Abstract
Objective
This case report describes a patient with nocturnal bruxism and related neck pain treated with botulinum toxin type A (BTX-A).
Clinical Features
The patient was a 27-year-old man with nocturnal bruxism and difficulty in active mouth opening and chewing and neck pain at rest. His numeric pain score was 7 of 10. Surface electromyography of the temporalis and masseter muscles showed typical signs of hyperactivity, characterized by compound muscle action potential amplitude alterations.
Intervention and Outcome
After clinical evaluation, he was treated with BTX-A to reduce masseter and temporalis muscle hyperactivity. After 3 days of treatment with BTX-A, with each masseter muscle injected with a dose of about 40 mouse units with a dilution of 1 mL and with temporal muscle bilaterally injected with 25 mouse units with the same dilution, a decrease in bruxism symptoms was reported. Neck pain also decreased after the first treatment (visual analog scale of 2/10) and then resolved completely. After 4 weeks, electromyography showed the reduction of muscle hyperactivity with a decrease in the amplitude of the motor action potential. The same reduction in signs and symptoms was still present at assessment 3 months posttreatment.
Conclusion
These findings suggest that BTX-A may be a therapeutic option for the treatment of bruxism and related disorders.
Key indexing terms: EES: bruxism, Neck pain, Botulinum toxin type A
Introduction
In the last 20 years, botulinum toxin type A (BTX-A) has been used as a therapeutic instrument to treat a variety of conditions characterized by muscular and gland hyperfunction. Recent reports have indicated that BTX-A is safe and effective in the treatment of neuromuscular disorders such as focal, segmental dystonia (torticollis, oromandibular dystonia, laryngeal dystonia, writer's cramp); hemifacial spasm1; and hypersecretory disorders such as hyperhidrosis and sialorrhea.2-4 Botulinum toxin type A injected into the skeletal muscle belly prevents the release of acetylcholine from the presynaptic axon of the motor endplate and blocks signal transmission at the neuromuscular junction. This process reduces muscle contraction, inducing a weakness condition.
Bruxism is a particular form of dystonia, a psychophysiologic disorder, and a common clinical issue in dentistry.5 Bruxism, defined as forcible clenching or grinding of the teeth, or a combination of both, has long been regarded as a disorder requiring treatment.6-8 Bruxism has also been defined as (a) the parafunctional grinding of teeth and (b) an oral habit consisting of involuntary rhythmic or spasmodic nonfunctional gnashing, grinding, or clenching of the teeth, in other than chewing movements of the mandible, which may lead to occlusal trauma—also called tooth grinding or occlusal neurosis, according to the Glossary of Prosthodontic Terms.9 Bruxism is often classified as diurnal (occurring when the individual is awake) or nocturnal (occurring when the individual is sleeping).6 In addition, bruxism may be audible (when teeth are grinding) or inaudible (when teeth are clenched).5 For a more operational definition, the American Academy of Sleep Medicine defined nocturnal bruxism as a sleep-related movement disorder characterized by grinding or clenching of the teeth during sleep, usually associated with sleep arousal.10
Bruxism, as dystonia, is characterized by pain and exacerbated by fatigue, stress, and emotional extremes. Chronic bruxing often leads to abnormal wear on teeth, damaged bone and gum structures, oral or facial pain, headaches, tooth sensitivity, and potentially tooth loss.5,6 Although data are limited, bruxism appears to be more common in individuals with developmental disabilities, specifically, profound/severe mental retardation, autism spectrum disorders, and Down syndrome.11
In the general adult population, the prevalence based on the self-reporting of clenching of the teeth during waking hours is about 20%, whereas the prevalence of clenching during the sleeping hours is about 10% and that of grinding of the teeth during the sleeping hours ranges from 8% to 16%.12-15 Incidence of self-reported nocturnal bruxism in 4 large samples of college students increased from 5.1% to 22.5% over the period 1966-2002.16 Moreover, incidence appeared to be equally common in males and females but appears to occur more often in adults than in children.17 Traditionally, bruxism has been treated with mouth guards to prevent dental wear; but in several cases, mouth guards can increase the risk of wear of the temporomandibular joint and myofascial pain.6 Myofascial pain is described as a muscle hyperactivity involving facial pain related to temporomandibular disorders (TMDs), a craniofaciocervical dysfunction not completely understood.18,19 Usually, masseter and temporal muscle hyperactivity determines tension headaches and neck pain.20,21 Therefore, it was hypothesized that the temporal and masseter muscles could be involved into the pathogenesis of bruxism; so BTX-A can be used to decrease the hyperactivity of these muscles for reducing this condition.22-24
