Abstract
Purpose
Epilepsy is common in sub-Saharan Africa but is poorly characterized. Most studies are hospital-based, and may not reflect the situation in rural areas with limited access to medical care. We examined people with active convulsive epilepsy (ACE), to determine if the clinical features could help elucidate the causes.
Methods
We conducted a detailed descriptive analysis of 445 people with ACE identified through a community-based survey of 151,408 people in rural Kenya, including the examination of electroencephalograms.
Results
Approximately half of the 445 people with ACE were children or adolescents. Seizures began in childhood in 78% of those diagnosed. An episode of status epilepticus was recalled by 36% cases, with an episode of status epilepticus precipitated by fever in 26%. Overall 169 had an abnormal electroencephalogram, 29% had focal features, 34% had epileptiform activity. In the 146 individuals who reported generalised tonic-clonic seizures only, 22% had focal features on their electroencephalogram. Overall 71% of patients with ACE had evidence of focal abnormality, documented by partial onset seizures, focal neurological deficits or focal abnormalities on the electroencephalogram. Increased seizure frequency was strongly associated with age and cognitive impairment in all ages and non-attendance at school in children (p < 0.01).
Discussion
Children and adolescents bear the brunt of epilepsy in a rural population in Africa. The predominance of focal features and the high proportion of patients with status epilepticus, suggests that much of the epilepsy in this region has identifiable causes, many of which could be prevented.
Keywords: epilepsy, convulsions, partial seizures, electroencephalogram, status epilepticus, sub-Saharan Africa
Introduction
Epilepsy is common in sub-Saharan Africa (SSA) but is poorly characterized (Preux and Druet-Cabanac, 2005;WHO, 2004). It is thought that the major causes differ from those in the resource rich countries, in particular infections of the central nervous system may be more common. Recently, exposure to severe malaria was associated with epilepsy (Carter et al., 2004;Ngoungou et al., 2006). Underlying causes may manifest as focal features, but in SSA these features are often difficult to elicit in the semiology because of the difficulties in language and culture perception of the symptoms. Many people with epilepsy do not use anti-epileptic drugs (AEDs) (Coleman et al., 2002;Meinardi et al., 2001;Scott et al., 2001;WHO, 2004), thus the considerable treatment gap increases the likelihood of a poor outcome. Also the common co-morbidities of epilepsy; cognitive, behavioural and motor impairments are poorly described in studies from SSA, and these may have a profound influence on social functioning and society’s acceptance of people with epilepsy.
Many studies that characterise epilepsy in SSA are hospital-based (Preux and Druet-Cabanac, 2005;WHO, 2004), but most people with epilepsy in SSA do not appear to use such facilities (WHO, 2004), for reasons of availability, cost or trust in the service (Mbuba et al., 2008). Thus the data based on hospital studies may not reflect the situation that many people with epilepsy encounter in SSA, particularly in rural areas. The studies that have been conducted in rural areas, either do not describe the features of epilepsy (Birbeck and Kalichi, 2004) or have not been conducted in malarious areas (Tekle-Haimanot et al., 1990). In recent studies of epilepsy in areas of Africa with malaria transmission, most seizures were reported as generalised (Dent et al., 2005;Ndoye et al., 2005;Winkler et al., 2009), but electroencephalography could have identified partial seizures (Kaiser et al., 2000), suggesting focal damage.
This study provides a detailed descriptive analysis of the demographic and clinical characteristics of people with active convulsive epilepsy (ACE) aged 6 years and above, identified during a large community-based survey in a rural malaria endemic area of Kenya (Edwards et al., 2008). In particular we wanted to determine the prevalence of focal features with electroencephalographic facilities available.
Methods
Study Population
This study was conducted in Kilifi District, a rural area on the coast of Kenya. An area of 891 km squared has been mapped and forms part of a demographic surveillance system (DSS) including re-enumeration every 4 months. Kilifi is the second poorest district within Kenya where income comes mainly from subsistence farming with low adult literacy and poor access to sanitation facilities. Malaria is endemic and pneumonia or bacteraemia are also common cause for admission to Kilifi District Hospital, the primary hospital for the district7,8.
