Abstract
Aims
To determine the incidence of long-term injection cessation and its association with residential relocation and neighborhood deprivation.
Design
ALIVE (AIDS Linked to the Intravenous Experience) is a prospective cohort with semi-annual follow-up since 1988. Multi-level discrete time-to-event models were constructed to investigate individual and neighborhood-level predictors of long-term injection cessation.
Setting
Baltimore, USA
Participants
1,697 active injectors from ALIVE with at least 8 semi-annual study visits.
Measurements
Long-term injection cessation was defined as three consecutive years without self-reported injection drug use.
Findings
706 (42%) injectors achieved long-term cessation (incidence = 7.6 per 100 person-years). After adjusting for individual-level factors, long-term injection cessation was 29% less likely in neighborhoods in the third quartile of deprivation (Hazard Ratio [HR] =0.71, 95% CI:0.53–0.95) and 43% less likely in the highest quartile of deprivation (HR=0.57, 95% CI:0.43, 0.76) as compared to the first quartile. Residential relocation was associated with increased likelihood of long-term injection cessation (HR=1.55, 95% CI:1.31, 1.82); however the impact of relocation varied depending on the deprivation in the destination neighborhood. Compared to those who stayed in less deprived neighborhoods, relocation from highly deprived to less deprived neighborhoods had the strongest positive impact on long-term injection cessation (HR=1.96, 95% CI:1.50, 2.57), while staying in the most deprived neighborhoods was detrimental (HR=0.76, 95% CI:0.63, 0.93).
Conclusions
Long-term cessation of injection of opiates and cocaine occurred frequently following a median of 9 years of injection and contextual factors appear to be important. Our findings suggest that improvements in the socio-economic environment may improve the effectiveness of cessation programs.
INTRODUCTION
Injection drug use is associated with substantial morbidity, mortality, social and economic consequences (1–6). Sustained injection cessation is the most effective way to prevent transmission of blood-borne infectious diseases and to improve the health of injectors. Despite the high public health burden of injection drug use, few studies have adequately examined the incidence and predictors of prolonged injection cessation.
Most research on cessation has examined short-term changes in drug-using behaviors (7–14). We previously demonstrated a high rate of short-term injection cessation in Baltimore, but 75% relapsed within one year of stopping (15). More recently in an analysis of patterns of injection over 20 years, we found that although 16% demonstrated frequent stopping and relapse, nearly half reported declining use over time, with approximately 20% demonstrating evidence of long-term cessation, and a median time of cessation of approximately 3 years in length (16).
The individual-level predictors of short-term injection cessation have been well characterized. There is increased recognition that contextual factors at multiple nested levels of influence (e.g., families and social networks within neighborhoods within cities) interact to influence individual health behaviors, physiological processes, and ultimately health (17). Conceptual models of addiction also suggest examining individual drug use within the context of broader interacting levels of influence (18,19). While accumulating research supports the role of the social, economic, and physical environment in shaping individual drug use (19,20,20–26), there remains a limited understanding of the impact of the environment on longer-term maintenance of cessation.
Contextual factors, like individual behaviors, are not static; changes in environment impact health behaviors and outcomes. For example, relocation out of high poverty neighborhoods has been associated with improvements in health outcomes (e.g., mental health status, frequency of drug use) among individuals who relocate (27–29). Relocation itself may directly and/or indirectly promote changes in drug use behaviors through the weakening of conditioned responses associated with elements of the environment (30). Alternatively, the benefits derived from relocation may reflect that new socio-economic and physical environments are more supportive of changes in drug use behaviors, particularly when moving out of high poverty neighborhoods characterized with high levels of drug activity.
In the current study, we characterized the incidence of long-term injection cessation among a well-defined community-based cohort of injection drug users (IDUs) with a specific focus on the effects of contextual (neighborhood deprivation and residential relocation) determinants of drug cessation.
METHODS
Study Participants
The ALIVE (AIDS Linked to the Intravenous Experience) study design and methods have been described in detail previously (31). Briefly, during three enrollment periods (1988–89, 1994–5, and 1998), 2,944 current and former IDUs were recruited into a prospective cohort of IDUs in Baltimore, Maryland. Individuals were eligible if they were older than 18 years of age, AIDS-free, and had a history of injecting at baseline. At baseline, the median age of the cohort was 34 years, 81% were male, 95% African American and 25% HIV-positive.
Since our focus was on long-term injection cessation, we restricted our analysis to participants who reported injecting during at least two follow-up visits and had six or more study visits after the second visit when they reported injecting (through June 2008) without a long lapse between visits (see Missing Data). Study participants without two injecting visits (n=581) were older, had shorter follow-up, fewer visits reporting injection, and fewer years of injection at baseline than active injectors (n = 2,363; p<0.001 for all comparisons). Those without six study visits (n=666) had fewer years of injection at baseline, fewer visits reporting injecting, and higher mortality than those who had six visits (n=1,697; p<0.001 for all comparisons). A total of 1,697 individuals with 33,945 observations, over a median nine visits (IQR: 2–20), were included.