There are several reports in the literature, including a few randomized controlled studies (RCTs) and systematic reviews,11,25-27 of the favorable effect by botulinum toxin on craniofacial and neck pain as well as bruxism. However, the previous studies have not investigated the effect of botulinum toxin on neck pain caused by bruxism, only jaw pain due to bruxism or neck pain due to cervical dystonias.18-21,28 Because neck pain is commonly coexisting with craniofacial pain in TMD, this case report may be of interest. The following is a case report of a patient presenting with nocturnal bruxism with related neck pain and treated with BTX-A.
Case report
The patient in this case was a 27-year-old man with neck pain related to bruxism. Anamnesis was negative for whiplash injuries. The patient had complete dentition and no periodontal problems or acute inflammatory oral diseases. His wife reported hearing tooth-grinding sounds during the night. Therefore, the onset of this condition was unclear; but it was present at the age of 23 years, when he started to sleep with his wife. Moreover, this condition appeared spontaneously; but it worsened during stressful periods. When he got up, he had difficulty in active mouth opening and chewing with pain at 15° of mouth opening. He experienced neck pain at rest. Occasionally, this patient suffered from headaches in the temporal muscle region when he awakened in the morning. He was treated for 2 months with a benzodiazepine (lorazepam tablet 2 mg, 1 tablet per day at night), physiotherapeutic intervention, cranial manipulation, and a nocturnal mouth guard to alleviate bruxism symptoms, without positive results. The patient had joint sounds caused by masseter hyperactivity during the night that persisted also with the nocturnal mouth guard. Moreover, he had difficulties on awakening in the morning with this treatment with benzodiazepines, which was withdrawn.
Physical examination included palpation of the masticatory and neck muscles, palpation of the temporomandibular joint, examination of the oral cavity, assessment of the temporomandibular joint, and neck movements. At muscle palpation, the masseter and temporalis muscles were tender bilaterally. On voluntary contraction, he had masseter and temporalis hypertrophy, although no limitations of cervical range of motion were found. On the basis of the participant's self-report and the clinical oral examination, and using the diagnostic criteria proposed by the American Sleep Disorder Association29 and revised by the American Academy of Sleep Medicine,10 a nocturnal bruxism for this patient was diagnosed. In particular, the patient was aware of tooth-grinding sounds during sleep as reported by his wife; and also, the following criteria were present: jaw muscle pain and jaw lock upon awakening, and masseter muscle hypertrophy upon voluntary forceful clenching. Furthermore, jaw muscle activity was not better explained by another current sleep disorder, medical or neurologic disorder, or medication use or substance use disorder. Moreover, on a questionnaire for detecting bruxers (Fig 1),30 the patient gave a positive response to 3 of the 6 items presented (tooth-grinding sounds during sleep, jaw fatigued on awakening in the morning, and temporal headaches on awakening in the morning). Subjects who were classified as bruxers based on a history and clinical examination gave a positive response to at least 2 of the 6 items.30 Neck pain was measured with the numeric pain scale and scored 7 of 10 on a 10-cm horizontal axis between a left end point of “no pain” and a right end point of “worst pain ever.” Radiographic examination of the cervical spine was negative for anatomical alterations. Surface electromyography of the temporalis and masseter muscles showed typical signs of hyperactivity, characterized by compound muscle action potential amplitude alterations.
Fig 1.
