Abstract
Addiction coopts the brain’s neuronal circuits necessary for insight, reward, motivation, and social behaviors. This functional overlap results in addicted individuals making poor choices despite awareness of the negative consequences; it explains why previously rewarding life situations and the threat of judicial punishment cannot stop drug taking and why a medical rather than a criminal approach is more effective in curtailing addiction.
Introduction
Substance use disorders (SUD) profoundly affect our society. Though the costs are usually translated in economic terms—approximately half a trillion dollars a year in the USA (ONDCP, 2004)—their impact is much more insidious, eroding the foundation of human relationships and the established social contract. Thus, it is not surprising that a significant portion of costs associated with SUD stems from costs associated with antisocial or criminal behavior and family services. The following letter excerpt (bold added for emphasis) painfully illustrates the devastation that SUD can bring upon individuals, their families, and society.
As I sit to compose this plea I can’t say with any amount of certainty that my son is alive. My son discovered narcotics at the age of 13. He experienced a severe orthopedic sports injury. There seems to be nothing that can induce him to stop for any appreciable length of time. I had him arrested May of 2006 for heroin possession and identity fraud, he stole 900 dollars from our checking account while I was in Connecticut burying my dad and his sister… tells me he cannot stop… Our family is being destroyed … we have exhausted our savings and retirement. Everything seems so hopeless…
Research on the neuroscience of SUD has started to shed light on the ways in which chronic drug abuse changes the brain to cause the profound disruption we see in the behavior of an addicted person. This is because drugs of abuse impact many neuronal circuits that are crucial for proper functioning in social environments. These changes are long-lasting, persisting even after years of drug discontinuation, which has led to the recognition of addiction as a chronic and relapsing disease, as illustrated by another letter excerpt.
I am a 42 year old male who has struggled with addiction to alcohol/drugs for almost two decades but I have also struggled with trying to find a way out of active addiction. My attempts have included about 15 stays at rehabilitation centers, numerous detoxification units, a stay at a long-term rehabilitation center, religion, philosophy, behavior modification and finally a 12 step program…. My life can be summed-up as a life of many failed attempts. Failed attempts in a lot of areas and I believe it is because I have not been able to stop abusing alcohol.
Addiction has a strong genetic component and both developmental stages (adolescents and young adults being at the highest risk for SUD) and environmental factors (e.g., exposure to stressful environments) play crucial roles in modulating the vulnerability for SUD in part through their influence on how the human brain works and responds and adapts to various types of stimuli (including drugs). Scientific insights into drug-induced impairments of specific brain circuits are beginning to answer many of the questions that had baffled us for so long, such as (1) why drugs can be so disruptive to social relationships, (2) why the social system used to deter behavior (e.g., the threats of incarceration or of loss of custody) does not work well in addicted subjects, (3) why social stressors (such as those that may be triggered by poverty) increase vulnerability for addictions, and (4) how to best harness the new information for the development of more effective prevention and treatment alternatives. Fundamental processes to addiction are the enhanced motivational drive for the drug and the weakening of control over this drive.
What’s Important to Addicts: Placing Value in All the Wrong Places
People’s ability to successfully identify, seek, and obtain what is important to them (but also avoid what’s undesirable) at a particular point in time is crucial for their well-being. That which motivates us toward obtaining certain goals plays a key role in how successfully we navigate complex social environments. The sinister nature of addiction is that the very neurobiological systems underpinning this process become dysfunctional, hijacked by a user’s drug (or drugs) of choice. From a biological perspective, this is believed to reflect the ability of chronic drug exposure to cause neuroadaptations in brain reward systems including the emergence of conditioned associations that link the rewarding experience from the drug to the multiple cues that surround it (Kalivas and Volkow, 2005).
