Viremia copy-years predicted all-cause mortality independent of traditional, cross-sectional viral load measures and time-updated CD4+ T-lymphocyte count in antiretroviral therapy-treated patients suggesting cumulative human immunodeficiency virus replication causes harm independent of its effect on the degree of immunodeficiency.
Abstract
Background. Cross-sectional plasma human immunodeficiency virus (HIV) viral load (VL) measures have proven invaluable for clinical and research purposes. However, cross-sectional VL measures fail to capture cumulative plasma HIV burden longitudinally. We evaluated the cumulative effect of exposure to HIV replication on mortality following initiation of combination antiretroviral therapy (ART).
Methods. We included treatment-naive HIV-infected patients starting ART from 2000 to 2008 at 8 Center for AIDS Research Network of Integrated Clinical Systems sites. Viremia copy-years, a time-varying measure of cumulative plasma HIV exposure, were determined for each patient using the area under the VL curve. Multivariable Cox models were used to evaluate the independent association of viremia copy-years for all-cause mortality.
Results. Among 2027 patients contributing 6579 person-years of follow-up, the median viremia copy-years was 5.3 log10 copy × y/mL (interquartile range: 4.9–6.3 log10 copy × y/mL), and 85 patients (4.2%) died. When evaluated separately, viremia copy-years (hazard ratio [HR] = 1.81 per log10 copy × y/mL; 95% confidence interval [CI], 1.51–2.18 per log10 copy × y/mL), 24-week VL (1.74 per log10 copies/mL; 95% CI, 1.48–2.04 per log10 copies/mL), and most recent VL (HR = 1.89 per log10 copies/mL; 95% CI: 1.63–2.20 per log10 copies/mL) were associated with increased mortality. When simultaneously evaluating VL measures and controlling for other covariates, viremia copy-years increased mortality risk (HR = 1.44 per log10 copy × y/mL; 95% CI, 1.07–1.94 per log10 copy × y/mL), whereas no cross-sectional VL measure was independently associated with mortality.
Conclusions. Viremia copy-years predicted all-cause mortality independent of traditional, cross-sectional VL measures and time-updated CD4+ T-lymphocyte count in ART-treated patients, suggesting cumulative HIV replication causes harm independent of its effect on the degree of immunodeficiency.
In the mid-1990s, plasma HIV RNA levels (or “viral load” [VL]) emerged as an essential surrogate biomarker, triggering a dynamic period of scientific discovery that resulted in pivotal advances in our understanding of viral pathogenesis and the natural history of HIV infection [1–4]. Contemporaneous advances in combination antiretroviral therapy (ART) allowed for landmark studies demonstrating the prognostic value of plasma HIV VL reduction on the occurrence of clinical disease progression following treatment initiation [5, 6]. Around the same time, the significant role of plasma VL in relation to HIV risk transmission was identified [7], providing the foundation for a “test-and-treat” HIV prevention strategy [8, 9]. Although plasma VL has been integral to HIV clinical practice and research initiatives for more than a decade, this biomarker has been used almost exclusively as a cross-sectional measure clinically and analytically, even though it is routinely measured serially. Although single plasma VL measures have demonstrated clear value in translational, clinical, and prevention research, cross-sectional measures fail to capture an individual’s cumulative exposure to viral replication over time.
Historically, the pathogenesis of plasma HIV VL was largely ascribed to the role of varying levels of viremia contributing to differential rates of CD4+ T lymphocyte decline [1, 2, 10, 11]. In recent years, this paradigm has expanded with increased recognition of an independent association of viremia with morbidity and mortality. These observations have largely been ascribed to de novo viral replication as a driver of inflammatory responses and immune system activation [12, 13]. Sustained periods of HIV replication may cause irreversible damage to the immune system, including lymphoid fibrosis, thymic destruction, exhaustion of hematopoietic stem cells, loss of gut mucosal integrity, and end-organ disease [14–18]. The inflammatory process associated with viral replication may also contribute to premature onset of atherosclerosis and other diseases not traditionally associated with AIDS [12].
Cross-sectional VL measures fail to capture a patient’s longitudinal exposure to HIV replication. Measurement of cumulative plasma VL burden is particularly relevant in the modern treatment era, potentially serving as a proxy measure of cumulative inflammation and immune system activation. Moreover, cumulative VL measures may also prove valuable in modeling HIV transmission dynamics, particularly in the evaluation of test-and-treat prevention interventions and simulation models [8, 9, 19].
We developed viremia copy-years as a measure of cumulative HIV burden that estimates the area under a patient’s longitudinal VL curve [20]. In this study, we evaluated the relationship between viremia copy-years and mortality among patients who started ART in a large, nationally distributed cohort receiving HIV care in the United States. We hypothesized a strong, positive relationship would be observed between viremia copy-years and the risk of all-cause mortality, independent of patient socio-demographic and clinical prognostic factors, including clinically relevant cross-sectional VL measures (baseline, 24-week, and most-recent VL measures) and time-updated CD4+ T-lymphocyte count.
METHODS
Sample and Procedures
The Centers for AIDS Research (CFAR) Network of Integrated Clinical Systems (CNICS) is a nationally distributed HIV clinical cohort that has been described in detail previously [21]. The CNICS cohort includes >21000 HIV-infected adults (contributing >60000 person-years follow-up) who have received HIV care at 1 of 8 CFAR sites, dating back to 1995. Every 2 months, sites transmit comprehensive and well-defined data elements captured from point-of-care electronic health-record systems using standardized terminology and format. The participating cohorts and this study were approved by local institutional review boards.
