Abstract
Abuse of drugs by pregnant women both in the United States and worldwide has raised many questions regarding the effects of prenatal drug exposure on the developing fetus and subsequent child outcomes. Studies using the neurobehavioral teratology model have been undertaken to determine specific prenatal drug effects on cognitive and behavioral development. Here we summarize the findings of studies that have investigated the developmental effects of prenatal exposure to tobacco, marijuana, stimulants, and opiates. These studies consider the timing and amount of prenatal exposure; other drug exposures; maternal characteristics; and other health, nutritional, and environmental factors. We review treatment options for pregnant, substance-dependent women and therapeutic interventions for exposed children.
Several well-designed and methodologically sound studies have described long-term effects of specific prenatal drug exposures on children’s health and development. Some longitudinal studies now extend into late adolescence and early adulthood and assess vulnerability to substance abuse and dependence.
The psychoactive substances widely used by women of childbearing age include alcohol, tobacco, marijuana, stimulants, and opioids. Here we summarize current knowledge of the effects of prenatal exposure to each of these drugs, except alcohol. The extensive research on prenatal alcohol exposure has been reviewed elsewhere (Manji et al., 2009; O’Connor and Paley, 2009; Paley and O’Connor, 2009). We also discuss promising findings from trials of interventions to help pregnant and postpartum substance-abusing women and prenatally drug-exposed children.
A MODEL FOR INVESTIGATION: NEUROBEHAVIORAL TERATOLOGY
The conceptual framework used to study prenatal drug exposure is neurobehavioral teratology, which addresses the impact of prenatal exposure to a foreign agent on a child’s central nervous system (CNS) and behavior. An important principle of teratology is that the harm caused by a toxic agent is a function of several factors, including the individual’s genetic makeup, the fetal and postnatal environment, the dose of the agent, and the developmental stage of the fetus at the time of exposure. Vorhees (1989) has added two specific neurobehavioral tenets:
Damage to the CNS during the prenatal period continues to have effects through fetal, neonatal, infant, and childhood development; and
CNS injury may result in behavioral impairments rather than physical birth defects.
Drug metabolites interact with an individual’s genetic makeup to influence cognitive development and behavior.
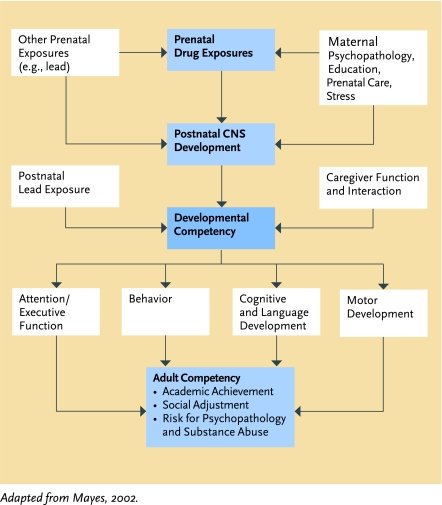
Mayes (2002) developed a model for neurobehavioral teratology research that highlights the direct and indirect effects of prenatal drug exposure and the ongoing reciprocal influences of CNS disruption, maternal characteristics, and environmental factors (Figure 1).
FIGURE 1.
Model to Study Effects of Prenatal Drug Exposure on Developmental Outcomes
Women often abuse more than one drug, so a child’s problems frequently reflect the combined impact of multiple exposures. Substance-abusing women often also have other characteristics that can result in fetal harm, including high stress, lack of prenatal care, sexually transmitted infections, and high-risk behaviors such as drug-trade activities that expose them to violence. Once the child is born, influences that may come into play include low maternal IQ and verbal abilities, maternal psychopathology and chaotic lifestyle, exposure to lead or other toxins, and placement in institutional or foster care. The child’s CNS disruption can hinder his or her odds of reaching full developmental and academic potential directly and in combination with parental and environmental factors. For example, a parent’s poor functioning in the caregiver role may compound the limiting impact that a child’s drug-related irritability and reduced self-regulatory abilities have on opportunities for regular, language-rich dyadic exchange. A child’s drug-related cognitive and learning disabilities may derail social and vocational adjustment, and both may increase the odds of substance abuse, psychopathology, and involvement with the criminal justice system.
Because of this merging of effects, research to evaluate the specific effects of prenatal exposure to a particular drug must include assessment of key covariates known to affect the developmental and behavioral outcomes under study (Table 1). Studies must generally include an adequate number of subjects to achieve statistical power, and longitudinal studies must retain most subjects over many years. A sufficiently large control group of similar sex, race, and socioeconomic status (SES) is essential. Recently, investigators have begun to apply new technologies to relate behavioral findings of prenatally drug-exposed children to brain structure and function and genetics.
TABLE 1.
Maternal and Caregiver Covariates to Be Considered in Prenatal Substance Exposure Research
| Prenatal drug use |
| Socioeconomic status |
| Marital status |
| Parity |
| Prenatal care |
| Psychological distress |
| Quality of home environment |
| Race |
| Cognitive ability |
| Years of education |
DRUG ACTION IN THE DEVELOPING FETUS
Although the placenta was once thought to protect the fetus against exposure to toxins, it is now known that metabolites of drugs, including cocaine, opiates, amphetamines, marijuana, and tobacco, enter the fetal bloodstream. Active metabolites can penetrate the fetal blood-brain barrier and interfere with early neuronal cell development or cause neuronal death (Lee et al., 2008). Researchers hypothesize that drug metabolites interact with an individual’s genetic makeup to influence cognitive development and behavior. Thus, for example, some individuals may be genetically more susceptible than others to cocaine’s deleterious effects on development.
Maternal drug abuse also affects the fetus indirectly. For example, crack cocaine, heroin, tobacco, and marijuana cause vasoconstriction that restricts the fetal oxygen supply. As well, substance abuse often conflicts with healthy maternal practices—such as eating a nutrient-rich diet and accessing prenatal care—that reduce pregnancy complications such as diabetes, preeclampsia, and pre-term labor. Conditions that commonly co-occur with drug abuse, including sexually transmitted infections, depression, post-traumatic stress disorder, and exposure to chronic stress and violence, also may lead to fetal injury. Neonatal abstinence syndrome (NAS), which occurs after opiate use during pregnancy, puts the infant under physiological stress that increases the risk of health and possibly developmental problems.
Neuroimaging studies have revealed evidence of physiological brain changes in prenatally drug-exposed children, some of which correlated with the results of behavioral assessments. However, the studies need to be replicated, because they had small sample sizes and some lacked controls for possible confounding factors.
TOBACCO
Despite wide awareness that smoking is bad for both mother and developing fetus, in 2007, an estimated 16.4 percent of pregnant American women were current tobacco smokers (SAMHSA, 2008). Although pregnant women overall had lower smoking rates than nonpregnant women, pregnant 15- to 17-year-olds had higher smoking rates than their nonpregnant age mates.
Smoking increases a woman’s risk of ectopic pregnancy and placenta previa, both of which increase the odds of maternal mortality. Women who smoke during pregnancy are somewhat less likely to develop preeclampsia than those who do not smoke; however, among pregnant women who develop preeclampsia, smoking seems to increase mortality (Cnattingius, 2004).
Tobacco use has also been linked to low birth weight and pregnancy complications, including prematurity, placental abruption, and intrauterine death. Low birth weight suggests that the fetus has not obtained important nutrients and oxygen, which are important for optimal brain growth and neuronal development. Some evidence indicates that maternal tobacco use during pregnancy doubles the likelihood of sudden infant death syndrome (Salihu and Wilson, 2007; Table 2).
TABLE 2.
Prenatal Drug Exposure: Potential Effects on Birth and Pregnancy Outcomes
| TOBACCO | MARIJUANA | STIMULANTS | HEROIN/OPIOIDS |
|---|---|---|---|
| Pregnancy complications | No fetal growth effects | Cocaine | Stillbirth |
| Prematurity | No physical abnormalities | Prematurity | Prematurity |
| Decreased birth weight | Decreased birth weight | Decreased birth weight | |
| Decreased birth length | Decreased birth length | Decreased birth length | |
| Decreased birth head circumference | Decreased birth head circumference | Decreased birth head circumference | |
| Sudden infant death syndrome (SIDS) | Intraventricular hemorrhage | Fetal and neonatal abstinence syndrome | |
| Increased infant mortality rate | Methamphetamine | Sudden infant death syndrome (SIDS) | |
| Small for gestational age | |||
| Decreased birth weight |
Neonates who were exposed to tobacco prenatally are more excitable, have greater muscle tension, require more handling to be calmed, and show more signs of CNS stress (e.g., abnormal sucking, excessive gas, gaze aversion) than unexposed infants (Law et al., 2003). Dose-response relationships have been established between maternal tobacco use, as measured by levels of salivary cotinine (the active metabolite of nicotine) or self-report, and signs of physiological stress.