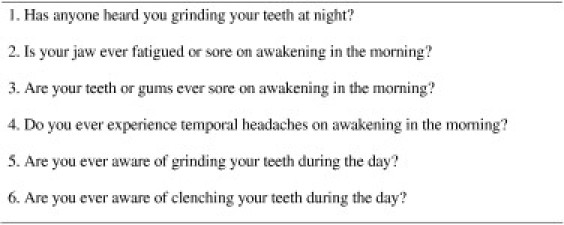
Questionnaire for detecting bruxers.30
After this clinical evaluation and after 2 months from the benzodiazepine withdrawal, he was treated with BTX-A to reduce masseter and temporal muscle hyperactivity. This combination can do more benefit than the masseter-only injections.20,21 Botulinum toxin type A was administered using specific guidelines as indicated in other reports.11 The dose of BTX-A (Xeomin; Merzpharma, Frankfurt, Germany) injected into each masseter muscle was 40 mouse units (MU) with a dilution of 1 mL, whereas 25 MU with the same dilution was injected into the temporalis muscles bilaterally. A 1-mL syringe and a 26-gauge needle was used, with 2 injection points. All injections were administered with electromyographic guidance. The injections were placed in the masseter muscles using the linear electronic probe Technos with 7.5 to 13 MHz (Esaote, Genoa, Italy) to avoid the injection into the parotid glands. The patient tolerated this procedure well. There was no evidence of muscle atrophy, jaw dislocation, or infection 3 days after injection.
The wife of the patient reported a decrease in his bruxism symptoms 3 days after treatment. On the questionnaire for detecting bruxers, the patient gave no positive response to the 6 items presented. The patient also reported that neck pain decreased after the first treatment (numeric pain scale score 2/10) and then resolved completely. A new electromyographic examination was repeated after 4 weeks to observe for the presence of chemical denervation as a consequence of the action of botulinum toxin. This interval was chosen because it is the mean time to observe electromyographic signs of denervation after nerve damage. An improvement was observed in the reduction of muscle hyperactivity with a decrease in the amplitude of the motor action potential related to the neuromuscular block caused by BTX-A. Assessment at 3 months posttreatment revealed that the clinical improvements were still present. The patient gave consent to have the details of his health condition published without including personal identifiers.
Discussion
In the present report, the clinical improvement of a 27-year-old man with nocturnal bruxism and related neck pain after a treatment of BTX-A injections in the masseter and temporal muscles bilaterally was described. Bruxism involves jaw clenching and grinding of the teeth, commonly causes myofascial pain, and is often resistant to treatment.
The etiology and neurologic mechanisms that generate nocturnal bruxism are not well understood. The 3 major hypothesized causes of nocturnal bruxism are neurologic factors, peripheral stimulus, and psychogenic elements.6 In the past, morphologic factors, such as occlusal discrepancies and deviations in the anatomy of the bony structures of the orofacial region, have been considered the main causative factors for bruxism.31 During the past decade, however, a number of studies have demonstrated the major role played by central factors in the development of nocturnal bruxism32,33; and a growing body of evidence suggests that it appears to be induced within the central nervous system and, in part, is associated with the phenomenon of arousal reactions during sleep.32 Several studies have shown that changes in the input feedback of peripheral oral receptors (eg, alternation in the occlusal contact relationship and an increased vertical dimension) temporarily diminish, but do not stop, bruxism.31 In addition, bruxism appears to be modulated by various neurotransmitters in the central nervous system. More specifically, disturbances in the central