The same functional impairments that make the reward pathways of an addicted individual more responsive to the abused drug and its associated cues (Volkow et al., 2009) also reduce their sensitivity to previously effective natural nondrug reinforcers, such as spending time with friends or family. The intrinsically high rewarding properties of drugs of abuse combined with their relatively weak potential for satiety (Acquas and Di Chiara, 1992) trigger neuroadaptations that ultimately make drug searching and consumption the main motivational drive for addicted individuals. As a result, in addicted subjects, the reward value of the drug of abuse and its associated cues is enhanced, whereas that of other reinforcers is markedly decreased (Volkow et al., 2003) (Figure 1). Ultimately, this leads to a cycle of drug abuse that is difficult to break free of, even when an addict may truly want to become drug-free, resulting in the typical pattern of drug relapse so often seen in addicted individuals.
Figure 1. Model Proposing a Network of Four Circuits Involved with Addiction: Reward, Motivation/Drive, Memory, and Control.
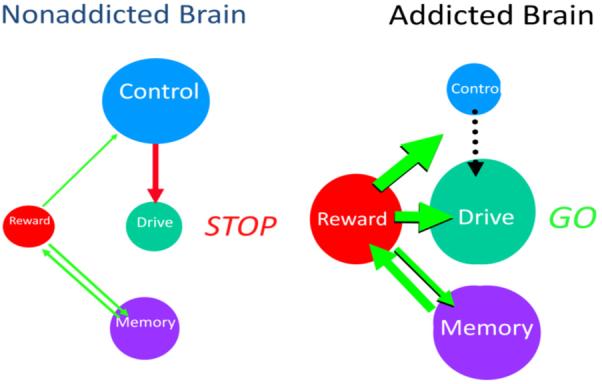
These circuits work together and change with experience. Each is linked to an important concept: reward (value of positive and negative reinforcers), drive (incentive motivation), memory (learned associations/ conditioning), and control (conflict resolution). During addiction, the enhanced value of the drug in the reward, motivation, and memory circuits overcomes the inhibitory control exerted by the prefrontal cortex, thereby favoring a positive-feedback loop initiated by the consumption of the drug and perpetuated by the enhanced activation of the motivation/drive and memory circuits (reprinted with permission [Volkow et al., 2003]).
Furthermore, while the value that an addicted individual places on drug reward becomes unsustainably exaggerated, the potential impact of deleterious consequences (e.g., familial dislocation, becoming the target of drug-related violence, or incarceration) becomes progressively devalued. The establishment of such a severe imbalance in how an addicted individual attributes value to both rewarding and aversive situations and stimuli has a profound and negative impact on the individual’s social competence. Their behaviors are now governed by the uncontrollable overvaluing of the drug and by a growing insensitivity to the deterrent value of potential punishments. The problem is further compounded by the tendency of many substance abusers, more so than nonusers, to routinely choose immediate rewards over delayed gratification (e.g., choose $20 dollars now rather than wait 1 week in order to get double that amount). This inability to appropriately weigh delayed rewards can be devastating to an addicted person who may be willing to sacrifice future gains or incur major losses in exchange for instant gratification. An individual in this situation may not think twice about the risk of losing his or her parole tomorrow in order to chase the high from the drug now.
This knowledge helps explain why the prevailing social system that dangles some future threat of imprisonment over an addict’s head does not work well in deterring immediate substance abuse-related behaviors in addicted subjects. It also highlights the need to provide addicted individuals with alternative reinforcers as a strategy both for the prevention of SUD as well as its treatment.
When Both Steering and Braking Systems Fail: Cognitive Function and Impulse Control Derailed
For many years, studies of addiction focused on the role of brain reward circuitry (Weiss and Koob, 2001). However, imaging studies have provided consistent evidence for the involvement of the brain’s cognitive system as well (i.e., prefrontal cortex [PFC]) in the addiction process (Volkow and Fowler, 2000). Both preclinical and clinical studies have explored the complex role that disrupted cognitive processing plays in the addiction cycle. In addition to the involvement of the PFC in classical cognitive operations, more recent work has also revealed that the PFC plays a crucial role in social cognition (Forbes and Grafman, 2010), which is necessary for proper social integration. For example, damage to ventral areas of this brain region can interfere with the ability of a person to accurately distinguish right from wrong in a socially acceptable manner, which can lead to socially inappropriate behaviors (Koenigs et al., 2007). Because the functions of these brain regions are also impaired in addicted individuals, this could explain an addict’s inability to accurately steer their behaviors in appropriate directions despite having access to the required knowledge.
