Abstract
Objectives
To measure the marginal and internal fit of three-unit fixed partial dentures (FPDs) using the micro-CT technique, testing the null hypothesis that there is no difference in the adaptation between the ceramic systems studied.
Methods
Stainless steel models of prepared abutments were fabricated to design the FPDs. Ten FPDs were produced from each framework ceramic (YZ - Vita In-Ceram YZ and IZ - Vita In-Ceram Zirconia) using CEREC inLab according to the manufacturer instructions. All FPDs were veneered using the recommended porcelain. Each FPD was seated on the original model and scanned using micro-CT. Files were processed using NRecon and CTAn software. Adobe Photoshop and Image J software were used to analyze the cross-sections images. Five measuring locations were used as follows: MG – marginal gap; CA - chamfer area; AW - axial wall; AOT - axio-occlusal transition area; OA - occlusal area. The horizontal marginal discrepancy (HMD) was evaluated in another set of images. Results were statistically analyzed using ANOVA and Tukey tests (α=0.05).
Results
The mean values for MG, CA, AW, OA and HMD were significantly different for all tested groups (p<0.05). IZ exhibited greater mean values than YZ for all measuring locations except for AW and AOT. OA showed the greatest mean gap values for both ceramic systems. MG and AW mean gap values were low for both systems.
Significance
The ceramic systems evaluated showed different levels of marginal and internal fit, rejecting the study hypothesis. Yet, both ceramic systems showed clinically acceptable marginal and internal fit.
Keywords: CAD-CAM, fixed partial dentures, zirconia, accuracy, non-destructive testing
Introduction
Ceramic systems with high crystalline content were introduced in dentistry with the objective of replacing the metal frameworks used for metal-ceramic crowns and fixed partial dentures (FPDs). All-ceramic structures are more translucent than the metallic ones, resulting in a natural-looking restoration [1, 2]. The finish line of the prepared tooth can be placed at the free gingival margin without compromising the esthetic appearance and avoiding the violation of the biological width, which reduces the risk of iatrogenic periodontal disease [3]. Also, ceramic materials have low thermal conductivity and are highly biocompatible [3-5].
Alumina and zirconia-based systems were developed to provide materials with superior mechanical properties to produce larger restorations, such as FPDs. The use of these materials was advanced by the introduction of the CAD/CAM technology, which made the processing method easier. Ceramic systems such as the yttria partially stabilized tetragonal zirconia polycristals (Y-TZP), e.g. In-Ceram YZ, and the glass-infiltrated zirconia-reinforced alumina-based ceramic, e.g. In-Ceram Zirconia (IZ), are available as prefabricated blocks for CAD/CAM processing [5].
In addition to esthetic and strength, all-ceramic restorations promise precision of fit. Poor marginal adaption can result in damage to the tooth, to the periodontal tissues and to the restoration [6]. Large marginal discrepancies result in dissolution of the luting agent and favor microleakage of bacteria and their byproducts [7]. As a consequence, the tooth becomes more susceptible to inflammation of the vital pulp (post-operative sensitivity), [8] secondary caries, and marginal discoloration [9]. Felton et al [10] investigated the in vivo the relationship between marginal adaptation and periodontal tissue health and noticed that an increase in the marginal discrepancy resulted in an increase in gingival inflammation. In addition, it has already been demonstrated that periodontal disease can be induced by changes in the subgingival microflora and plaque retention caused by an inadequate marginal adaptation [9, 11, 12].
The width of the internal adaptation (gap) or cement space is also an important aspect to be considered. Tuntiprawon and Wilson [13] observed that increasing the cement thickness of all-ceramic crowns reduced their fracture strength. In addition, there is evidence that excessive cement space could be related to failures on the veneering material [14]. The cement space should be uniform and facilitate seating without compromising retention or resistance forms [15].
The fitting accuracy of a restoration produced using the CAD/CAM technique is influenced by the scanning process, software design, milling and shrinkage effects [16, 17]. Y-TZP ceramic is available as: (1) fully sintered blocks fabricated by a process known as hot isostatic pressing (HIP), or (2) partially sintered pre-fabricated blocks, which are used to produce enlarged restorations to compensate the final sintering shrinkage. Milling of fully sintered blocks may produce more accurate fitting restorations but is associated to high wear rates of the milling burs and is time-consuming. Conversely, the increased milling efficiency obtained using partially-sintered blocks has the disadvantage of a potentially lower precision of fit due to the sintering shrinkage. Although a compensatory software design is used to guarantee an accurate fit, it is not sure that the shrinkage can be controlled in FPDs with long spans [5, 17, 18].
IZ is a ceramic core material used for CAD/CAM restorations. It consists of an alumina-based porous structure with addition of about 33% ceria partially stabilized zirconia infiltrated with a lanthanum oxide-based glass [19]. The system is available as dry-pressed blocks that can be milled into the final dimension and subsequently glass infiltrated [5, 16].