A large community-based screening survey was carried out in 2003 to identify people with ACE. The survey had two screening stages and a third and final diagnostic stage. During phase I, 151,408 individuals were screened by the census team during enumeration, using two questions with a sensitivity of 95% to identify individuals who experienced convulsions(Edwards et al., 2008). In Stage II, responses to Stage I questions were confirmed and additional questions asked to individuals experiencing convulsions, by fieldworkers more experienced with epilepsy screening, in order to improve specificity for the final diagnostic stage. During Stage III, a detailed medical history was taken by a clinician in the local language to make a diagnosis and classify epilepsy. All case notes were reviewed by a panel of neurologists (TK, JWS, BGN, CRN) to confirm diagnoses and seizure classification.
The survey identified 445 individuals aged 6 years and over, who were resident within the study area with ACE. Specificity of Stage II screening questions was high (95%) but stigma related non-response led to predictions of missed cases in specific parts of the large study area (Edwards et al., 2008). Detailed results regarding the prevalence, treatment gap and also risk factors from a nested case-control study are reported elsewhere (Edwards et al., 2008).
Definition of Active Convulsive Epilepsy
Two or more unprovoked convulsions, with one occurring within 12 months prior to Phase III, based on the most recent International League Against Epilepsy (ILAE) definition of active epilepsy at the time of study design (ILAE, 1997) and criteria for offering anti-epileptic drugs (AED) to patients in Kenya (Dekker, 1998;MOH, 1994). Individuals under 6 years were excluded in Phase II due to difficulty in differentiating between febrile seizures and epilepsy in younger children (El Sharkawy et al., 2006).
Seizure types were classified according to the ILAE criteria(ILAE, 1981). Cognitive impairment was assessed by the local clinician through assessing the patient’s response to questions (including person, place and time) and ease of following instructions. An electroencephalogram (EEG) was recorded for 30 minutes from 16 leads using the 10-20 system, with photic stimulation and hyperventilation. All EEGs were interpreted by an experienced neurophysiologist (SW) who classified the EEGs as normal or abnormal, identified focal features and epileptiform activity.
A blood sample was taken from those who gave consent, to test for levels of Phenobarbitone. Samples were also tested for Phenytoin but only if use was reported, due to financial limitations. Drug levels were measured with TDxFLx® fluorescence polarization immunoassay (Abbott Laboratories, Diagnostics Division, Abbott Park IL, USA) which detects concentrations of at least 10 mg/L in Phenobarbitone and Phenytoin. For the purposes of this study, an optimal level of Phenobarbitone was defined as 10 – 30 mg/L and for Phenytoin, 10 – 20 mg/L (Perucca, 2004).
Data Analysis
Data were double-entered and validated using Visual FoxPro v9.0 (Microsoft) and analysed using Stata, v9 (Stata Corporation, Texas USA). Comparisons of age and age at onset of seizures were compared using Mann-Whitney tests since data were not normally distributed. Categorical data were tabulated and compared using chi-squared test overall and for trend where appropriate. Seizure frequency was categorised into 5 groups; seizures occurring daily, weekly and monthly seizures and last seizure occurring 2-6 months or 7-12 months prior to diagnosis.
Ethical clearance
This study was approved institutional review boards in the United Kingdom (Institute of Child Health and London School of Hygiene and Tropical Medicine) and Kenya (Kenyan National Ethics Review Board and University of Nairobi). The patients or their guardians gave consent for participation in the study.
Results
Demographic characteristics
Of the 445 people, aged 6 years and over, diagnosed with ACE during the final phase of the screening survey, 225 (50.6%) were male. The overall median age was 18 years (IQR: 12 to 29 years) and the age distribution did not vary significantly by gender (Mann-Whitney z = 1.410, p = 0.158).
Seizure History
The age at onset of seizures was reported by 428 (96.2%) cases of ACE. The first seizure occurred before the age of 6 years in 228 (51.2%) cases, before the age of 13 years in 296 (66.5%) and before the age of 18 years in 346 (77.8%). There was no significant difference in age at onset by gender (Mann-Whitney z = 1.354, p = 0.176). An episode of status epilepticus (SE) was recalled by 161 (36.2%) people with epilepsy, with the episode precipitated by fever by 118 (26.5%). For a further 125 (28.1%), history of reported SE was not available. A history of SE was significantly higher in children (55.9%), than in adults (18.1%) (chi-squared = 56.2, p<0.001).
Classification of Seizures & EEG results
A single seizure type was determined in 322 (72.4%) people with ACE, two seizure types in 113 (25.4%) and three seizure types in 9 (2.0%) people. Partial evolving into generalised seizures (PSGS) and primary generalised tonic-clonic seizures (GTCS) were the most common seizures experienced (Table 1) with almost half of all cases experiencing each type. Simple partial and complex partial seizures were classified in fewer cases (12.8% and 20.9% respectively) and non-convulsive seizures classified in less than 3%. The proportion of adults and children experiencing each seizure type, as listed in Table 1, did not differ significantly (chi-squared p > 0.3).
