski A., Ezzaidi M.M. Complications of burns in children - A study of 266 severely burned children admitted to a burn centre. Ann. Burns and Fire Disasters. 1998;11:34–6. [Google Scholar]
- 51.Atiyeh B.S., Gunn S.W.A., Hayek S.N. Provision of essential surgery in remote and rural areas. J. Humanitarian Med. doi: 10.1016/j.ijsu.2010.07.291. [DOI] [PubMed] [Google Scholar]
- 52.Heimbach D. Burn patients, then and now. Burns. 1999;25:1–2. doi: 10.1016/s0305-4179(98)00154-5. [DOI] [PubMed] [Google Scholar]
- 53.Lorusso R., Geraci V., Masellis M. The treatment of superficial burns with biological and synthetic material: Frozen amnion and biobrane. Ann. Burns and Fire Disasters. 1989;2:79–84. [Google Scholar]
- 54.Starley I.F., Mohammeda P., Schneider G., Bickler S.W. The treatment of paediatric burns using topical papaya. Burns. 1999;25:636–9. doi: 10.1016/s0305-4179(99)00056-x. [DOI] [PubMed] [Google Scholar]
- 55.Ravishanker R., Batha A.S., Roy R. "Amnion Bank" - The use of long-term glycerol preserved amniotic membranes in the management of superficial and superficial partial-thickness burns. Burns. 2003;29:369–74. doi: 10.1016/s0305-4179(02)00304-2. [DOI] [PubMed] [Google Scholar]
- 56.Maral T., Borman H., Arslan H., Demirhan B., Akinbingol G., Haberal M. Effectiveness of human amnion preserved long-term in glycerol as a temporary biological dressing. Burns. 1999;25:625–35. doi: 10.1016/s0305-4179(99)00072-8. [DOI] [PubMed] [Google Scholar]
- 57.Atiyeh B.S., Gunn S.W.A., Hayek S.N. New technologies for burn wound closure and healing - Review of the literature. Burns. 2005;31:944–56. doi: 10.1016/j.burns.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 58.Purma Sai, K. Babul, M. Traditional medicine and practices in burn care:Need for newer scientific perspectives. Burns. 1998;24:387–8. doi: 10.1016/s0305-4179(98)00087-4. [DOI] [PubMed] [Google Scholar]
- 59.Hodges S.C., Mijumbi C., Okello M., et al. Anaesthesia services in developing countries:Defining the problems. Anaesthesia. 2007;62:4–11. doi: 10.1111/j.1365-2044.2006.04907.x. [DOI] [PubMed] [Google Scholar]
- 60.Kopp K., Wang G.Y., Horcha R.E., Palluac N., Ge S.D. Ancient traditional Chinese medicine in burn treatment:A historical review. Burns. 2003;29:473–8. doi: 10.1016/s0305-4179(03)00053-6. [DOI] [PubMed] [Google Scholar]
- 61.Keswani M.H., Vartaka A.M., Patila A., Davies J.W.L. Histological and bacteriological studies of burn wounds treated with boiled potato peel dressings. Burns. 1990;16:137–43. doi: 10.1016/0305-4179(90)90175-v. [DOI] [PubMed] [Google Scholar]
- 62.Patil A.R., Keswani M.H. Bandages of boiled potato peels. Burns. 1985;11:444–5. doi: 10.1016/0305-4179(85)90153-6. [DOI] [PubMed] [Google Scholar]
- 63.Jurjus A., Atiyeh B.S., Inaya A., Hussein H., Jurjus R.A., Hayek S.N., Abou Jaoude M., Gerges A., Tomeh R. Pharmacological modulation of wound healing in experimental burns. Burns. 2007;33:892–907. doi: 10.1016/j.burns.2006.10.406. [DOI] [PubMed] [Google Scholar]
- 64.Gore M.A., Akolekar D. Evaluation of banana leaf dressing for partial-thickness burn wounds. Burns. 2003;29:487–92. doi: 10.1016/s0305-4179(03)00050-0. [DOI] [PubMed] [Google Scholar]
- 65.Keswani M.H., Patil A.R. The boiled potato peel as a burn wound dressing:A preliminary report. Burns. 1985;11:220–4. doi: 10.1016/0305-4179(85)90075-0. [DOI] [PubMed] [Google Scholar]
- 66.Subrahmanyam M. Honey dressing for burns - An appraisal. Ann. Burns and Fire Disasters. 1996;9:33–5. [Google Scholar]
- 67."The Injury Chart Book - A Graphical Overview of the Global Burden of Diseases and Mental Health Cluster". World Health Organization, Geneva. 2002 [Google Scholar]
- 68.Subrahmanyam M. Addition of antioxidants and polyethylene glycol 4000 enhances the healing property of honey in burns. Ann. Burns and Fire Disasters. 1996;9:93–5. [Google Scholar]