Most authors agree that marginal openings below 120 μm are clinically acceptable [15, 18, 20, 21]. There is a large range of marginal fit values related to the location of a crown and type of restoration [21]. In vitro investigations with YZ an IZ all-ceramic FPDs reported mean marginal gap values in a range of 9 to 110 μm [18, 22-28]. Reich et al [16, 29] evaluated the clinical fit of all-ceramic and metal-ceramic FPDs and showed mean marginal gap values from 54 to 95 μm. An in vivo study reported a mean gap value of 190 μm in the cervical area for YZ FPDs [30].
Different methods have been used to evaluate internal and marginal gaps. The clinical marginal fit can be roughly estimated directly with a mirror and a probe, or indirectly by taking an impression of the tooth and producing an epoxy replica that can be taken to an optical or scanning electron microscope [10]. The internal fit can be assessed by a replica technique, in which a silicon impression of the cement space is used [16, 21, 31, 32]. In laboratory studies, it is possible to section the tooth-restoration sample for direct evaluation under a microscope [13, 18, 24]. A new method that uses micro-computed tomography (micro-CT) has been applied for non-destructive analysis of the restorations [33, 34]. This technique allows 2D and 3D investigation of the marginal and internal gaps within the range of a few micrometers at multiples sites and directions [33].
The purpose of this study was to measure the marginal and internal fit of three-unit all-ceramic FPDs using the micro-CT technique. Two ceramic framework materials (Vita In-Ceram YZ and Vita In-Ceram Zirconia) were evaluated, testing two hypotheses: a) that there is no difference in the internal and marginal gaps between these two systems and b) that there is no difference among the gaps measured in different locations for both ceramic systems.
Materials and Methods
The experimental groups and materials used in this study are described in Table 1.
Table 1.
Experimental groups and materials used in this study.
| Groups | Framework material* and basic composition | Veneering material* |
|---|---|---|
| YZ | Vita In-Ceram YZ - yttria partially stabilized tetragonal zirconia polycristal |
Vita VM9 |
| IZ | Vita In-Ceram Zirconia - glass infiltrated zirconia- reinforced alumina-based ceramic |
Vita VM7 |
Vita Zahnfabrik, Bad Sackingen, Germany.
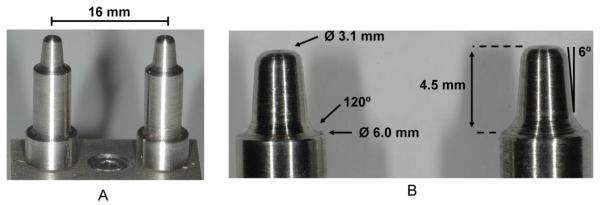
A stainless steel model simulating prepared abutment teeth was constructed. The prepared die has 4.5 mm height, 6° of taper and 120° chamfer as finish line, as proposed by Sundh et al [35] (Figure 1). The distance between the centers of the dies was 16 mm, corresponding to the distance between a lower second premolar and a lower second molar (span of 10 mm). An artificial gingiva was produced with acrylic resin (JET, Classico, Sao Paulo, SP, Brazil). A polyvinyl siloxane impression of the model was taken (Aquasil™, Dentsply, Petropolis, RJ, Brazil). A working cast was made using type IV special CAD/CAM stone (CAM-base, Dentona AG, Dortmund, Germany).
Figure 1.
A) Stainless steel models simulating prepared abutments; B) dimensions of the dies: 4.5 mm height, 6° of taper and 120° chamfer as finish line, 6.0 mm diameter in the marginal area and 3.1 mm diameter in the occlusal area.
The stone cast was digitized by the internal laser scanner component of CEREC inLab unit (Sirona Dental Systems, Charlote, NC, EUA) to generate a tridimensional image that was used to design the FPDs frameworks for both ceramic systems (YZ and IZ). After the milling process, YZ frameworks were sintered using the Zyrcomat furnace (Vita Zahnfabrik, Bad Sackingen, Germany) and IZ frameworks were glass infiltrated (Z21N Zirconia Glass Powder, Vita Zahnfabrik, Germany) using the Inceramat 3 furnace (Vita Zahnfabrik, Germany). The glass infiltration cycle was performed at 1110°C for 6 hours, according to the manufacturer’s instruction. The excess glass was removed with airborne particle abrasion using 50-μm aluminum oxide particles. Only the external surfaces of the FPDs were air abraded.
Vita In-Ceram YZ are porously pre-sintered zirconium dioxide blocks (Y-TZP), in which enlarged restorations are produced to compensate the final sintering shrinkage (around 20%). On the other hand, Vita In-Ceram Zirconia are dry-pressed blocks that can be milled into the final dimension, since these blocks are not subjected to a further sintering process, only to a glass infiltration process. Both types of ceramic blocks display a printed bar code, which can be read by the CEREC InLab scanner. This enables the shrinkage factor or absence of shrinkage of the batch used to be automatically read and taken into account for the grinding process in order to achieve an accurate final result. CEREC InLab software does not allow extensive customization. Thus, the manufacturer default recommendations were followed.