For this study, we included all antiretroviral-naive CNICS patients who started ART with at least 3 antiretroviral agents including either a ritonavir-boosted protease inhibitor (PI/r) or a nonnucleoside reverse transcriptase inhibitor (NNRTI) between 1 January 2000 and 31 December 2008 (n = 3075). We excluded patients with <24 weeks of follow-up (n = 313), without available pre-ART VL or CD4 cell count values (n = 355), or without at least 2 VL measures following ART initiation (n = 380). Patients were followed until the first of death from any cause; administrative censoring (July 31, 2009); or loss to follow-up defined as not having a VL measured in >12 months (with censoring at last available VL + 365 days).
Plasma Viral Load Measures
VL values obtained during routine clinical care were used for all analyses. The most commonly used VL assays were the Amplicor HIV-1 Ultrasensitive Monitor test (Roche Molecular Systems, 40%), Amplicor HIV-1 Monitor test (Roche Molecular Systems, 13%), other reverse-transcription polymerase chain reaction–based tests (21%), and quantitative branched DNA tests (25%). Values below a limit of assay detection were set to one-half the limit of detection for that assay. Cross-sectional VL measures used for analyses were selected based on clinical relevance and long-standing use in the published literature and included: baseline VL (most proximal within 6 months prior to ART initiation), 24-week VL following ART initiation, and most recent VL (observed >24 weeks post–ART initiation) [10, 22–24].
Viremia copy-years, the principal exposure of interest, is a time-varying measure of cumulative plasma HIV burden, akin to pack-years of cigarette smoking, which is calculated using methods described previously [20]. The trapezoidal rule is used to approximate the integral representing the area under each patient’s longitudinal VL curve. VL burden for each segment (time interval between 2 consecutive VL values) is calculated by multiplying the mean of the 2 VL values by the time interval. The copy × y/mL for each segment of a patient’s VL curve are then summed to calculate viremia copy-years. Formally, viremia copy-years is the number of copies of HIV RNA per mL of plasma over time. For example, 10000 copy-years of viremia is equal to having a VL of 10000 copies/mL for 1 year or a VL of 1000 copies/mL for 10 years. VL values prior to 24 weeks of ART initiation were excluded from calculating viremia copy-years to best capture the effect of cumulative VL exposure on mortality after allowing patients a reasonable window to respond to therapy.
Mortality Ascertainment
Mortality data were obtained from clinic sources and confirmed by the National Death Index, Social Security Death Index, or state death certificate data. These databases were searched at least annually for all CNICS participants who were not known to be alive. Because cause of death is subject to misclassification and often unknown, we did not evaluate cause-specific mortality.
Additional Covariates
Additional measures selected a priori included age, sex, race/ethnicity, men who have sex with men (MSM), and injection-drug use (IDU) as HIV risk transmission groups, year of ART initiation, PI/r- vs NNRTI-based initial ART regimen, baseline and time-updated CD4+ T-lymphocyte counts, and CNICS site. We used an intention-to-continue initial ART regimen approach and therefore did not account for changes or discontinuation of ART regimens [25].
Statistical Analyses
Spearman rank correlation coefficient was used to assess correlation between VL measures. Mortality rates were expressed as deaths per 100 person-years with 95% confidence intervals based on an exact Poisson distribution. Cox proportional hazards regression models were used to estimate the relationship between viremia copy-years and all-cause mortality, with time at risk accrued from 24 weeks post–ART initiation. Multivariable models were adjusted for covariates outlined above. Because viremia copy-years is affected by prior viremia copy-years and CD4+ T-lymphocyte counts, which themselves are affected by prior viremia copy-years, we used inverse probability–weighted marginal structural models [25, 26]. We estimated the inverse probability weights by fitting linear regression models to estimate each patient’s density of viremia copy-years. This is an extension of the previously outlined [26] standard marginal structural model with a binary treatment variable to that of a continuous variable. These models included the baseline and time-varying factors listed previously, where time-varying covariates were lagged by 1 visit to ensure proper temporal ordering.
We also adjusted for selection bias by estimating inverse probability of censoring weights and for differential attendance at clinic visits by estimating inverse probability of visit attendance weights [27]. These weights were conditional on measured baseline and time-varying covariates. Weights based on a density (eg, viremia copy-years) and probabilities (eg, censoring and visit attendance) were stabilized, the latter to improve efficiency. The mean of the estimated stabilized inverse probability weights was 1.00 (standard deviation, 0.24; minimum/maximum, 0.27/1.63). We fit a pooled logistic regression model weighted by the product of these weights to approximate a weighted Cox proportional hazards model [28]. The reference hazard was modeled using cubic splines and robust 95% confidence intervals were used. Departures from linearity were assessed by categorizing continuous measures. The proportional hazards assumption was explored graphically and assessed by inclusion of a product term with time. We plotted survival curves stratified by levels of time-updated viremia copy-years adjusted by inverse probability unstabilized weights, which were a product of viremia copy-years density weight, censoring weight, and visit-attendance weight, as described above [29].
