Summary
The aim of this study is to draw attention to acute acalculous cholecystitis, a rare complication that may occur during the post-burn period (usually within 20-30 days). A 42-yr-old male patient, the victim of 35% TBSA high-voltage electrical burns that caused the amputation of both upper extremities by day 45 post-burn, was brought to our operating theatre suffering from acute acalculous cholecystitis. Mild epigastric pain followed by reflex nausea, vomiting, and pain that shifts to the upper quadrant and considerably increases during the post-burn period should make the therapist think of acalculous cholecystitis and react immediately with an urgent operation. Diagnosis of acute acalculous cholecystitis in a burn patient depends on recognizing a combination of signs and symptoms which are often attributed to other problems. Once diagnosed, the best choice of treatment for acalculous cholecystitis is cholecystectomy in an otherwise clinically stable patient.
Keywords: ACUTE, ACALCULOUS, CHOLECYSTITIS, RARE, COMPLICATION, BURN INJURY
Abstract
Les Auteurs de cette étude attirent l'attention sur la cholécystite acalculeuse aiguë, une complication rare qui peut se manifester pendant la période postbrûlure (normalement après 20-30 jours). Un patient mâle âgé de 42 ans, atteint de brûlures électriques de haute tension dans 35% de la surface totale corporelle qui ont provoqué l'amputation des deux extrémités supérieures 45 jours après l'accident, a été porté en salle opératoire pour être opéré de cholécystite acalculeuse aiguë. Si un patient présente une légère douleur épigastrique, suivie par réflexe nauséeux, vomissement et une douleur qui se déplace au cadran supérieur et augmente sensiblement dans la période postbrûlure, il faut que le thérapeute pense à la possibilité d'une condition de cholécystite acalculeuse et que le patient soit opéré en urgence. Pour exprimer un diagnostic de cholécystite acalculeuse dans un patient brûlé il faut reconnaître une combinaison de signaux et symptômes souvent attribués à d'autres problèmes. Une fois diagnostiquée une condition de cholécystite acalculeuse, le meilleur traitement, pour un patient cliniquement stable, est la cholécystectomie.
Introduction
Acute acalculous cholecystitis (AAC), defined as an inflammation of the gallbladder without evidence of calculi (stones), comprises 2-14% of all cases of acute cholecystitis.
According to the literature, the conditions associated with the presence of AAC are burns, severe trauma, the administration of total parenteral nutrition (TPN), pancreatitis, sepsis, and critically illness in a patient following cardiac or abdominal vascular surgery. This inflammation is closely associated with gangrenous gallbladder, perforation of the cyst, empyema, and quite high mortality and morbidity rates. De novo presentation is possible, but there are some predisposing factors, such as major cardiovascular disorders, complicated diabetes mellitus, autoimmune disease, and AIDS.
Especially in burns, AAC seems to be a real timebomb for the patient, ready to explode if one is not careful in the early post-burn period. A series of universal pathological tests may mask the presence of AAC in a burn patient:
elevated white blood cell count
fever
increased liver function tests (non-specific and frequent in patients receiving TPN)
The trickiest aspect in diagnosis of the disease is the absence of clinical signs: there is no way of estimating a right quadrant tenderness or Murphy's sign in an intubated patient or when narcotic medication has been administered.
This makes the diagnosis of acute acalculous cholecystitis a real challenge for the plastic surgeon. Ultrasound tests are the gold standard for differential diagnosis. According to Chen and Aliopoulios, positive findings include:
presence of sludge in the gallbladder
thickening of the gallbladder wall
transverse diameter > 5 cm
wall thickness > 4 mm
Hepatoiminodiacetic acid and PIPIDA scans may confirm diagnosis of a non-filling gallbladder but they have low sensitivity (only 68%) and often require risky transport of the patient outside the burns unit. Computed tomography and diagnostic laparoscopy are also solutions in cases that are difficult to diagnose.
Various mechanisms are proposed for the aetiology of AAC, including bile stasis, change in bile pigment, gallbladder ischaemia, and the activation of XII-factor-dependent pathways. Bile stasis is mainly caused by dehydration during the first days post-burn, prolonged fasting when enteral nutritional support is not an option, the use of TPN (caution is necessary with refeeding after TPN), high doses of narcotics for pain control leading to contraction of the sphincter of Oddi, hypoalbuminaemia and local inflammation with direct result oedema, and obstruction of the ampulla of Vater, as well as multiple blood perfusions.
