Abstract
Research on the implementation of smoking cessation counseling within substance abuse treatment organizations is limited. This study examines associations among counselors’ implementation of therapy sessions dedicated to smoking cessation, organizational factors, and counselor-level variables. A two-level hierarchical linear model including organization- and counselor-level variables was estimated using survey data collected from 1,794 counselors working in 359 treatment organizations. Overall implementation of smoking cessation counseling was low. In the final model, implementation was positively associated with counselors’ knowledge of the Public Health Service’ s clinical practice guideline, perceived managerial support, and belief that smoking cessation had a positive impact on recovery. Private versus public funding and presence of a formal smoking cessation program were organization-level variables which interacted with these counselor-level effects. These results highlight the importance of organizational contexts as well as counselors’ knowledge and attitudes for effective implementation of smoking cessation counseling in substance abuse treatment organizations.
Introduction
There is growing recognition that integrating smoking cessation services into the usual care delivered by substance abuse treatment facilities has high public health significance.1–7 Smoking cessation services address a significant need for this population given than 70–80% of individuals receiving substance abuse treatment also smoke tobacco products.8–11 Longitudinal research examining the causes of premature death among individuals treated for substance abuse has found that much of the risk can be attributed to tobacco-related diseases.12,13 In addition, recent research suggests that continued smoking following treatment increases the likelihood of substance abuse relapse,9,14 while quitting smoking within 1 year of treatment increases the odds of abstinence up to 9 years later.15 Treating individuals with substance use disorders and co-occurring nicotine dependence is recommended in the clinical practice guideline, Treating Tobacco Use and Dependence: 2008 Update, published by the US Public Health Service (PHS).16
Implementation and counselor characteristics
The implementation of smoking cessation services in substance abuse treatment, particularly psychosocial interventions, requires the active involvement of counseling staff. There is a small, but growing, literature on counselors’ attitudes toward smoking cessation and their implementation of these services. A review by Guydish and colleagues in 2007 identified seven surveys of program staff on the barriers to providing smoking cessation during substance abuse treatment.17 Several surveys of counselors’ attitudes and practices regarding smoking cessation occurred in the 1990s, before the publication of the PHS guideline.18–24 More recent research about smoking cessation in substance abuse treatment has tended to focus on the organizational adoption of services25–27 or counselors’ ratings of the importance of integrating smoking cessation into treatment.28 Few studies, however, have investigated how routinely counselors implement these interventions with their clients. An exception is recent work measuring staff practices within six substance abuse treatment clinics in the Western US.29,30 Staff in these community-based treatment settings reported infrequently asking patients about smoking, advising quitting, assisting patients in quitting, and recommending nicotine replacement therapy29; clients in these programs also reported receiving very little smoking cessation counseling.31
Implementation of smoking cessation counseling may be associated with counselor-level factors, particularly knowledge, attitudes, and personal tobacco use. The PHS’s guideline about treating tobacco use and dependence includes counseling interventions as a key element for treating nicotine dependence.16 Familiarity with this guideline should enhance counselors’ skills in delivering smoking cessation counseling and therefore be positively associated with implementation.
Counselors’ beliefs about the relationship between smoking cessation and recovery may also be associated with implementation. The classic work of Everett Rogers suggests that implementation is more likely if an innovation is perceived to be consistent with one’s beliefs.32 Earlier studies reported that some counselors worried that smoking cessation placed clients at heightened risk of relapse, although more recent data suggest that clinicians are becoming more supportive of smoking cessation.18,22,23
Finally, counselors’ own tobacco use may influence implementation of smoking cessation counseling. Previous research has found that clinical staff who smoke are less likely to encourage clients to quit smoking.17,19,23,33 These findings are consistent with Rogers’ argument about the importance of compatibility between the characteristics of innovations and characteristics of the individuals who are responsible for implementation.32 Recommending that clients quit smoking would be incompatible with counselors’ own behaviors if they themselves use tobacco products.
Implementation and organizational contexts
While individual characteristics are likely to be associated with implementation, formal and informal sources of support within organizational contexts may also be related to counselors’ implementation behaviors. For example, organizations may invest in training counselors about an innovation. These formal investments in training should yield benefits in terms of innovation implementation.34 Furthermore, organizational adoption of an innovative service or program may be positively associated with counselor-level implementation, although it may not guarantee that all counselors are involved in the implementation process. While the presence of a formal smoking cessation program at the organizational level may be positively associated with greater levels of implementation, it is possible that only certain counselors are responsible for implementing that program. Importantly, counselors have considerable autonomy in how they conduct their therapy sessions, so organization-level adoption is not necessarily a prerequisite for implementation. Some counselors may still counsel patients about smoking even in the absence of a dedicated program.
In addition to formal organizational commitments, informal organizational norms may also be associated with counselor-level implementation.35–37 In particular, perceptions regarding management’s support for an innovation is often a key factor in achieving effective implementation.34,37 If employees perceive a lack of managerial support, they may be less likely to effectively implement the innovation.38,39
A multilevel modeling approach to studying implementation
Both counselor- and organization-level variables may influence whether smoking cessation counseling is implemented by individuals within a given agency’s context. However, existing research on smoking cessation practices within substance abuse treatment organizations is limited by methodological shortcomings regarding nested designs. Previous studies have either ignored the organizational contexts of counselors or have included organizational characteristics within counselor-level data—an approach that violates the assumptions of ordinary least squares regression and fails to account for correlated errors among counselors nested within agencies.40
In the current study, counselors’ self-reported implementation of individual and group therapy sessions specifically dedicated to smoking cessation is described, using data from 1,794 counselors working in 359 treatment organizations. A multilevel model of counselor-level implementation is estimated in order to consider the relationships among implementation, organizational characteristics, and counselor-level variables. It is hypothesized that counselor-level implementation of smoking cessation counseling is associated with the organizational context as well as counselors’ knowledge, beliefs, and tobacco use behaviors. Specifically, the relative importance of (a) formal commitments to smoking cessation services at the organizational-level and (b) counselor-level perceptions of managerial support, knowledge, beliefs, and personal smoking status are examined in a two-level hierarchical linear modeling (HLM) investigation of implementation.
