Summary
The Karolinska Burn Unit in Stockholm, Sweden, carried out a retrospective case review in order to compare the cost of the current protocol of care - in place since mid-2002 - with a previous protocol in paediatric burn patients. The study compared the years 2004 and 2007 with the year 2001. 2004 was the first full year in which the unit staff used ActicoatTM (Smith & Nephew Wound Management, Hull, England), IntraSite GelTM (idem), and Allevyn AdhesiveTM (idem) in the treatment of paediatric burns patients. In 2001 the unit used MepitelTM (Molnlycke, Göteborg, Sweden) together with a saline solution and peroxide for cleansing. This study examined differences in both labour and material costs, measured from the hospital's perspective. Our results show that the main impact of the new protocol was on length of stay for hospitalized patients. In 2001 the mean in-patient stay was 12.5 days; in 2004 the mean stay was 5.6 days and, in 2007, 4.5 days (p < 0.001). It is hypothesized that the reason for this significant reduction in length of stay is that most of the patients treated with Acticoat were sent home earlier to be treated as outpatients because there was less need for sedation and/or analgesics, and because the risk of infection was perceived to be less. Pure hospitalization costs per in-patient were approximately Swedish kronor (kr) 67,725 in 2001 (1 kr = approx. € 0.1 or US$ 0.15) and kr 30,305 and kr 24,440 in 2004 and 2007, respectively. This represents a saving of 55% and 64% with respect to 2001 costs.
Keywords: COST, BURN, PAEDRIATIC, HOSPITAL
Abstract
L'unité des grands brûlés Karolinska à Stockholm, en Suède, a effectué un examen rétrospectif des cas traités afin de comparer le coût de l'actuel protocole de soins - en place depuis mi-2002 - avec un protocole précédent utilisé pour les patients pédiatriques brûlés. L'étude a comparé les années 2004 et 2007 avec l'année 2001. L'année 2004 a été la première où le personnel d l'unité a utilisé l'ActicoatTM (Smith & Nephew Wound Management, Hull, Angleterre), IntraSite GelTM (idem) et Allevyn AdhesiveTM (idem) dans le traitement des patients brûlés pédiatriques. En 2001, l'unité utilisait MepitelTM (Molnlycke, Göteborg, Suède) avec une solution saline et de peroxyde pour le nettoyage. Cette étude a examiné les différences dans les coûts soit du personnel soit du matériel, mesurés du point de vue de l'hôpital. Nos résultats montrent que le principal impact du nouveau protocole a été sur la durée du séjour des patients hospitalisés. En 2001, la durée moyenne de l'hospitalisation était de 12,5 jours; en 2004 elle était de 5,6 jours et en 2007 de 4,5 jours (p < 0,001). Selon l'hypothèse des Auteurs, la raison de cette réduction significative de l'hospitalisation est que la plupart des patients traités avec l'Acticoat ont été renvoyés plus tôt à la maison pour être traités en clinique externe parce qu'ils avaient moins besoin de sédation et/ou de traitement analgésique et parce que le risque de l'infection a été évalué comme réduit. Les coûts de l'hospitalisation pure par patient ont été d'environ de couronnes suédoises (kr) 67.725 en 2001 (1 kr = env. € 0,1 ou 0,15 $US) et kr 30.305 et kr 24.440 en 2004 et 2007, respectivement. Cela représente une économie de 55% et 64% par rapport aux coûts de 2001.
Introduction
Owing to the current budgetary pressures in every European healthcare system, it is becoming increasingly important to look at costs as an additional important factor to bear in mind in modern medical practice. In a context of shrinking healthcare budgets, there is increasing pressure on all involved - healthcare professionals, managerial staff, economists, and even politicians - to demonstrate that the maximum quality of care is being achieved with the best possible 'value for money'. Studies, for instance by Mathews et al.,1 have shown that in the area of burn care significant savings can be made by changing the treatment protocol.