Measures
Baseline interviews provided information on socio-demographics, injection history, lifetime medical history, HIV-risk behaviors (sexual and drug-related) and drug treatment history. At each semi-annual visit, participants provided information on characteristics and behaviors with respect to the previous six months. Data were collected on socio-demographics, drug use behaviors (e.g., frequency and types of drugs injected, non-injection drug and alcohol use), health care utilization (e.g., methadone maintenance, outpatient visits), and life events (e.g., incarceration, homelessness). Healthcare utilization information was collected via interviewer-administered questionnaires; beginning in 1998, behavioral information was collected via Audio Computer-Assisted Self-Interview (ACASI). Participants were tested semi-annually for HIV infection.
Participants provided updated residential information at each study visit. Residential addresses were geocoded and mapped to US census tracts using ArcGIS version 9.3 (ESRI Inc, 2008). If participants reported homelessness, a shelter or temporary address was geocoded if available, otherwise it was excluded. Addresses from 1988–1999 were mapped to 1990 US Census tracts and addresses from 2000–2008 to 2000 US Census tracts. Neighborhood deprivation scores were created based on a scale previously validated in Baltimore, Maryland (32). Briefly, we conducted principal components analysis using the following eight indicators separately for 1990 and 2000: percent of individuals employed in professional/managerial occupations, percent of households with crowding, percent of households living in poverty, percent of female-headed households with dependent children (<18 years), percent of households on public assistance, percent of households earning low income, percent of individuals with less than high school education, and percent of unemployed males and females (>16 years). The resulting component, neighborhood deprivation, explained 68% and 64% of the total variability in Maryland in 1990 and 2000, respectively. Component loadings ranged from 0.27–0.40. Factor loadings were used to create standardized neighborhood deprivation scores for each census tract and quartiles were created based on cutoffs within Baltimore City. Residential relocation was defined as a change in residential information from the previous semi-annual visit. Residential relocation was further characterized according to deprivation in the origin and destination neighborhood.
Missing Data
Injection drug use and other covariates were carried forward for 1,299 short lapses in follow-up (up to 1.5 years). Data from the last study visit were carried forward and data from the subsequent study visit were dropped back for 447 longer lapses (1.5–2.2 years). Data from lapses greater in length than 2.2 years (<3% of visits) were not imputed and considered missing.
Statistical Analysis
The outcome of interest was long-term injection cessation, defined as six consecutive visits (three years) with no self-reported injection drug use. Differences in baseline characteristics by those who did and did not achieve cessation were examined using frequencies. Incidence rates of long-term injection cessation per person-year were calculated by baseline and time-varying characteristics.
Predictors of long-term injection cessation were identified using discrete-time survival analysis methods (complementary log-log). The time origin was the first eligible study visit (sixth consecutive visit following the second injecting visit). Individuals were censored either at the time of the outcome, death, when lost-to-follow-up, or administratively in June 2008. Time-fixed covariates included sex, age, race, educational attainment, marital status, income, employment, history of drug treatment, and years injected at baseline. Time-varying characteristics included injection-related behaviors (frequency and types of drugs injected, overdose), health care utilization (methadone maintenance, detoxification, inpatient admission, outpatient care, usual source of primary care), non-injection drug use (alcohol, marijuana, crack, snorting cocaine, snorting heroin), sexual behaviors (sex with an anonymous partner, sex with an IDU), HIV infection, and housing-related factors (residential relocation, homelessness) from the prior six months. Time-varying covariates were lagged to ensure temporality. Covariates were lagged six visits to correspond to the last visit where IDUs who achieved the outcome were injecting. Relocation, homelessness, and neighborhood deprivation were lagged five visits to correspond to the time when individuals who achieved the outcome stopped injecting (Figure 1).
Figure 1.
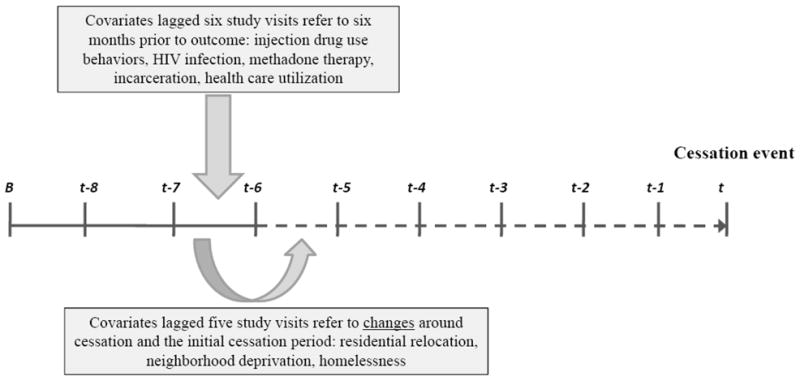
Diagram depicting cessation event and lagged covariates. Solid lines represent injection drug use, dotted lines represent no injection drug use. Cessation occurs at time t; baseline at time B.