Additional models included cross-sectional VL measures, which were evaluated individually and collectively in separate models. Analogous steps to those for viremia copy-years were followed to estimate inverse probability weights for most-recent VL used in analyses where this was the main exposure of interest. Because baseline and 24-week VLs are time-fixed, we did not construct inverse probability weights for these VL measures when they were the main exposure of interest; however, censoring and visit attendance weights were constructed as above. Sensitivity analyses were conducted assigning undetectable VL measures a value of zero, varying the start time of viremia copy-years calculation (from ART start, 48 weeks and 2-year post–ART-start), censoring patients at ART discontinuation (gaps in ART >30 days and >90 days), and excluding VL values proximal to death (within 30 and 90 days), all of which yielded estimates for viremia copy-years and mortality that were highly consistent with primary analyses (data not shown). All statistical analyses were performed using SAS version 9.2 (SAS Institute).
RESULTS
Among 2027 patients, the median age at ART initiation was 39 years (interquartile range [IQR]. 33–45 y), 81% were male, 52% were Caucasian/white, 36% were African American/black, and 54% were MSM (Table 1). The median baseline CD4+ T-lymphocyte count and VL were 222 cells/mm3 (IQR, 97–325 cells/mm3) and 4.8 log10 copies/mL (IQR, 4.2–5.3 log10 copies/mL), respectively. Of all patients, 30% started ART with a PI/r-based regimen. The median year of ART initiation was 2003 (IQR, 2002–2005). Patients were followed for a median of 2.7 years (IQR: 1.6–4.6) and contributed a total of 6579 person-years follow-up; 15% of patients (n = 296) had >12 months between VL measures during follow-up and were considered lost to follow-up.
Table 1.
Characteristics of 2027 Treatment-Naive HIV-Infected Patients at Initiation of Combination Antiretroviral Therapy and Over the Course of 6579 Person-Years Follow-up, CFAR Network of Integrated Clinical Systems (CNICS), 2000–2008a
| Characteristic | Baseline | Follow-up |
| Participants/observations | 2027 patients | 21665 VL measures |
| Age, years | 39 (33–45) | 42 (35–48) |
| Sex | ||
| Male | 1646 (81%) | 17117 (79%) |
| Female | 381 (19%) | 4548 (21%) |
| Race/ethnicity | ||
| Caucasian/white | 1045 (52%) | 10580 (49%) |
| African American/black | 731 (36%) | 8482 (39%) |
| Other | 251 (12%) | 2603 (12%) |
| Men who have sex with men | 1085 (54%) | 11157 (52%) |
| Intravenous drug use | 303 (15%) | 3355 (15%) |
| ART initiation year | ||
| 2000–02 | 466 (23%) | 7673 (35%) |
| 2003–05 | 765 (38%) | 9453 (44%) |
| 2006–08 | 796 (39%) | 4539 (21%) |
| Initial ART regimen | ||
| NNRTI-based | 1414 (70%) | 15150 (70%) |
| PI/r-based | 613 (30%) | 6515 (30%) |
| Baseline CD4 cell count, cells/mm3 | 222 (97–325) | 197 (74–310) |
| Most recent CD4 cell count, cells/mm3 | N/A | 363 (208–541) |
| Baseline VL, log10 copies/mL | 4.8 (4.2–5.3) | 4.9 (4.2–5.4) |
| 24-week VL <2.6, log10 copies/mL | 1635 (81%) | 17091 (79%) |
| Most recent VL, log10 copies/mL | N/A | <2.6 (<2.6–<2.6) |
| Viremia copy-years, log10 copy × y/mL | N/A | 5.3 (4.9–6.3) |
| Follow-up, years | 2.7 (1.6–4.6) | N/A |
| VL measures contributed | N/A | 8 (4–15) |
Abbreviations: ART, combination antiretroviral therapy; HIV, human immunodeficiency virus; NA, not applicable; NNRTI, nonnucleoside reverse transcriptase inhibitor; PI/r, ritonavir-boosted protease inhibitor; VL, plasma HIV viral load.
Data are presented as N (%) or median (interquartile range) unless otherwise specified.
Patients contributed a median of 8 VL measures (IQR, 4–15), for a total of 21665 VL measures. Most patients were virologically suppressed 24 weeks following ART initiation (n = 1635, 81%). During follow-up, most VL measures were below the limit of assay detection (n = 17 764, 82%). Over time, the median viremia copy-years was 5.3 log10 copy × years/mL (IQR, 4.9–6.3). Viremia copy-years was poorly correlated with baseline VL and somewhat correlated with 24-week and most-recent VLs (Table 2).
Table 2.
Spearman Rank Correlation Matrix for Measures of Plasma HIV Viral Load Among 2027 Treatment-Naive HIV-Infected Patients Initiating Combination Antiretroviral Therapy, CFAR Network of Integrated Clinical Systems (CNICS), 2000–2008
| Viremia copy-years | Baseline VL | 24-week VL | Most recent VL | |
| Viremia copy-years, copy × y/mL | 1 | |||
| Baseline VL, copies/mL | 0.10 | 1 | ||
| 24-week VL, copies/mL | 0.45 | 0.08 | 1 | |
| Most recent VL, copies/mL | 0.50 | 0.02 | 0.40 | 1 |
Abbreviations: HIV, human immunodeficiency virus; VL, plasma HIV viral load.
For repeat measures (viremia copy-years and most recent VL) the most recent value was used.
All P values for correlations are <.01 except for baseline VL and most recent VL (P = .624).
