Abstract
Purpose
To determine whether waist circumference (WC) is a better predictor of insulin resistance (IR) compared with body mass index (BMI) in US adolescents 12-18 years.
Methods
Using data from the National Health and Nutrition Examination Survey (NHANES) 1999-2002, we evaluated an ethnically diverse sample of 1571 adolescents with BMI, WC, and fasting glucose and insulin levels. Children were classified as having IR if they had a homeostasis model assessment of insulin resistance (insulin (μU/ml) × glucose (mmol/l))/22.5) greater than 4.39. We created receiver operating characteristic (ROC) curves predicting IR across various thresholds of WC and BMI, and area under the curve (AUC) was compared.
Results
The prevalence of IR for the population was 11.8%. Measures of test performance (sensitivity and specificity) for predicting IR were similar for abnormal BMI and WC thresholds; i.e. thresholds of BMI 85th% and WC 75th%, and thresholds of BMI 95th% and WC 90th% were quite similar. There were no significant differences in AUC for WC versus BMI 0.85 (95% CI 0.83-0.88) (p=0.84) for the overall population or for specific racial groups.
Conclusions
WC does not appear to provide a distinct advantage over BMI for identifying adolescents with IR.
Keywords: Body Mass Index, Waist circumference, Insulin Resistance
Introduction
Given recent reports of increases in obesity and type 2 diabetes among children and adolescents in the US,[1] there is increasing interest in early identification of children with insulin resistance (IR), which represents one of the critical risk factors for development of type 2 diabetes. The clinical predictor used most widely in the primary care setting and recommended by the American Academy of Pediatrics (AAP) is body mass index (BMI).[2]
Although BMI serves as a surrogate measure of total body adiposity, abdominal adiposity, as measured by waist circumference (WC), is believed to be a more precise predictor of IR in children and adults.[3] Some authors have therefore suggested that WC be measured in clinical practice to assess chronic disease risk among children.[3] In this current study we sought to determine whether WC is a better predictor of IR compared with BMI, in a racially diverse group of US adolescents.
Materials and Methods
We used the data from National Health and Nutrition Examination Survey (NHANES) 1999-2002. A description of the examination, fasting, and laboratory procedures has been previously published.[4] WC was measured to the nearest 0.1 cm at the high point of the iliac crest. Of 4339 adolescents aged 12-18 yrs, the sample consisted of 1571 non-diabetic, non-pregnant individuals, with fasting glucose/insulin levels and not on medications that interfere with glucose metabolism. Because NHANES has separate fasting sampling weights which account for the additional stage of sampling and nonresponse, the subsample represents a nationally representative sample.
BMI and WC were converted to age and sex-specific percentiles based on CDC growth charts, or previously published[5] and validated[6] universal WC percentiles. We used a validated measure of IR, homeostasis model assessment of insulin resistance [7]:HOMA-IR=(insulin (μU/ml) × glucose (mmol/l))/22.5, and defined adolescents having IR if their HOMA-IR was greater than 4.39.[4]
Sensitivity, specificity, positive and negative predictive value for identifying adolescents with IR were calculated for each BMI and WC threshold. Receiver operating characteristic (ROC) curves predicting IR for WC and BMI were then created. Area under the curve (AUC) was calculated and statistically compared for the overall population and for racial substrata (white, black, Mexican-American). Analyses were performed using Stata 10/SE.
Results
Mean age for the population was 15.0 years, and 52.9% were male. The weighted racial distribution of the population was 63.4% white, 13.8% black, 10.7% Mexican-American, and 12.1% other race. The prevalence of IR for the population was 11.8%, with higher prevalence among black (18.6%) and Mexican-American children (16.9%) compared with white children (9.3%).
The table displays test characteristics at specific BMI and WC thresholds. For both BMI and WC, there were tradeoffs between sensitivity and specificity across the thresholds. The figure displays the ROC curves; AUC for both BMI and WC was 0.85 (95% CI 0.83-0.88) which was not statistically significant (p=0.84). A similar lack of differences was seen for the race-specific ROC curve comparisons (see appendix figures 2-4), although we do note that AUC for white children (0.89-0.90) was higher than for black (0.82-0.83) or Mexican children (0.84).
Figure 1.