dopaminergic system have been described in relation to bruxism. Furthermore, factors like medication (eg, l-3,4-dihydroxyphenylalanine, selective serotonin reuptake inhibitors, propranolol),6 (illicit) drugs, genetics, trauma, and neurologic and psychiatric diseases may be involved in the etiology of bruxism.31 Psychosocial factors such as stress and personality are frequently mentioned in relation to bruxism as well. However, research into these factors comes to equivocal results and needs further attention. Taking all of the evidence together, nocturnal bruxism seems to be mainly regulated centrally, not peripherally. Diurnal bruxism should be differentiated from nocturnal bruxism because the 2 conditions occur under different circumstances. Diurnal bruxism, which mainly consists of clenching, is acquisitive behavior.6
Published studies concerning BTX-A treatment of bruxism describe successful treatment of bruxism associated with TMD or traumatic brain injury.23,28 Usually, bruxism and other TMDs are associated with neck and myofascial pain20,21 with muscle hyperactivity without specific anatomical modification. Among the jaw elevator muscles, the masseter and temporalis muscles are those most often assessed in clinical evaluations and injected with BTX-A, with great clinical success. The reduction of muscle hyperactivity may determine a reduction of tension in all cervical muscles and pain relief because the stomatognathic apparatus is composed of all of the head and upper cervical structures pertaining to the digestive apparatus, including the oral cavity, the teeth and supporting bones and gingivae, the tongue, the salivatory glands, the pharynx, the masticatory muscles, and the temporomandibular joint. In fact, the mandibular and neck muscles act as an integrated structure; and alterations in one part can derange other ones.34-37 In most of the studies we reviewed, BTX-A was found to be efficacious without adverse effects if correctly injected. The injections in masseter and temporal muscles were preferable to obtain a greater effect than masseter muscle treatment alone. Usually, the dose ranged from 25 to 50 MU with 1 mL dilution in 2 to 3 sites of injections to avoid the diffusion and weakness in surrounding muscles not injected.38
Various treatment modalities have been reported to be useful for bruxism and related disorders,39-46 but there is no general agreement as to what is the best therapeutic option. Other intervention approaches to bruxism and associated TMD include drugs,39,40 prosthodontics, dental surgery, and behavior modification.11,41 Physical therapy modalities including exercise interventions (isokinetic stretching exercises and mandibular exercises),42,43 manual therapy,44 and electrophysical modalities (shortwave diathermy, ultrasound, low-intensity laser therapy, biofeedback training, muscular awareness relaxation therapy, and transcutaneous electrical stimulation).44 Chiropractic care (temporomandibular joint mobilization, myofascial therapy, trigger point therapy, and cranial manipulation)45,46 may also provide conservative management of TMD.
Limitations
Some limitations in this study have to be considered. In fact, a polysomnograph in a sleep laboratory, currently considered as the most specific and accurate method for evaluating bruxism activity,47,48 was not performed for this patient. Moreover, as for any case report, the findings may have been due to the natural history of the condition, concurrent life events, other treatment modalities used by the patient in the same period, etc. In addition, it was not clear if the patient's neck pain was causally related to his bruxism. The 2 conditions could be also only coincidental.