In Sweden, the main component of the Karolinska Burn Unit's treatment protocol for paediatric burns since mid 2003 has been ActicoatTM (Smith & Nephew); it is used in combination with IntraSite GelTM and Allevyn AdhesiveTM (both Smith & Nephew). ActicoatTM is a nanocrystalline silver dressing composed of two layers of silver-coated highdensity polyethylene, enclosing a rayon/polyester core of apertured non-woven fabric. The elements that compose ActicoatTM are welded together ultrasonically. When moistened with water, microscopic nanocrystals of metallic silver are released from the dressing onto the wound bed. The silver has an anti-microbial action which destroys a range of bacteria, including both Gram-positive and Gram-negative bacteria.2 In the past, ActicoatTM has sometimes been perceived by hospitals as expensive and therefore, although many burn units do use it, its use is not particularly widespread.
In contrast, prior to mid-2003, the Karolinska Burn Unit used a dressing that consisted primarily of MepitelTM (Mölnlycke Health Care). This was used in combination with a saline solution and the wound was cleaned with peroxide at dressing changes. MepitelTM is a porous, semitransparent,low-adherent wound contact layer, designed for use on various different types of wounds, such as abrasions, burns, skin tears, and chronic wounds. The product is designed to allow exudate to pass into an outer absorbent dressing; it does not stick to the wound bed, but adheres to the healthy surrounding skin, and is therefore easy to remove for dressing changes. MepitelTM is almost transparent, which enables easier inspection by the medical staff. The aim of this study was to look at costs of the current treatment protocol (ActicoatTM) in order to compare them with those of the prior protocol (MepitelTM) from a hospital perspective. Therefore, only costs borne by the hospital were taken into consideration. For this purpose, the year 2001 was compared with the year 2004 (first full year when the new protocol of care was implemented) and the year 2007 (latest year for which data were available at the time we started our analysis). The key cost drivers analysed were dressing and labour costs, overall hospital length of stay, and antibiotic use.
Materials and methods
The study consisted of a retrospective case review, which examined costs in the Karolinska Burn Unit, Stockholm (Sweden) in three periods. The study periods were as follows:
January-December 2001. All patients treated with MepitelTM protocol
January-December 2004. Almost all patients treated with ActicoatTM protocol
January-December 2007. Almost all patients treated with ActicoatTM protocol
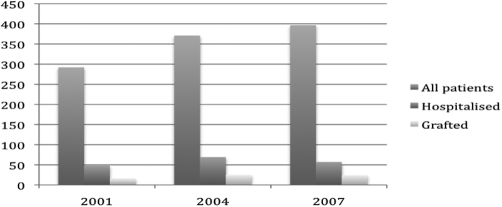
In 2001 292 paediatric burn patients were treated at the hospital, of whom 48 (16.4%) were treated as in-patients. In 2004 371 patients were treated, of whom 69 (18.6%) were in-patients. In 2007, out of 397 patients treated, only 57 (14.4%) were in-patients. Fig. 1 shows overall patient numbers, the number of patients admitted as inpatients, and the number of patients requiring grafting. An analysis of the data, using Medlog,3 a clinical data management system that employs standard statistical analysis, found the patients had the characteristics presented in Table I.
Fig. 1. Patient numbers.
Table I. Patients’ characteristics.

There was no evidence of any difference in the mean total body surface area burned between the three periods compared (p = 0.993).
Material and hospitalization costs were taken from 2001 hospital data, and updated to 2007 costs by applying Consumer Price Index data.4 For the purpose of measuring the differences between the groups, from a hospital perspective, we calculated the cost associated with dressing changes, the use of antibiotics, and the length of inpatient hospital stay.
Results
There was no difference in the proportion of patients admitted for in-patient care, but the mean length of stay (LOS) was significantly shorter in 2004 and in 2007 than in 2001. In 2001 the mean in-patient LOS for patients admitted to the hospital was 12.47 days. The mean LOS was 5.58 days (p < 0.001) in 2004 and 4.5 days in 2007 (p < 0.001 compared with 2001). The median of the LOS, which excludes the effect of some exceptional patients staying for protracted periods, shows a more distinct difference, with 11 days in 2001 and 2 days in 2004 and 2007 (p < 0.001). Our explanation of this significant reduction in LOS is that that most of the patients treated with Acticoat were sent home earlier to be treated as out-patients because there was less need for sedation and/or analgesics, and because the risk of infection was perceived to be less. When the original protocol was in place most patients stayed longer in hospital in order to facilitate frequent check-ups, which were considered necessary to prevent potential infections (check-ups tended to take place every second or third day).