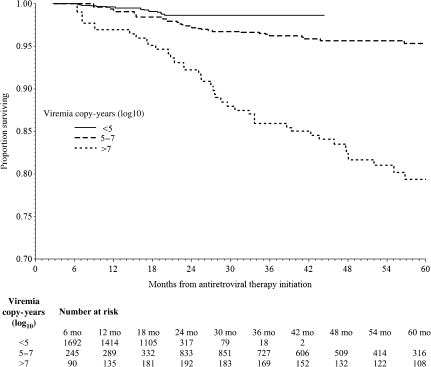
In all, 4% of patients died (n = 85), for an overall mortality rate of 1.3 deaths per 100 person-years (95% confidence interval [CI], 1.0–1.6 deaths). The median time until death was 2.0 years (IQR, 1.4–2.9 years). The unadjusted mortality hazard ratio (HR) for log10 viremia copy × years was 1.81 (95% CI: 1.51–2.18), indicating that for each log10 increase in viremia copy-years the hazard of death increased nearly 2-fold (Table 3). The increasing risk of death with greater viremia copy-years was confirmed after categorizing viremia copy-years and comparing the groups with 5–7 log10 viremia copy × y/mL (HR = 1.38; 95% CI, 0.61–3.13) and >7 log10 viremia copy × y/mL (HR = 5.54; 95% CI, 3.46–8.84) to patients with <5 log10 viremia copy y/mL (Figure 1). The effect of viremia copy-years on mortality did not vary appreciably across time.
Table 3.
All-Cause Mortality Following Initiation of Combination Antiretroviral Therapy Among 2027 Treatment-Naive HIV-Infected Patients According to Viremia Copy-Years and Other Viral Load Measures, CFAR Network of Integrated Clinical Systems, 2000–2008
| Hazard ratio | 95% confidence limits | P value | |
| Separate VL models, unadjusted and unweighted:a | |||
| Viremia copy-years, log10 copy × y/mL | 1.81 | 1.51, 2.18 | <.001 |
| Baseline VL, log10 copies/mL | 1.26 | 0.96, 1.64 | .09 |
| 24-week VL, log10 copies/mL | 1.74 | 1.48, 2.04 | <.001 |
| Most recent VL, log10 copies/mL | 1.89 | 1.63, 2.20 | <.001 |
| Combined VL model, unadjusted and unweighted:b | |||
| Viremia copy-years, log10 copy × y/mL | 1.62 | 1.25, 2.11 | <.001 |
| Baseline VL, log10 copies/mL | 1.08 | 0.85, 1.37 | .54 |
| 24-week VL, log10 copies/mL | 1.11 | 0.91, 1.34 | .31 |
| Most recent VL, log10 copies/mL | 1.23 | 1.01, 1.49 | .04 |
Abbreviations: HIV, human immunodeficiency virus; VL, plasma HIV viral load.
Models do not control for covariates, are not inverse probability weighted, and were fit via Cox proportional hazards regression.
Separate Cox models were fit for each VL measure listed.
One combined Cox model includes all VL measures listed.
Figure 1.
Adjusted survival curve for time-varying viremia copy-years among 2027 treatment-naive HIV-infected patients, CFAR Network of Integrated Clinical Systems (CNICS), 2000–2008. Adjusted survival curves modeling all-cause mortality among 2027 treatment-naive HIV-infected patients following antiretroviral therapy (ART) initiation stratified by levels of time-updated viremia copy-years. Viremia copy-years, the principal exposure of interest, is a time-varying measure of cumulative plasma HIV burden calculated as described in the methods section. Viral load values prior to 24 weeks of ART initiation were excluded from calculating viremia copy-years to best capture the effect of cumulative viral load exposure on mortality after allowing patients a reasonable window to respond to therapy. The survival curves were adjusted for confounding and selection bias due to age, sex, race/ethnicity, HIV transmission risk group, initial ART, year of ART initiation, CNICS site, most recent CD4 count, and visit frequency using inverse probability unstabilized weights, which were a product of viremia copy-years density weight, censoring weight, and visit attendance weight.
In unadjusted and unweighted analyses, cross-sectional VL measures following ART initiation, but not baseline VL, were predictive of mortality; 24-week log10 VL (HR = 1.74; 95% CI: 1.48, 2.04) and most recent log10 VL (HR = 1.89; 1.63,2.20, Table 3). In a combined VL model that included baseline, 24-week, and most recent VL, the effect of viremia copy-years was only slightly attenuated (HR = 1.62; 95% CI: 1.25, 2.11, Table 3).
In adjusted and weighted analyses, viremia copy-years was independently associated with mortality (HR = 1.65; 95% CI: 1.32, 2.06, Table 4). Results for each cross-sectional VL measure individually were consistent with unadjusted and unweighted results, albeit with attenuation of effect sizes (Table 4). In adjusted and weighted analyses that included demographic and clinical covariates as well as baseline, 24-week, and most-recent VL, the effect of viremia copy-years decreased slightly (HR = 1.44; 95% CI, 1.07–1.94); however, the cross-sectional VL measures were no longer associated with mortality (Table 4). In addition to viremia copy-years, lower most recent CD4+ T-lymphocyte count (0.72 per 100 cells/mm3; 95% CI, .61–.86) and older age (HR = 1.51 per 10 y; 95% CI, 1.18–1.94) were associated with increased mortality risk.