Table 1. Seizure types in 445 people with ACE.
| Types of seizure | Number identified from clinical history* n (%) |
Children* n (%) |
Adults* n (%) |
|---|---|---|---|
| Simple Partial | 57 (13.0) | 4 (1.9) | 7 (3.1) |
| Complex Partial | 93 (20.9) | 26 (12.4) | 15 (6.8) |
| Partial Seizures evolving into Generalised Seizure |
189 (42.6) | 77 (36.8) | 88 (38.6) |
| Primary Generalised Tonic-clonic |
214 (48.2) | 90 (43.1) | 115 (50.4) |
| Other Convulsive† | 9 (2) | 8 (3.8) | 0 (0) |
| Non-Convulsive‡ | 10 (2.3) | 3 (1.4) | 3 (1.3) |
| Unclassifiable | 2 (0.5) | 1 (0.5) | 0 (0) |
| Total | 545 | 209 | 228 |
Number (%) of all people with ACE; categories not mutually exclusive
Other convulsive seizures were defined where there was insufficient information to classify seizures as tonic-clonic, PSGS or simple partial.
Non-convulsive seizures included atonic or tonic seizures.
EEG examination was performed in 408 (91.7%) of cases. Age was associated with non consent for EEG examination (p = 0.017), 55.6% of those not consenting were children aged 6 – 12 years. Refusal for EEG occurred in more males than females (63.9% versus 36.1%) but evidence of an association was not strong (p = 0.095). Overall 169 had an abnormal EEG, 117 (28. 7%) had focal features, 139 (34.1%) had epileptiform activity (Table 2). Of the 214 individuals with GTCS, 51 (26.6%) had focal features on their EEG. In the 146 individuals who reported GTCS only (without any partial seizures), 36 (22.0%) of these had focal features on their EEG, suggesting that these seizures were PSGS. Abnormal responses to photosensitivity were uncommon.
Table 2. Seizure types and electroencephalographic findings.
| Electroencephalogram readings‡ | ||||||
|---|---|---|---|---|---|---|
| Type of seizure | Number identified from clinical history* |
Abnormal EEG n (%) |
Focal Features n (%) |
Epileptiform activity† n (%) |
Abnormal photosensitivity response, n (%) |
Not tested, n (%) |
| Simple Partial | 57 (12.8) | 25 (43.9) | 19 (33.3) | 21 (36.8) | 3 (5.3) | 5 (8.8) |
| Complex Partial | 93 (20.9) | 35 (37.6) | 25 (26.9) | 32 (34.1) | 1 (1.1) | 7 (7.5) |
| Partial Seizures evolving into Generalised Seizure |
189 (42.5) | 77 (40.7) | 58 (31.2) | 63 (33.3) | 3 (1.7) | 13 (6.9) |
| Primary Generalised Tonic-Clonic |
214 (48.1) | 79 (36.9) | 51 (23.8) | 65 (30.4) | 6 (2.8) | 22 (10.3) |
| Other Convulsive§ | 9 (2.0) | 1 (11.1) | 1 (11.1) | 1 (11.1) | 0 | 1 (11.1) |
| Non Convulsive | 11 (2.5) | 2 (18.2) | 2 (18.2) | 1 (9.1) | 0 | 1 (9.1) |
| Unclassifiable | 2 (0.5) | 0 | 0 | 0 | 0 | 0 |
Number (%) of 445 people with ACE; categories not mutually exclusive
includes spikes, sharp waves, spike and wave, rhythmic runs
Number (%) of people experiencing each seizure type
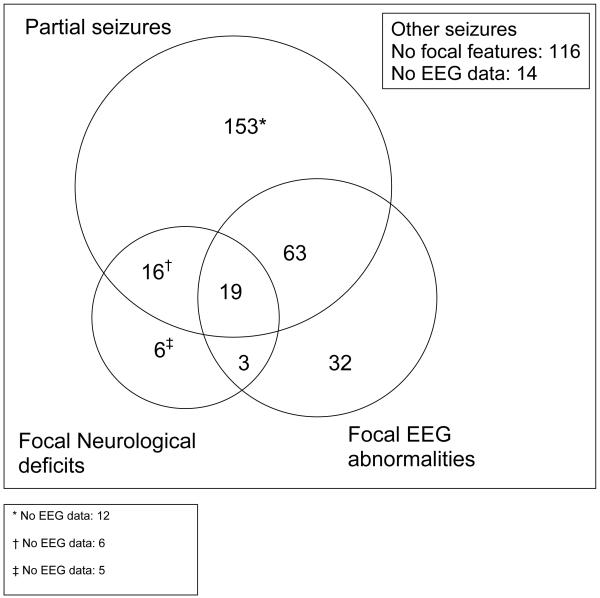
On neurological exam, 55 (12.4%) had focal neurological signs detected on physical examination, of whom 48 have a motor deficit such as monoparesis or hemiparesis. Overall 310 (70.9%) of patients with ACE had evidence of focal abnormality, documented by partial onset seizures (PSGS or the other partial seizures), focal neurological deficits or focal abnormalities on the EEG (Figure).
