Abstract
Objectives
This report presents, for the first time, findings on the vox populis as to who constitutes the ‘vulnerables in biomedical research’.
Methods
The 3-City Tuskegee Legacy Project (TLP) study used the TLP Questionnaire as administered via RDD telephone interviews to 1,162 adult Blacks, non-Hispanic Whites, and two Puerto Rican (PR) Hispanic groups: Mainland U.S. and San Juan (SJ) in 3 cities. The classification schema was based upon respondents’ answers to an open-ended question asking which groups of people were the most vulnerable when participating in biomedical research.
Results
Subjects provided 749 valid open-ended responses which were grouped into 29 direct response categories, leading to a 4 tier classification schema for vulnerability traits. Tier 1, the summary tier, had five vulnerability categories: 1) Race/ethnicity; 2) Age; 3) SES; 4) Health; and, 5) Gender. Blacks and Mainland U.S. PR Hispanics most frequently identified Race/Ethnicity as a vulnerability trait (42.1% of Blacks and 42.6% of Mainland U.S. PR Hispanics vs. 15.4% of Whites and 16.7% of San Juan R Hispanics) (p<.007), while Whites and SJ PR Hispanics most frequently identified Age (48.3% and 29.2%) as a vulnerability trait.
Conclusions
The response patterns on ‘who was vulnerable’ were similar for the two minority groups (Blacks and Mainland U.S. PR Hispanics), and notably different from the response patterns of the two majority groups (Whites and SJPR Hispanics). Further, the vox populis definition of vulnerables differed from the current official definitions as used by the U.S. federal government.
Keywords: sensitive population groups, disadvangtage, minoritities, minority subject recruitment, health disparities, biomedical research, and bioethics
INTRODUCTION
Public health research, by definition, is focused largely on the health needs and health access issues of the needy and the underserved in society. In the U.S. eras of studies of the poor were followed by decades of study of disadvantaged minorities, with this line of research today under the umbrella term of ‘health disparities’. Whatever the label-of-the-day in this chain of evolving era-specific terminology, this honorable and much needed line of health research has focused on studying health issues in ‘the vulnerables’ in society.
The Department of Health and Human Services (HSS), through its Office of Human Research Protection (OHRP), has formally defined, and thereby set U.S. national standards, for who constitutes the ‘vulnerable populations’ in biomedical research in its Code of Federal Guidelines for the Protection of Human Subjects document (1). Another formal definition of ‘vulnerable populations’ has been offered by the National Library of Medicine in their Medical Subject Heading (MeSH) database (2). Informally, one could construct the collective, albeit indirect ‘voice’ of the researchers themselves on defining ‘vulnerables in research’ by making a comprehensive list of ‘populations studied’ in the 3,605 articles identified via a PubMed search guided by the term ‘vulnerable populations’ (3). In fact, there is among those 3,605 articles only a very limited literature which directly focused on defining who constituted the ‘vulnerables’ in which authors present concepts or definitions of ‘vulnerables’ based on either ‘a researcher's perspective’ or ‘a public health practitioner's perspective’ (4-9). However, not one of those 3,605 citations identified a published article that sought and reported on the ‘voice of the people’ (i.e., voice of the common man or the vox populis) as to whom they considered to be the ‘vulnerables in biomedical research’.
Thus while various U.S. governmental branches, such as NIH and the National Library of Medicine, have formally weighed in with who constitutes the ‘vulnerables’ in biomedical research, and researchers have informally made (if not formally announced) their choices, the literature is silent as to the vox populis on this major societal issue in our democratic society. The primary aim of this analysis is to present, for the first time, findings on the vox populis as to who constitutes the ‘vulnerables in biomedical research’ as defined by a random sample of adults in three U.S. cities.
METHODS
This report uses data from the 3-City Tuskegee Legacy Project (TLP) study, which administered the Tuskegee Legacy Project (TLP) Questionnaire via random-digit-dial Computer Assisted Telephone Interviews (CATI) to Blacks, non-Hispanic Whites, and Puerto Rican Hispanics aged 18 years and older in 3 cities (New York City, New York; Baltimore, Maryland; and San Juan, Puerto Rico) (10-12). The 60-item TLP Questionnaire used in that study probed a number of topics related to an individual's willingness to participate in biomedical research, and the factors that might influence that willingness within the same research protocol in all three cities. Previous publications provide all the details on the development, methodological approach, and respondent demographics, as well as research findings, for this 3-City TLP Study which, as a major project within an NIDCR/NIH funded Oral Health Disparities Research Center, was the second TLP Study conducted (10-12). Additional methodological decisions related to use of the TLP Questionnaire can also be found in a set of publications from its antecedent study, the 4-City TLP Study, which had been conducted within an NIDCR/NIH funded Minority Oral Health Research Center between 1992-98 (13-19).