Table 4.
Estimated Effect of HIV Viral Load Measures on All-Cause Mortality Following Initiation of Combination Antiretroviral Therapy Among 2027 Treatment-Naive HIV-Infected Patients, CFAR Network of Integrated Clinical Systems (CNICS), 2000–2008
| Hazard ratio | 95% confidence limits | P value | |
| Separate VL models, adjusted and weighted:a | |||
| Viremia copy-years, log10 (copy × y/mL) | 1.65 | 1.32, 2.06 | <.001 |
| Baseline VL, log10 copies/mL | 1.05 | 0.82, 1.36 | .69 |
| 24-week VL, log10 copies/mL | 1.39 | 1.16, 1.66 | <.001 |
| Most recent VL, log10 copies/mL | 1.50 | 1.24, 1.81 | <.001 |
| Combined VL model, adjusted and weighted:b | |||
| Viremia copy-years, log10 copy × y/mL | 1.44 | 1.07, 1.94 | .02 |
| Baseline VL, log10 copies/mL | 0.99 | 0.77, 1.27 | .93 |
| 24-week VL, log10 copies/mL | 1.07 | 0.87, 1.32 | .51 |
| Most recent VL, log10 copies/mL | 1.15 | 0.94, 1.41 | .18 |
| Most recent CD4 cell count (per 100 cells/mm3) | 0.72 | 0.61, 0.86 | <.001 |
| Age (per 10 years) | 1.51 | 1.18, 1.94 | .001 |
| Female | 1.26 | 0.69, 2.29 | .45 |
| Caucasian/white race/ethnicity | 1.78 | 1.13, 2.81 | .01 |
| Men who have sex with men | 0.88 | 0.52, 1.47 | .62 |
| Intravenous drug use | 0.86 | 0.47, 1.54 | .60 |
| PI/r-based initial ART regimen | 1.50 | 0.94, 2.40 | .09 |
| Year of ART initiation (per 1 year increase) | 1.02 | 0.91, 1.14 | .75 |
All estimates are adjusted for baseline covariates including age, sex, race/ethnicity, HIV transmission risk group, initial ART, year of ART initiation, and CNICS site. Additionally, time-varying covariates including most recent CD4+ T-lymphocyte count were controlled through the inverse probability weights for time-varying VL measures. Inverse probability weights were used in all models to control for selection bias and visit frequency.
Abbreviations: ART, combination antiretroviral therapy; HIV, human immunodeficiency virus; PI/r, ritonavir-boosted protease inhibitor; VL , plasma HIV viral load.
Separate Cox models were fit for each VL measure listed.
One combined Cox model includes all VL measures listed.
DISCUSSION
Viremia copy-years, a measure of cumulative plasma HIV RNA exposure and de novo viral replication, demonstrated a strong association with all-cause mortality in a large sample of HIV-infected patients who started ART. When controlling for clinically meaningful, cross-sectional and time-updated VL measures and time-updated CD4+ T-lymphocyte count, as well as other covariates, an independent 44% increase in mortality risk was observed per 1 unit increase in log10 copy × year/mL of cumulative VL burden. We suggest viremia copy-years play an important and complementary role to cross-sectional VL measures and transform the role of VL in future translational, clinical, and prevention research initiatives, as well as clinical care.
Cross-sectional VL measures obtained at various single time points in HIV-infected patient’s trajectory have provided important prognostic value in the eras preceding and following the introduction of modern ART [1, 2, 5, 6, 11, 22–24]. Baseline VL demonstrated clear prognostic value for disease progression prior to the combination ART era [1, 2]. However, in the modern treatment era, baseline VL is poorly predictive of clinical events following ART start, whereas single, cross-sectional VL measures on treatment (eg, 6-month) have proven valuable in predicting AIDS and non-AIDS clinical events, including mortality [22–24]. As expected, in the current study, cross-sectional measures of 24-week and most-recent VLs were predictive for all-cause mortality when evaluated individually. However, these findings were substantially attenuated when controlling for viremia copy-years in adjusted models.
In addition to viremia copy-years, a 51% increased mortality risk for each additional 10 years of age at ART start, and a 28% reduction in risk per additional 100 cells/mm3 in time-updated CD4+ T-lymphocyte count, was observed. The association of viremia copy-years with mortality when controlling for most recent CD4+ T-lymphocyte count is particularly noteworthy. These findings substantiate growing recognition that HIV replication may cause or accelerate disease independent of its effect on peripheral CD4+ T-cell depletion. In this regard, the relationship between plasma HIV VL and markers of inflammation or immune system activation have gained considerable attention, particularly in relation to the occurrence of non–AIDS-related clinical events [12, 13].
In primary study analyses of the Strategic Management of Antiretroviral Therapy (SMART) trial, the proportion of follow-up time with detectable plasma viremia, all-cause mortality and other clinical events were significantly higher among the drug conservation arm, which received intermittent ART, relative to the viral suppression group [30]. Notably, an increased, albeit attenuated, risk of opportunistic diseases or death was observed in the drug conservation arm of the SMART study even after reinitiating continuous ART [31]. Among patients in the drug conservation arm of the study, a strong, positive relationship was observed between change in plasma HIV VL and change in inflammatory biomarkers interleukin-6 and D-dimer, both of which were associated with all-cause mortality [12]. SMART study authors postulated long-term effects of elevated inflammatory biomarkers contributed to the excess residual risk of clinical events in the drug conservation group even after resuming continuous ART. We speculate the number of viremia copy-years, as a measure of cumulative plasma HIV burden, serves as a surrogate for and perhaps is the underlying driver of cumulative inflammation and immune system activation that approximates such long-term inflammatory biomarker effects. As patients with HIV infection in developed countries are living longer and increasingly experiencing morbidity and mortality from non-AIDS events [24, 32–35], many of which are associated with inflammation and immune system activation [12, 13], cumulative measures of HIV burden may take on increased importance in the coming years.