Behavioral inhibition is fundamental to the success of social intercourse, which is critically dependent on a person’s ability to control impulsive behaviors whenever this is needed. It is therefore interesting to note that impaired impulse behavior, which is also dependent on the PFC, is another key symptom of addictive individuals. For most people, the combination of biological (e.g., individual-level characteristics) and environmental (e.g., culture, laws, religion) factors build up a sufficiently robust mechanism to inhibit or at least help manage internally or externally generated temptations. But the system is not fail-safe and some individuals at one extreme of the impulsivity distribution curve, as is the case in addiction, are the constant victims of very powerful, unstoppable urges. By perturbing the function of the PFC, the addiction process degrades the very substrates that enable an individual to exert free will. There is no doubt that the impaired function of neuronal systems involved in social behaviors in addicted individuals contributes to the stigma associated with SUD.
Social Stressors and Addiction
Lingering economic uncertainty, social dislocation, isolation, inequalities, and the ubiquitous threat of global terrorism are just a few examples of modern life’s steady diet of stressful stimuli that could exacerbate the risk of mental illness including SUD. Stress systems greatly contribute to the addiction cycle of drug craving and withdrawal, pushing the addicted individual toward compulsive drug taking (Koob and Zorrilla, 2010). Indeed, epidemiological studies have shown a direct dose-dependent relationship between the number and type of adverse childhood experiences (ACE) and early initiation of drug use (Dube et al., 2003). Such ACEs appear to explain at least half of the risk for SUD later in life.
Of particular interest for neuroscience research has been the role of social stressors in SUD. For example, in non-human primates stressful alterations in an animal’s social environment disrupted their expression of dopamine D2 receptors (D2R) in striatum and increased their subsequent propensity for drug use (Morgan et al., 2002). Similarly, imaging studies in humans have documented an inverse relationship between social status and striatal D2R expression (Martinez et al., 2010). This is relevant because both preclinical and clinical studies have shown that low striatal D2R expression is associated with impulsivity and propensity for compulsive drug use. Indeed, one of the most replicated findings from imaging studies of addiction is that of reduced striatal D2R levels (Volkow et al., 2009). Hence, one possible mechanism through which social stressors might enhance the risk for drug use could involve the downregulation of striatal dopamine signaling.
Social stressors have also been shown to have a deleterious impact on the developmental processes that connect the PFC with the limbic brain (including the amygdala, which processes emotions and stress reactivity) and that are indispensable for the establishment of cognitive control of emotions and desires. For example, children reared in an orphanage showed a delayed connectivity in these pathways that was proportional to the years they spent at that institution (Behen et al., 2009).
The fact that stressful stimuli and environments can exert such negative and long-lasting effects on the formation and function of the brain substrates responsible for protecting us against drug abuse and addiction (among others) should make us pause and rethink our prevention strategies. For example, should we consider how the enhanced stress of having an incarcerated parent may affect the risk for drug use in the children of incarcerated drug abusers or consider the neurobiological consequences of incarceration in the drug abuser and how this will affect their ability to recover once released into their communities?
Implications for Treatment and Social Policy
As we’ve discussed above, addiction involves persistent drug-induced adaptations in the brain systems responsible for controlling behaviors that are necessary for proper integration into complex social systems. Hence, therapeutic interventions should take this into consideration and create incentives for the substance abusers to engage and stay in treatment including strategies that help strengthen social ties with family and community. Social interactions are powerful reinforcers that can provide the addicted individual with alternatives to help counteract the perceived high-reward value of drugs.