To identify ‘vulnerability traits’, all subjects giving ‘No’ responses to the lead-in question taken from the TLP Questionnaire, “Do you believe that it is equally safe for all groups to participate in medical research studies?” were asked an open-ended follow-up question to probe to identify vulnerable, or at-risk, groups. No definition or guidance was given to subjects on the meaning of the word ‘safe’ in the opening ‘lead-in’ question to ensure each subject would interpret it as broadly as possible in order to ensure the widest range of detailed responses to the critical follow-up question in which they were asked to identify vulnerable, or at-risk, groups. Individuals surveyed were probed to exhaustion by the interviewer (i.e. by asking “Any others?”) to ensure that everyone was given the opportunity to fully list as many “at risk” groups as they could.
A classification schema (Table 1) was then created, via a series of group discussions among two dental summer research students and the senior investigator to categorize all recorded open-ended responses, with disagreements actively debated until a consensus was reached. The classification schema of vulnerability traits was built from the ‘bottom-up’. i.e., all valid responses as directly stated by the subjects were first put into direct response categories, grouping responses that conveyed the exact same meaning. The nearly 750 individual responses provided by respondents to this open-ended question led to the creation of 29 direct response categories which were, in turn, organized to create the final classification hierarchy resulting in a classification schema with four Tiers, as shown in Table 1. The 29 direct response categories derived directly from respondents’ answers are marked with asterisks in Table 1; any category in Table 1 without an asterisk indicates it was a higher and summative category created by the research team (i.e., all categories in Tier 1 and three categories in Tier 2). The goal was to organize the full range of responses into meaningful categories of ‘vulnerability’ to allow for an insightful analysis of the findings. The end result of this process, as shown in Table 1, lead to the creation of 5 Tier 1 categories of vulnerable traits: 1) Race/ethnicity Vulnerability; 2) Age Vulnerability; 3) SES Vulnerability; 4) Health Vulnerability; and 5) Gender Vulnerability. Note that the numbers given with any term are the number of subjects (and not the number of responses, as some subjects gave more than one response), so all numbers within any given Tier do not add up to, nor predict, the sum for any other Tier.
TABLE 1.
Vulnerability Traits Classification Schema
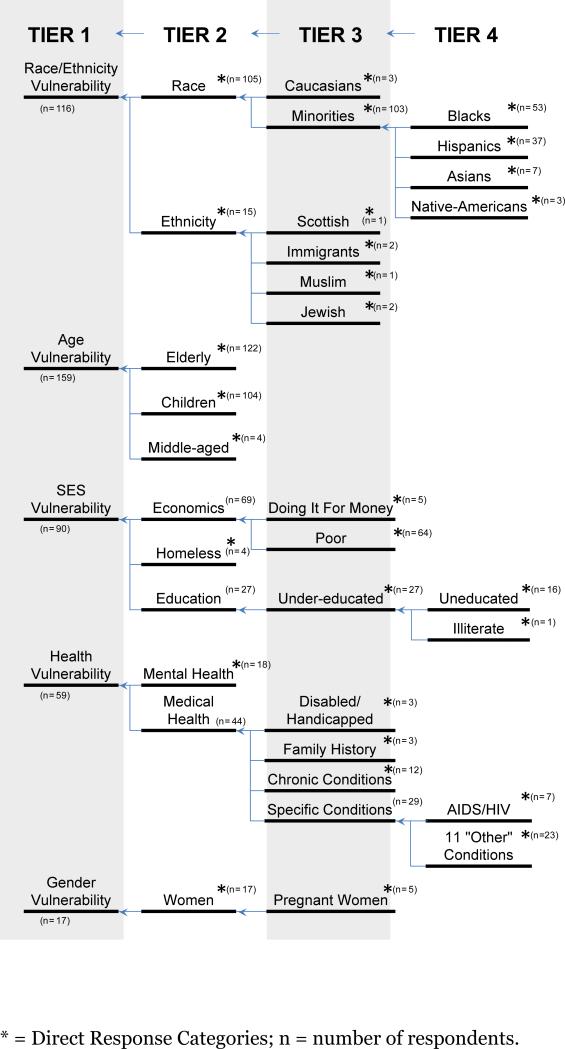
|
The creation of this classification schema initially involved skimming through the complete list of responses and identifying clusters of popular responses with the same meaning in which we classified as distinct categories. For instance, we took “African-Americans”, “Afro-Americans”, and “Blacks” as being the same response in meaning, albeit not in precise words. These three distinct direct responses from respondents were then lumped together into the direct response category of ‘Blacks’, a Tier 4 category which was subsequently lumped with 3 other related Tier 4 direct response categories (Hispanics, Asians, and Native Americans) to create a Tier 3 category labeled ”Minority”. In turn this Tier 3 category of ”Minority” was combined with another Tier 3 category of ‘Caucasian’ to form a Tier 2 category of ‘Race’. In the final step to create the Tier 1 category, this Tier 2 category of ‘Race’ was combined with a related Tier 2 category of Ethnicity to create the final Tier 1 category of ”Race/ethnicity” as an identified vulnerable group for the final analyses.
