Abstract
Models of social phobia highlight the importance of anticipatory anxiety in the experience of fear during a social situation. Anticipatory anxiety has been shown to be highly correlated with performance anxiety for a variety of social situations. A few studies show that average ratings of anxiety during the anticipation and performance phases of a social situation decline following treatment. Evidence also suggests that the point of confrontation with the feared stimulus is the peak level of fear. No study to date has evaluated the pattern of anxious responding across the anticipation, confrontation, and performance phases before and after treatment, which is the focus of the current study. Socially phobic individuals (N=51) completed a behavioral avoidance task before and after two types of manualized cognitive behavioral therapy, and gave ratings of fear during the anticipation and performance phases. Results from latent growth curve analysis were the same for the two treatments and suggest that before treatment, anxiety sharply increased during the anticipation phase, was highly elevated at the confrontation, and, to a gradually increased during the performance phase. After treatment, anxiety increased during the anticipation phase, although at a much slower rate than at pretreatment, peaking at confrontation, and declined at the performance phase. The findings suggest that anticipatory experiences are critical to the experience of fear for public speaking and should be incorporated into exposures.
Keywords: Social Anxiety, Latent Growth Curve Modeling, Behavioral Avoidance Task
Anticipatory anxiety is theorized to be important in the maintenance of anxiety disorders, as it leads to avoidance of feared stimuli, which in turn prevents extinction and safety learning (Foa & Kozak, 1986; Otto, Smits, & Reese, 2005). Theoretical models of social phobia also highlight the role of anticipatory anxiety in the phenomenology of the disorder, such that anxiety is posited to rapidly increase in anticipation of a feared social situation and to remain at an elevated plateau for the duration of the encounter (Clark & Wells, 1995; Rapee & Heimberg, 1997). Experimental studies show a positive relation between anticipatory anxiety and performance anxiety using various formats, including self report measures, behavioral avoidance tasks (BATs), and neuroimaging (Brown & Stopa, 2007; Tillfors, Furmark, Marteinsdottir, & Fredrikson, 2002; Vassilopoulos, 2008). Despite evidence that increased anticipatory anxiety is associated with increased performance anxiety, there is very little research to date that examines continuous patterns of anxious responding across anticipatory and performance phases and how such patterns may change after treatment.
Such a question could be answered using a behavioral avoidance test (BAT). BATs are designed to replicate feared situations to allow for a more ecologically valid assessment of behaviors and cognitions during a target scenario (McNeil, Ries, & Turk, 1995). Indeed, BATs may be the most ecologically valid method of assessing social fears when the task successfully replicates a feared scenario (Becker & Heimberg, 1988; Bellack, 1983). Most studies utilizing BATs report either peak fear ratings for the entire task, or average ratings of anticipatory and performance anxiety, making it difficult to determine how anxiety fluctuates across these phases (Beidel, Rao, Scharfstein, Wong, & Alfano, 2010; Levin, Saoud, Strauman, & Gorman, 1993). Understanding patterns of anxious responding is important, given advances in the theory of extinction learning. Habituation, or a decrease in peak or overall anxious responding as a result of repeated confrontations with the feared stimulus, had long been discussed as a key mechanism for exposure therapy (Foa & Kozak, 1986). Consistent with this framework, the majority of prior research has examined changes in mean anxiety ratings. Recent research suggests that effective exposure therapy is characterized by safety learning - new learning that competes with old fear memories (Craske, et al., 2008). From this perspective, examining patterns of anxious responding is helpful, as it sheds light on the dynamic experience of approaching and confronting a feared stimulus.
Within social phobia, one study used multiple ratings to examine patterns of self-reported anxiety across the anticipation and performance phase of a BAT (Coles & Heimberg, 2000). Using cluster analysis, Coles and Heimberg identified 4 clusters of anxious responding. Three of the four clusters showed a similar pattern of increasing anxiety during the anticipatory phase that peaked and then plateaued during the performance phase. The highest ratings of anxiety were consistently obtained during the confrontation phase, the minute before and minute after encountering the feared stimulus (Behnke & Sawyer, 1999). A 4th cluster showed high levels of anxiety during the anticipatory phase that peaked during the confrontation phase and slightly decreased during the performance phase. These findings highlight the importance of the confrontation phase as the potential point of peak anxiety during a public speaking task. The findings also highlight the utility of examining patterns of anxious responding during an encounter with a feared stimulus, rather than focusing on average anxiety ratings.