Figure. Venn diagram showing evidence of focal brain damage from seizure type, physical examination and EEG abnormalities.
Use of Anti-Epileptic Drugs (AED), Seizure frequency and Consequences of ACE
Overall, 257 (57.8%) people with ACE reported very frequent seizures; 61 (13.7%) daily, 56 (12.6%) weekly and 140 (31.5%) monthly (Table 3). There was strong evidence of a difference in seizure frequency between adults and children (p = 0.008) with similar proportions of adults and children experiencing daily or weekly seizures, but more children having their last seizure more than a month previously, compared to adults. There was no difference in seizure frequency by sex (p = 0.933). Anti-epileptic drugs were detected in 132 patients; phenobarbital in 127 and Phenytoin in xxx. Seizure frequency was not associated with detection of AED in blood samples in adults (p = 0.417) or in children (p = 0.823).
Table 3. Seizure Frequency, Anti-Epileptic Drug Use and Possible Consequences of Active Convulsive Epilepsy.
| Seizure Frequency | |||||||
|---|---|---|---|---|---|---|---|
| Daily | Weekly | Monthly | Last seizure within 2 to 6 months |
Last seizure within 7 to 12 months |
Total | ||
| Children * | N = 33 | N = 24 | N = 51 | N = 97 | N = 8 | 213 | |
| AED | Not detected | 21 (63.6) | 12 (50.0) | 29 (58.6) | 59 (60.8) | 3 (37.5) | 124 |
| Detected | 4 (12.1) | 2 (8.3) | 5 (9.8) | 9 (9.3) | 1 (12.5) | 21 | |
| Optimal Range | 5 (15.2) | 7 (29.2) | 11 (21.6) | 17 (17.5) | 0 (0) | 40 | |
| Not tested | 3 (9.1) | 3 (12.5) | 6 (11.8) | 12 (12.4) | 4 (50.0) | 28 | |
| Cognitive Impairment | 14 (42.4) | 15 (62.5) | 18 (35.3) | 17 (17.5) | 0 (0) | 64 | |
| Not attending school | 25 (75.8) | 18 (75.0) | 32 (62.8) | 41 (42.3) | 1 (12.5) | 117 | |
| Adults * | N = 28 | N = 32 | N = 89 | N = 75 | N = 8 | 232 | |
| AED | Not detected | 18 (64.3) | 17 (53.1) | 58 (65.2) | 53 (70.7) | 6 (75.0) | 152 |
| Detected | 6 (21.4) | 9 (28.1) | 19 (21.4) | 12 (16.0) | 2 (25.0) | 48 | |
| Optimal Range | 4 (14.3) | 5 (15.6) | 7 (7.9) | 7 (9.3) | 0 (0) | 46 | |
| Not tested | 0 (0) | 1 (3.1) | 5 (5.6) | 3 (4.0) | 0 (0) | 9 | |
| Cognitive Impairment | 18 (64.3) | 11 (34.4) | 25 (28.1) | 3 (4.0) | 0 (0) | 57 | |
| Unemployed | 26 (92.9) | 26 (81.3) | 66 (74.2) | 68 (90.7) | 7 (87.5) | 250 | |
| Marital Status‡ |
Not married | 23 (82.1) | 19 (59.4) | 51 (57.3) | 25 (33.3) | 2 (25.0) | 120 |
| Married | 3 (10.7) | 6 (18.8) | 21 (23.6) | 38 (50.7) | 4 (50.0) | 72 | |
| Separated/Divorced | 1 (3.6) | 4 (12.5) | 10 (11.2) | 5 (6.7) | 0 (0) | 20 | |
| Widowed | 1 (3.6) | 3 (9.4) | 7 (7.9) | 6 (8.0) | 2 (25.0) | 19 | |
Children; 6 to 17 years, adults; 18 years and above
1 missing value for marital status in adults
On a clinical assessment, 122 (27.2%) had evidence of cognitive impairment, with no difference between children and adults. There was no difference by gender in the frequency of cognitive impairment (p = 0.256) or motor deficits (p = 0.135).