We constructed several models; those that included neighborhood deprivation and residential relocation included a random-intercept to account for the clustering of participants within neighborhood. Model I included quartiles of neighborhood deprivation and individual-level factors. Model II added residential relocation, parameterized as a dichotomous variable (yes/no) in the prior six months. For Model III relocation was categorized by the level of deprivation in the origin and destination neighborhoods concurrent to cessation (i.e., lagged five semi-annual visits). The reference group was living in the most deprived neighborhood without having relocated in the prior six months. In adjusted models, non-injection cocaine and heroin use were combined into a single summary variable. Time-fixed socio-demographic factors and time-varying confounders that were included in all adjusted models were determined a priori from previous research (15,20,33). Adjusting for baseline demographic characteristics controlled for factors associated with selection into neighborhoods in Baltimore City, as well as injection behaviors. The time-varying confounders included preceded relocation (i.e., lagged six semi-annual visits) and were factors associated with drug use and drug use treatment in order to address any selection of neighborhood due to drug use behaviors (see Figure 1). Adjusted models were compared to the model with only time-fixed predictors using the change in log likelihood. Model fit was further examined using Akaike’s Information Criteria (AIC) and Bayesian Information Criteria (BIC) statistics, since some model comparisons were non-nested (34). All statistical analyses were conducted in Stata version 10.1 (College Station, TX).
RESULTS
Sample Characteristics
Of the 1,697 individuals, 75% were male, 95% were African-American, 57% did not have a high school diploma, and 66% had never married at the baseline assessment (Table 1). The median age was 35 years (IQR: 30–39) and the median number of years injected was 14 (IQR: 7–20). Approximately 50% reported injecting daily or more frequently and 65% reported injecting both heroin and cocaine (speedball).
Table 1.
Baseline (Time-fixed) Characteristics and Crude Hazard Ratios (and 95% Confidence Intervals [CI]) of Long-Term Injection Cessation among 1,697 Injection Drug Users in the ALIVE Study in Baltimore, Maryland (1988–2008).
| Total | No long-term cessation | Long-term cessation | Crude Hazard Ratio (95% CI) | |
|---|---|---|---|---|
| (n=1,697) | (n=991) | (n=706) | ||
| % | % | % | ||
| Total | 58.4 | 41.6 | -- | |
| Sex | ||||
| Male | 74.7 | 77.6 | 70.5 | 1.00 |
| Female | 25.3 | 22.4 | 29.5 | 1.16 (0.99, 1.37) |
| Age | ||||
| <30 yrs | 24.1 | 23.3 | 25.2 | 1.00 |
| 30–34 yrs | 28.1 | 27.0 | 29.5 | 1.01 (0.83, 1.23) |
| 35–39 yrs | 20.8 | 21.9 | 19.3 | 0.76 (0.61, 0.95) |
| >40 yrs | 27.1 | 27.8 | 26.1 | 1.11 (0.91, 1.36) |
| Race | ||||
| White/Other | 4.8 | 5.0 | 4.5 | 1.00 |
| African-American | 95.2 | 95.0 | 95.5 | 0.92 (0.67, 1.24) |
| Educational attainment | ||||
| Less than HS | 57.0 | 56.6 | 56.4 | 1.00 |
| HS diploma | 30.8 | 29.7 | 32.3 | 1.12 (0.95, 1.31) |
| Greater than HS | 12.7 | 13.7 | 11.3 | 0.88 (0.69, 1.12) |
| Marital status | ||||
| Never married | 65.7 | 66.8 | 64.0 | 1.00 |
| Married | 5.4 | 4.2 | 6.9 | 1.28 (0.96, 1.72) |
| Other | 29.0 | 29.0 | 29.0 | 1.04 (0.88, 1.22) |
| Income, annually at baseline | ||||
| <$5,000 | 75.9 | 76.5 | 73.7 | 1.00 |
| >=$5,000 | 24.1 | 23.5 | 26.3 | 1.16 (0.98, 1.37) |
| Employed at baseline | ||||
| No | 81.2 | 81.6 | 80.7 | 1.00 |
| Yes | 18.8 | 18.4 | 19.3 | 0.86 (0.57, 1.31) |
| History of drug treatment | ||||
| No | 41.6 | 43.9 | 38.4 | 1.00 |
| Yes | 58.4 | 56.1 | 61.6 | 1.12 (0.96, 1.30) |
| Number of years injected | ||||
| 1–7 years | 25.8 | 22.9 | 29.8 | 1.00 |
| 8–14 years | 25.1 | 25.7 | 24.4 | 0.90 (0.73, 1.10) |
| 15–20 years | 26.2 | 25.7 | 26.9 | 0.85 (0.70, 1.03) |
| Over 20 years | 22.9 | 25.8 | 19.0 | 0.81 (0.65, 1.00) |
The majority (58%) resided in the most deprived (4th quartile) neighborhoods over the study period; 24% resided in the 3rd quartile, 11% in the 2nd quartile, and only 7% in the least deprived (1st quartile). Study participants reported residential relocation in 30% of study visits. The median number of relocations per participant was 4 (IQR: 2–7), with 10% of participants reporting ten or more moves and 8% never having moved. Of the visits with a move, 44% were moves between or within the most deprived neighborhoods (see Figure 2).
Figure 2.