Several studies show that anxiety during a BAT decreases following cognitive behavioral treatment for social phobia (Heimberg, Dodge, Hope, & Kennedy, 1990; Heimberg, et al., 1998; Rapee, Gaston, & Abbott, 2009). In the most recent study, a large clinical sample was randomized across 1) stress management, 2) cognitive restructuring with in vivo exposure, and 3) cognitive restructuring with in vivo exposure that was “enhanced” with additional strategies (Rapee, et al., 2009). Results suggested that the average level of state anxiety during an impromptu speech task decreased following each treatment, but declined most for the “enhanced” CBGT condition. Another large randomized clinical trial compared phenelzine, CBGT, pill placebo, and a psychoeducation control (Heimberg, et al. 1998). Average anxiety ratings for anticipatory and performance phases of an individualized BAT decreased for all groups. At posttreamement, there were no between-group differences in mean anxiety ratings during the anticipation phase. During the performance phase, average fear ratings were lowest in participants receiving phenelzine, and ratings for those receiving CBGT were lower than for those receiving psychoeducation or a pill placebo. However, both of these studies used aggregated measures of anxiety for the anticipatory and performance phases. Thus, it is unclear as to how treatment impacted patterns of anxious responding generally, and the confrontation phase specifically.
Only one study has reported multiple ratings of fear during the anticipation, confrontation, and performance phases of a BAT before and after treatment (Heimberg, et al., 1990). Participants with social phobia were randomly assigned to either CBGT or a credible psychoeducation control (ES). For both groups, results showed that relative to pretreatment, posttreatment ratings of fear were lower at each time point assessed. Between-group comparisons at posttreatment indicated that anxiety ratings were lower for CBGT at each time point. Furthermore, at posttreatment, CBGT patients’ anxiety remained relatively stable across the anticipation and confrontation phases, whereas ES patients’ ratings increased. However, these ratings were not fitted to a statistical model, and so it is unclear as to whether variation in anxiety across anticipation, confrontation, and performance phases changed following treatment. of the posttreatment BAT is meaingful.
Thus, no study to date has evaluated the pattern of anxiety across the anticipation, confrontation, and performance phases during a BAT before and after treatment. A better understanding of changes across these phases is relevant for the treatment process, because treatments for social phobia typically emphasize exposure to the performance phase of a social interaction (Heimberg, et al., 1990; Hofmann, 1999), and the confrontation phase has been shown to be the point of highest anxiety during the course of a social event (Coles & Heimberg, 2000; Heimberg, et al., 1990). \Thus, further research examining whether the pattern of anxious responding changes following treatment is needed. The current study used latent growth curve modeling to evaluate the pattern of anxiety during the anticipation, confrontation, and performance phases of a speech task before and after cognitive behavioral treatment within a sample of adults with social phobia who endorse a primary fear of public speaking. Based on prior literature, we hypothesize that at pretreatment, anxiety will increase during the anticipation phase, peak during the confrontation phase, and plateau during the performance phase of the BAT. Given the lack of prior literature, we make no hypotheses regarding the pattern of anxious responding following treatment, although it is predicted that participants will report lower ratings of anxiety during the BAT at posttreatment relative to pretreatment.
Methods
Participants
Participants were 51 individuals diagnosed with social phobia who reported public speaking as the primary social fear. They were recruited broadly through newspaper advertisements, posted flyers, and internet-based outlets. Inclusion criteria included speakers of English meeting DSM-IV (APA, 2000) criteria for a diagnosis of social phobia. Participants on psychoactive medication were required to be stabilized on their current medication(s) and dosage(s) for at least 3 months and were to remain at the same dosage throughout the course of the study. Individuals meeting any of the following criteria were excluded, (a) history of mania, schizophrenia, or other psychoses; (b) current suicidal ideation; (c) current alcohol or substance dependence; (d) inability to tolerate the virtual reality helmet; (e) history of seizures.
The majority of the participants did not have a comorbid diagnosis (n = 34, 67%). The sample was predominately female (57%, n = 29) with an average age of M = 41.02, SD = 12.44. Participants self-identified as “Caucasian” (n = 30), “African American” (n = 9), “Hispanic” (n = 3), or “Other” (n = 9). The sample was well educated, with 62% completing college and with 61% reporting their relationship status as married. Most participants (54%) reported an annual income of $50,000 or more.