Increased seizure frequency was associated with cognitive impairment (chi-squared tests for trend p < 0.001) in both adults and children (Table 3). In adults, there was some evidence that increased seizure frequency was associated with being unemployed (p = 0.036), however cognitive impairment was not associated with unemployment (p = 0.403). Increased seizure frequency was associated with being unmarried, compared to ever having been married (p < 0.001). After taking into account seizure frequency, cognitive impairment was also associated with being unmarried (Likelihood ratio test p = 0.003).
In children, more frequent seizures were associated (p < 0.001) with non-attendance at school. Significantly fewer cognitively impaired children attend school (p < 0.001). In the 185 children whose parents gave consent for blood testing, there was no evidence of an association between AED use and school attendance (p = 0.928).
Overall, 69 (15.5%) people with ACE were recorded as having burn marks, often extensive, with significantly more in females (20.7%) than males (12.3%) (p = 0.021) and significantly more in adults (22.3%) than children (10.1%) (p = 0.001).
Other medical history and examination
A family history of unprovoked seizures was reported in approximately one third of people with ACE and a history of febrile seizures in 14% (Table 4). A dysmorphic facial appearance was found in less than 3% of people with ACE and in none were features of a neurocutaneous syndrome identified. The parents of children included in the study were asked about perinatal difficulties, among whom 15% of mothers reported problems before delivery or neonatal difficulties during or soon after birth. Serious head injuries requiring admission to hospital were reported in 8% of patients. There was no difference in the prevalence of head injuries by children and adults (p = 0.346) but weak evidence of a difference by sex in adults, with more male adults experiencing head injuries than women (12.8% versus 5.7%, p = 0.058).
Table 4. Possible aetiologies in Adults and Children.
| Children N = 213 |
Adults N = 232 |
All N = 445 |
|
|---|---|---|---|
| Neonatal difficulties | 34 (16.0) | - | |
| Past history of status epilepticus (SE)*, n (%) | 119 (55.9) | 42 (18.1) | 161 (36.2) |
| Past history of febrile status epilepticus, n (%) | 91 (42.7) | 27 (11.6) | 118 (26.5) |
| Head injury†, n (%) | 14 (6.6) | 21 (9.1) | 35 (7.9) |
| Dysmorphic facial syndrome | 9 (4.2) | 3 (1.3) | 12 (2.7) |
| Family history of convulsive seizures‡: | |||
| None reported | 138 (64.8) | 159 (68.5) | 297 (66.7) |
| First degree relatives | 57 (26.8) | 58 (25.0) | 115 (25.8) |
| Extended family | 9 (4.2) | 6 (2.6) | 15 (3.4) |
| Both first and extended relatives | 8 (3.8) | 7 (3.0) | 15 (3.4) |
| Family history of febrile seizures§ | 35 (16.4) | 28 (12.1) | 63 (14.2) |
43 missing values in children, 82 in adults
2 missing values for adults
2 missing values for adults, 1 for children
1 missing value for adults
Discussion
This study has been performed on data from people with ACE, identified through the largest door-to-door prevalence survey carried out in sub-Saharan Africa to date(Edwards et al., 2008). It demonstrates that the burden of epilepsy in this rural area lies with the adolescents and young adults, despite excluding children less than 6 years of age. A high proportion had a history of status epilepticus, often occurring in childhood, associated with a febrile illness. The high proportion of focal features in the semiology, physical examination and EEG suggest that an underlying cause may be identifiable by the use of magnetic resonance imaging. The high prevalence of status epilepticus and those with focal seizures, suggest that many cases of epilepsy may be preventable. Furthermore these patients have substantial co-morbidity in terms of neurological deficits and cognitive impairment, with reduced schooling, employment and marriage. Also they considerably under-utilise AEDs, the use of which may improve their outcome in terms of functioning within society.