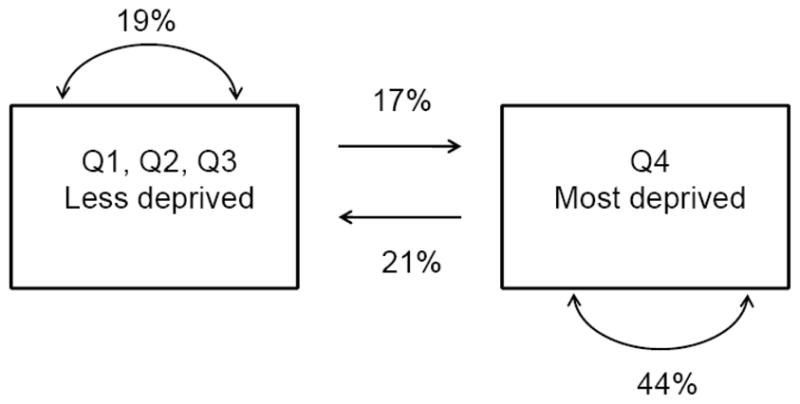
Diagram showing residential relocation between and within neighborhoods of differing levels of deprivation among ALIVE study participants in Baltimore City, 1988–2008. Q1–Q4: quartiles of neighborhood deprivation in Baltimore City.
Long-term Injection Cessation
Seven hundred and six individuals (42%) achieved long-term cessation (incidence rate: 7.6 per 100 person-years; 95% CI: 7.0, 8.1). The median time from the first eligible visit to long-term injection cessation was 9 years (IQR: 4–15). Forty-six of the 1,697 participants (3%) died before the median time to long-term injection cessation without having had the outcome and 14% (n=235) were alive, but were lost-to-follow-up without having had the outcome. Table 1 presents the frequency of long-term injection cessation by time-fixed characteristics. There were no significant associations between the incidence of long-term injection cessation and baseline characteristics.
Predictors of Long-term Injection Cessation
In unadjusted analyses, there was a dose-response relationship between quartiles of neighborhood deprivation at the time of cessation and long-term injection cessation (Table 2). Living in a highly deprived neighborhood decreased the likelihood of long-term injection cessation. Residential relocation predicted long-term injection cessation; however, the relationship varied by the type of origin and destination neighborhoods.
Table 2.
Crude Hazard Ratios and 95% Confidence Intervals (95% CI) of Long-Term Injection Cessation by Time-Varying Characteristics
| Crude Hazard Ratio (95% CI) | |
|---|---|
| Neighborhood deprivation, quartiles | |
| Q1: least deprived | 1.00 |
| Q2 | 0.98 (0.72, 1.34) |
| Q3 | 0.76 (0.58, 1.01) |
| Q4: most deprived | 0.55 (0.43, 0.71) |
| Residential relocation | 1.41 (1.20, 1.65) |
| Residential relocation by neighborhood quartile | |
| No move, Q1–Q3* | 1.00 |
| No move, Q4 | 0.72 (0.59, 0.88) |
| Moved, Q1–Q3 to Q1–Q3 | 1.26 (0.92, 1.71) |
| Moved, Q4 to Q1–Q3 | 1.75 (1.35, 2.27) |
| Moved, Q1–Q3 to Q4 | 1.12 (0.80, 1.58) |
| Moved, Q4 to Q4 | 0.87 (0.67, 1.13) |
| In the prior 6 months | |
| Homeless | 0.49 (0.38, 0.63) |
| HIV infection | 1.02 (0.87, 1.19) |
| Crack use | 0.56 (0.45, 0.70) |
| Snort cocaine | 0.41 (0.28, 0.62) |
| Snort heroin | 0.78 (0.61, 1.00) |
| Any alcohol use | 0.31 (0.26, 0.36) |
| Marijuana use | 0.52 (0.42, 0.63) |
| Frequency of injection | |
| Less than daily | 1.00 |
| Daily or more frequent | 0.45 (0.38, 0.53) |
| Type of drug injected | |
| Heroin only | 1.00 |
| Cocaine only | 0.93 (0.73, 1.20) |
| Mixed use | 0.42 (0.35, 0.52) |
| Overdose | 0.78 (0.53, 1.16) |
| Methadone maintenance | 1.61 (1.33, 1.93) |
| Detoxification | 2.29 (1.89, 2.77) |
| Inpatient admission | 1.47 (1.22, 1.76) |
| Outpatient care | 1.44 (1.21, 1.72) |
| Usual source of primary care | 1.16 (0.96, 1.39) |
| Sex with anonymous partner | 0.98 (0.77, 1.23) |
| Sex with IDU partner | 0.66 (0.56, 0.79) |
| Incarceration, at least 7 days | 0.76 (0.61, 0.96) |
Q1–Q4: Quartiles of neighborhood deprivation, where Q4 is the most deprived; Non-injection drug use, HIV, frequency of injection, type of drug injected, overdose, methadone, detoxification, inpatient admission, outpatient care, usual source of primary care, sexual behavior, and incarceration were lagged six study visits to precede cessation; Neighborhood deprivation, residential relocation, homelessness were lagged five study visits to correspond to the first visit of cessation; Neighborhood deprivation and residential relocation models included a random intercept.
Homelessness, daily injection, mixed cocaine/heroin injection, crack use, snorting cocaine, sex with an IDU partner, and recent incarceration were inversely related to long-term injection cessation. Methadone maintenance, recent detoxification, inpatient and outpatient care, were positively associated with long-term injection cessation. HIV-infection, recent overdose, having had a usual source of primary care, and sex with an anonymous partner were not associated with long-term injection cessation in unadjusted analysis.