Methods
Samples and data collection
Treatment organizations were identified through their previous participation in the National Treatment Center Study (NTCS; n=1,167; thorough descriptions of the sampling procedures used in the NTCS have been previously published41,42). Of these treatment organizations, 90 were no longer in operation when re-contacted between September 2006 and January 2008. Among the 1,077 organizations still open, 923 administrators (85.7%) provided verbal informed consent and participated in a brief telephone interview about smoking cessation services. At the end of the interview, participating administrators were invited to provide a list of current counselors so each counselor could receive a survey packet mailed to the treatment organization’s address. This packet included a letter describing of the study, informed consent forms, the survey, a postage-paid return envelope, and an honorarium form; counselors received $20 for returning the questionnaire. Surveys were received from 2,127 counselors (55.5% response rate) working in 438 unique treatment organizations. The institutional review boards of the University of Georgia and University of Kentucky approved all research procedures.
Measures
Dependent variable
The dependent variable of interest was implementation of smoking cessation counseling. This mean scale was constructed from counselors’ responses to two items measuring how frequently they conduct individual and group therapy sessions specifically dedicated to smoking cessation (Cronbach’s α=0.76). A six-point Likert response format was used for each item, ranging from 0 (never) to 5 (very often).
Level 1 variables
Four tobacco-related indicators were measured at the level of individual counselors. A single item measured counselors’ perceptions about the extent of managerial support for smoking cessation services (0–5 scale, with higher response options indicate greater perceived support). Counselors also reported about the extent to which they were knowledgeable about the Public Health Service’ s clinical practice guideline (0–5 scale, with higher response options indicate higher levels of knowledge) and the perceived impact of smoking cessation interventions on recovery from substance abuse (1–5 scale, 1= “definitely decrease chances,” 3= “no effect,” 5= “definitely increase chances”).21 The fourth tobacco-related measure was personal tobacco use, consisting of three categories: current tobacco users (cigarettes or smokeless tobacco products), former tobacco users, and non-users (the reference category).
Socio-demographic characteristics included sex (1=female, 0=male), race/ethnicity (1=white, 0= nonwhite), and age in years. Mean substitution was used to address missing data on age for which 3% of cases were missing. Counselors were also asked about their educational attainment (1=master’s degree or higher, 0=less than master’s degree), and personal recovery status (1=in recovery from substance abuse, 0=not in recovery).
Level 2 variables
Two measures of formal organization-level commitments to smoking cessation were assessed during the interviews. First, administrators indicated the percentage of counselors who received training in counseling approaches to smoking cessation in the past year (divided by 100 for analyses). Mean substitution was used to address missing data on this variable (8% of organizations). Second, administrators indicated if the treatment center offered a formal smoking cessation program that included individual and/or group therapy sessions (1=formal program, 0= no formal program).
In addition, five basic organizational characteristics were drawn from the prior wave of NTCS data. Organizations were categorized by sample type (privately funded, therapeutic community, or publicly funded organization as the reference category). Treatment organizations were categorized based on available levels of care (inpatient/residential-only, mixture of inpatient/residential and outpatient, and outpatient-only as the reference category). Location in a hospital (1=hospital, 0= non-hospital), profit status (1=for-profit, 0=non-profit), and government ownership (1=govern-ment-owned, 0=not government-owned) were also measured.
Data analysis
Two-level HLM, a multilevel modeling framework for hierarchically structured data, was used to estimate models of implementation of smoking cessation counseling (HLM for Windows, version 6.08). While a counselor-level outcome was the focus of the study, the clustering of counselors within organizations created special considerations appropriate for multilevel analyses.40 Specifically, the characteristics, knowledge, attitudes, and behaviors of counselors within a single organization were likely to be more similar than those in different organizations, and organization-level variables (i.e., sample type, level of care, etc.) were by definition identical for counselors within a single organization. To address the complexities of hierarchically structured data, HLM analyses allowed the outcome for each counselor to depend on counselor-level variables (level 1), each of which could further depend on organization-level variables (level 2). In addition to accounting for the nesting of counselors within organizations, HLM methods allowed for the detection of cross-level interactions40; in other words, the associations between a counselor-level variable and the outcome of interest could differ depending on the value of an organization-level variable, and HLM analyses facilitated identification of these interactions.
Several data preparation steps were taken. To address variables with no meaningful zero values, counselor age was centered at the grand mean, while belief about the impact of smoking cessation on recovery was recoded from a 0–5 scale to a scale with a midpoint of 0, ranging from −2 to 2 (thus, negative values indicated belief that smoking cessation would detract from recovery, zero indicated belief in no effect, and positive values indicated belief in positive effects on recovery). Additionally, organizations with only one counselor (n=78) and those in which all counselors were missing the outcome variable (n=1) were excluded, leaving an average of six counselors nested within each of 359 organizations. Finally, counselors with missing data on the outcome variable or other level 1 variables were deleted listwise from models including those variables.