Half of the cases were less than 18 years of age, with onset of seizures before the age of 18 years in two-thirds. Over half of the cases had seizures starting before 6 years of age, but it was difficult to differentiate between febrile seizures, seizures as part of acute infections and unprovoked seizures in this context. The recall for febrile status epilepticus was much better in children than adults, because the parents provided the information. The finding that over a quarter of all patients had an episode of status epilepticus associated with febrile illness, suggests that infections may be an important cause of epilepsy, particularly malaria. In other contexts febrile status epilepticus is associated with a very high rate of subsequent epilepsy (Annegers et al., 1988). We have documented a high incidence of acute symptomatic seizures (Idro et al., 2008) and convulsive status epilepticus (Sadarangani et al., 2008) in this area and found that malaria was the most common cause. Severe falciparum malaria is associated with the subsequent development of epilepsy(Carter et al., 2004;Ngoungou et al., 2006).
The proportion of patients with abnormal interictal EEG findings using a 30-minute sample without sleep in this rural population, is higher than that reported from Ethiopia(Tekle-Haimanot et al., 1990), but lower than in an area with a high prevalence of epilepsy and onchocerciasis(Kaiser et al., 2000). The EEG indicated that over a fifth of patients with GTCS only, had focal abnormalities suggesting that these seizures are likely to be partial in origin. This supports data from other parts of Africa(Kaiser et al., 2000;Tekle-Haimanot et al., 1990). The overall high prevalence of focal abnormalities would suggest insults to the brain and this is supported by the identification of adverse perinatal events (Mung’Ala-Odera et al., 2008;Sadarangani et al., 2008) and head injury as significant risk factors.
Over half children and adults had seizures more frequently than once per month with frequency associated with cognitive impairment on clinical examination. In previous studies cognitive impairment was found to be associated with behavioural difficulties and poor control of the seizures(Sillanpaa et al., 1998). The cognitive impairment may also explain the lower attendance and lack of progression in school in the children. It may also explain the difficulties in obtaining a job and reduce the prospects of marriage in the adults and possibly predict a higher mortality.
In these patients there was considerable evidence for the detrimental effects of epilepsy, in terms of physical manifestations i.e. burns, impaired schooling and reduced chances of marriage. The increased frequency of burns in females is probably related to their domestic duties of cooking over open fires. The severity of burns suggests a hidden mortality. The severe underutilisation of AED is likely to contribute to social functioning difficulties.
The causes of epilepsy could not be determined in most patients because documentation of antenatal, perinatal and postnatal events was missing and the lack of facilities for investigation. In a multivariate case-control analysis of this group of patients, family history of febrile convulsions and unprovoked seizures and adverse perinatal events were identified as independent risk factors (Edwards et al., 2008). The associations with adverse perinatal events has emerged in other studies of children in this area (Mung’Ala-Odera et al., 2008) and elsewhere(Banu et al., 2003) and needs further investigation to understand the pathogenetic relationship. In the analysis of individual cases, head injury appeared to precede the onset of epilepsy in 8% (Table 4). As nearly three-quarters of the patients had focal features from the semiology of their seizures, on the EEG and/or focal neurological deficits, this would suggest that many other causes may be found with neuro-imaging, particularly magnetic resonance.
The epidemiological study screened only for convulsive seizures in order to identify those at highest risk in terms of mortality and comorbidity and therefore those in greatest need of diagnosis and treatment. Hence, this study under-estimated non-convulsive epilepsies e.g. absences, which were only recognised in addition to convulsive seizures. Undetected cases of all ages, due to stigma related non-response in early screening phases of the prevalence survey, may mean that the prevalence of certain characteristics within cases of ACE has been underestimated here. Recall bias is likely, particularly in adults who did not have a guardian available to provide additional information. The classification of seizure types and the determination of the onset of unprovoked seizures may also have been influenced by a lack of additional information. The cultural perceptions of symptoms may have influenced the diagnosis and classification of epilepsy. The clinical assessment of cognition is likely to have underestimated the prevalence of cognitive impairment. Finally we examined only children greater than 6 years since there are difficulties in differentiating febrile seizures from epilepsy.
Despite these limitations, it is clear that epilepsy affects mainly children and young adults in this part of Africa, and that it has a profound impact on their functioning in society, reducing their chances for attending school, obtaining a job and getting married. There is considerable co-morbidity in terms of cognitive impairment and physical manifestations such as burns. The lack of evidence of an association between AED use and seizure frequency further highlights the need for increased awareness of epilepsy as a treatable condition. The high proportion of focal features in these patients suggests that a cause of the epilepsy could be identified with further investigation particularly neuro-imaging. These findings together with the high prevalence of febrile status epilepticus suggests that much epilepsy could be prevented in this area.