In recent years, others have begun to evaluate longitudinal plasma HIV VL measures. Short-term area under the curve VL measures (48–56 weeks post–ART initiation) relative to baseline VL values have been evaluated in clinical trials as a predictor of clinical events and used as an outcome measure [36, 37]. Additionally, a recent study identified a strong association between longer-term cumulative viremia and AIDS-related lymphoma among patients receiving combination ART [38].
Our study has limitations. As with all observational studies, we can identify associations but not ascribe causality because our findings are subject to possible uncontrolled confounding. Plasma VL measures were assessed relatively infrequently, with variable numbers and timing of measures observed for patients, reflecting the realities of HIV clinical care. We used inverse probability weighting to account for between-patient heterogeneity in number and timing of VL measures in an effort to address this limitation. We evaluated the effect of viremia copy-years on mortality over a relatively short follow-up period; future studies are needed to validate the prognostic value of this measure over longer follow-up. Specifically, studies are indicated to further elucidate the predictive value of viremia copy-years among patients who achieve and maintain virologic suppression over longer follow-up, who experience brief periods of detectable viremia and those who experience periods of detectable low-level viral replication. We had insufficient information on cause-specific mortality to evaluate the relationship between viremia copy-years with AIDS and non-AIDS deaths.
In conclusion, viremia copy-years, a novel measure of cumulative plasma HIV burden, demonstrated prognostic value for all-cause mortality independent of traditional, clinically relevant cross-sectional VL measures and time-updated CD4+ T-lymphocyte count in patients who started modern ART. Future research should evaluate the relationship between viremia copy-years and biomarkers of inflammation and immune system activation longitudinally, as well as the value of this measure in predicting AIDS and non-AIDS clinical events, and in modeling HIV risk transmission over time.
Notes
Acknowledgments.
We would like to thank the patients, principal investigators, coinvestigators, and research staff at participating CFAR Network of Integrated Clinical Systems sites at the following institutions: Case Western Reserve University; University of Alabama at Birmingham; University of California, San Francisco; the University of Washington; the University of California, San Diego; Fenway Community Health Center of Harvard University; University of North Carolina; and Johns Hopkins University. In particular, we thank Stephen Van Rompaey of the Data Management Core at University of Washington and Donna Porter of the Administrative Core at University of Alabama at Birmingham for their assistance in the conduct of this study. We also thank Rosemary McKaig of the National Institute of Allergy and Infectious Disease, National Institutes of Health, for her critical review of this manuscript.
M. J. M. and S. N. led the conception and design of this study, contributed to data acquisition and interpretation, prepared the initial draft of the manuscript, had full access to all the data in the study and take final responsibility for the decision to submit for publication. S. R. C., J. J. E., B. L., and M. S. S. substantively contributed to the conception and design of this study, data acquisition or interpretation and provided critical revision of the manuscript. Remaining authors provided substantial contributions to the study design, data acquisition or interpretation of data and provided critical revision of the manuscript. All authors approved the final version of the manuscript.
Financial support.
This work was supported by the National Institutes of Health (grants 1R21AI087360-01, 1R24AI067039-04, P30-AI027767, P30-AI50410, and K01-AI071754 [to B. L.]); the Agency for Healthcare Research and Quality (R01HS018731 [to S. N.]). The funding sources did not participate in the study design; collection, analysis and interpretation of data; in the writing of the manuscript; or in the decision to submit the paper for publication.
Potential conflicts of interest.