Following recommendations of Raudenbush and Bryk,40 model-building proceeded in four stages. Model 1 represented an unconditional means model, revealing organizational differences in mean levels of implementation of smoking cessation counseling, absent any independent variables. This model provided a baseline for comparing the fit of subsequent models that incorporated level 1 and 2 variables. Model 2 added level 1 variables, allowing for the determination of how counselor-level variables influenced the intercepts and slopes of implementation across organizations; this random coefficients model was akin to conducting separate regression models for each organization and obtaining the mean intercept and slope coefficients. Model 3, a random intercept model, omitted the level 1 variables, instead incorporating level 2 variables to determine the associations of organization-level variables with counselors’ implementation. Finally, the results of models 1–3 were reviewed to determine a theoretically- and empirically-derived final model 4; this random slopes and intercepts model included a meaningful and interpretable set of level 1 and 2 variables.
Results
Table 1 presents summary statistics for the counselor- and organization-level variables, both for the original full sample (2,127 counselors in 438 organizations) and the sample included in the final model (1,794 counselors in 359 organizations). Counselors reported limited knowledge of the PHS clinical practice guideline and moderate managerial support for smoking cessation. A majority indicated that smoking cessation would improve clients’ chances for recovery. At the organization level, only 17% reported offering a smoking cessation program, and on average, programs trained fewer than 20% of counselors about smoking cessation counseling in the past year (median=0%).
Table 1.
Counselor and organizational characteristics of full sample and sample from final model
| Full sample, percent (n) or mean (SD) | Final model sample, percent (n) or mean (SD) | |
|---|---|---|
| Counselor-level variablesa | ||
| Tobacco use status | ||
| Current tobacco user | 20.0% (425) | 20.6% (369) |
| Former tobacco user | 46.6% (991) | 47.8% (857) |
| Non-tobacco user | 30.8% (656) | 31.7% (568) |
| Knowledge of PHS guidelines | 1.3 (1.6) | 1.2 (1.6) |
| Perceived managerial support of smoking cessation services | 2.5 (1.8) | 2.5 (1.8) |
| Belief of impact of smoking cessation on client’s chances for maintaining recovery | 3.6 (1.0) | 3.6 (1.0) |
| Mean age in years | 45.9 (11.6) | 45.8 (11.5) |
| White | 67.3% (1432) | 69.5% (1247) |
| Female | 59.9% (1274) | 61.1% (1097) |
| Masters degree or higher | 41.4% (880) | 43.1% (774) |
| In recovery from substance abuse | 47.2% (1003) | 48.0% (862) |
| N of counselors | 2127 | 1794 |
| Organizational-level variables | ||
| Sample type | ||
| Publicly funded | 32.0% (140) | 34.0% (122) |
| Privately funded | 39.7% (174) | 39.0% (140) |
| Therapeutic community | 28.3% (124) | 27.0% (97) |
| Formal smoking cessation programb | 17.6% (77) | 17.3% (62) |
| Mean % counselors trained about smoking cessation counseling in the past year | 17.3 (30.9) | 16.1 (29.7) |
| Located in a hospital | 21.2% (93) | 20.6% (74) |
| Available levels of carec | ||
| Outpatient only | 34.0% (149) | 34.0% (122) |
| Inpatient only | 28.8% (126) | 28.4% (102) |
| Mixed inpatient/outpatient | 36.8% (161) | 37.3% (134) |
| For profit | 12.6% (55) | 10.9% (39) |
| Government owned | 10.5% (46) | 10.6% (38) |
| N of organizations | 438 | 359 |
Missing data for 1–4% of counselors for each counselor-level variable
Missing data for one agency
Missing data for two agencies
HLM results
Model 1
The unconditional mean model provided an estimate of the overall variation in levels of implementation of smoking cessation counseling (Table 2). The grand mean across organizations was 0.92 (SE=0.04), reflecting a low level of implementation. The intraclass correlation coefficient (ICC) was 0.22, indicating that 22% of the variance in implementation occurred between organizations, while 78% was attributable to within-organization effects. This ICC value suggested that HLM analyses were appropriate to investigate the associations of both counselor- and organization-level variables on implementation.43 Deviance of the model was 6,151.48, with two parameters estimated; these values were used in likelihood-ratio tests to assess comparative model fit with subsequent models.
Table 2.