A few direct response categories as stated by respondents had multiple words that fit into two different categories, e.g., the direct response of “poor minorities” fit into two of our direct response categories: “poor” and “minorities”. In such cases, a decision was made to enter this single response into both of the direct response categories (i.e., in both the ”poor” and ”minorities” categories). This decision is in keeping with the overall goal of this analysis, i.e., to have the vox populis identify those characteristics that would make one “vulnerable” in biomedical research.
Initially planned statistical analyses consisted of an overall Chi-squared analysis to compare the distribution of response frequencies identifying the five Vulnerability Traits across the three ethnic/racial groups that served as the sampling frame for this study, i.e., Blacks, non-Hispanic Whites, and Puerto-Rican Hispanics . Subsequent analyses dichotomized this latter group into those living in Puerto Rico and those living in the U.S. mainland.
RESULTS
In this 3-City TLP study, the TLP Questionnaire was administered to 1162 adults (356 Blacks, 313 Puerto Rican (PR) Hispanics, and 493 non-Hispanic Whites) in New York City, New York; Baltimore, Maryland; and San Juan (SJ), Puerto Rico. Response rates for the 3 cities were 44%, 51%, and 52%, respectively. The 313 Puerto Rican Hispanics were comprised of 157 Puerto Ricans living on the U.S. mainland (150 New York Puerto Ricans + 7 Baltimore Puerto Ricans) and 156 San Juan Puerto Ricans. While Puerto Rican Hispanics are identified as a minority group on the US mainland (Mainland U.S. PR Hispanics), San Juan Puerto-Rican (SJPR) Hispanics are not so designated within Puerto Rico. These two groups were analyzed separately to avoid masking any possible differences due to the self-perception factor of being a minority or majority population in their place of residence.
Of the 1162 adults surveyed, 37.2% (n=432) answered “No” to the lead-in question (Q29), “Do you believe that it is equally safe for all groups or types of people to volunteer for medical research studies,” and provided at least one response to the open-ended follow-up question (Q30), “Which groups or type of people do you feel are at greater risk.” Of the 432 valid responses, 126 were from Blacks, 201 were from Whites, 57 were from Mainland U.S. PR Hispanics, and 48 were from San Juan PR (SJPR) Hispanics.
The first detailed analysis, conducted to determine the number of responses to Q30, revealed that the majority of the respondents provided 1- 2 responses to the open-ended question; i.e., 82.5% of Blacks, 77.6% of Whites, 87.5% of SJPR Hispanics, and 83.3% of Mainland U.S. Hispanics. The remaining respondents within each of the four ethnic/racial groups provided between 3 and 5 responses to this open-ended question. Table 1 shows the hierarchical 4 tier distribution of number of respondents who according to their specific open-ended responses.
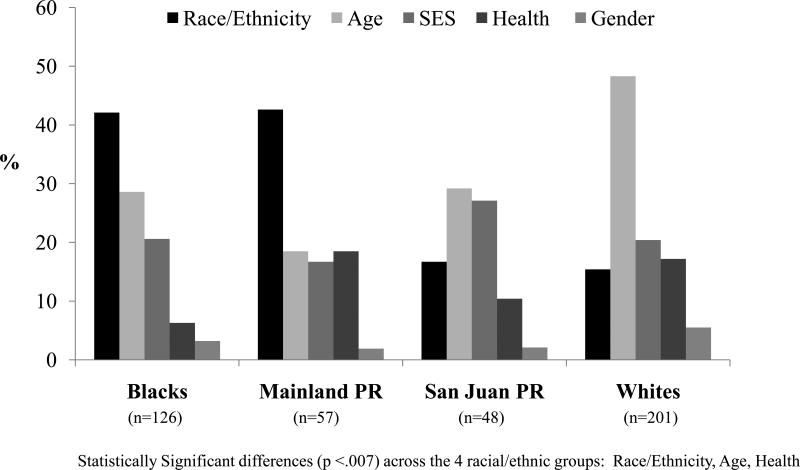
Figure 1 shows the percentage of responses provided by 432 Blacks, Mainland U.S. PR Hispanics, SJPR Hispanics, and Whites for each of the five Tier 1 Vulnerable Group Categories: Race/ethnicity, Age, Socioeconomic Status, Health, and Gender. Chi squared analyses revealed statistically significant differences across the four ethnic/racial groups in their Tier 1 answer patterns for three of the five vulnerability traits: Race, Age, and Health (all at p<.007). Only one of the 6 twoway contrasts revealed as many statistically significant differences as the overall analysis and that was the contrast between Blacks and Whites, which showed differences on the same three vulnerability traits: Whites being significantly less likely to name Race, and conversely more likely to name Age and Health (each at p<.001). The next biggest difference was detected in the contrast between Whites vs Mainland U.S. PR Hispanics, as they differed in their frequency of naming Race and Age (both at p<.000), echoing how Whites had differed from Blacks on those two vulnerability traits. SJPR Hispanics were observed to statistically differ from Blacks on the frequency of naming Race as vulnerability trait (p=.001), but they did not differ from Whites on the naming of that vulnerability trait (p=.49).