In adjusted analysis, the dose-response relationship observed between long-term injection cessation and quartiles of neighborhood deprivation persisted (Model I), with long-term injection cessation being 29% and 43% less likely in neighborhoods of the third and fourth quartiles of deprivation compared with the least deprived quartile, respectively (HR=0.71, 95% CI: 0.53, 0.96; HR=0.57, 95% CI: 0.43, 0.76). Model II again demonstrated the dose-response relationship between neighborhood deprivation and long-term injection cessation; however, after controlling for residential relocation, which was associated with an increased likelihood of long-term injection cessation (HR=1.55, 95% CI: 1.31, 1.82), the associations were slightly weakened. Compared with no relocation and living in less deprived neighborhoods (Model III), staying in the most deprived neighborhoods decreased the likelihood of achieving long-term injection cessation (HR=0.76, 95% CI: 0.63, 0.93). Moving from the most deprived (Q4) to less deprived neighborhoods (Q1–Q3) increased the likelihood of long-term injection cessation by nearly twofold (HR=1.96, 95% CI: 1.50, 2.57), while moving within less deprived neighborhoods slightly increased the likelihood of the outcome (HR=1.39, 95% CI: 1.02, 1.89). There was no association between long-term injection cessation and moving within the most deprived neighborhoods (HR=1.01, 95% CI: 0.77, 1.32) or moving from a less deprived neighborhood into the most deprived neighborhoods (HR=1.26, 95% CI: 0.89, 1.79).
DISCUSSION
In this community-based cohort of IDUs, long-term injection cessation was frequently observed over 20 years of observation. Beyond the individual-level factors that have previously been associated with shorter periods of injection cessation, our analyses demonstrated an important role for contextual factors. Neighborhood deprivation impacted successful long-term injection cessation and relocation out of the most deprived neighborhoods appeared to be the most beneficial move for IDUs in relation to cessation.
This study is one of the first to examine long-term injection cessation in a community-based sample. Previous analyses in this cohort demonstrated that a large majority of IDUs quit injecting for short periods of time, however, more than three-quarters relapsed within one year of stopping (15,33). Interestingly, many of the individual-level factors such as homelessness, methadone maintenance, and less intense injection behaviors, previously identified as predictors of short-term cessation, were also important for long-term cessation. However, while use of non-injection cocaine was not a predictor of short-term injection cessation previously (15), it was associated with a decreased likelihood of long-term injection cessation. Our results collectively suggest that while some factors that facilitate short term-behavior change are also important for long-term behavior change, further research is needed to understand the relationships between injection, non-injection drug use, and long-term cessation.
Our study further expands on existing research by characterizing the role of environmental determinants. We observed that increased deprivation in residential neighborhoods was negatively associated with long-term injection cessation among IDUs. These findings support the results of other work in Baltimore that showed that neighborhood-level poverty was associated with decreased injection cessation in the short-term (20,21).
There are many potential social and economic mechanisms at work in highly deprived neighborhoods that impact drug use. Economically deprived neighborhoods foster and support active and visible drug markets more so than less disadvantaged neighborhoods (35–38). The presence and widespread exposure to drug markets may shape social norms regarding involvement in the drug trade and resultant drug use, creating social environments more tolerant of drug use and with limited social control against drug use. Neighborhoods with active drug markets may also have more visible cues to inject than neighborhoods with less active drug markets. A prior study in Baltimore reported that persistent injectors were more likely to have bought drugs near their residence compared to those who stopped injecting in the short-term (10), suggesting that living in an area where drugs are not readily accessible or tolerated may contribute to cessation. Together the same social and economic forces supporting the drug trade may function to impede cessation among active IDUs in the area.
It is also possible that the association between neighborhood deprivation and long-term injection cessation reflects the topography of social networks in deprived neighborhoods. Social networks in poor neighborhoods may have a higher density of individuals within the drug subculture and limited ties outside of poor neighborhoods. As a result, networks in poor neighborhoods may contain inadequate social and economic capital specifically supportive of behavior change and disengagement with the drug subculture. For example, living in deprived neighborhoods may constrain the number of network ties to employed individuals, a network property that has been shown to reduce drug use (21).
Finally deprived neighborhoods place a considerable psychosocial burden on residents, prompting continued drug use (26). In Baltimore neighborhood social disorder was recently shown to predict depressive symptoms among drug users, which were in turn predictive of injection behaviors (39). Additional research is needed to determine the specific mechanisms through which neighborhood deprivation, as well as additional features of the environmental context, acts on long-term injection behaviors and cessation.
The impact of neighborhood deprivation on long-term injection cessation was further reinforced by the observation that moving from a highly deprived into a less deprived neighborhood was predictive of sustained positive behavior change. Several studies have demonstrated how changes in environment were associated with reduced drug use behaviors and dependence (40, 27, 29). Changes in residential environments may reflect disruptions to the social and economic environments which constrain behaviors, or in the conditioned responses to cues and triggers in the environment. Prior studies have demonstrated that drug users form conditioned responses (e.g., craving, withdrawal symptoms) to elements of the environment when consistently paired with drug use (30,41); residential relocation to a new environment lacking such conditioned stimuli may reduce physiological prompts to use, resulting in increased probability of maintaining abstinence. However, in this study, the most beneficial move was from a highly deprived to a less deprived neighborhood. Moving between other types of neighborhoods did not demonstrate a positive association, suggesting that altering the social and economic contextual elements of the environment may be more important to long-term cessation than disrupting the conditioned elements of the environment. Our data suggest that the traditional strategy -- of changing “people, places and things”-- may work only for those who are able to markedly improve their social and economic surroundings. Residential relocation into less deprived neighborhoods is an appealing strategy in theory; however, the extent to which poor, inner city IDUs have the resources to relocate out of deprived neighborhoods is limited. In fact the vast majority of relocations in this study were between and within the most deprived neighborhoods.