Hierarchical linear modeling estimates of the effects of level 1 and 2 predictors on implementation of smoking cessation counseling
| Effects | Model 1: unconditional means estimate (RSE) | Model 2: random coefficient estimate (RSE) | Model 3: means as outcomes estimate (RSE) | Model 4: intercepts and slopes as outcomes estimate (RSE) |
|---|---|---|---|---|
| Level 1 fixed effects (counselors) | ||||
| Group average (intercept) | 0.92 (0.04)*** | 0.13 (0.08) | ||
| Current smokera | −0.10 (0.08) | |||
| Former smokera | 0.08 (0.06) | |||
| Knowledge of PHSa | 0.22 (0.02)*** | |||
| Perceived managerial supporta | 0.16 (0.01)*** | |||
| Belief re: recoverya | 0.16 (0.02)*** | |||
| Centered agea | −0.00 (0.00) | |||
| White | −0.03 (0.09) | |||
| Female | 0.04 (0.05) | |||
| Masters degree | −0.05 (0.05) | |||
| In recovery | −0.00 (0.05) | |||
| Level 2 fixed effects (agencies) | ||||
| Group average (intercept) | 0.78 (0.09)*** | |||
| Privately funded | −0.15 (0.11) | |||
| Therapeutic community | −0.08 (0.12) | |||
| Formal cessation program | 0.73 (0.13)*** | |||
| % Counselors trained/100 | 0.48 (0.18)** | |||
| Hospital | −0.13 (0.11) | |||
| Inpatient only | 0.02 (0.12) | |||
| Mixed in/outpatient | 0.07 (0.09) | |||
| For profit | 0.03 (0.13) | |||
| Government owned | 0.11 (0.15) | |||
| Cross-level interactions | ||||
| Group average (intercept) | 0.19 (0.07)* | |||
| Privately funded | −0.17 (0.10) | |||
| Therapeutic community | −0.01 (0.11) | |||
| Formal cessation program | 0.00 (0.19) | |||
| % Counselors trained/100 | 0.03 (0.21) | |||
| Current smokera | −0.17 (0.13) | |||
| Privately funded | 0.06 (0.17) | |||
| Therapeutic community | −0.05 (0.17) | |||
| Formal cessation program | 0.24 (0.20) | |||
| % Counselors trained/100 | 0.03 (0.25) | |||
| Former smokera | 0.06 (0.09) | |||
| Privately funded | 0.13 (0.13) | |||
| Therapeutic community | −0.20 (0.14) | |||
| Formal cessation program | 0.08 (0.18) | |||
| % Counselors trained/100 | −0.08 (0.23) | |||
| Knowledge of PHSa | 0.21 (0.03)*** | |||
| Privately funded | −0.09 (0.04)* | |||
| Therapeutic community | −0.01 (0.05) | |||
| Formal cessation program | 0.19 (0.05)** | |||
| % Counselors trained/100 | 0.00 (0.06) | |||
| Perceived managerial supporta | 0.14 (0.02)*** | |||
| Privately funded | 0.01 (0.03) | |||
| Therapeutic community | 0.02 (0.04) | |||
| Formal cessation program | 0.00 (0.06) | |||
| % Counselors trained/100 | 0.03 (0.05) | |||
| Belief re: recoverya | 0.11 (0.04)** | |||
| Privately funded | 0.03 (0.06) | |||
| Therapeutic community | 0.02 (0.06) | |||
| Formal cessation program | 0.04 (0.08) | |||
| % Counselors trained/100 | 0.18 (0.09) | |||
| Proportion variance explained | 29% (within) | 23% (between) | 22% (total) | |
| Deviance (number of parameters estimated) | 6,151.48 (2) | 5,079.47 (29) | 6,081.34 (2) | 5,272.24 (22) |
Est. Unstandardized estimate; RSE robust standard error
Level 1 predictors modeled as random effects
p<0.05,
p<0.01,
p<0.001
Model 2
The random coefficients model allowed for the investigation of the relationships between the counselor-level variables and the outcome of interest, while accounting for the nesting of counselors within organizations (Table 2). In this model, level 1 variables significantly and positively associated with implementation of smoking cessation counseling included knowledge of the PHS clinical practice guidelines, perception of management as supportive of smoking cessation services, and belief that smoking cessation would enhance progress toward recovery (all p’s<0.001). In addition, estimation of variance components revealed that the effects of being a current (p=0.01) or former (p=0.01) tobacco user, knowledge of PHS clinical practice guidelines (p<0.01), and perceiving managers as supportive of smoking cessation efforts (p=0.04) differed significantly across organizations, supporting their designation as random effects. Non-significant counselor-level variables included age, race/ethnicity, educational attainment, and personal recovery status. Compared to model 1, the inclusion of level 1 variables reduced within-organization variance by 29% and constituted a significantly better-fitting model (−2LL=1072.01, df=27, p<0.001).
Model 3
In the random intercepts model investigating the effects of level 2 variables (Table 2), the only organization-level variables significantly associated with implementation were the percentage of counselors within the organization trained in smoking cessation counseling in the past year (p= 0.001) and the availability of a formal smoking cessation program within the organization (p< 0.001). Both variables were positively associated with the outcome. The other organization-level measures (i.e., sample type, location in a hospital, available levels of care, profit status, and government ownership) were not significantly associated with implementation. The reduction in the variance component for the intercept, relative to model 1, indicated that adding the level 2 variables reduced between-group variance in implementation by 23%; a high level of variance associated with the intercept term suggested that significant unexplained variation between organizations still remained.
Model 4
To develop the final random slopes and intercepts model, empirical findings from models 1–3 were combined with theoretical considerations from the existing literature on innovation implementation (Table 2). Counselor-level variables were selected based on the significant variables from model 2, while organization-level variables were chosen based on statistical significance in model 3. In addition, sample type was included in model 4 to reflect the construction of the three separate samples of treatment organizations in the original NTCS. Inclusion of all counselor- and organization-level variables would have required the estimation of a prohibitive number of parameters, decreased power, and limited the interpretability of results. For these reasons, the reduced set of variables was selected for the final model.
Notable results in the final model included significant positive associations between implementation of smoking cessation counseling and three counselor-level variables: knowledge of PHS clinical guidelines (p<0.001), perceiving managers as supportive of smoking cessation practices (p<0.001), and the belief that smoking cessation would enhance clients’ progress toward recovery (p=0.01). Two cross-level interaction terms were also significant: The slope coefficient associated with knowledge of PHS clinical guidelines was significantly lower for privately-funded compared to publicly funded organizations (p=0.04), and was significantly higher for those organizations with formal smoking cessation programs compared to those without (p=0.001). Estimation of variance components suggested that the strengths of the relationships between implementation of smoking cessation counseling and (a) current smoking status, (b) former smoking status, and (c) knowledge of PHS clinical guidelines, differed significantly among organizations based on sample type, percentage of counselors trained in smoking cessation intervention, and existence of a formal smoking cessation program in the organization. The variance component of the level 1 intercept term was not significant, indicating that mean levels of implementation of smoking cessation counseling did not differ between organizations. Furthermore, the ICC for model 4 demonstrated that only 3% of the variance in the outcome variable was attributable to the between-groups effect. However, the inclusion of level 2 variables explained 22% of the total variance in implementation of smoking cessation counseling, highlighting the utility of HLM analyses for this type of research question and data structure. Fit of the final model was significantly better than that of model 1 (−2LL=879.24, df=20, p<0.001).