Conclusion
The treatment of bruxism and TMD could be another use for the ever-expanding possible indications for BTX-A. Nonetheless, large randomized controlled trials on BTX-A treatment of bruxism and related disorders are needed to create guidelines for dosages, dilutions, muscles, and sites of injections and to determine more conclusively that this treatment modality is effective in treating neck pain related to bruxism.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
References
- 1.Jankovic J., Schwartz K., Donovan D.T. Botulinum toxin treatment of cranial-cervical dystonia, spasmodic dysphonia, other focal dystonias and hemifacial spasm. J Neurol Neurosurg Psychiatry. 1990;53:633–639. doi: 10.1136/jnnp.53.8.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naumann M., So Y., Argoff C.E., Childers M.K., Dykstra D.D., Gronseth G.S. Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Assessment: botulinum neurotoxin in the treatment of autonomic disorders and pain (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2008;70:1707–1714. doi: 10.1212/01.wnl.0000311390.87642.d8. [DOI] [PubMed] [Google Scholar]
- 3.Santamato A., Ianieri G., Ranieri M., Megna M., Panza F., Fiore P. Botulinum toxin type A in the treatment of sialorrhea in Parkinson's disease. J Am Geriatr Soc. 2008;56:765–767. doi: 10.1111/j.1532-5415.2008.01612.x. [DOI] [PubMed] [Google Scholar]
- 4.Santamato A., Panza F., Solfrizzi V., Frisardi V., Ranieri M., Fiore P. Botulinum toxin type A and type B for sialorrhoea in Parkinson's disease: a case for switching therapy? J Rehabil Med. 2008;40:882–883. doi: 10.2340/16501977-0257. [DOI] [PubMed] [Google Scholar]
- 5.Clark G.T., Ram S. Four oral motor disorders: bruxism, dystonia, dyskinesia and drug-induced dystonic extrapyramidal reactions. Dent Clin North Am. 2007;51:225–243. doi: 10.1016/j.cden.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Koyano K., Tsukiyama Y., Ichiki R., Kuwata T. Assessment of bruxism in the clinic. J Oral Rehabil. 2008;35:495–508. doi: 10.1111/j.1365-2842.2008.01880.x. [DOI] [PubMed] [Google Scholar]
- 7.Nadler S.C. Bruxism, a classification: critical review. J Am Dent Assoc. 1957;54:615–622. doi: 10.14219/jada.archive.1957.0097. [DOI] [PubMed] [Google Scholar]
- 8.Attanasio R. Intraoral orthotic therapy. Dent Clin North Am. 1997;41:309–324. [PubMed] [Google Scholar]
- 9.The Academy of Prosthodontics The glossary of prosthodontic terms, eighth edition (GPT-8) J Prosthet Dent. 2005;94:1–92. [Google Scholar]
- 10.AASM . 2nd ed. American Academy of Sleep Medicine; Westchester: 2005. International classification of sleep disorders. [Google Scholar]
- 11.Lang R., White P.J., Machalicek W., Rispoli M., Kang S., Aquilar J. Treatment of bruxism in individuals with developmental disabilities: a systematic review. Res Dev Disabil. 2009;30:809–818. doi: 10.1016/j.ridd.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Lavigne G.J., Montplaisir J.Y. Restless legs syndrome and sleep bruxism: prevalence and association among Canadians. Sleep. 1994;17:739–743. [PubMed] [Google Scholar]
- 13.Ohayon M.M., Li K.K., Guilleminault C. Risk factors for sleep bruxism in the general population. Chest. 2001;119:53–61. doi: 10.1378/chest.119.1.53. [DOI] [PubMed] [Google Scholar]
- 14.Carlsson G.E., Egermark I., Magnusson T. Predictors of bruxism, other oral parafunctions, and tooth wear over a 20-year follow-up period. J Orofac Pain. 2003;17:50–57. [PubMed] [Google Scholar]
- 15.Redding G.R., Rubright W.C., Zimmerman S.O. Incidence of bruxism. J Dent Res. 1966;45:1198–1204. doi: 10.1177/00220345660450042701. [DOI] [PubMed] [Google Scholar]