The current study has several limitations. Problems related to violations of the exchangeability criteria due to the presence of time-varying exposures and confounders when the time-varying confounders are affected by prior exposure, such as the non-random allocation of people into neighborhoods in this study, limit our ability to make causal statements about the relationships observed (42). There may also be unmeasured common causes of residential relocation and long-term injection cessation. For example, residential relocation may be a proxy for previous attempts to quit injecting prior to study enrollment, or individual characteristics that foster upward mobility, among IDUs who have begun to change their behaviors and also relocate to sustain their behavior change.
The focus of our analysis was on predictors of cessation; thus we did not include covariates during the period of cessation because these might reflect consequences of cessation. With respect to incarceration and non-injection drug use, this is an important limitation. While the current analysis excluded long periods of incarceration due to the restrictions on the sample, it is possible that some of the IDUs who achieved long-term cessation did so at least partially during a period of incarceration. Additionally we examined only cessation of injection drugs, and acknowledge that the participants may have been using non-injection drugs during the cessation period.
Other limitations include potential survival bias since our sample was limited to IDUs who survived long enough to complete sufficient follow-up. Our analysis may not completely account for the competing risks of mortality and losses to follow-up. Drug use may also be influenced by factors operating on a smaller scale than the census tract, or IDUs may not spend the majority of their time in their neighborhood of residence. Administrative data were only available decennially and may not capture finer changes in neighborhood indicators over time; however, there was little substantive change in the indicators defining neighborhood deprivation in Baltimore City from the years 1990 to 2000. The semi-annual structure of data collection also limited our ability to determine the precise temporality of residential relocation during the prior six months. Finally, findings from this cohort of IDUs in Baltimore may not be generalizable to other IDU populations, particularly those who are younger and not African-American. However the results are relevant for marginalized groups with long histories of drug use, a growing population in the US and other countries.
Our findings collectively support efforts to treat addiction as a chronic condition and suggest that programs must offer treatment and care designed to maintain long-term behavioral changes among drug users (43). Given that there is no accepted definition of long-term cessation, future research should examine the appropriateness of three years as a measure of long-term changes in behaviors. Future research should also determine the mechanisms through which relocation and neighborhood deprivation impact long-term changes in drug use. Programs to promote cessation among drug users may consider improving the social and economic environment of the drug user in order to maximize effectiveness and decrease drug use in the long-term. As a start, programs may consider providing permanent stable housing options, outside of deprived neighborhoods, for IDUs who are stopping injecting (44, 45). The findings of this study add to our knowledge of injection drug use cessation; however, the recommendations offered here may also be considered by public health programs targeted to alcohol, tobacco, and other drug cessation, as well as other health behaviors that contribute to chronic conditions.
Table 3.
Adjusted* Hazard Ratios and 95% Confidence Intervals (95% CI) of Long-term Injection Cessation by Neighborhood Deprivation and Residential Relocation
| Adjusted Model I | Adjusted Model II | Adjusted Model III | |
|---|---|---|---|
| HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Neighborhood deprivation | |||
| Q1: least deprived | 1.00 | 1.00 | |
| Q2 | 0.90 (0.65, 1.26) | 0.91 (0.65, 1.27) | |
| Q3 | 0.71 (0.53, 0.95) | 0.72 (0.53, 0.96) | |
| Q4: most deprived | 0.57 (0.43, 0.76) | 0.58 (0.44, 0.77) | |
| Residential relocation | |||
| No | 1.00 | ||
| Yes | 1.55 (1.31, 1.82) | ||
| Residential relocation, by type of destination and origin neighborhood | |||
| No move, Q1–Q3† | 1.00 | ||
| No move, Q4 | 0.76 (0.63, 0.93) | ||
| Moved from Q1–Q3 to Q1–Q3 | 1.39 (1.02, 1.89) | ||
| Moved from Q4 to Q1–Q3 | 1.96 (1.50, 2.57) | ||
| Moved from Q1–Q3 to Q4 | 1.26 (0.89, 1.79) | ||
| Moved from Q4 to Q4 | 1.01 (0.77, 1.32) |
All models included a random intercept and adjusted for homelessness at time of cessation, methadone maintenance, detoxification, sex with an IDU partner, incarceration, non-injection drug use, alcohol use, and number of prior moves from time preceding cessation, and all baseline characteristics in Table 1;
Q1–Q4: Quartiles of neighborhood deprivation, where Q4 is the most deprived
Footnotes
Declaration of interest: This study was supported by the National Institute on Drug Abuse at the National Institutes of Health (Dissertation Research Award R36DA025501, and grant numbers R01DA012568, R01DA004334).