Examples of predicted values for specific scenarios
In HLM analyses with multiple level 1 and 2 variables as well as cross-level interaction terms, consideration of predicted values of the dependent variable can elucidate the meaning of the results. Examples presented in Figure 1 illustrate the predicted values of implementation of smoking cessation services associated with particular combinations of level 1 and 2 variables. (HLM equations used to calculate predicted values are available by request.)
Figure 1.
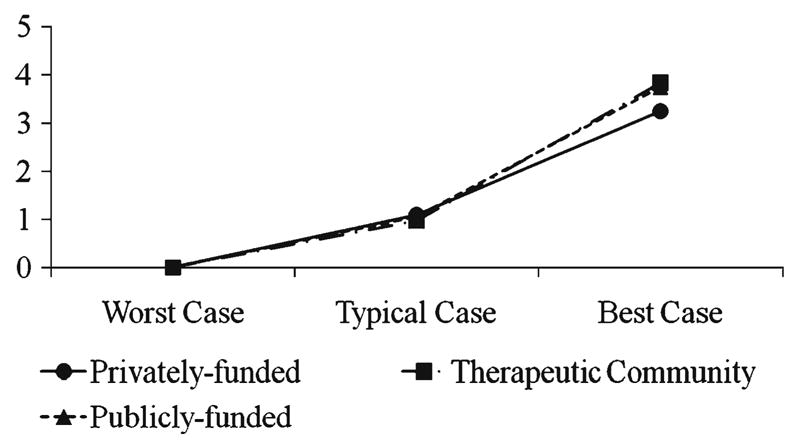
Predicted values of level of implementation of smoking cessation counseling for several scenarios within each type of organization. Appropriate values for level 1 and 2 predictors were substituted into HLM equations to represent worst case, typical case, and best case scenarios
“Worst-case” scenario
Predicted values for a “worst-case” scenario were obtained by substituting the appropriate values into the multilevel regression equations to represent a currently smoking individual with no knowledge of the PHS guideline, no perceived managerial support for smoking cessation services, and a belief that smoking cessation is very detrimental to recovery, who works in an organization with no formal smoking cessation program and no counselors trained in smoking cessation. Predicted values were calculated for the three types of organizations (i.e., privately funded, publicly funded, and therapeutic communities). Results are depicted in Figure 1. For all three groups, this combination of variables would likely result in no implementation of smoking cessation counseling (outcome=0, +/− random error).
“Best-case” scenario
Values were substituted into the equations to represent a non-smoking individual with the highest degree of knowledge of the PHS guideline, greatest perceived managerial support, and a belief that smoking cessation would have very positive effects on recovery, who works in an organization with a formal smoking cessation program and 100% of counselors trained in the past year (Fig. 1). Give or take random error, those working under these circumstances in therapeutic communities would be expected to report the highest degree of implementation of smoking cessation counseling (3.84; possible values ranged from 0 to 5), followed by those working in publicly funded organizations (3.76), and finally by those in privately funded organizations (3.25).
“Typical” scenario
Finally, predicted values were calculated using values for level 1 and 2 variables reflecting the most frequent responses observed in the data. This “typical” scenario represented a former smoker with no knowledge of the PHS practice guidelines, the greatest amount of perceived managerial support, and a belief that smoking cessation would have somewhat positive effect on recovery, who worked in an organization with no formal smoking cessation program and no counselors trained in smoking cessation counseling in the past year. Results are depicted in Figure 1 and suggest that, not accounting for fluctuations due to random error, counselors working at all three types of organizations would tend to report similar, relatively low levels of implementation (privately funded=1.10, publicly funded=1.06, TC=0.97).
Discussion
This research, which integrated data from a large number of counselors working in more than 350 treatment organizations, adds to the growing literature on the implementation of innovations. Hierarchical linear models supported the conceptualization of implementation of smoking cessation counseling as having both individual- and organization-level components. While most of the variance in implementation occurred at the counselor-level, the unconditional means model showed nearly one-quarter of the variance was attributable to differences between organizations.
Controlling for the nesting of counselors within organizations, influential level 1 variables were counselors’ knowledge of the PHS guideline, belief about the impact of smoking cessation on sobriety, and perceived managerial support for smoking cessation (models 2 and 4). These findings are consistent with the broader literature on innovation implementation, which has highlighted the importance of organizational leadership in communicating their support for the innovation to employees as well as the compatibility between an innovation and the beliefs of the individuals who are responsible for implementation.32,34,38 Previous studies have often attributed fears about smoking cessation promoting relapse as a barrier to integrating smoking cessation into addiction treatment centers. 44–46 The current findings suggest that such beliefs may remain a barrier to implementation, although endorsement of this negative attitude among counselors was not common.
Interestingly, counselors’ own tobacco use was not associated with the implementation of smoking cessation counseling in model 2. Earlier studies have suggested that current smokers were less likely to engage clients in the process of smoking cessation.17 It may be that the measure of implementation of counseling sessions dedicated to smoking cessation used in the current study reflects, in part, formal organizational decisions about service delivery in the form of counselors’ work assignments. Future research should also examine informal smoking cessation counseling or the extent to which counselors address tobacco-related issues on an ad-hoc basis during regular substance abuse treatment sessions. It may be the case that current tobacco use is more relevant for this type of informal counseling that occurs at the discretion of individual counselors.