- 16.Granada S., Hicks R.A. Changes in self-reported incidence of nocturnal bruxism in college students: 1966-2002. Percept Mot Skills. 2003;97(3 Pt 1):777–778. doi: 10.2466/pms.2003.97.3.777. [DOI] [PubMed] [Google Scholar]
- 17.Glaros A.G., Rao S.M. Bruxism: a critical review. Psychol Bull. 1977;4:767–781. doi: 10.1037/0033-2909.84.4.767. [DOI] [PubMed] [Google Scholar]
- 18.de Wijer A., Steenks M.H., Bosman F., Helders P.J.M., Faber J. Symptoms of the stomatognathic system in temporomandibular and cervical spine disorders. J Oral Rehabil. 1996;23:733–741. doi: 10.1046/j.1365-2842.1996.00427.x. [DOI] [PubMed] [Google Scholar]
- 19.Watts M.W., Tan E.K., Jankovic J. Bruxism and cranial-cervical dystonia: is there a relationship? Cranio. 1999;17:196–201. doi: 10.1080/08869634.1999.11746095. [DOI] [PubMed] [Google Scholar]
- 20.Molina O.F., Dos Santos J., Jr, Nelson S.J., Grossman E. Prevalence of modalities of headaches and bruxism among patients with craniomandibular disorder. Cranio. 1997;15:314–325. doi: 10.1080/08869634.1997.11746026. [DOI] [PubMed] [Google Scholar]
- 21.Ciancaglini R., Gherlone E.F., Radaelli G. The relationship of bruxism with craniofacial pain and symptoms from the masticatory system in the adult population. J Oral Rehabil. 2001;28:842–848. doi: 10.1046/j.1365-2842.2001.00753.x. [DOI] [PubMed] [Google Scholar]
- 22.Tan E.K., Jankovic J. Treating severe bruxism with botulinum toxin. J Am Dent Assoc. 2000;131:211–216. doi: 10.14219/jada.archive.2000.0149. [DOI] [PubMed] [Google Scholar]
- 23.Van Zandijcke M., Marchau M.M. Treatment of bruxism with botulinum toxin injections. J Neurol Neurosurg Psychiatry. 1990;53:530. doi: 10.1136/jnnp.53.6.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chikhani L., Dichamp J. Bruxism, temporo-mandibular dysfunction and botulinum toxin. Ann Readapt Med Phys. 2003;46:333–337. doi: 10.1016/s0168-6054(03)00115-6. [DOI] [PubMed] [Google Scholar]
- 25.Guarda-Nardini L., Manfredini D., Salamone M., Salmaso L., Tonello S., Ferronato G. Efficacy of botulinum toxin in treating myofascial pain in bruxers: a controlled placebo pilot study. Cranio. 2008;26:126–135. doi: 10.1179/crn.2008.017. [DOI] [PubMed] [Google Scholar]
- 26.Lee S.J., McCall W.D., Jr, Kim Y.K., Chung S.C., Chung J.W. Effect of botulinum toxin injection on nocturnal bruxism: a randomized controlled trial. Am J Phys Med Rehabil. 2010;89:16–23. doi: 10.1097/PHM.0b013e3181bc0c78. [DOI] [PubMed] [Google Scholar]
- 27.Ihde S.K., Konstantinovic V.S. The therapeutic use of botulinum toxin in cervical and maxillofacial conditions: an evidence-based review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e1–e11. doi: 10.1016/j.tripleo.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz M., Freund B. Treatment of temporomandibular disorders with botulinum toxin. Clin J Pain. 2002;18(6 Suppl):S198–S203. doi: 10.1097/00002508-200211001-00013. [DOI] [PubMed] [Google Scholar]
- 29.American Sleep Disorders Association . Parasomnia. In: Thorpy M.J., editor. International classification of sleep disorders: diagnostic and coding manual. ASDA; Rochester (Minn): 1990. pp. 142–185. [Google Scholar]
- 30.Pintado M.R., Anderson G.C., DeLong R., Douglas W.H. Variation in tooth wear in young adults over a two-year period. J Prosthet Dent. 1997;77:313–320. doi: 10.1016/s0022-3913(97)70189-6. [DOI] [PubMed] [Google Scholar]
- 31.Lobbezoo F., Van Der Zaag J., Naeije M. Bruxism: its multiple causes and its effects on dental implants—an updated review. J Oral Rehabil. 2006;33(4):293–300. doi: 10.1111/j.1365-2842.2006.01609.x. [DOI] [PubMed] [Google Scholar]