Fig 1.
Distribution of Tier 1 Vulnerability Traits as Identified by the Racial/ethnicity groups for the 432 Subjects with Valid Open-ended Responses in the 3-City TLP Study
Fig 1 clearly shows that Blacks and Mainland U.S. PR Hispanics most frequently identified Race/Ethnicity as the factor that defined being vulnerable, or “at-risk” (42.1% of Blacks and 42.6% of Mainland U.S. PR Hispanics vs. 15.4% of Whites and 16.7% of SJPR Hispanics). In contrast, Whites most frequently identified Age (48.3%) as the quality that defines at-risk group. Also, like the Whites on the US mainland, SJPR Hispanics identified Age as the most frequently named Vulnerable Group (29.2%), with SES (27.1%) as their close second response. Overall, Fig 1 shows that the response patterns for the two minority groups (Blacks and Mainland U.S. PR Hispanics) were similar and notably different from the response patterns of the two majority groups (Whites and SJPR Hispanics).
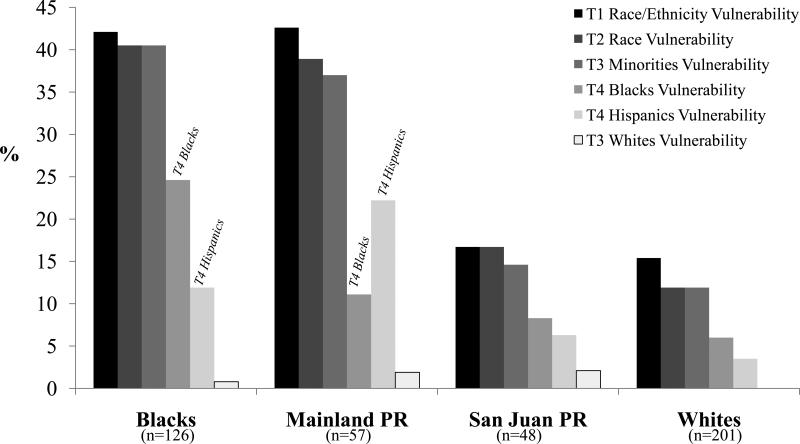
Fig 2 shows the analysis of the Tier 1 Vulnerability Trait of Race/Ethnicity across its four lower tiers for Blacks, non-Hispanic Whites, Mainland U.S. PR Hispanics and SJPR Hispanics. As was evident with the findings for Fig 1, the two self-perceived “minority status” groups (Blacks and Mainland U.S. PR Hispanics) had similar patterns of responses in identifying “vulnerability traits” and these patterns were markedly different from the self-perceived “majority status” groups (non-Hispanic Whites and SJPR Hispanics). The self-perceived “minority status” groups were more than twice as likely to identify ‘Race/Ethnicity’ as a Tier 1 vulnerability trait and to identify ‘Race’ as a Tier 2 vulnerability trait. Figure 2 also shows that Blacks and Mainland U.S. PR Hispanics, as compared to the two self-perceived ‘majority groups’, were almost three times as likely to identify their own racial/ethnic trait (Tier 4 Direct Response Category, vulnerability trait of being either Black or Hispanic) as making individuals vulnerable when participating in biomedical research studies.
Fig 2.
Distribution of the Race/Ethnicity Vulnerability Trait across Tiers 1-4 within each Racial/ethnicity Group for the 432 Subjects with Valid Open-ended Responses in the 3-City TLP Study
DISCUSSION
The United States Public Health Service (USPHS) Syphilis Study at Tuskegee, commonly referred to as the ‘Tuskegee Syphilis Study’, stands as the most egregious biomedical research study in U.S. history (20,24). That study was a 40 year epidemiological follow-up study of African American males in Alabama to observe the effects of untreated syphilis on various organ systems. Subsequent to the ending of that study in 1972, there was a widespread belief that a major legacy of that unethical research study was a strong reluctance among U.S. African Americans about participating in clinical research studies (25,26). The aftermath of the 1972 newspaper headlines which made this unethical study conducted by the U.S. government known to all across the U.S. led directly—not only to the near immediate ending of that 40 year abusive study—but was also a major factor in the establishment of our current IRB system of ethical review of proposed biomedical studies in the U.S., and subsequently around the world (27-29).