The third model revealed that implementation was associated with the level 2 variables of counselor training and presence of a smoking cessation program. The independent association of implementation with training, controlling for the presence of a formal program, is particularly interesting, suggesting that the breadth of investment in training may yield measurable differences in implementation. In the final model, the presence of a formal smoking cessation program (but not percentage of counselors trained) influenced the magnitude of the relationship for counselor-level knowledge of PHS guidelines. Those counselors with higher levels of knowledge were even more likely to implement smoking cessation counseling when working in organizations with formal smoking cessation programs. Similarly, the association between counselor-level knowledge of PHS guidelines and implementation was greater among those working in publicly funded treatment organizations versus privately funded organizations.
As with any research, this study has several limitations that must be noted. First, these are cross-sectional data, limiting the ability to draw causal inferences. Second, all data were self-reported, so there may be errors due to over- or under-reporting. While direct observation of counseling sessions would yield more objective measures of implementation, such an approach would be clinically intrusive and highly costly. The response rate of 55% was slightly lower than prior studies of counselors,47 which may increase the risk of nonresponse bias. However, recent research suggests that response rates, in the absolute sense, are a weak predictor of nonresponse bias48 and that higher response rates may actually have limited impact on point estimates or substantive results.49,50 One particularly problematic form of nonresponse could occur if current tobacco users were less likely to respond to the survey. Although this cannot be directly ascertained, the rate of current tobacco use as reported by counselors (20.7%) is virtually identical to administrators’ average estimate of the percentage of clinical staff that smoke (mean=21.5%).51
Other limitations were related to requirements of HLM analyses with regard to data structure. In particular, 78 cases were lost to analysis because their programs only had data available from a single counselor; 119 counselors were missing the outcome variable; 23 counselors were excluded due to missing organization-level data in models 3 and 4; and missing level 1 predictors resulted in listwise deletion of 113 counselors from the final model. The 1,794 counselors in the final model represent 47% of counselors who were mailed the survey. However, both counselor- and organization-level sample characteristics for the final model were nearly identical to the descriptive statistics for the original full sample. Formal comparisons of included versus excluded cases at the counselor and program levels on the study variables revealed no differences at the Bonferroni-corrected levels of significance. Finally, these analyses may have been improved if there had been a larger number of counselors nested within each organization. Despite these limitations, however, this study contributes to the literature on innovation implementation by utilizing appropriate analytical methods capable of identifying both counselor- and organization-level variables associated with implementation.
Implications for Behavioral Health
Individuals treated for substance abuse are more likely to die from tobacco-related diseases than their use of alcohol or other drugs,12,13 which increases the importance of delivering smoking cessation services during substance abuse treatment. By extrapolating predicted levels of implementation of smoking cessation counseling using values consistent with a “best case” scenario, this research indicated that high levels of implementation may be possible. Building such a “best case” to support implementation may involve eliciting strong managerial support for smoking cessation services, widespread training of the counseling workforce, and establishing formal smoking cessation programs. Training efforts may improve counselors’ knowledge of the PHS clinical guideline and increase support for the belief that smoking cessation can help clients achieve stable recovery. Data from the “typical case” indicate, however, that the absence of these key elements may help to explain the current levels of implementation, which are quite low. Efforts aimed at increasing the implementation of evidence-based practices may benefit from attending to both organizational contexts and the counselors who responsible for implementing innovative services.
Acknowledgments
Primary data collection for this research and manuscript preparation was supported by the National Institute on Drug Abuse (R01DA020757). Construction of the original samples was also supported by NIDA (R01DA13110, R01DA14482, and R01DA14976) through research support to Dr. Paul M. Roman at the University of Georgia. The opinions expressed are those of the authors and do not represent the official position of the funding agency. The authors are grateful to the research staff at the University of Georgia, particularly Jennifer Shaikun who managed the counselor-level data collection.
Contributor Information
Hannah K. Knudsen, Email: hannah.knudsen@uky.edu, Department of Behavioral Science, University of Kentucky, 109 Medical Behavioral Science Bldg., Lexington, KY 40536-0086, USA. Phone: +1-859-3233947; Fax: +1-859-3235350.
Christina R. Studts, Email: tina.studts@uky.edu, Department of Behavioral Science, University of Kentucky, Lexington, KY, USA. Phone: +1-859-3231788; Fax: +1-859-3235350.
Jamie L. Studts, Email: jamie.studts@uky.edu, Department of Behavioral Science, University of Kentucky, Lexington, KY, USA. Phone: +1-859-3230895; Fax: +1-859-3235350.