- 69.Subrahmanyam M., Sahapure A.G., Nagane N.S, Bhagwat V.R., Ganu J.V. Effects of topical application of honey on burns wound healing. Ann. Burns and Fire Disasters. 2001;14:143–5. [Google Scholar]
- 70.Subrahmanyam M., Hemmady A.R., Pawar S.G. The sensitivity to honey of multidrug-resistant Pseudomonas aeruginosa from infected burns. Ann. Burns and Fire Disasters. 2003;16:84–7. [Google Scholar]
- 71.Medaa A., Lamiena C.E., Millogob J., Romitoc R., Nacoulmaa O.G. Therapeutic uses of honey and honeybee larvae in central Burkina Faso. J. Ethnopharmacology. 2004;95:103–7. doi: 10.1016/j.jep.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 72.Subrahmanyam M. Honey dressing versus boiled potato peel in the treatment of burns: A prospective randomized study. Burns. 1996;22:491–3. doi: 10.1016/0305-4179(96)00007-1. [DOI] [PubMed] [Google Scholar]
- 73.Ang E.S., Lee S.T., Gan C.S., See P. The role of alternative therapy in the management of partial-thickness burns of the face - Experience with the use of moist exposed burn ointment (MEBO) compared with silver sulphadiazine. Ann. Acad. Med. Singapore. 2000;29:7. [PubMed] [Google Scholar]
- 74.Atiyeh B.S., Ioannovich J., Magliacani G., Masellis M., Costagliola M., Dham R., Al-Musa K.A. A new approach to local burn wound care: Moist exposed therapy. A multiphase, multicenter study. J. Burns and Surgical Wound Care. 2003;2:18. [Google Scholar]
- 75.Karim K., Alam I., Hasan N., Khan A. The socio-economic factors of burn injuries in children. Burns. 1975;1:145–8. [Google Scholar]
- 76.Atiyeh B.S., Gunn S.W.A., Hayek S.N. State of the art in burn treatment. World J. Surg. 2005;29:131–48. doi: 10.1007/s00268-004-1082-2. [DOI] [PubMed] [Google Scholar]
- 77.Linn B.S., Stephenson S.E., Bergstresser P.R., et al. Do dollars spent relate to outcomes in burn care? Med. Care. 1979;17:835–43. doi: 10.1097/00005650-197908000-00006. [DOI] [PubMed] [Google Scholar]
- 78.Lofts J.A. Cost analysis of a major burn. N.Z. Med. J. 1991;16:488–90. [PubMed] [Google Scholar]
- 79.Munster A.M., Smith-Meek M., Sharkey P. The effect of early surgical intervention on mortality and cost-effectiveness in burn care (1978-1991). Burns. 1994;20:61–4. doi: 10.1016/0305-4179(94)90109-0. [DOI] [PubMed] [Google Scholar]
- 80.Ramzi P.I., Barret J.P., Herndon D.N. Thermal injury. Crit. Care Clin. 1999;15:333–52. doi: 10.1016/s0749-0704(05)70058-0. [DOI] [PubMed] [Google Scholar]
- 81.Ramakrishnan K.M., Jayaraman V. Management of partial-thickness burn wounds by amniotic membrane: A cost-effective treatment in developing countries. Burns. 1997;23:S33–S36. doi: 10.1016/s0305-4179(97)90099-1. [DOI] [PubMed] [Google Scholar]
- 82.Atiyeh B.S., Ioannovich J., Magliacani G., et al. A new approach to local burn wound care: Moist exposed therapy. A multiphase, multicenter study. J. Burns Surg. Wound Care. 2003;2:18. [Google Scholar]
- 83.Broz L., Vogtova D., Königová R. Experience with banked skin in the Prague Burn Center. Acta Chir. Plast. 1999;41:54–8. [PubMed] [Google Scholar]
- 84.Atiyeh B., Costagliola M. Cultured epithelial autograft (CEA):Three decades later. Burns. 2007;33:404–13. doi: 10.1016/j.burns.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 85.Hodges S.C., Mijumbi C., Okello M., McCormick B.A., Walker I.A., Wilson I.H. Anaesthesia services in developing countries: Defining the problems. Anaesthesia. 2007;62:4–11. doi: 10.1111/j.1365-2044.2006.04907.x. [DOI] [PubMed] [Google Scholar]
- 86.Bösenberg A.T. Pediatric anesthesia in developing countries. Current Opinion Anaesthesiology. 2007;20:204–10. doi: 10.1097/ACO.0b013e3280c60c78. [DOI] [PubMed] [Google Scholar]
- 87.Chongchet V. The use of sterile, steamed banana leaves in the local treatment of burns. Burns. 1980;6:264–5. [Google Scholar]