The frameworks were veneered with the manufacturer recommended porcelain, i.e., VM9 for YZ and VM7 for IZ. The porcelains were sintered according to the following cycle: pre-drying at 500°C for 6 min, heating to 910°C at a rate of 55°C/min under vacuum, heating at 960°C for 1 min and slow cooling (~6 min). Before veneering, a bonding agent (Effect Bonder, Vita Zahnfabrik, Bad Sackingen, Germany) was applied on the YZ framework in order to improve bonding between the core and veneering material. The bonding agent was sintered according to the cycle recommended by the manufacturer. Ten three-unit FPDs were fabricated for each group.
Each FPD was seated on the original stainless steel model and scanned by the micro-CT equipment SkyScan 1172 with 10 megapixel camera (Skyscan, Aartselaar, Belgium). The scanning parameters were: accelerating voltage of 100 kV, current of 100 μA, exposure time of 2950 ms per frame, Al+Cu filter, and rotation step at 0.4° (180° rotation). The x-ray beam was irradiated perpendicularly to the preparation long axis, and the image pixel size was 17 μm. The x-ray projections were reconstructed using SkyScan’s volumetric reconstruction software (Nrecon) that uses the set of acquired angular projections to create a set of cross section slices through the object. This program uses a modified Feldkamp algorithm with automatic adaptation to the scan geometry in each micro-CT scanner. Reconstructed slices were saved as a stack of bmp-type files. Beam hardening correction of 80% and ring artifact correction of 7 were used for the reconstruction. No internal adjustment was made in the crowns and the scanning procedure was performed before cementation.
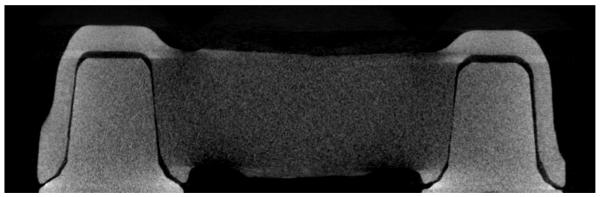
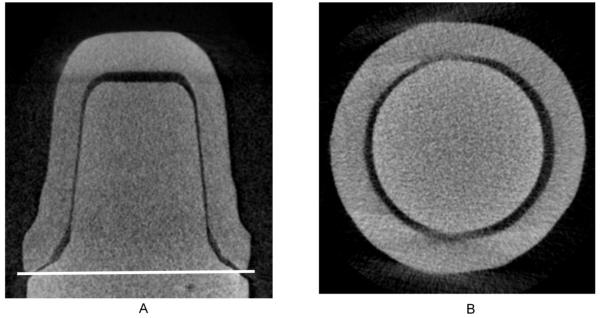
The CTAn software (Skyscan, Aartselaar, Belgium) was used to obtain cross-section images through the center of the die (x-axis), in the mesio-distal (Figure 2) and bucco-lingual directions (Figure 4A). Using this software it was possible to choose a region of interest (ROI) and the number of slices for the selected region. Therefore, the number of slices was standardized for all specimens, and the same slice, corresponding to the center of the crown, in both bucco-lingual and mesio-distal directions, was analyzed for each crown. These images were transferred to Adobe Photoshop software to delimit the internal space between the die and the crown, and Image J software was used to perform the measurements. All measurements were performed by a single examiner. The presence of small radiographic artifacts did not allow the use of any automatic tool. Therefore, all measurements were manually taken, and the measuring locations were standardized to minimize errors.
Figure 2.
Cross-section image of an IZ FPD in the mesio-distal direction.
Figure 4.
A) Cross-section image of a crown in the bucco-ligual direction (x-axis). The white line indicates where the HMD was recorded. B) Cross-section image in the y-axis used to measure the HMD.
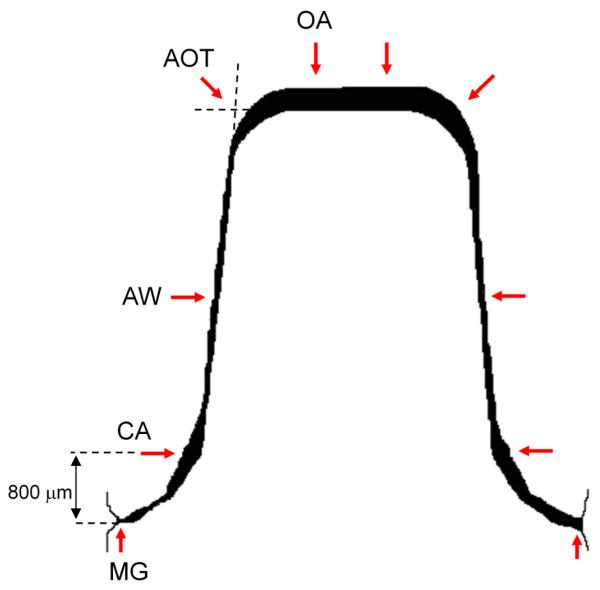
Five measuring locations were used (Figure 3): MG - marginal gap: perpendicular measurement from the internal surface of the crown to the margin of the die [12]; CA -chamfer area: 800 μm occlusal to the margin of the die; AW - axial wall: internal adaption at the midpoint of the axial wall; AOT - axio-occlusal transition area: transition from the occlusal plateau to the axial wall, this location was determined by the dotted lines in Figure 3; (5) OA - occlusal area: 500 μm from the axio-occlusal angle in the direction of the center of the occlusal plateau.