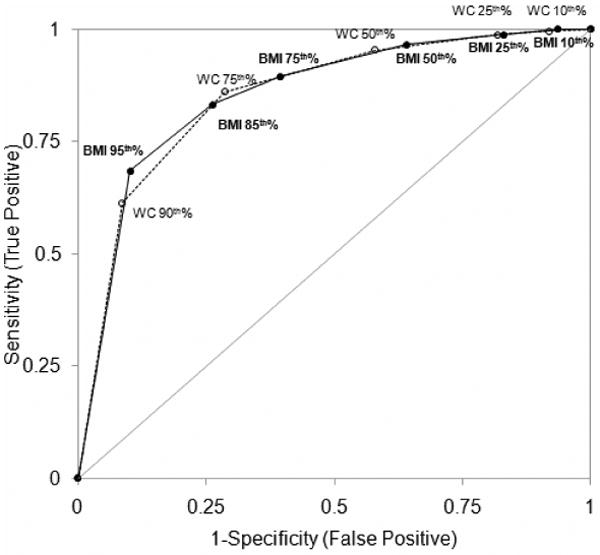
Comparison of receiver operator characteristic curves for predicting insulin resistance using body mass index versus waist circumference percentiles (AUC, 95% CI 0.83-0.88 for both) (p=0.84) (n=1571). Dark circles, solid line=body mass index; open circles, dotted line=waist circumference.
Discussion
We found that the sensitivity and specificity of the current abnormal BMI thresholds (85th% and 95th%) for predicting IR are similar to previously proposed abnormal waist circumference thresholds (75th% and 90th%)(Table 1).[6] This is reflected by the lack of significant differences in AUC, which would seem to indicate that WC percentiles do not appear to offer valuable additional information beyond that of BMI percentiles for identifying children with IR.
Table 1. Test Characteristics of Specific BMI and Waist Circumference Thresholds for Predicting Insulin Resistance.
| Body Mass Index | Waist Circumference | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI or WC Percentile Threshold | Sensitivity (True Positive Rate) |
Specificity (True Negative Rate) |
1-Specificity | Positive Predictive Value | Negative Predictive Value | Sensitivity (True Positive Rate) |
Specificity (True Negative Rate) |
1-Specificity | Positive Predictive Value | Negative Predictive Value |
| ≥10th% | 1.0 | 0.06 | 0.94 | 0.16 | 1.0 | 1.0 | 0.08 | 0.92 | 0.16 | 0.99 |
| ≥25th% | 0.99 | 0.17 | 0.83 | 0.18 | 0.99 | 0.99 | 0.18 | 0.82 | 0.18 | 0.99 |
| ≥50th% | 0.97 | 0.36 | 0.64 | 0.21 | 0.98 | 0.95 | 0.42 | 0.58 | 0.23 | 0.98 |
| ≥75th% | 0.90 | 0.61 | 0.39 | 0.29 | 0.97 | 0.86 | 0.71 | 0.29 | 0.35 | 0.97 |
| ≥85th% | 0.83 | 0.74 | 0.26 | 0.36 | 0.96 | - | - | - | - | - |
| ≥90th% | - | - | - | - | - | 0.61 | 0.91 | 0.09 | 0.56 | 0.93 |
| ≥95th% | 0.68 | 0.90 | 0.10 | 0.55 | 0.94 | - | - | - | - | - |
Our findings are consistent with previously published studies. Messiah et al. reported that BMI and WC appeared to have similar predictive capacity for identifying US adolescent children with ≥ 3 cardiovascular risk factors,[8] and investigators from other countries have demonstrated that BMI and WC display similar correlations with insulin levels and IR indices.[9]
In contrast, one previous study compared the relationship of BMI percentiles and WC with IR, as measured by the hyperinsulinemic-euglycemic clamp,[3] and found that WC remained a significant correlate of IR even after controlling for BMI percentile in multiple regression analyses. The authors therefore suggested that WC, in addition to BMI, might be a useful screening tool for detecting children with increased metabolic risk. The use of clamp studies, a more sensitive measure of IR, and the smaller sample of adolescents (56 black and 89 white youths) with a slightly lower age range (starting at 8 years) may account for some of the differences seen with our findings. Furthermore, the method of analysis may also be a factor; although WC is a statistically significant independent predictor of IR within a linear regression model, statistical significance may not translate to clinical significance.