Infant CNS functional abnormalities related to pre-natal tobacco exposure include deficits in self-regulation (the infant’s ability to soothe or quiet itself) (Table 3). At 2 to 4 weeks and at 7 months of age, prenatally tobacco-exposed infants exhibited, compared with unexposed infants, more negative affect and manifestations of sadness, distress in response to limitations, decreased soothability, and fear during a test used to assess emotional self-regulation (Schuetze and Eiden, 2007; Schuetze, Eiden, and Coles, 2007). Low birth weight and reduced head growth may underlie these disturbances.
TABLE 3.
Prenatal Drug Exposure: Potential Effects on Central Nervous System Development, Cognitive Function, and Behavior*
| TOBACCO | MARIJUANA | STIMULANTS | OPIATES |
|---|---|---|---|
| Disturbed maternal-infant interaction Excitability Hypertonia Stress abstinence signs Conduct disorder Reduced IQ Aggression Antisocial behavior Impulsivity ADHD Tobacco use and dependence |
Mild withdrawal symptoms Delayed state regulation Reading, spelling difficulty Executive function impairment Early tobacco and marijuana use |
Cocaine Neonatal/Infancy Early neurobehavioral deficits: Orientation, state regulation, autonomic stability, attention,sensory and motor asymmetry, jitteriness Poor clarity of infant cues during feeding interaction Delayed information processing General cognitive delay Childhood Lower nonverbal perceptual reasoning Lower weight for height Lower weight curve trajectories Attention problems Disruptive behaviors by self-report and caregiver report |
Neonatal abstinence syndrome Less rhythmic swallowing Strabismus Possible delay in general cognitive function Anxiety Aggression Feelings of rejection Disruptive/inattentive behavior |
|
Methamphetamine Poor movement quality (3rd trimester exposure) Lower arousal Increased lethargy Increased physiological stress No mental or motor delay (infant/toddler) |
Effects may be subtle and transient.
Prenatal tobacco exposure has been consistently associated with lower IQ throughout childhood (Fried, 2002; Herrmann, King, and Weitzman, 2008). In one study, children of women who smoked more than 16 cigarettes a day while pregnant had a mean IQ in the average range, but 8 points lower than those of unexposed children (Fried, Watkinson, and Gray, 2003). Children prenatally exposed to tobacco are also at increased risk for attention problems during the early elementary school years (Cornelius et al., 2007; Langley et al., 2005; Linnet et al., 2003).
In 2007, an estimated 16.4 percent of pregnant American women were current tobacco smokers.
Conduct disorder can be an adverse outcome of prenatal tobacco exposure. In one study, adolescent children of mothers whose blood cotinine levels during pregnancy had been in the top 20 percent of those tested were twice as likely as the 20 percent of children with the least exposure to develop a conduct disorder (Braun et al., 2008). Postnatal exposure to secondhand smoke may also contribute substantially to diagnoses of conduct disorder in U.S. children (Braun et al., 2008). Recent data suggest that prenatal tobacco exposure may promote later conduct disorders by inhibiting the brain enzyme monoamine oxidase (MAO) during fetal development (Baler et al., 2008). MAO participates in the regulation of the levels of monoaminergic neurotransmitters that are critical for fetal forebrain development.
Prenatal tobacco exposure has also been implicated in depression and anxiety in early childhood through late adolescence (Robinson et al., 2008). However, these internalizing symptoms have not received as much attention as conduct disorder, perhaps because they are less disruptive to families and classrooms.
Prenatal tobacco exposure appears to increase the likelihood of tobacco use in childhood and early adolescence. In one study, the risk differential of exposed and unexposed children at age 10 was more than five-fold after controlling for environmental factors, other prenatal exposures, current maternal smoking, and child and maternal psychological covariates (Cornelius et al., 2005). However, when the children in this study were 14, prenatal tobacco exposure was no longer a significant predictor of their tobacco use when factors such as peer smoking were taken into account.
A magnetic resonance imaging (MRI) study of children aged 10 to 14 found reductions in cortical gray matter and parenchyma volumes, as well as head circumference, in those whose mothers had smoked while pregnant (Rivkin et al., 2008). Some researchers have suggested that prenatal tobacco exposure accelerates puberty among males (Fried, James, and Watkinson, 2001).
Treatment Recommendations
Behavioral interventions are recommended as the first treatment options to help pregnant women stop smoking (Oncken and Kranzler, 2009; Slotkin, 1998). Several studies have demonstrated that contingency management (CM), a strategy that dispenses cash or other tangible prizes as incentives for achieving treatment goals, helps pregnant smokers maintain abstinence (Donatelle et al., 2000; Heil, Scott, and Higgins, 2009; Higgins et al., 2004). CM may be more effective with low-income pregnant smokers (Donatelle et al., 2004), whose quit rates with CM have ranged from 19 to 40 percent, compared with 6.6 to 20.5 percent with other behavioral interventions. On its own, cognitive-behavioral therapy (CBT) yields only modest reductions in smoking-cessation rates among pregnant women. Combined treatment with CBT and nicotine replacement therapy (NRT) is more effective than CBT alone for pregnant moderate to heavy smokers (Osadchy, Kazmin, and Koren, 2009).
Behavioral interventions are recommended as the first treatment options to help pregnant women stop smoking.
Although NRT is widely used and effective in the general population, there are concerns regarding its effectiveness for pregnant smokers and safety for the fetus. At issue is whether the risks for both mother and child outweigh the harmful effects of cigarette smoking on the fetus. Some researchers endorse the use of NRT under a physician’s close supervision in combination with behavioral interventions for moderate to heavy smokers (Osadchy, Kazmin, and Koren, 2009). For heavy smokers, the benefits of NRT likely outweigh the risks of smoking during pregnancy because NRT (1) usually delivers a dose of nicotine less than or the same as what the person gets from smoking, (2) may eliminate fetal exposure to other toxins in cigarette smoke, and (3) may reduce the overall dose and duration of nicotine exposure (Oncken and Kranzler, 2003). When used, NRT therapy should begin as early in the pregnancy as possible, because a fetus may be especially sensitive to the adverse effects of nicotine exposure after the first trimester (Slotkin, 1998). The safety and efficacy of bupropion, another medication that is effective for smokers in the general population, has not been established for pregnant smokers (Oncken and Kranzler, 2003).
Abstinence from smoking during the first 2 weeks of a quit attempt is critical to long-term success (Higgins et al., 2006). It is therefore important to closely monitor early abstinence and adjust treatment as needed. Clinicians should continue to encourage women to quit even if they initially fail, because quitting at any time before childbirth reduces the risk of complications for both the mother and child.
MARIJUANA
The Ottawa Prenatal Prospective Study (OPPS), the Maternal Health Practices and Child Development (MHPCD) study, and other well-controlled studies have not implicated in utero marijuana exposure in any major fetal growth or physical abnormalities (Day et al., 1992; Fried and Smith, 2001; Table 2). The OPPS study did find a 1-week-shorter gestation period and two abnormalities associated with the visual system: true ocular hypertelorism (widely spaced eyes) and severe epicanthus (skin folds at the corners of the upper eyelids) among infants whose mothers smoked more than five joints per week while pregnant (Fried and Smith, 2001). However, the study authors concluded that the visual abnormalities were likely related to prenatal alcohol exposure rather than directly to marijuana exposure.
Studies of neonatal neurobehavioral outcomes of pre-natal marijuana exposure have observed mild withdrawal symptoms and poor autonomic control, particularly of state regulation (the ability to adjust one’s level of alertness as required for a task). Autonomic control was normal, however, when assessed at 6 months or 1 year of age (Fried, 1995; Table 3).
The OPPS and MHPCD study examined the relationship between marijuana exposure and developmental problems throughout childhood. Children of women who smoked one or more marijuana joints a day during the first trimesters were more likely than controls to exhibit deficits in school achievement, particularly in reading and spelling (Goldschmidt et al., 2004). Pre-natal marijuana exposure had persistent negative effects through age 16 on higher-order thinking, including problem solving, memory, planning, impulsivity, and attention (Fried, 2002; Fried, Watkinson, and Gray, 2003; Goldschmidt et al., 2008; Richardson, Goldschmidt, and Larkby, 2007). Researchers did not find overall suppression of IQ.