References
- 1.Robertson JR, Ronald PJ, Raab GM, Ross AJ, Parpia T. Deaths, HIV infection, abstinence, and other outcomes in a cohort of injecting drug users followed up for 10 years. BMJ. 1994;309:369–372. doi: 10.1136/bmj.309.6951.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bargagli AM, Sperati A, Davoli M, Forastiere F, Perucci CA. Mortality among problem drug users in Rome: an 18-year follow-up study, 1980–97. Addiction. 2001;96:1455–1463. doi: 10.1046/j.1360-0443.2001.961014559.x. [DOI] [PubMed] [Google Scholar]
- 3.Hulse GK, English DR, Milne E, Holman CD. The quantification of mortality resulting from the regular use of illicit opiates. Addiction. 1999;94:221–229. doi: 10.1046/j.1360-0443.1999.9422216.x. [DOI] [PubMed] [Google Scholar]
- 4.Lumbreras B, Jarrin I, del Amo J, Perez-Hoyos S, Muga R, Garcia-de la Hera M, et al. Impact of hepatitis C infection on long-term mortality of injecting drug users from 1990 to 2002: differences before and after HAART. AIDS. 2006;20:111–116. doi: 10.1097/01.aids.0000196164.71388.3b. [DOI] [PubMed] [Google Scholar]
- 5.Santibanez SS, Garfein RS, Swartzendruber A, Purcell DW, Paxton LA, Greenberg AE. Update and overview of practical epidemiologic aspects of HIV/AIDS among injection drug users in the United States. J Urban Health. 2006;83:86–100. doi: 10.1007/s11524-005-9009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372:1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- 7.Steensma C, Boivin JF, Blais L, Roy E. Cessation of injecting drug use among street-based youth. J Urban Health. 2005;82:622–637. doi: 10.1093/jurban/jti121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bouhnik AD, Carrieri MP, Rey D, Spire B, Gastaut JA, Gallais H, et al. Drug injection cessation among HIV-infected injecting drug users. Addict Behav. 2004;29:1189–1197. doi: 10.1016/j.addbeh.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Bruneau J, Brogly SB, Tyndall MW, Lamothe F, Franco EL. Intensity of drug injection as a determinant of sustained injection cessation among chronic drug users: the interface with social factors and service utilization. Addiction. 2004;99:727–737. doi: 10.1111/j.1360-0443.2004.00713.x. [DOI] [PubMed] [Google Scholar]
- 10.Sherman SG, Hua W, Latkin CA. Individual and environmental factors related to quitting heroin injection. Subst Use Misuse. 2004;39:1199–1214. doi: 10.1081/ja-120038683. [DOI] [PubMed] [Google Scholar]
- 11.Warner LA, Alegria M, Canino G. Remission from drug dependence symptoms and drug use cessation among women drug users in Puerto Rico. Arch Gen Psychiatry. 2004;61:1034–1041. doi: 10.1001/archpsyc.61.10.1034. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein MF, Deren S, Magura S, Kayman DJ, Beardsley M, Tortu S. Cessation of drug use: impact of time in treatment. J Psychoactive Drugs. 2000;32:305–310. doi: 10.1080/02791072.2000.10400454. [DOI] [PubMed] [Google Scholar]
- 13.Langendam MW, van Brussel GH, Coutinho RA, van Ameijden EJ. Methadone maintenance and cessation of injecting drug use: results from the Amsterdam Cohort Study. Addiction. 2000;95:591–600. doi: 10.1046/j.1360-0443.2000.95459110.x. [DOI] [PubMed] [Google Scholar]
- 14.Latkin CA, Knowlton AR, Hoover D, Mandell W. Drug network characteristics as a predictor of cessation of drug use among adult injection drug users: a prospective study. Am J Drug Alcohol Abuse. 1999;25:463–473. doi: 10.1081/ada-100101873. [DOI] [PubMed] [Google Scholar]
- 15.Shah NG, Galai N, Celentano DD, Vlahov D, Strathdee SA. Longitudinal predictors of injection cessation and subsequent relapse among a cohort of injection drug users in Baltimore, MD, 1988–2000. Drug Alcohol Depend. 2006;83:147–156. doi: 10.1016/j.drugalcdep.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 16.Genberg BL, Gange SJ, Go VF, Celentano DD, Kirk GD, Mehta SH. Trajectories of injection drug use over 20 years (1988–2008) in Baltimore, Maryland. Am J Epidemiol. 2011 doi: 10.1093/aje/kwq441. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glass TA, McAtee MJ. Behavioral science at the crossroads in public health: extending horizons, envisioning the future. Soc Sci Med. 2006;62:1650–1671. doi: 10.1016/j.socscimed.2005.08.044. [DOI] [PubMed] [Google Scholar]
- 18.Galea S, Ahern J, Vlahov D. Contextual determinants of drug use risk behavior: a theoretic framework. J Urban Health. 2003;80:50–58. doi: 10.1093/jurban/jtg082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61:1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 20.Nandi A, Glass TA, Cole SR, Chu H, Galea S, Celentano DD, et al. Neighborhood poverty and injection cessation in a sample of injection drug users. Am J Epidemiol. 2010;171:391–398. doi: 10.1093/aje/kwp416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams CT, Latkin CA. Neighborhood socioeconomic status, personal network attributes, and use of heroin and cocaine. Am J Prev Med. 2007;32:S203–210. doi: 10.1016/j.amepre.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fuller CM, Borrell LN, Latkin CA, Galea S, Ompad DC, Strathdee SA, et al. Effects of race, neighborhood, and social network on age at initiation of injection drug use. Am J Public Health. 2005;95:689–695. doi: 10.2105/AJPH.2003.02178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Latkin CA, Williams CT, Wang J, Curry AD. Neighborhood social disorder as a determinant of drug injection behaviors: a structural equation modeling approach. Health Psychol. 2005;24:96–100. doi: 10.1037/0278-6133.24.1.96. [DOI] [PubMed] [Google Scholar]