PEEP ventilation is also a factor known to cause bile stasis and gallbladder ischaemia by reducing blood flow through the choleduodenal junction and increasing venous congestion. Inhalation injuries and airway burns requiring a period of ventilator support also lead to further bile stasis and the development of AAC.
Gallbladder ischaemia secondary to shock (by decreased perfusion) and vascular insufficiency during the hypotensive shock state are acknowledged as leading to histopathological findings such as gallbladders that are gangrenous or present areas of focal necrosis. Sepsis in the post-burn period plays a controversial role in the development of AAC: we still cannot distinguish whether sepsis is the primary mechanism or a secondary event in an already damaged gallbladder. We do know, though, that bacterial endotoxins can activate factor-XII-dependent pathways, and fragments of this factor can be found in blood transfusion products, probably due to cold storage.
The direct exposure of plasma to collagen during a burn can increase factor XII and lead to gallbladder injury.
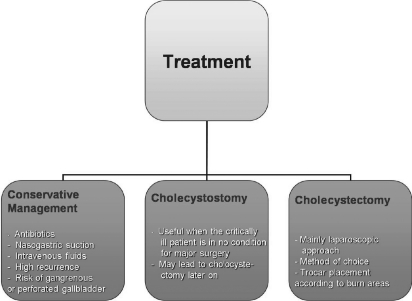
The treatment of AAC is presented (Fig. 1).
Fig 1. Treatment of acute acalculous cholecystitis.
Materials and methods
A 42-yr-old patient presented with a 35% TBSA electrical burn. On post-burn day 45, after amputation of both arms, he complained of:
sudden pain in the right upper quadrant
nausea
steadily increasing vomiting
Lab tests revealed an elevated white blood cell count and hepatic enzymes, plus mild jaundice.
Even though Murphy's sign was negative, the persistent fever and the acute change of the clinical course gave rise to suspicion of acute acalculous cholecystitis.
Results
Ultrasound tests of the abdomen revealed the presence of sludge in the gallbladder, increased wall thickness, and hypervascularization during the power Doppler examination (Figs. 2,3). The patient's clinical condition was critical and he was taken to the operating theatre, where laparotomy revealed free bile in the abdomen caused by perforation of a gangrenous gallbladder, despite of the lack of any clinical signs. His condition has been stable ever since.
Fig 2. Ultrasound findings.
Fig 3. Ultrasound findings.
Discussion
In the first 30 days post-burn our patient received high doses of mercurochrom on the burn areas. According to the literature, mercury partially absorbed by the skin remains in organs such as the liver and kidneys for a long time in high concentrations, and here we present a case of mercury-induced acalculous cholecystitis. There is not enough evidence yet to connect the use of mercury and the development of AAC. From our clinical experience, prompt initiation of enteral nutrition prevents bacterial dislocation and further gallbladder complications.
Successful resuscitation of hypovolaemic shock in burns is essential for preventing peptic tube ischaemia.
Antibiotics play an important role in the management of critically ill patients, but cannot prevent the recurrence of cholecystitis.
As a preventive step one can propose early escharectomy when the area of the right upper quadrant is burned.
Skin grafting on abdominal necrotic eschars prepares the "ground" for possible (open or laparoscopic) cholecystectomy, when needed.
References
- 1.Dermott M.W., Scudamore C.H., Boileau L.O., Snelling C.F., Kramer T.A. Acalculous cholecystitis: Its role as a complication of major burn injury. Can. J. Surg. 1985;28:529–533. [PubMed] [Google Scholar]
- 2.Ross D.C., Lee K.C., Peters W.J., Douglas L.G. Acalculous cholecystitis in association with major burns. Burns. 1987;13:488–491. doi: 10.1016/0305-4179(87)90229-4. [DOI] [PubMed] [Google Scholar]
- 3.Still J., Scheirer R., Law E. Acute cholecystectomy performed through cultured epithelial autografts in a patient with burn injuries: A case report. J. Burn Care Rehabil. 1996;17:429–431. doi: 10.1097/00004630-199609000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Owen C., Jain R. Acute acalculous cholecystitis. Curr. Treat. Options Gastroenterol. 2005;8:99–104. doi: 10.1007/s11938-005-0001-4. [DOI] [PubMed] [Google Scholar]