An important consequence of the longterm brain adaptations is that most addicted patients will require a long period of treatment, during which relapse is likely to occur, which should be considered a predictable setback and not a failure of the treatment. This also explains why the best treatment outcomes are reported by programs that offer continuity of care for a 5-year period (McLellan et al., 2008). In addition, chronic drug abuse has recently been recognized to be associated with impaired self-awareness (including interoceptive or bodily awareness), which manifests as compromised recognition of disease severity and/or the need for treatment, but that has frequently been interpreted as denial (Goldstein et al., 2009). This in turn contributes to the low rates of treatment initiation and high-dropout rates.
According to the 2010 National Survey on Drug Use and Health (NSDUH) (SAMHSA, 2010), in 2009, 22.5 million persons aged 12 or older needed treatment for an illicit drug or alcohol use problem, but only 2.6 million received treatment at a specialty facility. This means that 20.9 million persons who needed treatment did not get it. The reason for such high undertreatment rates is instructive: the vast majority of addicts did not even perceive a need for treatment and among those who did admit needing treatment over half either didn’t make any effort to seek it or were unable to procure it. The persistence of such a vast SUD treatment gap—the result of a combination of inadequate infrastructure and lack of interest—is a great concern because it continues in spite of the availability of effective interventions.
The disconnect that exists between treatment needs and access is even more apparent in the context of criminal justice system populations. The fact is that most prisoners (80%–85%) who could benefit from drug abuse treatment do not receive it (Mumola and Karberg, 2006). This is a missed opportunity because integrating treatment into the criminal justice system would enable us to provide treatment to individuals who otherwise would neither seek nor receive it, and it has been shown to improve medical outcomes and reduce recidivism particularly when maintained throughout the critical postrelease period (Chandler et al., 2009). This is because returning to a neighborhood awash with so many drug-associated cues can trigger powerful cravings and relapse to compulsive drug-seeking behaviors. This is further compounded by the systemic difficulties and stressors these individuals face when reintegrating into society, including that of finding a job while under the shadow of a criminal record. This is vividly illustrated by the following letter.
I am writing as the mother of a crack addict. My daughter has been an addict for 12 years. She is the mother of 4 children all of which she has lost parental rights to. She has been in prison most of the 12 years, and had many programs, doing well in what was offered during incarceration. When she is released from prison, she is always hopeful for success…. She is immediately faced with 4 major challenges: getting a place to live, finding a job, transportation, and obtaining continuing recovery treatment…. Now she just got [out] of jail 3 weeks ago, went through what I just described above, and went back on the streets. She was broke and shop-lifting, and now will go back to jail, do the program for probably the 10th time, and be released again the same way. There are many like my daughter, so addicted they will end up dead.
Forward-Looking Agenda
I wonder how many times my son has left in him. Is there any hope for the alcoholic/addict who has reached bottoms so deep and so dark that it is hard to imagine that there is any place left to go? That there is anything left to lose. When there are no more resources, no money, no free treatment options that are available during the unending crisis—what then? When a bright, educated man can no longer work because of his addiction, where do we turn? I ask because I have done everything and I have done nothing and neither strategy has worked.
Social isolation is not only a marker but a well-recognized risk factor of physical and mental illness (Karelina and DeVries, 2011). Yet, by most accounts, stigmatization and/or incarceration have been society’s prevailing responses to addicted individuals. Such stigmatization impedes the search for treatment and further isolates addicted individuals and their families.
The ideas expressed here could be easily construed as advocating a sort of moral relativism at the expense of individual responsibility. Yet nothing could be farther from the truth. We merely state the fact that addiction is a brain disorder that impacts the very same circuits that enable self-monitoring and complex social functioning. Granted, our understanding of the brain systems whose function or dysfunction shape subjective value and decision-making and how drugs affect them is still incomplete. Nonetheless, the recognition that social stressors such as stigma and isolation can further impair the function of neuronal systems necessary for an addicted person’s recovery highlights the need to treat addiction as a disease rather than as a criminal behavior.