Prenatal marijuana exposure may have long-term emotional and behavioral consequences. At age 10, children who had been exposed to the drug during their first and third trimester of gestation reported more depressive symptoms than did unexposed controls (Gray, 2005). Among 16- to 21-year-olds, prenatal exposure to marijuana at least doubled the risk of both tobacco and marijuana use (Day, Goldschmidt, and Thomas, 2006; Porath and Fried, 2005). Adolescents with histories of daily prenatal marijuana exposure were 1.3 times as likely as those with less or no exposure to be high-frequency users of the drug, even after extensive control for other factors known to increase the risk of adolescent substance abuse (Day, Goldschmidt, and Thomas, 2006).
A recent functional MRI study of 18- to 22-year-olds linked prenatal marijuana exposure to altered neural functioning during a psychological test that involves remembering the placement of images that flash on a screen. Compared with a control group, the exposed group showed greater activation of neurons in the inferior and middle frontal gyri and superior temporal gyri (Smith et al., 2006).
Treatment Recommendations
Although they have not been studied specifically with pregnant users, CBT, motivational enhancement, and CM therapies have been demonstrated to be effective for reducing marijuana use (McRae, Budney, and Brady, 2003). Controlled studies of pharmacotherapies for marijuana dependence are still needed, as is intervention research specifically targeting pregnant marijuana users.
Abstinence from smoking during the first 2 weeks of a quit attempt is critical to long-term success.
COCAINE AND OTHER STIMULANTS
Several recent prospective studies have examined the consequences of prenatal cocaine exposure. Relatively few, in contrast, have addressed prenatal exposure to methamphetamine, ecstasy, or methylphenidate (Ritalin or Concerta) or other stimulant medications used to treat attention-deficit/hyperactivity disorder (ADHD).
Cocaine
At the height of the most recent crack-cocaine epidemic, in the late 1980s and the first half of the 1990s, an estimated 100,000 prenatally exposed children were born yearly in the United States. As many as 18 percent of live births were affected in some urban, primarily low-SES areas (Kandel, Warner, and Kessler, 1998; Ostrea et al., 1992; SAMHSA, 2000). Nearly 2 million Americans living today were prenatally exposed to cocaine, many of whom are now adolescents or young adults. Currently, an estimated 50,000 infants are born in the Nation each year having been prenatally exposed to cocaine.
Impact on neonatal and infant development
A majority of studies have reported that infants with histories of prenatal cocaine exposure have reduced weight, head circumference, and/or length at birth (Bada et al., 2005; Eyler et al., 1998; Singer et al., 2002b; Zuckerman et al., 1989). A meta-analysis of 33 studies conducted between 1989 and 1997 attempted to distinguish the direct effects of cocaine, as opposed to other risks commonly associated with cocaine abuse (e.g., abuse of other drugs, poor prenatal care) on these and other neonatal features and on pregnancy complications. The results confirmed two problems as directly attributable to cocaine-related physiological stress in the prenatal environment: amniotic sac rupture more than 1 hour before labor begins and separation of the placenta from the uterus prior to delivery (Addis et al., 2001).
Considerable evidence implicates prenatal cocaine exposure in subtle CNS abnormalities. When assessed with the Brazelton Neonatal Behavioral Assessment Scale, exposed infants showed deficits—albeit with much variability—in orientation, habituation, state regulation, autonomic stability, reflexes, tone, motor performance, irritability, alertness, and excitability (Singer et al., 2000). Compared with infants of mothers with similarly low SES who used other drugs during pregnancy, cocaine-exposed infants showed higher rates of sensory and motor asymmetry, poor muscle tone, jitteriness (Singer et al., 2000), and reduced novelty preference (Singer et al., 1999). Both of these studies correlated greater prenatal cocaine exposure with poorer assessment scores in non-verbal reasoning (Table 3).
Studies of the impact of prenatal cocaine exposure on development during the first 3 years of life have produced inconsistent results. For example, among low-SES children who may also have been prenatally exposed to alcohol, tobacco, and marijuana, Richardson and colleagues reported an association between cocaine exposure during the second and third trimester of gestation and decrements in motor but not in mental abilities, as measured by the Bayley Scales of Infant Development (BSID) (Richardson, Goldschimdt, and Willford, 2008). In contrast, Frank and colleagues (2002) reported no correlation between cocaine exposure and either mental or motor scores on the same instrument. Singer and colleagues (2002a) used the BSID mental development index to compare prenatally cocaine-exposed and non-cocaine-exposed 2-year-olds; the cocaine-exposed group scored 6 points lower and were twice as likely to have significant mental delay. Other research suggests that cocaine has an indirect effect on mental development through reduced head size (Behnke et al., 2006a).
Because cocaine targets the monoaminergic (dopamine, norepinephrine, epinephrine, and serotonin) neurotransmitter systems, which are known to regulate attention, researchers have been interested in the drug’s impact on children’s capacity for attention. Studies indicate that prenatal cocaine exposure can impair visual attention, visual processing speed, and visual memory in infancy and throughout the first year of life (Jacobson et al., 1996; Singer et al., 1999; 2005).
How cocaine effects measured in infancy will play out in later childhood, adolescence, and adulthood is unclear. Early CNS abnormalities are considered potential early warning signs of underlying damage that may manifest later as self-regulatory problems. However, psychological assessments made before age 4 are generally weak predictors of how a child will perform later, although reduced novelty preference has been correlated with subsequent low IQ.
Impact on children 4 years and up
No childhood physical abnormalities have been definitively attributed to prenatal cocaine exposure (Minnes et al., 2006). However, some evidence points to enduring growth consequences with lower weight-to-height ratios at 6 years of age (Minnes et al., 2006) and slower head circumference and weight trajectories from 1 to 10 years (Richardson, Goldschmidt, and Larkby, 2007).
As children grow older, psychological assessments become more stable. Subtle negative effects involving perceptual reasoning have been associated with prenatal cocaine exposure in children 4 to 9 years of age (Singer et al., 2004; 2008). Perceptual reasoning refers to one’s ability to envision solutions to nonverbal problems, such as recreating a spatial design with 3D colored blocks.
Problems of attention are particularly worrisome because they relate to poor school achievement and behavior problems. Prenatally cocaine-exposed 4- to 7-year-olds performed below standard norms on tests that measure sustained attention (Bandstra et al., 2001) and selective attention (Noland et al., 2005). On the tests, which require subjects to watch a computer screen and respond appropriately each time a particular image or stimulus appears, they made more than the average number of incorrect responses, indicating impulsivity, and omitted more correct responses (Accornero et al., 2007), indicating general inattention.
Considerable evidence implicates prenatal cocaine exposure in subtle CNS abnormalities.
Rule breaking, aggression, and other externalizing behaviors are associated with prenatal cocaine exposure and are attributed to a lack of self-regulation. Ratings completed by teachers, experimenters, and caregivers indicate that being prenatally cocaine-exposed, being male, and living in a high-risk environment are each independently predictive of aggressive behavior (Bendersky, Bennett, and Lewis, 2006). Linares and colleagues (2006) reported that among prenatally cocaine-exposed 6-year-olds:
17 percent reported symptoms of oppositional defiant disorder, compared with 9 percent of unexposed age mates; and
12 percent reported clinically elevated levels of ADHD symptoms, compared with 7 percent of unexposed peers.
At 10 years, boys with histories of prenatal cocaine exposure were more likely than unexposed boys to report high-risk traits, including aggression, substance use, and disregard for safety, on the Youth Risk Behavior Survey (Bennett, Bendersky, and Lewis, 2007). Teachers attribute high rates of behavioral problems, particularly hyperactivity, to prenatally cocaine-exposed boys (Delaney-Black et al., 2004). One longitudinal study associated clinically elevated delinquent behavior with prenatal cocaine exposure in girls (Minnes et al., 2010). Some studies have found that recent caregiver drug use and psychological symptoms, but not prenatal cocaine exposure, predicted behavioral problems (Accornero et al., 2002; 2006; Sheinkopf et al., 2006; Warner et al., 2006b). Overall, however, the evidence suggests that children with prenatal cocaine exposure should be routinely screened for behavioral problems.
There are growing concerns regarding the widespread use of stimulant medications for ADHD by women of childbearing age.
Imaging studies
Several researchers have deployed brain imaging to study the effects of prenatal cocaine exposure. These studies documented:
reduced gray matter in the right parietal and left occipital lobes and corpus callosum of 7- to 8-year-olds (Dow-Edwards et al., 2006; Singer et al., 2006) and the caudate in a group averaging 14 years of age (Avants et al., 2007);
higher diffusion in white matter frontal projections at ages 10 to 11 (Warner et al., 2006a);
decreased volume of the right anterior cerebellum at 11 years of age (Dow-Edwards et al., 2006; Behnke et al., 2006b);
significantly smaller caudate in adolescents (Avants et al., 2007); and
also in adolescents, more functional connectivity in the default mode network (related to arousal regulation) and a greater signal increase when shown emotionally arousing stimuli (Li et al., 2011).