The mean cost per patient per day spent in the hospital was 5,431 Swedish kronor (kr) (1 kr = approx. € 0.1 or US$ 0.15). The cost of pure hospitalization per patient for the 2001 group amounted to approximately kr 67,725, while in 2004 it was kr 30,305 and in 2007 kr 24,440 This represents a saving of kr 37,420 and 43,285 per in-patient in 2004 and 2007 respectively. If we add in the cost of dressing changes the overall picture does not change.
Although the frequency of dressing changes tended to be lower with the current protocol than with that of 2001 (approximately 1.82 versus 2.66 changes per week respectively), we did not record enough data to be able to calculate p values and for the purpose of our exercise we therefore assumed a frequency of 2.66 changes per week for both protocols.
Despite the higher unit cost of the dressings used since mid-2002 (kr 278 per change compared to kr 83 per change with the 2001 protocol), the dressing cost difference did not outweigh the reduction in cost linked to the reduction in length of stay observed that year (Table II).
Table II. Cost differences to the hospital per in-patient.

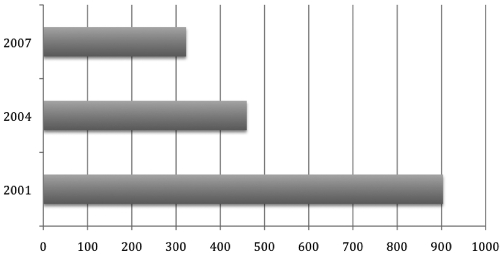
While the most important factor in the study was the length of stay, one more factor worth noting was analysed: the need to use antibiotics also fell with the introduction of the new care protocol. While in 2001 70% of hospitalized patients required antibiotics, in 2007 this figure fell to 25% (p < 0.001). In economic terms this translates into a small saving of kr 581.84 per in-patient treated with the current protocol (Fig. 2).
Fig. 2. Mean cost per patient (in kronor) of antibiotic use.
Discussion and conclusion
Our study results show that the difference in length of stay was by far the most important component in terms of cost. Other findings, although of interest, had relatively little impact on the overall cost to the hospital. The treatment with Acticoat introduced in mid-2002 meant that many patients could be sent home earlier to be treated on an out-patient basis, while when the old protocol was in place patients needed to stay in hospital for significantly longer periods of time.
The study had a number of limitations, of which perhaps the most important was that it compared different protocols at different points in time. Thus, changes in protocols other that the actual products used could also have had an impact on the overall results of the analysis.
Furthermore, it was the aim of the study to look solely at costs and not at health outcomes. Future studies capturing both could be very informative.
Our study nevertheless does show real-life results seen at the Karolinska hospital burn unit following the introduction of the new protocol, which indicate that treating patients with dressings that could help control and prevent infections and that do not require very frequent dressing changes could reduce some of the current budgetary pressures that most burn hospital units are exposed to.
Another area where additional research could be of great value is that of the burden imposed on family members when a paediatric patient is sent home. The psychological and economical impact on the family should be evaluated in order to obtain the full picture.
References
- 1.Mathews J, Supple K, Calistro A et al. A burn centre costreduction program. J Burn Care RehabiL. 1997;18:358–363. doi: 10.1097/00004630-199707000-00016. [DOI] [PubMed] [Google Scholar]
- 2.Yin HQ, Langford R, Burrell RE. Comparative analysis of the antimicrobial activity of ACTICOAT antimicrobial barrier dressing. J Burn Care Rehabil. 1999;20:195–200. doi: 10.1097/00004630-199905000-00006. [DOI] [PubMed] [Google Scholar]
- 3.www.medlog.com [Google Scholar]
- 4.Consumer Price Index. The Economist Intelligence Unit, www.eiu.com. 2006 [Google Scholar]