References
- 1.Reid MS, Fallon B, Sonne S, et al. Implementation of a smoking cessation treatment study in substance abuse rehabilitation programs: Smoking behavior and treatment feasibility across varied community-based outpatient programs. Journal of Addiction Medicine. 2007;1:154–160. doi: 10.1097/ADM.0b013e31813872e4. [DOI] [PubMed] [Google Scholar]
- 2.Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: What you need to know. Journal of Substance Abuse Treatment. 2009;36:205–219. doi: 10.1016/j.jsat.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Schroeder SA, Morris CD. Confronting a neglected epidemic: Tobacco cessation for persons with mental illnesses and substance abuse problems. Annual Review of Public Health. 2010;31:297–314. doi: 10.1146/annurev.publhealth.012809.103701. [DOI] [PubMed] [Google Scholar]
- 4.Hall SM, Prochaska JJ. Treatment of smokers with co-occurring disorders: Emphasis on integration in mental health and addiction treatment settings. Annual Review of Clinical Psychology. 2009;5:409–431. doi: 10.1146/annurev.clinpsy.032408.153614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kalman D, Kim S, DiGirolamo G, et al. Addressing tobacco use disorder in smokers in early remission from alcohol dependence: The case for integrating smoking cessation services in substance use disorder treatment programs. Clinical Psychology Review. 2010;30:12–24. doi: 10.1016/j.cpr.2009.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prochaska JJ. Failure to treat tobacco use in mental health and addiction treatment settings: A form of harm reduction? Drug and Alcohol Dependence. 2010;110:177–182. doi: 10.1016/j.drugalcdep.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richter KP, Arnsten JH. A rationale and model for addressing tobacco dependence in substance abuse treatment. Substance Abuse Treatment, Prevention, and Policy. 2006;1:23. doi: 10.1186/1747-597X-1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kalman D, Hayes K, Colby SM, et al. Concurrent versus delayed smoking cessation treatment for persons in early alcohol recovery. A pilot study. Journal of Substance Abuse Treatment. 2001;20:233–238. doi: 10.1016/s0740-5472(00)00174-4. [DOI] [PubMed] [Google Scholar]
- 9.McCarthy WJ, Collins C, Hser YI. Does cigarette smoking affect drug abuse treatment? Journal of Drug Issues. 2002;32:61–80. [Google Scholar]
- 10.Richter KP, Ahluwalia HK, Mosier MC, et al. A population-based study of cigarette smoking among illicit drug users in the United States. Addiction. 2002;97:861–869. doi: 10.1046/j.1360-0443.2002.00162.x. [DOI] [PubMed] [Google Scholar]
- 11.Williams JM, Ziedonis D. Addressing tobacco among individuals with a mental illness or an addiction. Addictive Behaviors. 2004;29:1067–1083. doi: 10.1016/j.addbeh.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 12.Hurt RD, Offord KP, Croghan IT, et al. Mortality following inpatient addictions treatment. Role of tobacco use in a community-based cohort. JAMA. 1996;275:1097–1103. doi: 10.1001/jama.275.14.1097. [DOI] [PubMed] [Google Scholar]
- 13.Hser YI, McCarthy WJ, Anglin MD. Tobacco use as a distal predictor of mortality among long-term narcotics addicts. Preventive Medicine. 1994;23:61–69. doi: 10.1006/pmed.1994.1009. [DOI] [PubMed] [Google Scholar]
- 14.Lemon SC, Friedmann PD, Stein MD. The impact of smoking cessation on drug abuse treatment outcome. Addictive Behaviors. 2003;28:1323–1331. doi: 10.1016/s0306-4603(02)00259-9. [DOI] [PubMed] [Google Scholar]
- 15.Tsoh J, Chi FW, Mertens JR, et al. Stopping smoking during first year of substance use treatment predicted 9-year alcohol and drug treatment outcomes. Drug and Alcohol Dependence. 2011;114:110–118. doi: 10.1016/j.drugalcdep.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fiore MC, Jaen CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Dept. of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- 17.Guydish J, Passalacqua E, Tajima B, et al. Staff smoking and other barriers to nicotine dependence intervention in addiction treatment settings: a review. Journal of Psychoactive Drugs. 2007;39:423–433. doi: 10.1080/02791072.2007.10399881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gill BS, Bennett DL, Abu-Salha M, et al. Addiction professionals’ attitudes regarding treatment of nicotine dependence. Journal of Substance Abuse Treatment. 2000;19:317–318. doi: 10.1016/s0740-5472(00)00106-9. [DOI] [PubMed] [Google Scholar]
- 19.Bobo JK, Gilchrist LD. Urging the alcoholic client to quit smoking cigarettes. Addictive Behaviors. 1983;8:297–305. doi: 10.1016/0306-4603(83)90025-4. [DOI] [PubMed] [Google Scholar]
- 20.Bobo JK, Davis CM. Cigarette smoking cessation and alcohol treatment. Addiction. 1993;88:405–412. doi: 10.1111/j.1360-0443.1993.tb00828.x. [DOI] [PubMed] [Google Scholar]
- 21.Hurt RD, Croghan IT, Offord KP, et al. Attitudes toward nicotine dependence among chemical dependence unit staff–before and after a smoking cessation trial. Journal of Substance Abuse Treatment. 1995;12:247–252. doi: 10.1016/0740-5472(95)00024-y. [DOI] [PubMed] [Google Scholar]
- 22.Knapp JM, Rosheim CL, Meister EA, et al. Managing tobacco dependence in chemical dependency treatment facilities: a survey of current attitudes and policies. Journal of Addictive Diseases. 1993;12:89–104. doi: 10.1300/J069v12n04_07. [DOI] [PubMed] [Google Scholar]
- 23.Hahn EJ, Warnick TA, Plemmons S. Smoking cessation in drug treatment programs. Journal of Addictive Diseases. 1999;18:89–101. doi: 10.1300/J069v18n04_08. [DOI] [PubMed] [Google Scholar]
- 24.Weinberger AH, Reutenauer EL, Vessicchio JC, et al. Survey of clinician attitudes toward smoking cessation for psychiatric and substance abusing clients. Journal of Addictive Diseases. 2008;27:55–63. doi: 10.1300/J069v27n01_06. [DOI] [PubMed] [Google Scholar]