Methamphetamine
In the only large-scale, well-controlled study of the effects of prenatal methamphetamine exposure—the Infant Development, Environment, and Lifestyle Study—exposed infants were 3.5 times as likely as controls to be small for gestational age and had a lower average birth weight (Smith et al., 2006). By using the Neonatal Intensive Care Unit Network Neurobehavioral Scale, prenatal methamphetamine exposure has been associated with lower arousal from sleep, lack of energy, and physiological symptoms indicating withdrawal. Preliminary findings indicate no impact on scores on the BSID at age 1, 2, or 3 (Lester and Lagasse, 2010). Additional followup of this cohort at later ages is needed to evaluate more subtle learning and behavioral problems.
Stimulant Medications for ADHD
There are growing concerns regarding the widespread use of stimulant medications for ADHD by women of childbearing age. To date, research has uncovered no clear pattern of negative effects on pregnancy or offspring when the medications are taken at therapeutic doses (Humphreys et al., 2007). However, no well-controlled prospective studies have been completed.
Treatment Recommendations
All stimulant drugs, including prescribed medications, should be avoided during pregnancy. Women who wish to use prescribed stimulants during pregnancy should be assessed to determine whether the potential benefits to the mother outweigh any risk to the fetus (Goodman and Quinn, 2002).
CM is a reliably effective treatment for cocaine dependence in the general population, and the use of voucher-based incentives has demonstrated promising results with pregnant women (Higgins, Alessi, and Dantona, 2002). CM used in conjunction with behaviorally based substance abuse treatment can reinforce both cocaine abstinence and compliance with prenatal care in terms of weekly attendance at prenatal clinic visits (Elk et al., 1995; 1998). In one study, CM did not greatly reduce dropout from residential treatment participation, but improved outpatient treatment retention during the transition from residential care (Svikis et al., 2007).
Methamphetamine and cocaine abusers often respond similarly to treatment (Cretzmeyer et al., 2003). Although they have not been investigated with pregnant women, CBT, CM, and the Matrix Model may be the most effective treatment approaches for stimulant abuse and dependence (Winslow, Voorhees, and Pehl, 2007).
OPIATES
Rates of prenatal opiate exposure are difficult to obtain and vary widely from less than 1 percent to 21 percent, depending on the risk status of those screened and the time period (Ostrea, 1992; Yonkers et al., 2010). A U.S. multicenter study investigating the rates of prenatal drug use by meconium analyses and maternal self-report indicated that 10.7 percent of 8,527 infants screened were exposed to cocaine or opiates (Lester et al., 2001). Although today more people abuse prescription pain relievers than illegal opiates, most research on opiates has involved subjects who are addicted to heroin or receiving opioid agonist therapy.
Fluctuations in an expectant mother’s daily heroin use due to voluntary abstinence or lack of access to the drug affect the fetus as well. If abrupt, these changes can precipitate fetal abstinence syndrome, which increases the risk of premature delivery, low birth weight, stillbirth, and sudden infant death syndrome (Joseph, Stancliff, and Langrod, 2000; Table 2). NAS occurs when birth abruptly deprives an infant of opiates it received via the placenta during gestation. NAS can manifest with serious but usually not persistent CNS symptoms, such as seizures, in 2 to 11 percent of neonates (Bandstra et al., 2010).
Heroin exposure decreases birth weight, birth length, and head circumference, but has not been associated with congenital malformations. Prenatal opiate exposure has greater adverse impact than prenatal cocaine exposure on the infant CNS and autonomic nervous system (Das, Poole, and Bada, 2004), with effects that include abnormally high muscle tone, inconsolability, irritability, sneezing, stuffiness, excessive sucking, poor sucking ability, and high-pitched cry (Table 3). The high-pitched cry signifies a CNS abnormality that can result from increased cranial pressure or a congenital malformation. Infants who were exposed to both opiates and cocaine had louder and higher-pitched cries than infants exposed to either drug alone (Lester et al., 2002).
Followup studies of children prenatally exposed to opiates have had sample sizes too small to control for important covariates. Some have found evidence of delayed general cognitive function at 3 years (Wilson et al., 1979), lower verbal ability, and impaired reading and arithmetic skills (Ornoy et al., 2001); others found no cognitive delay at 6 to 13 years of age (deCubas and Field, 1993). Prenatal opiate exposure has frequently been associated with behavioral problems in childhood. One small study indicated that opiate-exposed children were more likely to have ADHD or other disruptive behavior diagnoses at 10 years of age (Hans, 1989).
In summary, studies of prenatal opiate exposure and infants’ early cognitive development have yielded mixed results, but there seems to be a pattern linking the exposure to behavioral problems, including increases in ADHD and other disruptive behaviors.
Treatment Recommendations
Since the late 1970s, it has been widely recognized that pregnant women addicted to heroin benefit from opioid agonist therapy with methadone. By stabilizing opiate withdrawal symptoms, such treatment reduces the use of illegal heroin and increases attendance in prenatal care, healthy diet, and other positive maternal health behaviors (SAMHSA, 2005; 2006). Methadone maintenance therapy stabilizes a mother’s opiate dose at a low level and reduces physiological withdrawal effects for the fetus. Heroin-addicted women who receive such therapy have infants with higher birth weights and lower rates of intrauterine growth retardation than those who are untreated. However, newborns whose mothers are maintained on methadone have a high incidence of NAS (SAMHSA, 2005; 2006). It is recommended that NAS be treated by giving a very low dose of opiate to the infant and then slowly tapering the dose (O’Grady, Hopewell, and White, 2009).
Studies that have evaluated whether treating expectant mothers with methadone maintenance affects child development are difficult to compare because they have used different methodologies and measurements (Jones et al., 2008). A current NIDA-funded study called MOTHER is designed to address questions left open because of these methodological concerns. MOTHER will also seek to clarify whether methadone or buprenorphine is the superior pharmacotherapy for opioid-dependent pregnant women and their children (Jones et al., 2008). Buprenorphine, an alternative to methadone in opioid agonist therapy, is currently not FDA-approved for use during pregnancy because of a lack of adequate well-controlled studies with pregnant women.
Critical to the success of opioid agonist therapy is the use of supportive services, including behavioral therapy and assistance with domestic violence issues, employment, housing, food, and educational needs. Psychological interventions are indicated to address disruptions in the mother-child relationship, guilt, depression, low self-esteem and victimization, and past trauma.
A prenatally drug-exposed infant’s high-pitched cry may be due to a CNS abnormality that results from increased cranial pressure.
INTERVENTIONS FOR DRUG-EXPOSED CHILDREN
Most research on intervention services for drug-exposed infants has evaluated intensive home-based services provided to substance-abusing mothers by community nurses. These services are designed to educate and support mothers to improve the home environment, parenting skills, and child development. Strengthening maternal functioning has been the goal, because most studies of prenatal drug exposure have found that mothers’ level of psychological distress consistently predicts prenatally exposed children’s cognitive and behavioral outcomes (Minnes et al., 2010). Few studies have examined interventions that are drug-specific or directed to the infants themselves (Barnard and McKeganey, 2004).
Studies demonstrate that early intervention services improve the home environment and mothers’ parenting behavior.
Several studies demonstrate that early intervention services improve the home environment and mothers’ parenting behavior. In one, nurses visited substance-abusing mothers and their infants every other week during the first 18 months of the child’s life (Black et al., 1994). The nurses guided the women through a curriculum about normal child development, child care, and safety; modeled parent-child activities that promote child development; addressed mothers’ concerns, such as relationship problems, affordable housing, and financial issues; and provided information about community resources and advocacy. The mothers who received the intervention were marginally more likely than a control group to be drug-free, keep primary health care appointments, be more emotionally responsive, provide a stimulating home environment, and score lower on a measure of child-abuse potential at the end of the 18-month study period.
As part of the Seattle Birth to 3 Program, paraprofessional advocates visited substance-abusing women and their children weekly for the first 6 weeks after birth, then at least biweekly, depending on need, for 3 years. The advocates worked to establish trusting relationships with the mothers and motivate them to identify and work toward personal goals. They made and monitored followup on community referrals for drug treatment and other services for mother and child, and offered guidance and supervision to ensure that the child was in a safe environment and received appropriate care. At 36 months postpartum, 69 percent of the children receiving the intervention service were in what the research team considered to be an appropriate custody situation relative to their mother’s current use of alcohol/drugs (i.e., with mother in recovery for at least 6 months or not with mother unable to maintain abstinence), compared with 29 percent of children in a control group (Ernst et al., 1999).
Butz and colleagues (2001) found that mothers participating in another intensive home nurse intervention program reported a trend toward less parenting stress.