Measures
Structured Clinical Interview for the DSM-IV (SCID: First, Gibbon, Spitzer, & Williams, 2002)
The SCID is a diagnostic interview used to assess psychological disorders based upon the criteria of the DSM-IV. For the current project, the SCID was used to obtain clinical diagnoses for participants. A licensed clinical psychologist viewed videotapes of the diagnostic interview from a randomly selected subset of the sample (n =15) and made independent ratings of the primary diagnosis. Interrater reliability among the licensed clinical psychologist and the interviewers for the primary diagnosis was perfect with κ = 1.00
Behavioral Avoidance Task
The BAT was based on a standardized speech assessment protocol (Beidel, Turner, Jacob, & Cooley, 1989). Participants blindly selected one of five note cards, which contained three relatively controversial or esoteric topics (e.g., abortion, religion in school, space exploration). Participants were asked to talk for ten minutes on one or more of the topics listed on the notecard. Participants were then given three minutes to prepare their speech. At the end of the preparation time, the interviewer introduced the participant to the audience and the speech began. Anxiety ratings were taken using the subjective units of distress scale (SUDs) at five points during the task: prior to giving instructions for the task (T1), after the instructions are presented (T2), after preparation for the speech (T3), the confrontation – immediately after introduction to the audience but before the speech began (T4), and a retrospective rating of peak anxiety during the speech (T5). During the pretreatment BAT, the audience consisted of one person - the interviewer conducting the pretreatment assessment. Participants were prompted to verbally provide SUDs ratings to the assessor for each time point. During the posttreatment assessment, the audience consisted of 2–3 audience members, who were blind to treatment condition. Audience members were instructed to not provide feedback to the participant during the course of the speech and to sit with neutral facial expressions. During each BAT, the speech was video recorded, with the equipment in full view of the participant. Participants were told that the video recording would be used during the course of treatment.
SUDs Ratings
Subjective units of distress (SUDs) ratings were used to assess fear on a 0 (no fear) to 10 (extreme fear) scale. Participants were oriented towards the SUDs scale prior to the task. The 10 point version of the SUDs scale has shown to be a valid measure of assessing distress in prior studies (Fairbank & Keane, 1982; Rowe & Craske, 1998; Turner, Beidel, & Jacob, 1994). Ratings were solicited and noted by an audience member/interviewer at 5 time points during the task, as noted above.
Procedure
Eligibility for the current study was assessed using a two part process that began with a telephone screen to determine if participants met obvious exclusion criteria (e.g., current treatment for social phobia). Candidates were then invited for an in person assessment during which the SCID was used to determine if the participant met inclusion criteria for a primary diagnosis of social phobia and to identify comorbid disorders.
Assessments
Following the completion of the pretreatment assessment, participants were randomized to one of the three groups: exposure group therapy (EGT; Hofmann, 2004), virtual reality exposure therapy (VRE; Anderson, Zimand, Hodges, & Rothbaum 2005), or a waiting list control (WL). At the posttreatment assessment, participants completed self-report measures and the BAT. (Participants were not allowed to talk on the same topics as the pretreatment BAT.)
Treatment
Treatment was administered by five study therapists; two senior therapists were licensed psychologists with prior experience implementing manualized cognitive behavior therapy, and three junior therapists were doctoral students. Each therapist administered both treatments. Prior to administering therapy, study therapists attended a two day intense training workshop led by the developers of the respective treatments.
Both treatments consisted of eight sessions of cognitive behavioral therapy designed to target several processes shown to maintain social phobia, including self-focused attention, negative perceptions of self and others, perceptions of lack emotional control, rumination, and realistic goal setting for social situations. The primary difference between the two therapies was the modality of exposure, delivered either in a group setting using other group members for exposure (EGT) or using virtual reality for exposure (VRE). Both treatments were administered according to a manualized protocol (Anderson, Zimand, Hodges, & Rothbaurn, 2005; Hofmann, 2004). The virtual reality (VR) scenarios included 1) a conference room (approximately 5 audience members), 2) a classroom (approximately 35 audience members), and 3) a large auditorium (approximately 100 audience members). These scenarios were presented via a head mounted display (HMD) that consisted of a helmet with headphones and goggles.
EGT was conducted in groups of 3–6 participants led by two therapists. Exposures primarily consisted of having participants give brief speeches in front of the group, with the group members providing feedback. Later sessions involved exposure utilizing social mishaps. The final session for both treatments discussed relapse prevention and reviewed what was learned during the course of therapy.
Ratings of adherence in delivering the protocols were provided by the developers of the respective treatments for a randomly selected subset of videotaped sessions (14%). Compliance was quite good for each treatment, with 92% and 93% of the essential elements of the protocol being completed for VRE and EGT, respectively; one infraction for each treatment arm across all sessions reviewed.