Figure 3.
Representation of the measuring locations: MG; CA; AW; AOT; OA.
In addition, cross-section images from the marginal area of the FPDs, taken at the horizontal plane (y-axis), were analyzed to measure the horizontal marginal discrepancy (HMD) (Figure 4). For this measurement, the selection of the slice that would be evaluated using the CTAn software was also standardized, as previously described. One slice from each crown was analyzed, and the mean horizontal marginal discrepancy was calculated using twelve measurement points.
For each material, results from different measurement points were statistically analyzed using one way analysis of variance (ANOVA) and Tukey tests at a significance level of 5%. To compare the values at each measurement location for the two ceramic systems t-test was used (p<0.05). The correlation between the measurement locations was tested using Pearson correlation test.
Results
The results at each measurement location for the two different abutments were compared using t-test (p<0.05) and no significant difference was found. Therefore, data from the two abutments were analyzed together to compare the different framework materials.
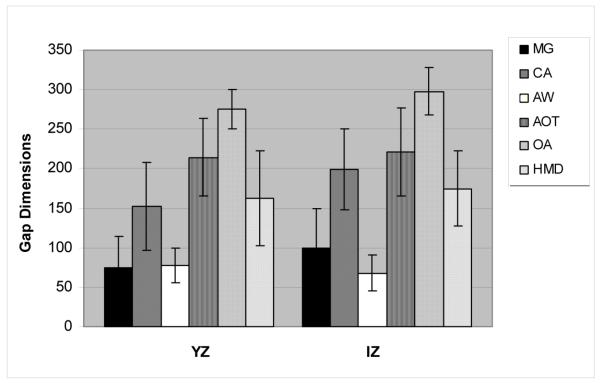
The mean and standard deviation values of the gaps (μm) at the different measuring locations and the statistical groupings are shown in Table 2 and Figure 5. IZ showed significantly greater mean gap values than YZ for locations MG, CA and OA. At these locations, the gap values for IZ were from 8 to 32% higher than those measured for YZ. At the measurement point AW, the gap value obtained for YZ was 15% higher than that of IZ, and this difference was also statistically significant. No statistical difference was found in the mean AOT values obtained for the two ceramic materials (p≥0.05).
Table 2.
Mean and standard deviation (SD) values of the gaps (μm) at the measurement points and statistical grouping for the experimental groups.
| Measuring Locations |
Mean and SD values for the gap (μm) | |
|---|---|---|
| YZ | IZ | |
| 1. MG | 75 (39) b D | 99 (60) a C |
| 2. CA | 150 (56) b C | 200 (51) a B |
| 3. AW | 78 (22) a D | 68 (23) b D |
| 4. AOT | 210 (49) a B | 220 (25) a B |
| 5. OA | 280 (25) b A | 300 (30) a A |
| HMD | 160 (47) b | 180 (47) a |
Mean values followed by similar small letters in same line do not show statistical difference (p≥0.05).
Mean values followed by similar capital letters in same column do not show statistical difference (p≥0.05).
Figure 5.
Gap dimensions (μm) for all measuring locations of both ceramic systems.
Analyzing the precision of fit of each material individually, it is possible to note that for both ceramics the measurement points OA and AOT gave significantly higher gap values compared to the other locations. Nevertheless, with regard to the other measurement locations, the two ceramic materials showed different results. While for IZ, the gap values obtained for CA, MG and AW were statistically different in this decreasing order, for YZ the gap value obtained at MG and AW were statistically similar and significantly lower than the value obtained for CA. As for the horizontal marginal discrepancy (HMD), the value obtained for IZ was 8% higher than that of YZ and this difference was statistically significant.
For YZ material, a small correlation (−0.3< r <−0.1 and 0.1< r <0.3) was found between the measurement points. Except for CA and OA that presented no correlation (r = −0.025, p= 0.825). Considering IZ group, a large correlation was found between MG and CA (r = 0.598, p= 0.001) and no correlation was observed between MG and AW (r = −0.040, p= 0.725) and between AW and OA (r = 0.014, p= 0.905).
Discussion
The use of all-ceramic systems for FPDs is increasing due to improvements in the mechanical properties of these materials and also to the development of superior CAD/CAM technologies. Long-term clinical evaluations of zirconia-based all-ceramic FPDs showed high success rate [6]. However, most complications were related to chipping of the veneering material, loss of retention of the restoration and presence of secondary caries [36-39]. Some of these problems may be related to the marginal and internal accuracy of the restorations. Thus, an adequate fit is an important factor in the restorative treatment prognosis.