- 32.Kato T., Thie N.M., Huynh N., Miyawaki S., Lavigne G.J. Topical review: sleep bruxism and the role of peripheral sensory influences. J Orofac Pain. 2003;17:191–213. [PubMed] [Google Scholar]
- 33.Lavigne G.J., Khoury S., Abe S., Yamaguchi T., Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35:476–494. doi: 10.1111/j.1365-2842.2008.01881.x. [DOI] [PubMed] [Google Scholar]
- 34.Ivanhoe C.B., Lai J.M., Francisco G.E. Bruxism after brain injury: successful treatment with botulinum toxin-A. Arch Phys Med Rehabil. 1997;78:1272–1273. doi: 10.1016/s0003-9993(97)90343-9. [DOI] [PubMed] [Google Scholar]
- 35.Ferrario V.F., Tartaglia G.M., Galletta A., Grassi G.P., Sforza C. The influence of occlusion on jaw and neck muscle activity: a surface EMG study in healthy young adults. J Oral Rehabil. 2006;33:341–348. doi: 10.1111/j.1365-2842.2005.01558.x. [DOI] [PubMed] [Google Scholar]
- 36.Ferrario V.F., Tartaglia G.M., Luraghi F.E., Sforza C. The use of surface electromyography as a tool in differentiating temporomandibular disorders from neck disorders. Man Ther. 2007;12:372–379. doi: 10.1016/j.math.2006.07.013. [DOI] [PubMed] [Google Scholar]
- 37.Eriksson P.O., Zafar H., Häggman-Henrikson B. Deranged jaw-neck motor control in whiplash-associated disorders. Eur J Oral Sci. 2004;112:25–32. doi: 10.1111/j.0909-8836.2004.00098.x. [DOI] [PubMed] [Google Scholar]
- 38.Bhidayasiri R., Cardoso F., Truong D.D. Botulinum toxin in blepharospasm and oromandibular dystonia: comparing different botulinum toxin preparations. Eur J Neurol. 2006;13(Suppl 1):21–29. doi: 10.1111/j.1468-1331.2006.01441.x. [DOI] [PubMed] [Google Scholar]
- 39.Lobbezoo F., Lavigne G.J., Tanguay R., Montplaisir J.Y. The effect of catecholamine precursor l-DOPA on sleep bruxism: a controlled clinical trial. Mov Disord. 1997;12:73–78. doi: 10.1002/mds.870120113. [DOI] [PubMed] [Google Scholar]
- 40.Mohamed S.E., Christensen L.V., Penchas J. A randomized double-blind clinical trial of the effect of amitriptyline on nocturnal masseteric motor activity (sleep bruxism) Cranio. 1997;15:326–332. doi: 10.1080/08869634.1997.11746027. [DOI] [PubMed] [Google Scholar]
- 41.Thompson B.A., Blount B.W., Krumholz T.S. Treatment approaches to bruxism. Am Fam Physician. 1994;49:1617–1622. [PubMed] [Google Scholar]
- 42.Lewit K., Simons D.G. Myofascial pain: relief by post-isometric relaxation. Arch Phys Med Rehabil. 1984;65:452–456. [PubMed] [Google Scholar]
- 43.Quinn J.H. Mandibular exercises to control bruxism and deviation problems. Cranio. 1995;13:30–34. doi: 10.1080/08869634.1995.11678039. [DOI] [PubMed] [Google Scholar]
- 44.McNeely M.L., Armijo Olivo S., Magee D.J. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther. 2006;86:710–725. [PubMed] [Google Scholar]
- 45.Houle S., Descarreaux M. Conservative care of temporomandibular joint disorder in a 35-year-old patient with spinal muscular atrophy type III: a case study. J Chiropr Med. 2009;8:187–192. doi: 10.1016/j.jcm.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Babadağ M., Sahin M., Görgün S. Pre- and posttreatment analysis of clinical symptoms of patients with temporomandibular disorders. Quintessence Int. 2004;35:811–814. [PubMed] [Google Scholar]
- 47.Bowley J.F., Stockstill J.W., Pierce C.J. Reliability and validity of instrumentation used to record nocturnal clenching and ⁄or grinding. J Orofac Pain. 1993;7:378–385. [PubMed] [Google Scholar]
- 48.Gallo L.M., Lavigne G., Rompré P., Palla S. Reliability of scoring EMG orofacial events: polysomnography compared with ambulatory recordings. J Sleep Res. 1997;6:259–263. doi: 10.1111/j.1365-2869.1997.00259.x. [DOI] [PubMed] [Google Scholar]