M. J. M has received consulting fees from Bristol-Myers Squibb, Merck Foundation and Gilead Sciences, and grant support from Bristol-Myers Squibb, Pfizer, Tibotec Therapeutics and Definicare LLC. S. N. has received grant support from GlaxoSmithKline, Pfizer, Bristol-Myers Squibb, Merck, Virco and Abbott. J. J. E has received consulting fees from Tibotec, Bristol-Myers Squibb, Merck, GlaxoSmithKline, ViiV and Pfizer, lecture fees from Roche, Bristol-Myers Squibb, Tibotec, and Merck, and grant support from GlaxoSmithKline, Merck, ViiV and Boehringer-Ingelheim. J. H. W. has received consulting fees from Bristol-Myers Squibb and Gilead Sciences, and grant support from Bristol-Myers Squibb, Pfizer, Tibotec Therapeutics and Definicare LLC. R. D. M. has received consulting fees from Bristol-Myers Squibb and GlaxoSmithKline, lecture fees from Gilead, and grant support from Pfizer, Merck, and Gilead. S. G. D. has received consulting fees from GlaxoSmithKline and grant support from Merck and Gilead. M. S. S. has received consulting fees from Ardea Biosciences, Avexa, Boehringer-Ingelheim, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Merck, Monogram Biosciences, Pain Therapeutics, Panacos, Pfizer, Progenics, Roche Laboratories, Tibotec, Tobira Therapeutics, and Vicro and research support from Achillion Pharmaceuticals, Avexa, Boehringer-Ingelheim, GlaxoSmithKline, Merck, Panacos, Pfizer, Progenics, Theratechnologies and Tibotec. All other authors report no conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Mellors JW, Kingsley LA, Rinaldo CR, Jr, et al. Quantitation of HIV-1 RNA in plasma predicts outcome after seroconversion. Ann Intern Med. 1995;122:573–9. doi: 10.7326/0003-4819-122-8-199504150-00003. [DOI] [PubMed] [Google Scholar]
- 2.Mellors JW, Rinaldo CR, Jr, Gupta P, White RM, Todd JA, Kingsley LA. Prognosis in HIV-1 infection predicted by the quantity of virus in plasma. Science. 1996;272:1167–70. doi: 10.1126/science.272.5265.1167. [DOI] [PubMed] [Google Scholar]
- 3.Saag MS, Holodniy M, Kuritzkes DR, et al. HIV viral load markers in clinical practice. Nat Med. 1996;2:625–9. doi: 10.1038/nm0696-625. [DOI] [PubMed] [Google Scholar]
- 4.Piatak M, Jr, Saag MS, Yang LC, et al. High levels of HIV-1 in plasma during all stages of infection determined by competitive PCR. Science. 1993;259:1749–54. doi: 10.1126/science.8096089. [DOI] [PubMed] [Google Scholar]
- 5.Eron JJ, Benoit SL, Jemsek J, et al. Treatment with lamivudine, zidovudine, or both in HIV-positive patients with 200 to 500 CD4+ cells per cubic millimeter. North American HIV Working Party. N Engl J Med. 1995;333:1662–9. doi: 10.1056/NEJM199512213332502. [DOI] [PubMed] [Google Scholar]
- 6.O'Brien WA, Hartigan PM, Martin D, et al. Changes in plasma HIV-1 RNA and CD4+ lymphocyte counts and the risk of progression to AIDS. Veterans Affairs Cooperative Study Group on AIDS. N Engl J Med. 1996;334:426–31. doi: 10.1056/NEJM199602153340703. [DOI] [PubMed] [Google Scholar]
- 7.Quinn TC, Wawer MJ, Sewankambo N, et al. Viral load and heterosexual transmission of human immunodeficiency virus type 1. Rakai Project Study Group. N Engl J Med. 2000;342:921–9. doi: 10.1056/NEJM200003303421303. [DOI] [PubMed] [Google Scholar]
- 8.Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA. 2009;301:2380–2. doi: 10.1001/jama.2009.828. [DOI] [PubMed] [Google Scholar]
- 9.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: A mathematical model. Lancet. 2009;373:48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 10.Ledergerber B, Lundgren JD, Walker AS, et al. Predictors of trend in CD4-positive T-cell count and mortality among HIV-1-infected individuals with virological failure to all three antiretroviral-drug classes. Lancet. 2004;364:51–62. doi: 10.1016/S0140-6736(04)16589-6. [DOI] [PubMed] [Google Scholar]
- 11.Phillips AN, Lampe FC, Smith CJ, et al. Ongoing changes in HIV RNA levels during untreated HIV infection: Implications for CD4 cell count depletion. AIDS. 2010;24:1561–7. doi: 10.1097/QAD.0b013e32833a6056. [DOI] [PubMed] [Google Scholar]
- 12.Kuller LH, Tracy R, Belloso W, et al. Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med. 2008;5:e203. doi: 10.1371/journal.pmed.0050203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tebas P, Henry WK, Matining R, et al. Metabolic and immune activation effects of treatment interruption in chronic HIV-1 infection: Implications for cardiovascular risk. PLoS One. 2008;3:e2021. doi: 10.1371/journal.pone.0002021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brenchley JM, Price DA, Schacker TW, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12:1365–71. doi: 10.1038/nm1511. [DOI] [PubMed] [Google Scholar]
- 15.Choi AI, Shlipak MG, Hunt PW, Martin JN, Deeks SG. HIV-infected persons continue to lose kidney function despite successful antiretroviral therapy. AIDS. 2009;23:2143–9. doi: 10.1097/QAD.0b013e3283313c91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McCune JM. The dynamics of CD4+ T-cell depletion in HIV disease. Nature. 2001;410:974–9. doi: 10.1038/35073648. [DOI] [PubMed] [Google Scholar]
- 17.Schacker TW, Nguyen PL, Beilman GJ, et al. Collagen deposition in HIV-1 infected lymphatic tissues and T cell homeostasis. J Clin Invest. 2002;110:1133–9. doi: 10.1172/JCI16413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stebbing J, Gazzard B, Douek DC. Where does HIV live? N Engl J Med. 2004;350:1872–80. doi: 10.1056/NEJMra032395. [DOI] [PubMed] [Google Scholar]