The ceramic systems evaluated in the present study showed different levels of adaptation, rejecting the first hypothesis of this study. When the In-Ceram Zirconia system is used restorations can be milled directly in their final dimensions. Thus, it was expected that this system would have a superior fit compared to YZ, which requires predicting and compensating for the shrinkage resulting from sintering. Notwithstanding, IZ presented inferior marginal and internal adaptation than YZ. Hence, other factors related to the processing methods may be responsible for the observed differences in the adaptation level between the two systems. One possible explanation may reside in the fact that, even though at the moment of milling both IZ and YZ are very porous materials, they have different microstructure and hardness, which may affect in different ways how they interact with the CAD-CAM burs. It should be noted though that the better adaptation values obtained for YZ indicate that that CEREC InLab CAD/CAM system is able to successfully compensate the shrinkage due to sintering, even in large restorations like three-unit FPDs.
Metal-ceramic systems are considered to be a gold standard for prosthetic restorations. Although there is no control group in the present investigation, results from other studies suggested that restorations produced with CAD/CAM technology presented similar gap dimensions than metal-ceramic systems [16, 23]. A clinical evaluation showed differences in the mean cervical and axial gap values among zirconia-based and metal-ceramic FPDs. However, when the different die spacer thickness were taken into account and extracted from the measured gaps of both framework materials, no significant difference was observed between the systems [30].
Reich et al [16] investigated in vivo the internal and marginal fit of In-Ceram Zirconia FPDs and observed a mean marginal gap of 77 μm. They also measured the mid-axial gap, axio-occlusal transition gap and occlusal gap and found mean values around 156 μm, 210 μm and 343 μm, respectively. These mean values are higher than the ones found in the present study. One reason may be the fact that in vitro studies are performed in standardized conditions. Therefore many factors that are present in the clinical situation are neglected and the restoration fit is more precise [16]. Conversely, Beuer et al [24] observed better marginal and internal adaptation for In-Ceram YZ system than the mean values of the present study. This may be explained by the adaptation procedure used for the restorations previous to the measurements [24]. In the present investigation, no internal adjustment of the FPDs was performed. Studies reported mean marginal gap width varying from 47 μm to 88 μm for In-Ceram YZ system [23-25, 27, 28]. Bindl el al [27] measured the marginal and internal adaptation of In-Ceram Zirconia and In-Ceram YZ and found no differences between the systems. However, higher standard deviation values were observed for the In-Ceram Zirconia group, indicating a larger data scatter.
It is important to note that although the mean MG values obtained in the present study were statistically different for both ceramic systems tested, they were less than 120 μm, which is the reference MG value for clinical application [15, 18, 20, 21]. According to Tuntiprawon and Wilson [13] a mean axial wall width around 122 μm could reduce the fracture strength of the crowns. Considering such information and the mean axial wall values ranging from 68 μm to 78 μm in the present study, the ceramic systems examined should be adequate for clinical use. The occlusal area showed the largest gap for both ceramic systems. This could be a drawback if the space available for veneering is compromised [16].
The horizontal marginal discrepancy (HMD) was also measured in the present study and IZ showed higher mean value than YZ. It is important to differentiate the concepts of marginal gap and HMD. The measuring location, number of measurements per location and terminology can vary between studies. In this research the definition of marginal gap and HMD is according to Holmes et al [12], where the MG is a perpendicular measurement from the internal surface of the casting to the margin of the preparation and HMD is the horizontal marginal misfit measured perpendicular to the path of drawn of the casting. The marginal gap can be considered the most critical dimension, but still leaves unresolved the problem of overextended and underextended margins that can also be detrimental to the tooth and adjacent tissues [12].
The second hypothesis of this study was also rejected since that there were differences among the gap values measured in different locations for both ceramic systems. Both groups presented a similar pattern, larger mean gap values in the occlusal area, followed by the AOT and CA locations. Other studies also reported differences in the restoration fit according to the measuring locations [16, 18, 21]. Those studies reported an increase in the mean gap values from the marginal area to central measuring locations, suggesting that the adaptation of CAD/CAM restorations is less accurate in the internal areas.
These differences in the adaptation level as function of the location may be related to the quality of acquisition and processing of the digital data, as this is an important factor for the restoration accuracy when using CAD-CAM technology [17]. CEREC InLab has a laser triangulation scanner in the milling unit, which creates line by line a three-dimensional model [40]. An increase of internal discrepancy can result from rounded edges produced because of the finite scanning resolution of the measuring system [41]. A phenomenon called “overshoot”, that simulate virtual peaks near the edges, can also be responsible for wider internal gaps [16, 42]. Considering the CAM process, the diameter and shape of the milling instrument can limit the machining of internal contours [16, 17, 41].
A small AW mean value could be related to larger MG and OA dimensions if there was a misfit in the restoration. However, there was no correlation between the AW and the MG or the OA dimensions for IZ group. Although there was a negative correlation between this measurement points for YZ group, the correlation coefficient (r) was small (approximately −0.15). These results suggest that additional adaptation procedure in the axial wall area would not significantly improve the restoration fit in the marginal and occlusal areas.