Child Development
Findings regarding the impact of intervention services on child development have been mixed, perhaps because the services usually consist of family case management rather than interventions directed specifically toward the children. Of note, even when children appeared to benefit from an intervention, exposed children in the comparison group who did not receive it usually performed within normal limits on developmental assessments.
Kilbride and colleagues (2000) followed a group of cocaine-exposed infants and their mothers for 3 years, providing intensive family case management, enriched nursery care, and regular evaluations, and found no differences in mean cognitive, psychomotor, or language quotients compared with a group of exposed infants who received only routine followup and a group of unexposed infants. However, at 36 months, verbal scores of the cocaine-exposed infants who received case management were significantly higher than those of the routinely managed children, suggesting that “early intervention may have offset detrimental effects of the crack cocaine environment on verbal development.”
In another study, infants who participated in an intensive home intervention program had significantly higher mental and psychomotor development scores compared with control infants (Schuler, Nair, and Kettinger, 2003).
In contrast, Black and colleagues (1994) reported that children receiving home-based intervention services had somewhat higher cognitive scores relative to controls at 6 months of age, but not at 12 and 18 months. Ernst and colleagues (1999) found that the cognitive development of children of substance-abusing mothers who received in-home advocacy services was equivalent at 36 months to that of children whose mothers did not receive the services.
Impact of Child Placement
Drug-exposed infants are often placed outside of the mother’s home in kinship, foster, or adoptive care to prevent child abuse or neglect. Researchers have investigated the possibility that such placement might avoid the ill effects of an unstable environment on children’s development, but studies show inconsistent results. For example:
Tyler and colleagues (1997) found that drug-exposed infants who remained with their biological mothers demonstrated better cognitive development at 6 months of age compared with infants placed in the care of other relatives. In another study by Frank and colleagues (2002), infants in kinship care scored lower on mental development than infants in the care of their biological mothers or in foster care at 6 and 24 months of age (Frank et al., 2002). In the latter study, children in foster care lagged behind children in their biological mothers’ care at 6 months, but surpassed them at 24 months.
Brown and colleagues (2004) observed more positive social-emotional development in 24-month-old cocaine-exposed children placed in nonparental care compared with those in parental care. Within the nonparental care group, those with nonkin caregivers scored higher in mental development, communicative gestures, and positive interactions during feeding than those in the care of relatives.
Singer and colleagues (2004; 2008) consistently found that over time, cocaine-exposed children fared better in cognitive and language development when placed in non-kin foster care or adoptive homes than when raised in a relative’s care or their birth mother’s custody. These children experienced better home environments and had more educated, less depressed caregivers than children who remained with their mothers or with relatives (Lewis et al., 2004; Singer et al., 2004; 2008).
Bada and colleagues (2008) found that instability in living arrangements, such as multiple moves, changes in caregivers, and prolonged involvement with child protection services, predicted negative behavioral outcomes during the first 3 years of life in a cohort of prenatally drug-exposed children. Total behavior problem scores on the Child Behavior Checklist increased 2.3 and 1.3 points, respectively, with each move per year and each year of child protective services involvement.
A Comprehensive Approach
Bandstra and colleagues (2010) have proposed a prevention and intervention model for substance-abusing mothers and their infants that addresses the complex, multiple risk factors associated with maternal drug use. The model proposes the delivery of medical and behavioral health and parenting services to the mother, health and development services to the child, and care coordination and family support to reduce the barriers to accessing services.
Intervention services for this population need to extend beyond infancy and the toddler years, since problems in cognitive, language, and behavioral functioning may persist throughout childhood. Developmental assessment and intervention should continue during the preschool and school years, when children may benefit from enriched educational programs and screening for special education services. Problems can compound when cognitive demands increase during the early school years. Other critical transitional periods occur in the first, fourth, and sixth or seventh grades, when subtle learning or behavior problems may become more evident and lead to functional impairments (Weitzman et al., 2002). Externalizing behavior problems and inattention in particular should not be ignored, as they are known to interfere with school achievement, school completion, and the development of healthy relationships.
Parents should be trained in the skills necessary to address behavior problems throughout childhood to prevent more serious disruptive and risky behaviors in adolescence and young adulthood. Moreover, birth mothers are likely to need ongoing intervention to maintain sobriety and to address mental health symptoms and parenting. As the effects of prenatal drug exposure and their relationships with environmental factors become more clearly understood, more specific early intervention programs for drug-exposed children targeting areas of development that are known to be at risk should be developed and rigorously evaluated (Table 4).
Intervention services for substance-abusing mothers and their children need to extend beyond infancy and the toddler years.
TABLE 4.
Suggested Interventions Following Prenatal Drug Exposure
| MATERNAL/CAREGIVER | CHILD |
|---|---|
Intensive home-based services
|
Specific individual therapy
|
| Mental health treatment | Early intervention/enrichment |
| Substance use treatment | Ongoing cognitive and behavioral assessment |
CONCLUSION
Substance use during pregnancy can affect the developing fetus both directly, through passage of the drug through the placenta, and indirectly, through poor maternal health habits and environmental conditions. Numerous well-designed studies indicate that specific learning and behavior problems may result from prenatal exposure to tobacco and illicit drugs in combination with negative environmental conditions postpartum. Longitudinal studies indicate that some of the negative effects of cocaine, tobacco, and marijuana exposure persist into later childhood and adolescence. Although some early CNS symptoms remit over the first year of life, they may be precursors to later developmental outcomes.
Pregnancy is a unique time when a woman may seek treatment out of concern for the health and well-being of her child.
Developmental outcomes of prenatally drug-exposed children are determined by factors including the specific drug or drugs, dosage, and timing of prenatal exposure as well as pre- and postnatal environmental conditions, including continued caregiver drug use, psychological symptoms, quality of the home environment, postnatal exposures to lead and other toxins, caregiver stability, and type of caregiver. The effects of negative environmental conditions associated with low SES may sometimes overshadow the effects of prenatal drug exposure.
Pregnancy is a unique time when a woman may seek treatment out of concern for the health and well-being of her child. To prevent postpartum substance abuse relapse, interventions should focus on cessation rather than temporary abstinence. The ongoing consequences of parental substance abuse on child growth and development should be emphasized, and followup should continue into the postpartum period (Muhuri and Gfroerer, 2009). Interventions that reduce substance abuse in the general population are now being investigated in pregnant substance abusers with promising results. The use of CM appears to increase treatment retention and prolong abstinence in pregnant women with cocaine, opiate, and nicotine dependence. Some medications used to treat addiction, such as methadone, can be relatively safe for pregnant women and their babies. However, the safety and effectiveness of NRT for pregnant smokers requires further investigation.
Additional research is needed on the development of specific interventions for drug-exposed infants and children. Each child must be individually assessed for his or her cumulative risk factors, domain of developmental difficulty, and the quality of the caregiving environment. Developmental outcomes may be optimized by interventions that occur early in life, are tailored for specific problem areas, and target caregivers’ level of stress, mental health functioning, continued substance abuse, and parenting interactions.
Acknowledgments
The preparation of this paper was supported by the National Institute on Drug Abuse (NIDA) grant R01 DA07957 to Dr. Minnes.