- 19.Walensky RP, Paltiel AD, Losina E, et al. Test and treat DC: Forecasting the impact of a comprehensive HIV strategy in Washington DC. Clin Infect Dis. 2010;51:392–400. doi: 10.1086/655130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cole SR, Napravnik S, Mugavero MJ, Lau B, Eron JJ, Jr, Saag MS. Copy-years viremia as a measure of cumulative human immunodeficiency virus viral burden. Am J Epidemiol. 2010;171:198–205. doi: 10.1093/aje/kwp347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kitahata MM, Rodriguez B, Haubrich R, et al. Cohort profile: The Centers for AIDS research Network of Integrated clinical systems. Int J Epidemiol. 2008;37:948–55. doi: 10.1093/ije/dym231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chene G, Sterne JA, May M, et al. Prognostic importance of initial response in HIV-1 infected patients starting potent antiretroviral therapy: analysis of prospective studies. Lancet. 2003;362:679–86. doi: 10.1016/s0140-6736(03)14229-8. [DOI] [PubMed] [Google Scholar]
- 23.Egger M, May M, Chene G, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: A collaborative analysis of prospective studies. Lancet. 2002;360:119–29. doi: 10.1016/s0140-6736(02)09411-4. [DOI] [PubMed] [Google Scholar]
- 24.Marin B, Thiebaut R, Bucher HC, et al. Non-AIDS-defining deaths and immunodeficiency in the era of combination antiretroviral therapy. AIDS. 2009;23:1743–53. doi: 10.1097/QAD.0b013e32832e9b78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cole SR, Hernan MA, Robins JM, et al. Effect of highly active antiretroviral therapy on time to acquired immunodeficiency syndrome or death using marginal structural models. Am J Epidemiol. 2003;158:687–94. doi: 10.1093/aje/kwg206. [DOI] [PubMed] [Google Scholar]
- 26.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11:550–60. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Hernán MA, McAdams M, McGrath N, Lanoy E, Costagliola D. Observation plans in longitudinal studies with time-varying treatments. Stat Methods Med Res. 2009;18:27–52. doi: 10.1177/0962280208092345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abbott RD. Logistic regression in survival analysis. Am J Epidemiol. 1985;121:465–71. doi: 10.1093/oxfordjournals.aje.a114019. [DOI] [PubMed] [Google Scholar]
- 29.Westreich D, Cole SR, Tien PC, et al. Time scale and adjusted survival curves for marginal structural cox models. Am J Epidemiol. 2010;171:691–700. doi: 10.1093/aje/kwp418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.El-Sadr WM, Lundgren JD, Neaton JD, et al. Strategies for Management of Antiretroviral Therapy (SMART) Study Group. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283–96. doi: 10.1056/NEJMoa062360. [DOI] [PubMed] [Google Scholar]
- 31.El-Sadr WM, Grund B, Neuhaus J, et al. Strategies for Management of Antiretroviral Therapy (SMART) Study Group. Risk for opportunistic disease and death after reinitiating continuous antiretroviral therapy in patients with HIV previously receiving episodic therapy: A randomized trial. Ann Intern Med. 2008;149:289–99. doi: 10.7326/0003-4819-149-5-200809020-00003. [DOI] [PubMed] [Google Scholar]
- 32.Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet. 2008;372:293–9. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lau B, Gange SJ, Moore RD. Risk of non-AIDS-related mortality may exceed risk of AIDS-related mortality among individuals enrolling into care with CD4+ counts greater than 200 cells/mm3. J Acquir Immune Defic Syndr. 2007;44:179–87. doi: 10.1097/01.qai.0000247229.68246.c5. [DOI] [PubMed] [Google Scholar]
- 34.Lewden C, May T, Rosenthal E, et al. ANRS EN 19 Motalite Study Group and Mortavic1. Changes in causes of death among adults infected by HIV between 2000 and 2005: the “Mortalite 2000 and 2005” surveys (ANRS EN19 and Mortavic) J Acquir Immune Defic Syndr. 2008;48:590–8. doi: 10.1097/QAI.0b013e31817efb54. [DOI] [PubMed] [Google Scholar]
- 35.Palella FJ, Jr, Baker RK, Moorman AC, et al. HIV Outpatient Study Investigators. Mortality in the highly active antiretroviral therapy era: Changing causes of death and disease in the HIV outpatient study. J Acquir Immune Defic Syndr. 2006;43:27–34. doi: 10.1097/01.qai.0000233310.90484.16. [DOI] [PubMed] [Google Scholar]
- 36.Kim S, Hughes MD, Hammer SM, Jackson JB, DeGruttola V, Katzenstein DA. AIDS Clinical Trials Group Study 175 Virology Study Team. Both serum HIV type 1 RNA levels and CD4+ lymphocyte counts predict clinical outcome in HIV type 1-infected subjects with 200 to 500 CD4+ cells per cubic millimeter. AIDS Res Hum Retroviruses. 2000;16:645–53. doi: 10.1089/088922200308873. [DOI] [PubMed] [Google Scholar]
- 37.Puls RL, Srasuebkul P, Petoumenos K, et al. Altair Study Group. Efavirenz versus boosted atazanavir or zidovudine and abacavir in antiretroviral treatment-naive, HIV-infected subjects: Week 48 data from the Altair study. Clin Infect Dis. 2010;51:855–64. doi: 10.1086/656363. [DOI] [PubMed] [Google Scholar]
- 38.Zoufaly A, Stellbrink HJ, Heiden MA, et al. ClinSurv Study Group. Cumulative HIV viremia during highly active antiretroviral therapy is a strong predictor of AIDS-related lymphoma. J Infect Dis. 2009;200:79–87. doi: 10.1086/599313. [DOI] [PubMed] [Google Scholar]