ACKNOWLEDGEMENTS
We thank the staff of the KEMRI unit at Kilifi, particularly Godfrey Otieno and the epilepsy field team led by Francis Yaah. This paper is published with the permission of the Director, KEMRI. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
This work received financial support from KEMRI and Wellcome Trust through grants to Professor C.R.J.C Newton (WT083744) as part of the Wellcome Trust Senior Research fellow programme.
Footnotes
Disclosure of Conflicts of Interest
None of the authors has any conflict of interest to disclose in connection with this paper.
Reference List
- Annegers JF, Hauser WA, Beghi E, Nicolosi A, Kurland LT. The risk of unprovoked seizures after encephalitis and meningitis. Neurology. 1988;38:1407–1410. doi: 10.1212/wnl.38.9.1407. [DOI] [PubMed] [Google Scholar]
- Banu SH, Khan NZ, Hossain M, Jahan A, Parveen M, Rahman N, Boyd SH, Neville B. Profile of childhood epilepsy in Bangladesh. Dev Med Child Neurol. 2003;45:477–482. doi: 10.1017/s0012162203000884. [DOI] [PubMed] [Google Scholar]
- Birbeck GL, Kalichi EM. Epilepsy prevalence in rural Zambia: a door-to-door survey. Trop Med Int Health. 2004;9:92–95. doi: 10.1046/j.1365-3156.2003.01149.x. [DOI] [PubMed] [Google Scholar]
- Carter JA, Neville BG, White S, Ross AJ, Otieno G, Mturi N, Musumba C, Newton CR. Increased prevalence of epilepsy associated with severe falciparum malaria in children. Epilepsia. 2004;45:978–981. doi: 10.1111/j.0013-9580.2004.65103.x. [DOI] [PubMed] [Google Scholar]
- Coleman R, Loppy L, Walraven G. The treatment gap and primary health care for people with epilepsy in rural Gambia. Bull World Health Organ. 2002;80:378–383. [PMC free article] [PubMed] [Google Scholar]
- Dekker PA. Epilepsy: A manual for Medical and Clinical Officers in Kenya. 2 Ed. SMD Educative Uitgevers; 1998. [Google Scholar]
- Dent W, Helbok R, Matuja WB, Scheunemann S, Schmutzhard E. Prevalence of active epilepsy in a rural area in South Tanzania: a door-to-door survey. Epilepsia. 2005;46:1963–1969. doi: 10.1111/j.1528-1167.2005.00338.x. [DOI] [PubMed] [Google Scholar]
- Edwards T, Scott AG, Munyoki G, Odera VM, Chengo E, Bauni E, Kwasa T, Sander LW, Neville BG, Newton CR. Active convulsive epilepsy in a rural district of Kenya: a study of prevalence and possible risk factors. Lancet Neurol. 2008;7:50–56. doi: 10.1016/S1474-4422(07)70292-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Sharkawy G, Newton C, Hartley S. Attitudes and practices of families and health care personnel toward children with epilepsy in Kilifi, Kenya. Epilepsy Behav. 2006;8:201–212. doi: 10.1016/j.yebeh.2005.09.011. [DOI] [PubMed] [Google Scholar]
- Idro R, Gwer S, Kahindi M, Gatakaa H, Kazungu T, Ndiritu M, Maitland K, Neville BG, Kager PA, Newton CR. The incidence, aetiology and outcome of acute seizures in children admitted to a rural Kenyan district hospital. BMC Pediatr. 2008;8:5. doi: 10.1186/1471-2431-8-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ILAE Proposal for revised clinical and electroencephalographic classification of epileptic seizures. Epilepsia. 1981;22:489–501. doi: 10.1111/j.1528-1157.1981.tb06159.x. [DOI] [PubMed] [Google Scholar]
- ILAE The epidemiology of the epilepsies: future directions. Epilepsia. 1997;38:614–618. [PubMed] [Google Scholar]
- Kaiser C, Benninger C, Asaba G, Mugisa C, Kabagambe G, Kipp W, Rating D. Clinical and electro-clinical classification of epileptic seizure in west Uganda. Bull Soc Pathol Exot. 2000;93:255–259. [PubMed] [Google Scholar]