Metal dies were used in the present study to standardize the preparations that have chamfer finish line and flat occlusal surface. Lin et al [43] investigated the effect of preparation form on the fit of CAD/CAM produced crowns. They reported that chamfer and shoulder designs presented similar external marginal openings. The occlusal flat form produced adequate internal fit to the axial wall and central groove area, but at the cusp tips adaptation was inferior to other occlusal designs. In comparison, Bindl et al [27] observed better marginal adaptation for shoulder than for chamfer preparation. However, they also noticed that the chamfer design allowed a smaller internal gap. These findings suggest that the preparation form used in our investigation could also have some influence in the final results.
In the present study, the FPDs were scanned after veneering the ceramic framework, which corresponds to a more clinically relevant situation. A study by Sulaiman et al [44] evaluated the marginal discrepancies of all-ceramic systems and reported no significant differences among the three stages of porcelain application.
Micro-CT is a non-destructive method of analysis that allows high resolution investigation of the internal gap between tooth preparation and the restoration. 2D and 3D measurements can be performed in any angle or position. Therefore, in the present study, the marginal fit could be evaluated in the x- and y-axes, providing a more realistic perception of the internal and marginal gaps. However, is not possible to perform an accurate analysis in cases where insufficient radiographic contrast exists. Therefore, to improve the contrast between the metal die, the ceramic restoration and the internal gap, the scanning procedure was done without cementation. In addition, considering that all FPDs were produced using only one model and that all FPDs should be seated on the original model to obtain a reliable evaluation of the gap dimension, if the FPDs were cemented, after scanning, each FPD would have to be removed from the model to cement a new one. This process could cause some damage to the model and interfere with the gap measurement results. This fact also influenced the decision not to cement the FPDs. However, this could be considered a study limitation since the influence of the luting procedure and cement type in the gap width was neglected [33].
Although slices from the 3D reconstruction were analyzed, due to a small radiographic artifact produced by the asymmetric shape of the FPD, the limits between the metal dies and the restoration were not clear enough to perform a 3D analysis (i.e. to measure the volumetric dimension of the gap). Studies by Seo et al [33] and Pelekanos et al [34] applied the micro-CT technique to evaluate the fit of ceramic crowns and suggested that this method can be recommended as a useful tool for the marginal and internal fit evaluation of dental restorations. The authors of the present study corroborate with this recommendation.
Conclusions
The ceramic systems evaluated showed different levels of marginal and internal fit, rejecting the first study hypothesis. YZ showed lower gap values than IZ FPDs, for the majority of the measuring locations. The second study hypothesis was also rejected since there were differences among the gap values measured in different locations for these ceramic systems. Despite of the differences, both ceramic systems demonstrated clinically acceptable fit at the marginal and internal areas.
Acknowledgements
The authors acknowledge the Brazilian agencies FAPESP, CNPq and CAPES for the financial support of the present research.
This investigation was also supported in part by research grants DE013358 and DE017991 from the NIH-NIDCR.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Heffernan MJ, Aquilino SA, Diaz-Arnold AM, Haselton DR, Stanford CM, Vargas MA. Relative translucency of six all-ceramic systems. Part II: core and veneer materials. J Prosthet Dent. 2002;88(1):10–5. [PubMed] [Google Scholar]
- 2.Heffernan MJ, Aquilino SA, Diaz-Arnold AM, Haselton DR, Stanford CM, Vargas MA. Relative translucency of six all-ceramic systems. Part I: core materials. J Prosthet Dent. 2002;88(1):4–9. [PubMed] [Google Scholar]
- 3.Raigrodski AJ, Chiche GJ. The safety and efficacy of anterior ceramic fixed partial dentures: A review of the literature. J Prosthet Dent. 2001;86(5):520–5. doi: 10.1067/mpr.2001.120111. [DOI] [PubMed] [Google Scholar]