The ethical imperative for the formation of IRBs in the mid-1970s was the then clearly realized need—primarily based on the national outrage over the revelation of the USPHS Syphilis Study at Tuskegee—to formally and officially protect all participating research subjects, with special attention to protecting the most vulnerable in society. Current U.S. federal guidelines on the protection of human subjects in research state that:
“When some or all of the subjects are likely to be vulnerable to coercion or undue influence, such as children, prisoners, pregnant women, mentally disabled persons, or economically or educationally disadvantaged persons, additional safeguards have been included in the study to protect the rights and welfare of these subjects.” (30)
These U.S. federal guidelines for the protection of human subjects in research also contain special sections precisely detailing what is required for the protection of three of these named vulnerable groups with specific sections on: 1) pregnant women, human fetuses, and neonates; 2) prisoners; and 3) children (31).
Defining who constitutes the ‘vulnerable’ in biomedical research has also been done formally by the National Library of Medicine (NLM) in their Medical Subject Heading (MeSH) database where they define ‘vulnerable populations’ as “groups of persons whose range of options is severely limited, who are frequently subjected to coercion in their decision making, or who may be compromised in their ability to give informed consent.” (2) While a search for articles guided by the term ‘vulnerable populations’ produced a total listing of 3,605 articles, the vast majority of those articles were selected by the search engine based either upon ‘the population studied’ or a descriptor term used within that article which, by those authors labeling of their study subjects as ‘vulnerables’. Collectively, this latter approach of seeing which groups health researchers described as constituting ‘the vulnerables’ creates an informal, but highly operational definition of ‘vulnerables in biomedical research’. That collective voice, as summarized in a small set of articles focused directly on defining ‘vulnerable populations’ in research, largely identified the same ‘vulnerables’ as had the above OHRP, DHHS definition as appears in the U.S. federal guidelines on the protection of human subjects in research (4-9). Unexpectedly however, not one of those 3,605 citations identified an article that reported on the ‘voice of the people’ (i.e., the vox populis) as to whom they considered to be the ‘vulnerables in biomedical research’.
Interestingly, the vox populis’ list of vulnerables from this research study differed from the specifically worded lists of vulnerables as provided by the U.S. federal government (i.e., the NIH Office of Human Subject Protection (OHSP) guidelines), but reflected the ‘targeted subjects of published articles’ found under the NLM's MeSH listing for vulnerable populations. Logically, the NIH OHSP guidelines may have been intended only as ‘guidelines’ and never meant to provide a definitive list of vulnerables, and only intended to describe the characteristics of vulnerables. One might further argue, in the broadest defense of the NIH vulnerable populations definition, that its listed term of ‘economically or educationally disadvantaged persons’ might ‘cover’ minorities, but it certainly does not limit itself to ‘minorities’, as our vox populis did—given our vox populis separately listed ‘SES’ as a vulnerability trait, specifically as the 3rd most frequently cited vulnerability trait.
Regardless of whether one interprets the U.S. federal government's list of vulnerables as either highly reflective of, or differing from, the vox populis based on the overall findings from the total study sample in this study, the sub-analysis by racial/ethnic groups clarifies this issue. Our sub-analysis of the data by racial/ethnic groups clearly revealed that the two minority groups (i.e., Blacks and Mainland U.S. PR Hispanics) did differ significantly and meaningfully from the listing of the U.S. federal government as to who constitutes the vulnerables in biomedical research, as they not only listed SES as a vulnerability trait, but also (separately as well as most frequently) listed Race/Ethnicity. This would indicate that they saw SES and Race/Ethnicity as ‘separate’ traits, and hence their collective view would not support the interpretative reasoning that the phrase ‘economically or educationally disadvantaged persons’ would fully ‘cover’ minorities. Also, further evidence of this perceived difference from the U.S federal government listing by the two minority groups was provided by the fact that each minority group listed themselves as the most vulnerable group. This suggests that their prism on being vulnerable when they themselves participated in biomedical research saw something related ‘to being Black’ or ‘to being a Mainland U.S. Puerto Rican Hispanic’ separate from, and beyond, the trait of being ‘economically or educationally disadvantaged’. Likely this ‘something’ lies in the realm of racism and prejudice, an issue that goes, presumably, beyond being ‘economically or educationally disadvantaged’, per se. This same concern of Blacks and Hispanics was detected in other findings analyzed in prior publications of the Tuskegee Legacy Project, certainly in the higher measured levels on the Guinea Pig Fear Factor Scale for both of these minority groups as compared to Whites (10,15), but most overtly in previous TLP findings which reported that these two minority groups’ perceptions that they were more ‘at-risk’ than Whites when participating not only in biomedical research, but also when participating in a ‘standard of care’ cancer screening (18).