- Mbuba CK, Ngugi AK, Newton CR, Carter JA. The epilepsy treatment gap in developing countries: A systematic review of the magnitude, causes, and intervention strategies. Epilepsia. 2008;49:1491–1503. doi: 10.1111/j.1528-1167.2008.01693.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinardi H, Scott RA, Reis R, Sander JW. The treatment gap in epilepsy: the current situation and ways forward. Epilepsia. 2001;42:136–149. doi: 10.1046/j.1528-1157.2001.32800.x. [DOI] [PubMed] [Google Scholar]
- MOH . Clinical Guidelines - For Diagnosis and Treatment of Common Hospital Conditions in Kenya. The Regal Press; Nairobi: 1994. [Google Scholar]
- Mung’Ala-Odera V, White S, Meehan R, Otieno GO, Njuguna P, Mturi N, Edwards T, Neville BG, Newton CR. Prevalence, incidence and risk factors of epilepsy in older children in rural Kenya. Seizure. 2008;17:396–404. doi: 10.1016/j.seizure.2007.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndoye NF, Sow AD, Diop AG, Sessouma B, Sene-Diouf F, Boissy L, Wone I, Toure K, Ndiaye M, Ndiaye P, de Boer H, Engel J, Mandlhate C, Meinardi H, Prilipko L, Sander JW. Prevalence of epilepsy its treatment gap and knowledge, attitude and practice of its population in sub-urban Senegal an ILAE/IBE/WHO study. Seizure. 2005;14:106–111. doi: 10.1016/j.seizure.2004.11.003. [DOI] [PubMed] [Google Scholar]
- Ngoungou EB, Dulac O, Poudiougou B, Druet-Cabanac M, Dicko A, Mamadou TA, Coulibaly D, Farnarier G, Tuillas M, Keita MM, Kombila M, Doumbo OK, Preux PM. Epilepsy as a consequence of cerebral malaria in area in which malaria is endemic in Mali, West Africa. Epilepsia. 2006;47:873–879. doi: 10.1111/j.1528-1167.2006.00558.x. [DOI] [PubMed] [Google Scholar]
- Perucca E. General principles of medical management. In: Shorvon S, Perucca E, Fish DR, Dodson WE, editors. The Treatment of Epilepsy. 2nd Ed. Balckwell Science; Malden: 2004. pp. 139–173. [Google Scholar]
- Preux PM, Druet-Cabanac M. Epidemiology and aetiology of epilepsy in sub-Saharan Africa. Lancet Neurol. 2005;4:21–31. doi: 10.1016/S1474-4422(04)00963-9. [DOI] [PubMed] [Google Scholar]
- Sadarangani M, Seaton C, Scott JA, Ogutu B, Edwards T, Prins A, Gatakaa H, Idro R, Berkley JA, Peshu N, Neville BG, Newton CR. Incidence and outcome of convulsive status epilepticus in Kenyan children: a cohort study. Lancet Neurol. 2008;7:145–150. doi: 10.1016/S1474-4422(07)70331-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott RA, Lhatoo SD, Sander JW. The treatment of epilepsy in developing countries: where do we go from here? Bull World Health Organ. 2001;79:344–351. [PMC free article] [PubMed] [Google Scholar]
- Sillanpaa M, Jalava M, Kaleva O, Shinnar S. Long-term prognosis of seizures with onset in childhood. N Engl J Med. 1998:1715–1722. doi: 10.1056/NEJM199806113382402. [DOI] [PubMed] [Google Scholar]
- Tekle-Haimanot R, Forsgren L, Abebe M, Gebre-Mariam A, Heijbel J, Holmgren G, Ekstedt J. Clinical and electroencephalographic characteristics of epilepsy in rural Ethiopia: a community-based study. Epilepsy Res. 1990;7:230–239. doi: 10.1016/0920-1211(90)90020-v. [DOI] [PubMed] [Google Scholar]
- Belhocine M, de Boer H, Mandlhate C, editors. WHO. Epilepsy in the WHO African region: bridging the gap. World Health Organization; Geneva: 2004. [Google Scholar]
- Winkler AS, Kerschbaumsteiner K, Stelzhammer B, Meindl M, Kaaya J, Schmutzhard E. Prevalence, incidence, and clinical characteristics of epilepsy--a community-based door-to-door study in northern Tanzania. Epilepsia. 2009;50:2310–2313. doi: 10.1111/j.1528-1167.2009.02184.x. [DOI] [PubMed] [Google Scholar]