- 25.Friedmann PD, Jiang L, Richter KP. Cigarette smoking cessation services in outpatient substance abuse treatment programs in the United States. Journal of Substance Abuse Treatment. 2008;34:165–172. doi: 10.1016/j.jsat.2007.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richter KP, Choi WS, McCool RM, et al. Smoking cessation services in U.S. methadone maintenance facilities. Psychiatric Services. 2004;55:1258–1264. doi: 10.1176/appi.ps.55.11.1258. [DOI] [PubMed] [Google Scholar]
- 27.McCool RM, Richter KP, Choi WS. Benefits of and barriers to providing smoking treatment in methadone clinics: Findings from a national study. American Journal on Addictions. 2005;14:358–366. doi: 10.1080/10550490591003693. [DOI] [PubMed] [Google Scholar]
- 28.Fuller BE, Guydish J, Tsoh J, et al. Attitudes toward the integration of smoking cessation treatment into drug abuse clinics. Journal of Substance Abuse Treatment. 2007;32:53–60. doi: 10.1016/j.jsat.2006.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tajima B, Guydish J, Delucchi K, et al. Staff Knowledge, Attitudes, and Practices Regarding Nicotine Dependence Differ by Setting. Journal of Drug Issues. 2009;39:365–383. doi: 10.1177/002204260903900208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Delucchi KL, Tajima B, Guydish J. Development of the Smoking Knowledge, Attitudes, and Practices (S-Kap) Instrument. Journal of Drug Issues. 2009;39:347–363. doi: 10.1177/002204260903900207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guydish J, Tajima B, Chan M, et al. Measuring smoking knowledge, attitudes and services (S-KAS) among clients in addiction treatment. Drug and Alcohol Dependence. 2011;114:237–241. doi: 10.1016/j.drugalcdep.2010.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rogers EM. Diffusion of Innovations. 5. New York: Free Press; 2003. [Google Scholar]
- 33.Bobo JK, Slade J, Hoffman AL. Nicotine addiction counseling for chemically dependent patients. Psychiatric Services. 1995;46:945–947. doi: 10.1176/ps.46.9.945. [DOI] [PubMed] [Google Scholar]
- 34.Fixsen D, Naoom S, Blase K, et al. Implementation Research: A Synthesis of the Literature. Tampa: University of South Florida, Louis de la Parte Florida Mental Health Institute; 2005. [Google Scholar]
- 35.Klein KJ, Sorra JS. The challenge of innovation implementation. Academy of Management Review. 1996;21:1055–1080. [Google Scholar]
- 36.Rogers EM. Diffusion of innovations. 5. New York: Free Press; 1995. [Google Scholar]
- 37.Klein KJ, Conn AB, Sorra JS. Implementing computer technology: An organizational analysis. Journal of Applied Psychology. 2001;86:811–824. doi: 10.1037/0021-9010.86.5.811. [DOI] [PubMed] [Google Scholar]
- 38.Klein KJ, Knight AP. Innovation implementation - Overcoming the challenge. Current Directions in Psychological Science. 2005;14:243–246. [Google Scholar]
- 39.Rodgers JH, Barnett PG. Two separate tracks? A national multivariate analysis of differences between public and private substance abuse treatment programs. American Journal of Drug and Alcohol Abuse. 2000;26:429–442. doi: 10.1081/ada-100100254. [DOI] [PubMed] [Google Scholar]
- 40.Raudenbush SW, Bryk AS. Hierarchical linear models : applications and data analysis methods. 2. Thousand Oaks: Sage Publications; 2002. [Google Scholar]
- 41.Knudsen HK, Ducharme LJ, Roman PM. The use of antidepressant medications in substance abuse treatment: The public-private distinction, organizational compatibility, and the environment. Journal of Health and Social Behavior. 2007;48:195–210. doi: 10.1177/002214650704800207. [DOI] [PubMed] [Google Scholar]
- 42.Knudsen HK, Ducharme LJ, Roman PM. Counselor emotional exhaustion and turnover intention in therapeutic communities. Journal of Substance Abuse Treatment. 2006;31:173–180. doi: 10.1016/j.jsat.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 43.Kreft I, de Leeuw J. Introducing Multilevel Modeling. London: Sage; 1998. [Google Scholar]
- 44.Bobo JK, McIlvain HE, Lando HA, et al. Effect of smoking cessation counseling on recovery from alcoholism: findings from a randomized community intervention trial. Addiction. 1998;93:877–887. doi: 10.1046/j.1360-0443.1998.9368779.x. [DOI] [PubMed] [Google Scholar]
- 45.Burling TA, Burling AS, Latini D. A controlled smoking cessation trial for substance-dependent inpatients. Journal of Consulting and Clinical Psychology. 2001;69:295–304. doi: 10.1037//0022-006x.69.2.295. [DOI] [PubMed] [Google Scholar]
- 46.Ziedonis DM, Guydish J, Williams J, et al. Barriers and solutions to addressing tobacco dependence in addiction treatment programs. Alcohol Research & Health. 2006;29:228–235. [PMC free article] [PubMed] [Google Scholar]
- 47.Knudsen HK, Ducharme LJ, Roman PM, et al. Buprenorphine diffusion: The attitudes of substance abuse treatment counselors. Journal of Substance Abuse Treatment. 2005;29:95–106. doi: 10.1016/j.jsat.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 48.Groves RM, Peytcheva E. The impact of nonresponse rates on nonresponse bias: A meta-analysis. Public Opinion Quarterly. 2008;72:167–189. [Google Scholar]
- 49.Davern M, McAlpine D, Beebe TJ, et al. Are lower response rates hazardous to your health survey? An analysis of three state telephone health surveys. Health Services Research. 2010;45:1324–1344. doi: 10.1111/j.1475-6773.2010.01128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mealing NM, Banks E, Jorm LR, et al. Investigation of relative risk assessments from studies of the same population with contrasting response rates and designs. Bmc Medical Research Methodology. 2010;10:26. doi: 10.1186/1471-2288-10-26. http://www.biomedcentral.com/1471-2288/1410/1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Knudsen HK, Studts JL, Boyd S, et al. Structural and cultural barriers to the adoption of smoking cessation services in addiction treatment organizations. Journal of Addictive Diseases. 2010;29:294–305. doi: 10.1080/10550887.2010.489446. [DOI] [PMC free article] [PubMed] [Google Scholar]