REFERENCES
- Accornero VH, et al. Behavioral outcome of preschoolers exposed prenatally to cocaine: Role of maternal behavioral health. Journal of Pediatric Psychology. 2002;27(3):259–269. doi: 10.1093/jpepsy/27.3.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Accornero VH, et al. Prenatal cocaine exposure: An examination of childhood externalizing and internalizing behavior problems at age 7 years. Epidemiologiae Psichiatria Sociale. 2006;15(1):20–29. [PMC free article] [PubMed] [Google Scholar]
- Accornero VH, et al. Impact of prenatal cocaine exposure on attention and response inhibition as assessed by continuous performance tests. Journal of Developmental and Behavioral Pediatrics. 2007;28(3):195–205. doi: 10.1097/01.DBP.0000268560.72580.f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addis A, et al. Fetal effects of cocaine: An updated meta-analysis. Reproductive Toxicology. 2001;15(4):341–369. doi: 10.1016/s0890-6238(01)00136-8. [DOI] [PubMed] [Google Scholar]
- Avants BB, et al. Effects of heavy in utero cocaine exposure on adolescent caudate morphology. Pediatric Neurology. 2007;37(4):275–279. doi: 10.1016/j.pediatrneurol.2007.06.012. [DOI] [PubMed] [Google Scholar]
- Bada HS, et al. Low birth weight and preterm births: Etiologic fraction attributable to prenatal drug exposure. Journal of Perinatology. 2005;25:631–637. doi: 10.1038/sj.jp.7211378. [DOI] [PubMed] [Google Scholar]
- Bada HS. Importance of stability of early living arrangements on behavior outcomes of children with and without prenatal drug exposure. Journal of Developmental and Behavioral Pediatrics. 2008;29(3):173–182. doi: 10.1097/DBP.0b013e3181644a79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baler RD, et al. Is fetal brain monoamine oxidase inhibition the missing link between maternal smoking and conduct disorders? Journal of Psychiatry and Neuroscience. 2008;33(3):187–195. [PMC free article] [PubMed] [Google Scholar]
- Bandstra ES, et al. Longitudinal investigation of task persistence and sustained attention in children with prenatal cocaine exposure. Neurotoxicology and Teratology. 2001;23(6):545–559. doi: 10.1016/s0892-0362(01)00181-7. [DOI] [PubMed] [Google Scholar]
- Bandstra ES, et al. Prenatal drug exposure: Infant and toddler outcomes. Journal of Addictive Diseases. 2010;29(2):245–258. doi: 10.1080/10550881003684871. [DOI] [PubMed] [Google Scholar]
- Barnard M, McKeganey N. The impact of parental problem drug use on children: What is the problem and what can be done to help? Addiction. 2004;99(5):552–559. doi: 10.1111/j.1360-0443.2003.00664.x. [DOI] [PubMed] [Google Scholar]
- Behnke M, et al. Outcome from a prospective, longitudinal study of prenatal cocaine use: Preschool development at 3 years of age. Journal of Pediatric Psychology. 2006a;31(1):41–49. doi: 10.1093/jpepsy/jsj027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behnke M, et al. Neuroimaging in prenatally cocaine-exposed children. Neurotoxicology and Teratology. 2006b;28:386–402. doi: 10.1016/j.ntt.2005.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendersky M, Bennett D, Lewis M. Aggression at age 5 as a function of prenatal exposure to cocaine, gender, and environmental risk. Journal of Pediatric Psychology. 2006;31(1):71–84. doi: 10.1093/jpepsy/jsj025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett D, Bendersky M, Lewis M. Preadolescent health risk behavior as a function of prenatal cocaine exposure and gender. Journal of Developmental and Behavioral Pediatrics. 2007;28(6):467–472. doi: 10.1097/DBP.0b013e31811320d8. [DOI] [PubMed] [Google Scholar]
- Black MM, et al. Parenting and early development among children of drug-abusing women: Effects of home intervention. Pediatrics. 1994;94(4):440–448. [PubMed] [Google Scholar]
- Braun JM, et al. Association of environmental toxicants and conduct disorder in U.S. children: NHANES 2001–2004. Environmental Health Perspectives. 2008;116(7):956–962. doi: 10.1289/ehp.11177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JV, et al. Prenatal cocaine exposure: A comparison of 2-year-old children in parental and nonparental care. Child Development. 2004;75(4):1282–1295. doi: 10.1111/j.1467-8624.2004.00739.x. [DOI] [PubMed] [Google Scholar]
- Butz AM, et al. Effectiveness of a home intervention for perceived child behavioral problems and parenting stress in children with in utero drug exposure. Archives of Pediatrics and Adolescent Medicine. 2001;155(9):1029–1037. doi: 10.1001/archpedi.155.9.1029. [DOI] [PubMed] [Google Scholar]
- Cnattingius S. The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine & Tobacco Research. 2004;6(S2):S125–S140. doi: 10.1080/14622200410001669187. [DOI] [PubMed] [Google Scholar]
- Cornelius MD, et al. Is prenatal tobacco exposure a risk factor for early adolescent smoking? A follow-up study. Neurotoxicology and Teratology. 2005;27(4):667–676. doi: 10.1016/j.ntt.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Cornelius MD, et al. Smoking during teenage pregnancies: Effects on behavioral problems in offspring. Nicotine & Tobacco Research. 2007;9(7):739–750. doi: 10.1080/14622200701416971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cretzmeyer M, et al. Treatment of methamphetamine abuse: Research findings and clinical directions. Journal of Substance Abuse Treatment. 2003;24(3):267–277. doi: 10.1016/s0740-5472(03)00028-x. [DOI] [PubMed] [Google Scholar]
- Das A, Poole WK, Bada HS. A repeated measures approach for simultaneous modeling of multiple neurobehavioral outcomes in newborns exposed to cocaine in utero. American Journal of Epidemiology. 2004;159(9):891–899. doi: 10.1093/aje/kwh114. [DOI] [PubMed] [Google Scholar]
- Day NL, et al. The effects of prenatal tobacco and marijuana use on offspring growth from birth through 3 years of age. Neurotoxicology and Teratology. 1992;14(6):407–414. doi: 10.1016/0892-0362(92)90051-b. [DOI] [PubMed] [Google Scholar]
- Day NL, Goldschmidt L, Thomas CA. Prenatal marijuana exposure contributes to the prediction of marijuana use at age 14. Addiction. 2006;101(9):1313–1322. doi: 10.1111/j.1360-0443.2006.01523.x. [DOI] [PubMed] [Google Scholar]
- deCubas MM, Field T. Children of methadone-dependent women: Developmental outcomes. American Journal of Orthopsychiatry. 1993;63(2):266–276. doi: 10.1037/h0079429. [DOI] [PubMed] [Google Scholar]
- Delaney-Black V, et al. Prenatal cocaine: Quantity of exposure and gender moderation. Journal of Developmental and Behavioral Pediatrics. 2004;25(4):254–263. doi: 10.1097/00004703-200408000-00005. [DOI] [PubMed] [Google Scholar]
- Donatelle RJ, et al. Randomised controlled trial using social support and financial incentives for high risk pregnant smokers: Significant Other Supporter (SOS) program. Tobacco Control. 2000;9(S3):iii67–iii69. doi: 10.1136/tc.9.suppl_3.iii67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donatelle RJ, et al. Incentives in smoking cessation: Status of the field and implications for research and practice with pregnant smokers. Nicotine & Tobacco Research. 2004;6(S2):S163–S179. doi: 10.1080/14622200410001669196. [DOI] [PubMed] [Google Scholar]
- Dow-Edwards DL, et al. Neuroimaging of prenatal drug exposure. Neurotoxicology and Teratology. 2006;28(3):386–402. doi: 10.1016/j.ntt.2006.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elk R, et al. Behavioral treatment of cocaine-dependent pregnant women and TB–exposed patients. Addictive Behaviors. 1995;20(4):533–542. doi: 10.1016/0306-4603(94)00076-b. [DOI] [PubMed] [Google Scholar]
- Elk R, et al. Cessation of cocaine use during pregnancy: Effects of contingency management interventions on maintaining abstinence and complying with prenatal care. Addictive Behaviors. 1998;23(1):57–64. doi: 10.1016/s0306-4603(97)00020-8. [DOI] [PubMed] [Google Scholar]
- Ernst CC, et al. Intervention with high-risk alcohol and drug-abusing mothers: II. Three-year findings from the Seattle model of paraprofessional advocacy. Journal of Community Psychology. 1999;27(1):19–38. [Google Scholar]
- Eyler FD, et al. Birth outcome from a prospective, matched study of prenatal crack/cocaine use: I. Interactive and dose effects on health and growth. Pediatrics. 1998;101(2):229–237. doi: 10.1542/peds.101.2.229. [DOI] [PubMed] [Google Scholar]
- Frank DA, et al. Level of prenatal cocaine exposure and scores on the Bayley Scales of Infant Development: Modifying effects of caregiver, early intervention, and birth weight. Pediatrics. 2002;110(6):1143–1152. doi: 10.1542/peds.110.6.1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried PA. Prenatal exposure to marihuana and tobacco during infancy, early and middle childhood: Effects and an attempt at synthesis. Archives of Toxicology. Supplement. 1995;17:233–260. doi: 10.1007/978-3-642-79451-3_21. [DOI] [PubMed] [Google Scholar]