There is increasing interest in measures of abdominal adiposity to assess for chronic disease risk in children, and providers may be unsure of whether they should be measuring BMI, WC, or both. Our findings suggest that further studies are needed before WC is included as part of routine pediatric primary care screening. Currently, the AAP recommends that primary care providers use BMI as a screening tool for identifying overweight and obese children, yet only a minority routinely follow this recommendation.[10] Given the poor adherence of providers and the additional training and time required for accurate measurement of WC in clinical practice, national organizations that issue screening guidelines should continue to encourage providers to focus on solely on BMI measurement for now.
Limitations of our study include the fact that HOMA-IR is not as sensitive as other gold standard methods such as hyperinsulinemic-euglycemic clamp. However, it would be impossible from a practical standpoint to use the above mentioned methods in large population based studies. Strengths of our study include the large representative nature of the NHANES surveys as well as the racial and ethnic diversity of our sample, which allowed us to perform separate analyses for race strata, yielding similar findings.
Conclusions
WC does not appear to provide a distinct advantage over BMI for identifying adolescents with IR in the clinical setting, although further studies are needed to confirm this finding.
Acknowledgments
This work was presented at the American Diabetes Association, June 2008. Dr. Kotlyarevska was supported by NIDDK T32DK071212.
Dr. Lee was supported by NIDDK K08DK082386 and the Clinical Sciences Scholars Program at the University of Michigan.
Abbreviations
- AUC
Area under the curve
- BMI
Body Mass Index
- IR
Insulin Resistance
- NHANES
National Health and Nutrition Examination Survey
- ROC
Receiver operating characteristic
- WC
Waist circumference
- AAP
American Academy of Pediatrics
- HOMA-IR
Homeostasis model assessment of insulin resistance
Appendix
Appendix Figure 2.
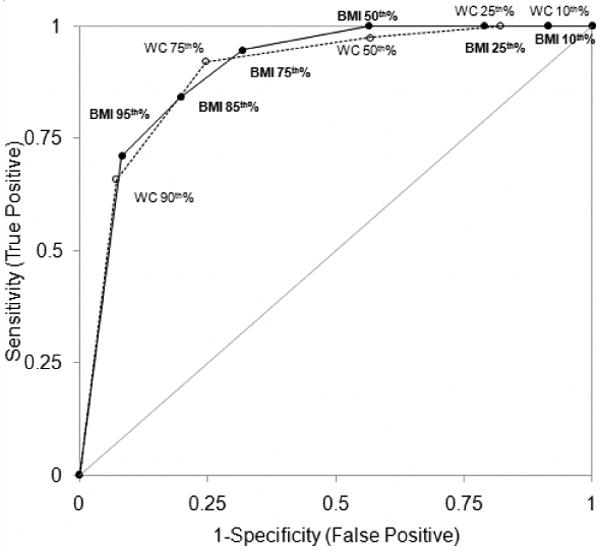
Comparison of receiver operator characteristic curves for predicting insulin resistance using body mass index (AUC 0.90, 95% CI 0.86-0.94) versus waist circumference percentiles (AUC 0.89 (95%CI, 0.85-0.94) for White children (n=428). Dark circles, solid line=body mass index; open circles, dotted line=waist circumference.
Appendix Figure 3.
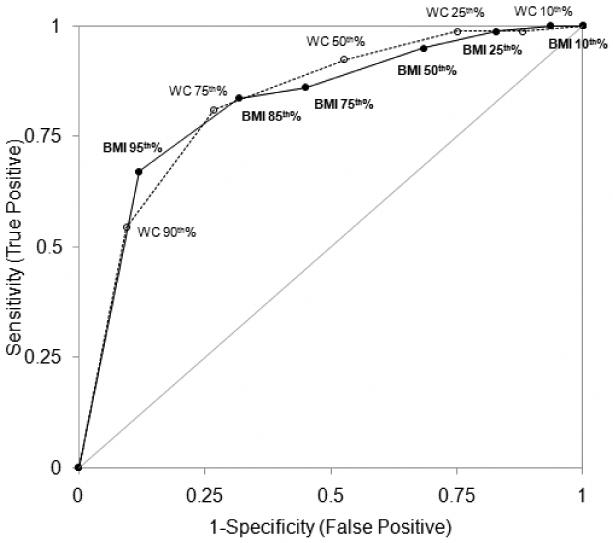
Comparison of receiver operator characteristic curves for predicting insulin resistance using body mass index (AUC 0.82, 95% CI 0.77-0.87) versus waist circumference percentiles (AUC 0.83, 95%CI 0.78-0.88) for Black children (n=439). Dark circles, solid line=body mass index; open circles, dotted line=waist circumference.