- 4.Sorensen JA, Cruz M, Mito WT, Raffeiner O, Meredith HR, Foser HP. A clinical investigation on three-unit fixed partial dentures fabricated with a lithium disilicate glass-ceramic. Pract Periodontics Aesthet Dent. 1999;11(1):95–106. quiz 108. [PubMed] [Google Scholar]
- 5.Della Bona A. Bonding to ceramics: scientific evidences for clinical dentistry. 1° ed. Artes Médicas; 2009. p. 254. [Google Scholar]
- 6.Della Bona A, Kelly JR. The clinical success of all-ceramic restorations. J Am Dent Assoc. 2008;139(Suppl):8S–13S. doi: 10.14219/jada.archive.2008.0361. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs MS, Windeler AS. An investigation of dental luting cement solubility as a function of the marginal gap. J Prosthet Dent. 1991;65(3):436–42. doi: 10.1016/0022-3913(91)90239-s. [DOI] [PubMed] [Google Scholar]
- 8.Bergenholtz G, Cox CF, Loesche WJ, Syed SA. Bacterial leakage around dental restorations: its effect on the dental pulp. J Oral Pathol. 1982;11(6):439–50. doi: 10.1111/j.1600-0714.1982.tb00188.x. [DOI] [PubMed] [Google Scholar]
- 9.Valderhaug J, Heloe LA. Oral hygiene in a group of supervised patients with fixed prostheses. J Periodontol. 1977;48(4):221–4. doi: 10.1902/jop.1977.48.4.221. [DOI] [PubMed] [Google Scholar]
- 10.Felton DA, Kanoy BE, Bayne SC, Wirthman GP. Effect of in vivo crown margin discrepancies on periodontal health. J Prosthet Dent. 1991;65(3):357–64. doi: 10.1016/0022-3913(91)90225-l. [DOI] [PubMed] [Google Scholar]
- 11.Lang NP, Kiel RA, Anderhalden K. Clinical and microbiological effects of subgingival restorations with overhanging or clinically perfect margins. J Clin Periodontol. 1983;10(6):563–78. doi: 10.1111/j.1600-051x.1983.tb01295.x. [DOI] [PubMed] [Google Scholar]
- 12.Holmes JR, Bayne SC, Holland GA, Sulik WD. Considerations in measurement of marginal fit. J Prosthet Dent. 1989;62(4):405–8. doi: 10.1016/0022-3913(89)90170-4. [DOI] [PubMed] [Google Scholar]
- 13.Tuntiprawon M, Wilson PR. The effect of cement thickness on the fracture strength of all-ceramic crowns. Aust Dent J. 1995;40(1):17–21. doi: 10.1111/j.1834-7819.1995.tb05607.x. [DOI] [PubMed] [Google Scholar]
- 14.Rekow D, Thompson VP. Near-surface damage--a persistent problem in crowns obtained by computer-aided design and manufacturing. Proc Inst Mech Eng H. 2005;219(4):233–43. doi: 10.1243/095441105X9363. [DOI] [PubMed] [Google Scholar]
- 15.May KB, Russell MM, Razzoog ME, Lang BR. Precision of fit: the Procera AllCeram crown. J Prosthet Dent. 1998;80(4):394–404. doi: 10.1016/s0022-3913(98)70002-2. [DOI] [PubMed] [Google Scholar]
- 16.Reich S, Wichmann M, Nkenke E, Proeschel P. Clinical fit of all-ceramic three-unit fixed partial dentures, generated with three different CAD/CAM systems. Eur J Oral Sci. 2005;113(2):174–9. doi: 10.1111/j.1600-0722.2004.00197.x. [DOI] [PubMed] [Google Scholar]
- 17.Tinschert J, Natt G, Hassenpflug S, Spiekermann H. Status of current CAD/CAM technology in dental medicine. Int J Comput Dent. 2004;7(1):25–45. [PubMed] [Google Scholar]
- 18.Beuer F, Naumann M, Gernet W, Sorensen JA. Precision of fit: zirconia three-unit fixed dental prostheses. Clin Oral Investig. 2009;13(3):343–9. doi: 10.1007/s00784-008-0224-6. [DOI] [PubMed] [Google Scholar]
- 19.Della Bona A, Donassollo TA, Demarco FF, Barrett AA, Mecholsky JJ., Jr. Characterization and surface treatment effects on topography of a glass-infiltrated alumina/zirconia-reinforced ceramic. Dent Mater. 2007;23(6):769–75. doi: 10.1016/j.dental.2006.06.043. [DOI] [PubMed] [Google Scholar]
- 20.McLean JW, von Fraunhofer JA. The estimation of cement film thickness by an in vivo technique. Br Dent J. 1971;131(3):107–11. doi: 10.1038/sj.bdj.4802708. [DOI] [PubMed] [Google Scholar]
- 21.Kokubo Y, Ohkubo C, Tsumita M, Miyashita A, Vult von Steyern P, Fukushima S. Clinical marginal and internal gaps of Procera AllCeram crowns. J Oral Rehabil. 2005;32(7):526–30. doi: 10.1111/j.1365-2842.2005.01458.x. [DOI] [PubMed] [Google Scholar]
- 22.Gonzalo E, Suarez MJ, Serrano B, Lozano JF. Marginal fit of Zirconia posterior fixed partial dentures. Int J Prosthodont. 2008;21(5):398–9. [PubMed] [Google Scholar]
- 23.Gonzalo E, Suarez MJ, Serrano B, Lozano JF. Comparative analysis of two measurement methods for marginal fit in metal-ceramic and zirconia posterior FPDs. Int J Prosthodont. 2009;22(4):374–7. [PubMed] [Google Scholar]