- 24.Galea S, Nandi A, Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26:36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 25.Schroeder JR, Latkin CA, Hoover DR, Curry AD, Knowlton AR, Celentano DD. Illicit drug use in one's social network and in one's neighborhood predicts individual heroin and cocaine use. Ann Epidemiol. 2001;11:389–394. doi: 10.1016/s1047-2797(01)00225-3. [DOI] [PubMed] [Google Scholar]
- 26.Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. J Health Soc Behav. 2001;42:151–165. [PubMed] [Google Scholar]
- 27.Maddux JF, Desmond DP. Residence relocation inhibits opioid dependence. Arch Gen Psychiatry. 1982;39:1313–1317. doi: 10.1001/archpsyc.1982.04290110065011. [DOI] [PubMed] [Google Scholar]
- 28.Leventhal T, Brooks-Gunn J. Moving to opportunity: an experimental study of neighborhood effects on mental health. Am J Public Health. 2003;93:1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rachlis BS, Wood E, Li K, Hogg RS, Kerr T. Drug and HIV-Related Risk Behaviors After Geographic Migration Among a Cohort of Injection Drug Users. AIDS Behav. 2008;14:854–861. doi: 10.1007/s10461-008-9397-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Childress AR, McLellan AT, O'Brien CP. Conditioned responses in a methadone population. A comparison of laboratory, clinic, and natural settings. J Subst Abuse Treat. 1986;3:173–179. doi: 10.1016/0740-5472(86)90018-8. [DOI] [PubMed] [Google Scholar]
- 31.Vlahov D, Anthony JC, Munoz A, Margolick J, Nelson KE, Celentano DD, et al. The ALIVE study, a longitudinal study of HIV-1 infection in intravenous drug users: description of methods and characteristics of participants. NIDA Res Monogr. 1991;109:75–100. [PubMed] [Google Scholar]
- 32.Messer LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, Culhane J, et al. The development of a standardized neighborhood deprivation index. J Urban Health. 2006;83:1041–1062. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Galai N, Safaeian M, Vlahov D, Bolotin A, Celentano DD. Longitudinal patterns of drug injection behavior in the ALIVE Study cohort,1988–2000: description and determinants. Am J Epidemiol. 2003;158:695–704. doi: 10.1093/aje/kwg209. [DOI] [PubMed] [Google Scholar]
- 34.Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford: Oxford University Press; 2003. [Google Scholar]
- 35.Saxe L, Kadushin C, Beveridge A, Livert D, Tighe E, Rindskopf D, et al. The visibility of illicit drugs: implications for community-based drug control strategies. Am J Public Health. 2001;91:1987–1994. doi: 10.2105/ajph.91.12.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Freisthler B, Lascala EA, Gruenewald PJ, Treno AJ. An examination of drug activity: effects of neighborhood social organization on the development of drug distribution systems. Subst Use Misuse. 2005;40:671–686. doi: 10.1081/ja-200055373. [DOI] [PubMed] [Google Scholar]
- 37.Storr CL, Chen CY, Anthony JC. “Unequal opportunity”: Neighborhood disadvantage and the chance to buy illegal drugs. J Epidemiol Community Health. 2004;58:231–237. doi: 10.1136/jech.2003.007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Crum RM, Lillie-Blanton M, Anthony JC. Neighborhood environment and opportunity to use cocaine and other drugs in late childhood and early adolescence. Drug Alcohol Depend. 1996;43:155–161. doi: 10.1016/s0376-8716(96)01298-7. [DOI] [PubMed] [Google Scholar]
- 39.Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. J Health Soc Behav. 2003;44:34–44. [PubMed] [Google Scholar]
- 40.Robins LN, Slobodyan S. Post-Vietnam heroin use and injection by returning US veterans: clues to preventing injection today. Addiction. 2003;98:1053–1060. doi: 10.1046/j.1360-0443.2003.00436.x. [DOI] [PubMed] [Google Scholar]
- 41.O'Brien CP, Childress AR, McLellan AT, Ehrman R. Classical conditioning in drug-dependent humans. Ann N Y Acad Sci. 1992;654:400–415. doi: 10.1111/j.1749-6632.1992.tb25984.x. [DOI] [PubMed] [Google Scholar]
- 42.Hernan MA, Hernandez-Diaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15:615–625. doi: 10.1097/01.ede.0000135174.63482.43. [DOI] [PubMed] [Google Scholar]
- 43.McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 44.Aidala A, Cross JE, Stall R, Harre D, Sumartojo E. Housing status and HIV risk behaviors: implications for prevention and policy. AIDS Behav. 2005;9:251–265. doi: 10.1007/s10461-005-9000-7. [DOI] [PubMed] [Google Scholar]
- 45.Acevedo-Garcia D, Osypuk TL, Werbel RE, Meara ER, Cutler DM, Berkman LF. Does housing mobility policy improve health? Hous Policy Debate. 2004;15:49–98. [Google Scholar]