Further, the data from this study provided a unique opportunity to explore the different perspectives that are found between minorities and non-minorities. In addition to surveying Blacks and Whites, this study surveyed two additional and contrasting, Hispanic groups: SJPR Hispanics and Mainland U.S. PR Hispanics. Given the task at hand, this intra-Hispanic comparison offers the opportunity for an intriguing comparison as Mainland U.S. PR Hispanics are considered a minority in the United States, while SJPR Hispanics comprise the vast majority of people living in the US Commonwealth of Puerto Rico, i.e., they neither view themselves, nor are they viewed, as minorities in Puerto Rico.
Of the 5 major vulnerability categories found in the classification schema, both Blacks and Mainland U.S. PR Hispanics most frequently cited Race/Ethnicity as a vulnerability trait, i.e., to them, minorities were the main vulnerable group. And, at the next level of analysis, a closer look at the data revealed that each of these two minority groups selected differing minority groups as the most frequently cited vulnerable groups, with each group most frequently citing themselves as the leading vulnerable group, i.e., Blacks were more likely to identify themselves as the most cited vulnerable group, while Mainland U.S. PR Hispanics were more likely to identify themselves as the most cited vulnerable group. For both Blacks and Mainland U.S. PR Hispanics, Age Vulnerability was a distant second as a cited vulnerability after Race/ethnicity.
In contrast, White respondents most frequently cited ‘Age’ as the leading vulnerability, with Race/ethnicity ranking a very distant 4th on their most frequently cited list. For Whites, the gap between Age and even their second and third most frequently cited ‘vulnerabilities’ (of SES and Health) was very large. Interestingly, the SJPR Hispanics, showed a pattern similar to Whites, with Age as the most frequently cited vulnerability, SES as the second most frequently cited vulnerability, and Race/ethnicity ranking a distant 3rd on their list. These data seem to clearly show that Mainland U.S. PR Hispanics like Blacks, both living as minorities in the broader ethnic/cultural U.S. mainland society, firmly believe that their racial/ethnic status predisposes them to being vulnerable. This prism of perception is not the same for SJPR Hispanics who like Whites, constitute the majority in their society.
As the first study to present direct data on the vox populis as to who constitutes the vulnerables in biomedical research, one major inherent limitation in interpreting these findings is the inevitable uncertainty as to generalizability of these findings in the absence of prior similar studies. Another factor affecting the generalizability of these findings is the reality of the shrinking standard response rates to random-digit dial telephone surveys in recent years which typically yield response rates in the range of 45-60% for surveys conducted by professional, high quality national survey companies. This well recognized phenomenon, often ascribed to the increased presence of caller ID and cell phones, results in less than the ideal response rates of 75-80% which were so achieveable 20 years ago. Taken together, these factors suggest caution should be taken in having a high confidence in generalizing the findings of this study. Nevertheless, in the absence of any other studies—much less any contradictory findings , both the rigor of the pre-study protocol review at NIH and the rigor used in the conducting the ensuing study, makes it reasonable to accept and utilize these findings while acknowledging the caution due any early findings on such a complex issue.
Considering that only six decades have passed since the Brown vs Board of Education decision in 1954 initiating the U.S.'s legal commitment to ending racial segregation (32), that even less time has passed since the infamous injustice of the Tuskegee Legacy project was ended, and that race and ethnicity vulnerability in research continue to be lively topics of debate and grave concern in the U.S. today as reflected both in 1997 Clinton apology for the USPH Syphilis Study in Tuskegee (33) and in the very recent 2010 U.S. apology for our country's major role the 1944-46 Guatemalan inoculation study on syphilis (34, 35), it is perhaps no surprise that we would find a clear reflection of these perceptions of racial/ethnic inequalities in our data from the Tuskegee Legacy Project study. Even if these specific historical events are not as acutely on the forefront of the mind of most individuals, it is overtly evident that a hierarchy based on an individual's job, an individual's status in the community, an individual's racial or ethnic group, and/or an individual's social class are still ubiquitous features of life in the U.S. today. These realities of inequality very much still exist, as can be ‘heard’ via the vox populis on ‘who are the vulnerables in biomedical research’ today. Clearly, researchers need to be acutely aware of these differing perceptions as to who constitutes ‘the vulnerables’ in our population across the range of research activities spanning planning to recruitment to completion stages as they strive conduct studies that richly address the health issues of all in our diverse national population.
Acknowledgements
The authors wish to thank Mr. Shahnam Shifteh, an NYU dental student, for his contributions to the discussions which created the classification schema presented in this paper. This study was funded by the National Institute of Dental and Craniofacial Research (NIDCR) at NIH via Grant U54 DE 14257, the NYU Oral Cancer RAAHP* Center (* = Research on Adolescent and Adult Health Promotion).