- 24.Beuer F, Aggstaller H, Edelhoff D, Gernet W, Sorensen J. Marginal and internal fits of fixed dental prostheses zirconia retainers. Dent Mater. 2009;25(1):94–102. doi: 10.1016/j.dental.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 25.Att W, Komine F, Gerds T, Strub JR. Marginal adaptation of three different zirconium dioxide three-unit fixed dental prostheses. J Prosthet Dent. 2009;101(4):239–47. doi: 10.1016/S0022-3913(09)60047-0. [DOI] [PubMed] [Google Scholar]
- 26.Tinschert J, Natt G, Mautsch W, Spiekermann H, Anusavice KJ. Marginal fit of alumina-and zirconia-based fixed partial dentures produced by a CAD/CAM system. Oper Dent. 2001;26(4):367–74. [PubMed] [Google Scholar]
- 27.Bindl A, Mormann WH. Fit of all-ceramic posterior fixed partial denture frameworks in vitro. Int J Periodontics Restorative Dent. 2007;27(6):567–75. [PubMed] [Google Scholar]
- 28.Komine F, Gerds T, Witkowski S, Strub JR. Influence of framework configuration on the marginal adaptation of zirconium dioxide ceramic anterior four-unit frameworks. Acta Odontol Scand. 2005;63(6):361–6. doi: 10.1080/00016350500264313. [DOI] [PubMed] [Google Scholar]
- 29.Reich S, Kappe K, Teschner H, Schmitt J. Clinical fit of four-unit zirconia posterior fixed dental prostheses. Eur J Oral Sci. 2008;116(6):579–84. doi: 10.1111/j.1600-0722.2008.00580.x. [DOI] [PubMed] [Google Scholar]
- 30.Wettstein F, Sailer I, Roos M, Hammerle CH. Clinical study of the internal gaps of zirconia and metal frameworks for fixed partial dentures. Eur J Oral Sci. 2008;116(3):272–9. doi: 10.1111/j.1600-0722.2008.00527.x. [DOI] [PubMed] [Google Scholar]
- 31.Boening KW, Wolf BH, Schmidt AE, Kastner K, Walter MH. Clinical fit of Procera AllCeram crowns. J Prosthet Dent. 2000;84(4):419–24. doi: 10.1067/mpr.2000.109125. [DOI] [PubMed] [Google Scholar]
- 32.Fransson B, Oilo G, Gjeitanger R. The fit of metal-ceramic crowns, a clinical study. Dent Mater. 1985;1(5):197–9. doi: 10.1016/s0109-5641(85)80019-1. [DOI] [PubMed] [Google Scholar]
- 33.Seo D, Yi Y, Roh B. The effect of preparation designs on the marginal and internal gaps in Cerec3 partial ceramic crowns. J Dent. 2009;37(5):374–82. doi: 10.1016/j.jdent.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 34.Pelekanos S, Koumanou M, Koutayas SO, Zinelis S, Eliades G. Micro-CT evaluation of the marginal fit of different In-Ceram alumina copings. Eur J Esthet Dent. 2009;4(3):278–92. [PubMed] [Google Scholar]
- 35.Sundh A, Molin M, Sjogren G. Fracture resistance of yttrium oxide partially-stabilized zirconia all-ceramic bridges after veneering and mechanical fatigue testing. Dent Mater. 2005;21(5):476–82. doi: 10.1016/j.dental.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 36.Molin MK, Karlsson SL. Five-year clinical prospective evaluation of zirconia-based Denzir 3-unit FPDs. Int J Prosthodont. 2008;21(3):223–7. [PubMed] [Google Scholar]
- 37.Sailer I, Feher A, Filser F, Gauckler LJ, Luthy H, Hammerle CH. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont. 2007;20(4):383–8. [PubMed] [Google Scholar]
- 38.Tinschert J, Schulze KA, Natt G, Latzke P, Heussen N, Spiekermann H. Clinical behavior of zirconia-based fixed partial dentures made of DC-Zirkon: 3-year results. Int J Prosthodont. 2008;21(3):217–22. [PubMed] [Google Scholar]
- 39.Vult von Steyern P, Carlson P, Nilner K. All-ceramic fixed partial dentures designed according to the DC-Zirkon technique. A 2-year clinical study. J Oral Rehabil. 2005;32(3):180–7. doi: 10.1111/j.1365-2842.2004.01437.x. [DOI] [PubMed] [Google Scholar]
- 40.Mormann WH, Bindl A. The Cerec 3--a quantum leap for computer-aided restorations: initial clinical results. Quintessence Int. 2000;31(10):699–712. [PubMed] [Google Scholar]
- 41.Bornemann G, Lemelson S, Luthardt R. Innovative method for the analysis of the internal 3D fitting accuracy of Cerec-3 crowns. Int J Comput Dent. 2002;5(2-3):177–82. [PubMed] [Google Scholar]
- 42.Pfeiffer J. Dental CAD/CAM technologies: the optical impression (II) Int J Comput Dent. 1999;2(1):65–72. [PubMed] [Google Scholar]
- 43.Lin MT, Sy-Munoz J, Munoz CA, Goodacre CJ, Naylor WP. The effect of tooth preparation form on the fit of Procera copings. Int J Prosthodont. 1998;11(6):580–90. [PubMed] [Google Scholar]
- 44.Sulaiman F, Chai J, Jameson LM, Wozniak WT. A comparison of the marginal fit of In-Ceram, IPS Empress, and Procera crowns. Int J Prosthodont. 1997;10(5):478–84. [PubMed] [Google Scholar]