Appendix Figure 4.
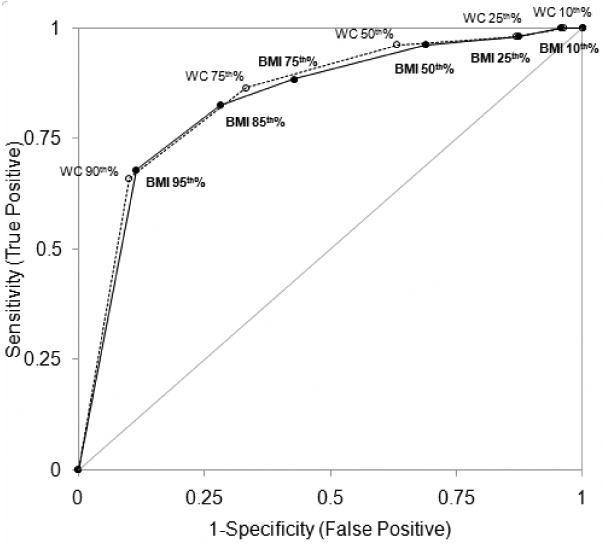
Comparison of receiver operator characteristic curves for predicting insulin resistance using body mass index (AUC 0.84, 95% CI 0.79-0.88) versus waist circumference percentiles (AUC 0.84 (95%CI, 0.80-0.88) for Mexican-American children (n=590). Dark circles, solid line=body mass index; open circles, dotted line=waist circumference.
Footnotes
Conflict of Interest: There are no competing financial interests in relation to the work described and the authors have nothing to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Pinhas-Hamiel O, Dolan LM, Daniels SR, et al. Increased incidence of non-insulin-dependent diabetes mellitus among adolescents. J Pediatr. 1996 May;128(5 Pt 1):608–615. doi: 10.1016/s0022-3476(96)80124-7. [DOI] [PubMed] [Google Scholar]
- 2.Krebs NF, Himes JH, Jacobson D, et al. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007 Dec;120 4:S193–228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 3.Lee S, Bacha F, Gungor N, et al. Waist circumference is an independent predictor of insulin resistance in black and white youths. J Pediatr. 2006 Feb;148(2):188–194. doi: 10.1016/j.jpeds.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 4.Lee JM, Okumura MJ, Davis MM, et al. Prevalence and determinants of insulin resistance among U.S. adolescents: a population-based study. Diabetes Care. 2006 Nov;29(11):2427–2432. doi: 10.2337/dc06-0709. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez JR, Redden DT, Pietrobelli A, et al. Waist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescents. J Pediatr. 2004 Oct;145(4):439–444. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 6.Lee JM, Davis MM, Woolford SJ, et al. Waist Circumference Percentile Thresholds for Identifying Adolescents with Insulin Resistance in Clinical Practice Pediatric Diabetes. doi: 10.1111/j.1399-5448.2008.00474.x. In press. [DOI] [PubMed] [Google Scholar]
- 7.Gungor N, Saad R, Janosky J, et al. Validation of surrogate estimates of insulin sensitivity and insulin secretion in children and adolescents. J Pediatr. 2004 Jan;144(1):47–55. doi: 10.1016/j.jpeds.2003.09.045. [DOI] [PubMed] [Google Scholar]
- 8.Messiah SE, Arheart KL, Lipshultz SE, et al. Body Mass Index, Waist Circumference, and Cardiovascular Risk Factors in Adolescents. J Pediatr. 2008 Jul 31; doi: 10.1016/j.jpeds.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Misra A, Madhavan M, Vikram NK, et al. Simple anthropometric measures identify fasting hyperinsulinemia and clustering of cardiovascular risk factors in Asian Indian adolescents. Metabolism. 2006 Dec;55(12):1569–1573. doi: 10.1016/j.metabol.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 10.Krebs NF. Screening for Overweight in Children and Adolescents: A Call to Action. Am Acad Pediatrics. 2005:238–239. doi: 10.1542/peds.2004-0755. [DOI] [PubMed] [Google Scholar]