REFERENCES
- 1.U.S. Department of Health and Human Services [7/19/10];Code of Federal Regulations, Title 45 Public Welfare, Part 46 Protection of Human Subjects, U.S. Office of Human Research Protection (OHRP) Revised January 15, 2009. At www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm.
- 2. [7/19/10];National Library of Medicine Medical Subject Heading (MeSH) database. at www.ncbi.nlm.nih.gov/mesh?term=vulnerable populations.
- 3.personal communication, a PubMed search under subject heading ‘vulnerable populations’ from BJ Frey, a consulting biomedical librarian in a professional email report, July 2010.
- 4.Braveman P. Health Disparities and health equity: concepts and measurement. Ann Rev Public Health. 2006;27:167–94. doi: 10.1146/annurev.publhealth.27.021405.102103. PMCID: 165331114. [DOI] [PubMed] [Google Scholar]
- 5.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006 Dec;96(12):2113–21. doi: 10.2105/AJPH.2005.077628. PMID: 17077411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hurst SA. Vulnerability in research and health care: describing the elephant in the room? Bioethics. 2008 May;22(4):191–202. doi: 10.1111/j.1467-8519.2008.00631.x. PMID: 18405317. [DOI] [PubMed] [Google Scholar]
- 7.Leffers JM, Martins DC, McGrath MM, Brown DG, Mercer J, Sullivan MC, Viau P. Development of a theoretical construct for risk and vulnerability from six empirical studies. Res Theory Nurs Prac. 2004;18(1):15–34. doi: 10.1891/rtnp.18.1.15.28060. Spring. PMID: 15083660. [DOI] [PubMed] [Google Scholar]
- 8.Purdy IB. Vulnerable: a concept analysis. Nurs Forum. 2004 Oct-Dec;39:25–33. doi: 10.1111/j.1744-6198.2004.tb00011.x. PMID: 15700483. [DOI] [PubMed] [Google Scholar]
- 9.Nyamathi A, Koniak-Griffin D, Greengold BA. Development of nursing theory and science in vulnerable populations research. Ann Rev Nurs Res. 2007;25:3–25. PMID: 17958287. [PubMed] [Google Scholar]
- 10.Katz RV, Green BL, Kressin NR, Claudio C, Wang MQ, Russell SL. Willingness of Minorities to Participate in Biomedical Studies: confirmatory findings from a follow-up study using the Tuskegee Legacy Project Questionnaire. J Natl Med Assoc. 2007;99(9):1050–62. PMCID: PMC2139897. [PMC free article] [PubMed] [Google Scholar]
- 11.Katz RV, Green BL, Kressin NR, James SA, Claudio C, Wang MQ, Russell SL. Exploring the ‘Legacy’ of the Tuskegee Syphilis Study: a follow-up study from the Tuskegee Legacy Project. J Natl Med Assoc. 2008 Feb;101(2):179–183. doi: 10.1016/s0027-9684(15)30833-6. PhD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz RV, Jean-Charles G, Green BL, Kressin NR, Claudio C, Wang MQ, Russell SL, Outlaw J. Identifying the Tuskegee Syphilis Study: implications of results from recall and recognition questions. BMC Public Health. 2009;9:468. doi: 10.1186/1471-2458-9-468. doi:10.1186/1471-2458-9-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katz RV, Kegeles SS, Green BL, Kressin NR, James SA, Claudio C. The Tuskegee Legacy Project: history, preliminary scientific findings and unanticipated societal benefits. Dental Clinics of North America. 2003;47(1):1–19. doi: 10.1016/s0011-8532(02)00049-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCallum JM, Arekere DM, Green BL, Katz RV, Rivers BM. Awareness and knowledge of the U.S.Public Health Service Syphilis Study at Tuskegee: Implications for Biomedical Research. J Health Care Poor and Underserved. 2006;17:716–733. doi: 10.1353/hpu.2006.0130. PMCID: PMC1828138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katz RV, Kegeles SS, Kressin NR, Green BL, Wang MQ, James SA, Russell SL, Claudio C. The Tuskegee Legacy Project: Willingness of Minorities to Participate in Biomedical Research. J Health Care for the Poor and Underserved. 2006;17:698–715. doi: 10.1353/hpu.2006.0126. PMCID: PMC1780164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Katz RV, Kegeles SS, Kressin NR, James SA, Green BL, Wang MQ, Russell SL, Claudio C. Awareness of the USPHS Syphilis Study at Tuskegee and the U.S. Presidential Apology and Their Influence on Minority Participation in Biomedical Research. Am J Pub Health. 2008;98:1137–1147. doi: 10.2105/AJPH.2006.100131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katz RV, Green BL, Kressin NR, Kegeles SS, Wang MQ, James SA, Russell SL, Claudio C, McCallum J. The Legacy of the Tuskegee Syphilis Study: Its Impact on Willingness to Participate in Biomedical Research Studies. J Health Care Poor and Underserved. 