- Fried PA. Conceptual issues in behavioral teratology and their application in determining long-term sequelae of prenatal marihuana exposure. Journal of Child Psychology and Psychiatry. 2002;43(1):81–102. doi: 10.1111/1469-7610.00005. [DOI] [PubMed] [Google Scholar]
- Fried PA, James DS, Watkinson B. Growth and pubertal milestones during adolescence in offspring prenatally exposed to cigarettes and marihuana. Neurotoxicology and Teratology. 2001;23(5):431–436. doi: 10.1016/s0892-0362(01)00161-1. [DOI] [PubMed] [Google Scholar]
- Fried PA, Smith AM. A literature review of the consequences of prenatal marihuana exposure: An emerging theme of a deficiency in aspects of executive function. Neurotoxicology and Teratology. 2001;23(1):1–11. doi: 10.1016/s0892-0362(00)00119-7. [DOI] [PubMed] [Google Scholar]
- Fried PA, Watkinson B, Gray R. Differential effects on cognitive functioning in 13- to 16-year-olds prenatally exposed to cigarettes and marihuana. Neurotoxicology and Teratology. 2003;25(4):427–436. doi: 10.1016/s0892-0362(03)00029-1. [DOI] [PubMed] [Google Scholar]
- Goldschmidt L, et al. Prenatal marijuana and alcohol exposure and academic achievement at age 10. Neurotoxicology and Teratology. 2004;26(4):521–532. doi: 10.1016/j.ntt.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Goldschmidt L, et al. Prenatal marijuana exposure and intelligence test performance at age 6. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(3):254–263. doi: 10.1097/CHI.0b013e318160b3f0. [DOI] [PubMed] [Google Scholar]
- Goodman MD, Quinn PO. Medication use during pregnancy: A concern for women with AD/HD. In: Nadeau K, Quinn PO, editors. Understanding Women with AD/HD. Silver Spring, MD: Advantage Books; 2002. pp. 69–85. [Google Scholar]
- Gray KA. Prenatal marijuana exposure: Effect on child depressive symptoms at ten years of age. Neurotoxicology and Teratology. 2005;27(3):439–448. doi: 10.1016/j.ntt.2005.03.010. [DOI] [PubMed] [Google Scholar]
- Hans SL. Developmental consequences of prenatal exposure to methadone. Annals of the New York Academy of Sciences. 1989;562:195–207. doi: 10.1111/j.1749-6632.1989.tb21018.x. [DOI] [PubMed] [Google Scholar]
- Heil SH, Scott TL, Higgins ST. An overview of principles of effective treatment of substance use disorders and their potential application to pregnant cigarette smokers. Drug and Alcohol Dependence. 2009;104(S1):S106–S114. doi: 10.1016/j.drugalcdep.2009.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann M, King K, Weitzman M. Prenatal tobacco smoke and postnatal secondhand smoke exposure and child neurodevelopment. Current Opinion in Pediatrics. 2008;20(2):187–190. doi: 10.1097/MOP.0b013e3282f56165. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Alessi SM, Dantona RL. Voucher-based incentives: A substance abuse treatment innovation. Addictive Behaviors. 2002;27(6):887–910. doi: 10.1016/s0306-4603(02)00297-6. [DOI] [PubMed] [Google Scholar]
- Higgins ST, et al. A pilot study on voucher-based incentives to promote abstinence from cigarette smoking during pregnancy and postpartum. Nicotine & Tobacco Research. 2004;6(6):1015–1020. doi: 10.1080/14622200412331324910. [DOI] [PubMed] [Google Scholar]
- Higgins ST, et al. Smoking status in the initial weeks of quitting as a predictor of smoking-cessation outcomes in pregnant women. Drug and Alcohol Dependence. 2006;85(2):138–141. doi: 10.1016/j.drugalcdep.2006.04.005. [DOI] [PubMed] [Google Scholar]
- Humphreys C, et al. Exposure to attention deficit hyperactivity disorder medications during pregnancy. Canadian Family Physician. 2007;53(7):1153–1155. [PMC free article] [PubMed] [Google Scholar]
- Jacobson SW, et al. New evidence for neurobehavioral effects of in utero cocaine exposure. Journal of Pediatrics. 1996;129(4):581–590. doi: 10.1016/s0022-3476(96)70124-5. [DOI] [PubMed] [Google Scholar]
- Jones HE, et al. Treatment of opioid-dependent pregnant women: Clinical and research issues. Journal of Substance Abuse Treatment. 2008;35(3):245–259. doi: 10.1016/j.jsat.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph H, Stancliff S, Langrod J. Methadone maintenance treatment (MMT): A review of historical and clinical issues. Mount Sinai Journal of Medicine. 2000;67(5–6):347–364. [PubMed] [Google Scholar]
- Kandel DB, Warner LA, Kessler RC. Epidemiology of Drug Use and Abuse Among Women. Rockville, MD: National Institutes of Health; 1998. [Google Scholar]
- Kilbride H, et al. Thirty-six-month outcome of prenatal cocaine exposure for term or near-term infants: Impact of early case management. Journal of Developmental and Behavioral Pediatrics. 2000;21(1):19–26. doi: 10.1097/00004703-200002000-00004. [DOI] [PubMed] [Google Scholar]
- Langley K, et al. Maternal smoking during pregnancy as an environmental risk factor for attention deficit hyperactivity disorder behavior. A review. Minerva Pediatrica. 2005;57(6):359–371. [PubMed] [Google Scholar]
- Law KL, et al. Smoking during pregnancy and newborn neurobehavior. Pediatrics. 2003;111(6):1318–1323. doi: 10.1542/peds.111.6.1318. [DOI] [PubMed] [Google Scholar]
- Lee C-T, et al. A mechanism for the inhibition of neural progenitor cell proliferation by cocaine. PLoS Medicine. 2008;5(6):e117. doi: 10.1371/journal.pmed.0050117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester BM, et al. The Maternal Lifestyle Study: Drug use by meconium toxicology and maternal self-report. Pediatrics. 2001;107(2):309–317. doi: 10.1542/peds.107.2.309. [DOI] [PubMed] [Google Scholar]
- Lester BM, et al. The Maternal Lifestyle Study: Effects of substance exposure during pregnancy on neurodevelopmental outcome in 1-month-old infants. Pediatrics. 2002;110(6):1182–1192. doi: 10.1542/peds.110.6.1182. [DOI] [PubMed] [Google Scholar]
- Lester BM, Lagasse LL. Children of addicted women. Journal of Addictive Diseases. 2010;29(2):259–276. doi: 10.1080/10550881003684921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis BA, et al. Four-year language outcomes of children exposed to cocaine in utero. Neurotoxicology and Teratology. 2004;26:617–627. doi: 10.1016/j.ntt.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Li A, et al. Increased “default mode” activity in adolescents prenatally exposed to cocaine. Human Brain Mapping. 2011;32(5):759–770. doi: 10.1002/hbm.21059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linares TJ, et al. Mental health outcomes of cocaine-exposed children at 6 years of age. Journal of Pediatric Psychology. 2006;31(1):85–97. doi: 10.1093/jpepsy/jsj020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linnet KM, et al. Maternal lifestyle factors in pregnancy risk of attention deficit hyperactivity disorder and associated behaviors: Review of the current evidence. American Journal of Psychiatry. 2003;160(6):1028–1040. doi: 10.1176/appi.ajp.160.6.1028. [DOI] [PubMed] [Google Scholar]
- Manji S, et al. A review of the verbal and visual memory impairments in children with foetal alcohol spectrum disorders. Developmental Neurorehabilitation. 2009;12(4):239–247. doi: 10.1080/17518420902980118. [DOI] [PubMed] [Google Scholar]
- Mayes LC. A behavioral teratogenic model of the impact of prenatal cocaine exposure on arousal regulatory systems. Neurotoxicology and Teratology. 2002;24(3):385–395. doi: 10.1016/s0892-0362(02)00200-3. [DOI] [PubMed] [Google Scholar]
- McRae AL, Budney AJ, Brady KT. Treatment of marijuana dependence: A review of the literature. Journal of Substance Abuse Treatment. 2003;24(4):369–376. doi: 10.1016/s0740-5472(03)00041-2. [DOI] [PubMed] [Google Scholar]
- Minnes S, et al. Dysmorphic and anthropometric outcomes in 6-year-old prenatally cocaine-exposed children. Neurotoxicology and Teratology. 2006;28(1):28–38. doi: 10.1016/j.ntt.2005.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnes S, et al. The effects of prenatal cocaine-exposure on problem behavior in children 4–10 years. Neurotoxicology and Teratology. 2010;32(4):443–451. doi: 10.1016/j.ntt.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhuri PK, Gfroerer JC. Substance use among women: Associations with pregnancy, parenting, and race/ethnicity. Maternal and Child Health Journal. 2009;13:376–385. doi: 10.1007/s10995-008-0375-8. [DOI] [PubMed] [Google Scholar]
- Noland JS, et al. Prenatal drug exposure and selective attention in preschoolers. Neurotoxicology and Teratology. 2005;27:429–438. doi: 10.1016/j.ntt.2005.02.001. [DOI] [PubMed] [Google Scholar]
- O’Connor MJ, Paley B. Psychiatric conditions associated with prenatal alcohol exposure. Developmental Disabilities Research Reviews. 2009;15(3):225–234. doi: 10.1002/ddrr.74. [DOI] [PubMed] [Google Scholar]