ACKNOWLEDGMENTS
The authors wish to recognize and thank the anonymous relatives and addicted individuals who, in their search for an answer to their problem, wrote the poignant letters.
REFERENCES
- Acquas E, Di Chiara G. J. Neurochem. 1992;58:1620–1625. doi: 10.1111/j.1471-4159.1992.tb10033.x. [DOI] [PubMed] [Google Scholar]
- Behen ME, Muzik O, Saporta AS, Wilson BJ, Pai D, Hua J, Chugani HT. Brain Imaging Behav. 2009;3:292–297. doi: 10.1007/s11682-009-9071-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler RK, Fletcher BW, Volkow ND. JAMA. 2009;301:183–190. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube SR, Felitti VJ, Dong M, Chapman DP, Giles WH, Anda RF. Pediatrics. 2003;111:564–572. doi: 10.1542/peds.111.3.564. [DOI] [PubMed] [Google Scholar]
- Forbes CE, Grafman J. Annu. Rev. Neurosci. 2010;33:299–324. doi: 10.1146/annurev-neuro-060909-153230. [DOI] [PubMed] [Google Scholar]
- Goldstein RZ, Craig AD, Bechara A, Garavan H, Childress AR, Paulus MP, Volkow ND. Trends Cogn. Sci. (Regul. Ed.) 2009;13:372–380. doi: 10.1016/j.tics.2009.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalivas PW, Volkow ND. Am. J. Psychiatry. 2005;162:1403–1413. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- Karelina K, DeVries AC. Psychosom. Med. 2011;73:67–74. doi: 10.1097/PSY.0b013e3182002116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenigs M, Young L, Adolphs R, Tranel D, Cushman F, Hauser M, Damasio A. Nature. 2007;446:908–911. doi: 10.1038/nature05631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF, Zorrilla EP. Curr. Opin. Investig. Drugs. 2010;11:63–71. [PMC free article] [PubMed] [Google Scholar]
- Martinez D, Orlowska D, Narendran R, Slifstein M, Liu F, Kumar D, Broft A, Van Heertum R, Kleber HD. Biol. Psychiatry. 2010;67:275–278. doi: 10.1016/j.biopsych.2009.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Skipper GS, Campbell M, DuPont RL. BMJ. 2008;337:a2038. doi: 10.1136/bmj.a2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan D, Grant KA, Gage HD, Mach RH, Kaplan JR, Prioleau O, Nader SH, Buchheimer N, Ehrenkaufer RL, Nader MA. Nat. Neurosci. 2002;5:169–174. doi: 10.1038/nn798. [DOI] [PubMed] [Google Scholar]
- Mumola C, Karberg J. Drug Use and Dependence, State and Federal Prisoners, 2004. Office of Justice Programs, Bureau of Justice Statistics; Washington, DC: 2006. Dept of Justice publication NCJ 213530. [Google Scholar]
- ONDCP . The economic costs of drug abuse in the United States. W. Executive Office of the President Office of National Drug Control Policy; 2004. http://www.ncjrs.gov/ondcppubs/publications/pdf/economic_costs.pdf, ed. [Google Scholar]
- SAMHSA Results from the 2009 National Survey on Drug Use and Health: National Findings. 2010 http://oas.samhsa.gov/NSDUH/2k9NSDUH/2k9ResultsP.pdf.
- Volkow ND, Fowler JS. Cereb. Cortex. 2000;10:318–325. doi: 10.1093/cercor/10.3.318. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ. J. Clin. Invest. 2003;111:1444–1451. doi: 10.1172/JCI18533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ, Baler R, Telang F. Neuropharmacology. 2009;56(Suppl 1):3–8. doi: 10.1016/j.neuropharm.2008.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss F, Koob GF. Neurotox. Res. 2001;3:145–156. doi: 10.1007/BF03033235. [DOI] [PubMed] [Google Scholar]