2008;19:1169–1181. doi: 10.1353/hpu.0.0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katz RV, Wang MQ, Green BL, Kressin NR, Claudio C, Russell SL, Sommervil C. Participation in Biomedical Research Studies and Cancer Screenings: Perceptions of Risks to Minorities. Cancer Control. 2008 Oct;15(4):344–351. doi: 10.1177/107327480801500409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Russell SL, Katz RV, Kressin NR, Green BL, Wang MQ, Claudio C, Tzvetkova K. Beliefs of Women's Risk as Research Subjects: A Four-City Study Examining Differences by Sex and by Race/Ethnicity. J Women's Health. 2009 Feb;18(2):235–243. doi: 10.1089/jwh.2007.0486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones JH. Bad Blood: the Tuskegee syphilis experiment. 1st ed. Free Press; New York: 1981. [Google Scholar]
- 21.Reverby SM, editor. Tuskegee's Truths: Rethinking the Tuskegee Syphilis Study. University of North Carolina Press; Chapel Hill, NC: 2000. Legacy Committee Request: The Tuskegee Syphilis Legacy Committee Report of 1996. pp. 559–566. [Google Scholar]
- 22.Mitchell A. The New York Times. Health Section; May 17, 1997. Clinton Regrets “Clearly Racist” U.S. Study. [Google Scholar]
- 23.Hunninghake DB, Darby CA, Probstfield JL. Recruitment experience in clinical trials: literature summary and annotated bibliography. Control Clin Trials. 1987;8(4 Suppl):6S–30S. doi: 10.1016/0197-2456(87)90004-3. [DOI] [PubMed] [Google Scholar]
- 24.Swanson MS, Ward AJ. Recruiting minorities into clinical trials: toward a participant-friendly system. J National Cancer Institute. 1995;87(23):1747–1759. doi: 10.1093/jnci/87.23.1747. [DOI] [PubMed] [Google Scholar]
- 25.Thomas SB, Quinn SC. Public Health Then and Now, The Tuskegee Syphilis Study, 1932 to 1972: Implications for HIV education and AIDS risk education programs in the black community. Am J Public Health. 1991;81(11):1498–1505. doi: 10.2105/ajph.81.11.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kressin NR, Meterko M, Wilson NJ. Participation in Biomedical Research: Are There Racial Disparities within VA? J Nat'l Med Assoc. 2000;92:62–69. [PMC free article] [PubMed] [Google Scholar]
- 27.Doing Bad in the Name of Good?: The Tuskegee Syphilis Study and its Legacy. Bioethics Symposium at the University of Virginia VA Conference; Center for Bioethics and UVA Library Historical Collections Section. 1994; [5/8/08]. { http://www.healthsystem.virginia.edu/Internet/library/wdc-lib/historical/medical-history/bad_blood/report.dfm] [Google Scholar]
- 28.Reverby SM. Introduction. More than a metaphor: an overview of the scholarship of the study. In: Reverby SM, editor. Tuskegee's Truths: rethinking the Tuskegee Syphilis Study. University of North Carolina Press; Chapel Hill,NC: 2000. p. 9. [Google Scholar]
- 29.Reverby SM. Examining Tuskegee. University of North Carolina Press; Chapel Hill, NC: 2009. [Google Scholar]
- 30.U.S. Department of Health and Human Services [7/19/10];Subpart A, Section 46.111. Criteria for IRB approval of research. Subsection b. Code of Federal Regulations, Title 45 Public Welfare, Part 46 Protection of Human Subjects, U.S. Office of Human Research Protection (OHRP) Revised January 15, 2009. At www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm.
- 31.U.S. Department of Health and Human Services [7/19/10];Subparts B, C & D, Additional Protection Sections 46.201-409. Code of Federal Regulations, Title 45 Public Welfare, Part 46 Protection of Human Subjects, U.S. Office of Human Research Protection (OHRP) Revised January 15, 2009. At www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm.
- 32.Brown vs Board of Education [10/17/10]; at http://www.archives.gov/education/lessons/brown-v-board.
- 33.Clinton W. [October 17, 2010];Presidential Apology for the U.S. Publich Health Service Syphilis Study at Tuskegee. http://www.cdc.gov/tuskegee/clintonp.htm.
- 34.McNeil DG., Jr US Infected Guatemalans with Syphilis in ‘40s. The New York Times. Oct 2, 2010. p. 1. Satuday.
- 35.Reverby SM. “Normal Exposure” and Inoculation Syphilis: a PHS “Tuskegee” Doctor in Guatemala, 1946-48. Journal of Policy History. 2011 January; (in press) [Google Scholar]