- O’Grady MJ, Hopewell J, White MJ. Management of neonatal abstinence syndrome: A national survey and review of practice. Archives of Disease in Childhood: Fetal and Neonatal Edition. 2009;94:F249–F252. doi: 10.1136/adc.2008.152769. [DOI] [PubMed] [Google Scholar]
- Oncken CA, Kranzler HR. Pharmacotherapies to enhance smoking cessation during pregnancy. Drug and Alcohol Review. 2003;22(2):191–202. doi: 10.1080/09595230100100633. [DOI] [PubMed] [Google Scholar]
- Oncken CA, Kranzler HR. What do we know about the role of pharmacotherapy for smoking cessation before or during pregnancy? Nicotine & Tobacco Research. 2009;11(11):1265–1273. doi: 10.1093/ntr/ntp136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornoy A, et al. Developmental outcome of school-age children born to mothers with heroin dependency: Importance of environmental factors. Developmental Medicine and Child Neurology. 2001;43(10):668–675. doi: 10.1017/s0012162201001219. [DOI] [PubMed] [Google Scholar]
- Osadchy A, Kazmin A, Koren G. Nicotine replacement therapy during pregnancy: Recommended or not recommended? Journal of Obstetrics and Gynaecology Canada. 2009;31(8):744–747. doi: 10.1016/S1701-2163(16)34281-5. [DOI] [PubMed] [Google Scholar]
- Paley B, O’Connor MJ. Intervention for individuals with fetal alcohol spectrum disorders: Treatment approaches and case management. Developmental Disabilities Research Reviews. 2009;15(3):258–267. doi: 10.1002/ddrr.67. [DOI] [PubMed] [Google Scholar]
- Porath AJ, Fried PA. Effects of prenatal cigarette and marijuana exposure on drug use among offspring. Neurotoxicology and Teratology. 2005;27(2):267–277. doi: 10.1016/j.ntt.2004.12.003. [DOI] [PubMed] [Google Scholar]
- Richardson GA, Goldschmidt L, Larkby C. Effects of prenatal cocaine exposure on growth: A longitudinal analysis. Pediatrics. 2007;120(4):e1017–e1027. doi: 10.1542/peds.2006-3482. [DOI] [PubMed] [Google Scholar]
- Richardson GA, Goldschmidt L, Willford J. The effects of prenatal cocaine use on infant development. Neurotoxicology and Teratology. 2008;30(2):96–106. doi: 10.1016/j.ntt.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivkin MJ, et al. Volumetric MRI study of brain in children with intrauterine exposure to cocaine, alcohol, tobacco, and marijuana. Pediatrics. 2008;121(4):741–750. doi: 10.1542/peds.2007-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson M, et al. Pre- and postnatal influences on preschool mental health: A large-scale cohort study. Journal of Child Psychology and Psychiatry. 2008;49(10):1118–1128. doi: 10.1111/j.1469-7610.2008.01955.x. [DOI] [PubMed] [Google Scholar]
- Salihu HM, Wilson RE. Epidemiology of prenatal smoking and perinatal outcomes. Early Human Development. 2007;83(11):713–720. doi: 10.1016/j.earlhumdev.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Schuetze P, Eiden RD. The association between prenatal exposure to cigarettes and infant and maternal negative affect. Infant Behavior and Development. 2007;30(3):387–398. doi: 10.1016/j.infbeh.2006.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuetze P, Eiden RD, Coles CD. Prenatal cocaine and other substance exposure: Effects on infant autonomic regulation at 7 months of age. Developmental Psychobiology. 2007;49(3):276–289. doi: 10.1002/dev.20215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler ME, Nair P, Kettinger L. Drug-exposed infants and developmental outcome: Effects of a home intervention and ongoing maternal drug use. Archives of Pediatrics and Adolescent Medicine. 2003;157(2):133–138. doi: 10.1001/archpedi.157.2.133. [DOI] [PubMed] [Google Scholar]
- Sheinkopf SJ, et al. Interactions between maternal characteristics and neonatal behavior in the prediction of parenting stress and perception of infant temperament. Journal of Pediatric Psychology. 2006;31(1):27–40. doi: 10.1093/jpepsy/jsj026. [DOI] [PubMed] [Google Scholar]
- Singer LT, et al. Neonatal visual information processing in cocaine-exposed and non-exposed infants. Infant Behavior & Development. 1999;22(1):1–15. doi: 10.1016/S0163-6383(99)80002-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, et al. Neurobehavioral outcomes of cocaine-exposed infants. Neurotoxicology and Teratology. 2000;22(5):653–666. doi: 10.1016/s0892-0362(00)00092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, et al. Cognitive and motor outcomes of cocaine-exposed infants. JAMA. 2002a;287(15):1952–1960. doi: 10.1001/jama.287.15.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, et al. Effects of cocaine/polydrug exposure and maternal psychological distress on infant birth outcomes. Neurotoxicology and Teratology. 2002b;24(2):127–135. doi: 10.1016/s0892-0362(01)00208-2. [DOI] [PubMed] [Google Scholar]
- Singer LT, et al. Cognitive outcomes of preschool children with prenatal cocaine exposure. JAMA. 2004;291(20):2448–2456. doi: 10.1001/jama.291.20.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, et al. Prenatal cocaine exposure and infant cognition. Infant Behavior and Development. 2005;28(4):431–444. doi: 10.1016/j.infbeh.2005.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, et al. Neuroimaging of prenatal drug exposure. Neurotoxicology and Teratology. 2006;28:386–402. doi: 10.1016/j.ntt.2006.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, et al. Prenatal cocaine exposure: Drug and environmental effects at 9 years. Journal of Pediatrics. 2008;153(1):105–111. doi: 10.1016/j.jpeds.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slotkin TA. Fetal nicotine or cocaine exposure: Which one is worse? Journal of Pharmacology and Experimental Therapeutics. 1998;285(3):931–945. [PubMed] [Google Scholar]
- Smith AM, et al. Effects of prenatal marijuana on visuospatial working memory: An fMRI study in young adults. Neurotoxicology and Teratology. 2006;28(2):286–295. doi: 10.1016/j.ntt.2005.12.008. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Preliminary Results from the 1999 National Household Survey on Drug Abuse. Rockville, MD: U.S. Department of Health and Human Services; 2000. [Google Scholar]
- SAMHSA . Medication-Assisted Treatment for Opioid Addiction in Opioid Treatment Programs. Rockville, MD: Center for Substance Abuse Treatment (CSAT); 2005 & 2006. [PubMed] [Google Scholar]
- SAMHSA . Results from the 2007 National Survey on Drug Use and Health: National Findings. Rockville, MD: U.S. Department of Health and Human Services, Office of Applied Studies; 2008. [Google Scholar]
- Svikis DS, et al. Behavioral strategies to improve treatment participation and retention by pregnant drug-dependent women. Substance Use and Misuse. 2007;42(10):1527–1535. doi: 10.1080/10826080701212121. [DOI] [PubMed] [Google Scholar]
- Tyler R, et al. Placement with substance-abusing mothers vs. placement with other relatives: Infant outcomes. Child Abuse and Neglect. 1997;21(4):337–349. doi: 10.1016/s0145-2134(96)00175-5. [DOI] [PubMed] [Google Scholar]
- Vorhees CV. Concepts in teratology and developmental toxicology derived from animal research. Annals of the New York Academy of Sciences. 1989;562:31–41. doi: 10.1111/j.1749-6632.1989.tb21005.x. [DOI] [PubMed] [Google Scholar]
- Warner TD, et al. Diffusion tensor imaging of frontal white matter and executive functioning in cocaine-exposed children. Pediatrics. 2006a;118(5):2014–2024. doi: 10.1542/peds.2006-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner TD, et al. Predicting caregiver-reported behavior problems in cocaine-exposed children at 3 years. Journal of Developmental and Behavioral Pediatrics. 2006b;27(2):83–92. doi: 10.1097/00004703-200604000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman M, et al. The effects of tobacco exposure on children’s behavioral and cognitive functioning. Neurotoxicology and Teratology. 2002;24(3):397–406. doi: 10.1016/s0892-0362(02)00201-5. [DOI] [PubMed] [Google Scholar]
- Wilson GS, et al. The development of preschool children of heroin-addicted mothers: A controlled study. Pediatrics. 1979;63(1):135. [PubMed] [Google Scholar]
- Winslow BT, Voorhees KI, Pehl KA. Methamphetamine abuse. American Family Physician. 2007;76(8):1169–1174. [PubMed] [Google Scholar]
- Yonkers KA, et al. Screening for prenatal substance use: Development of the Substance Use Risk Profile-Pregnancy scale. Obstetrics and Gynecology. 2010;116(4):827–833. doi: 10.1097/AOG.0b013e3181ed8290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman B, et al. Effects of maternal marijuana and cocaine use on fetal growth. New England Journal of Medicine. 1989;320(12):762–768. doi: 10.1056/NEJM198903233201203. [DOI] [PubMed] [Google Scholar]