Data Analysis
Anxiety trajectories across the pretreatment and posttreatment BAT were assessed with separate latent growth curve models (LGC) using full information maximum likelihood estimation with the Mplus 5 program (Muthén & Muthén, 2007). Model fit was assessed using the recommendation of Hu and Bentler (1999) for smaller samples, such that adequate fit was demonstrated by a model with a nonsignificant chi-square, a comparative fit index (CFI) greater than 0.96, and a standardized root and a mean-squared residual (SRMR) of less than 0.07. An initial linear model was fitted to the data that included latent factors of intercept and slope with the five measurements during the speech serving as indicators. Paths from intercept to the indicators were set to one and paths from each indicator to the slope factor were initially set to 0, 1, 2, and 3 to estimate a linear growth model. Based on the fit of this model, adjustments were made to obtain the model that best approximated the data. Two sets of models were run for the pretreatment and posttreatment BAT. The first examined changes in anxiety during the anticipation and confrontation phases (T1 through T4). If good fit was obtained for the anticipation/confrontation model, a second model was run that included the retrospective rating of peak anxiety (T5) to determine how anxiety changed from confrontation to performance. Results from the initial linear models and the optimal fitting models are presented.
Results
Pretreatment BAT
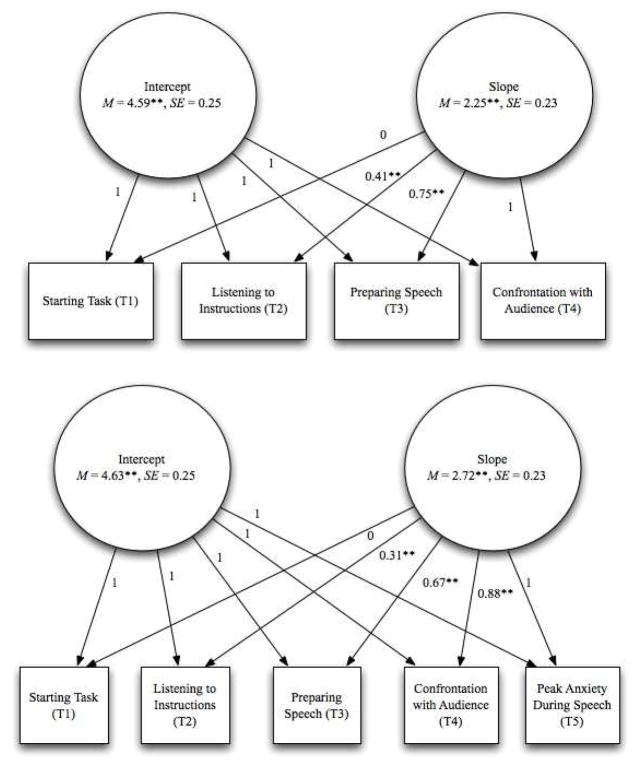
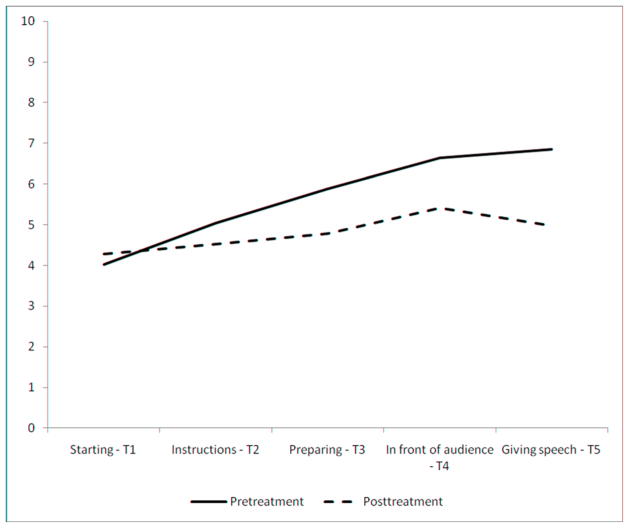
An initial linear growth curve model was fitted to the data to assess changes from the start of the task, T1, to the confrontation phase, T4. The model demonstrated poor fit, χ2 (8) = 15.32, p < 0.05; CFI = 0.93; RMSEA= 0.09, CI = 0.00 to 0.17; SRMR = 0.04. Several additional models were evaluated with a growth model that contained a latent slope demonstrating good fit, χ2 (6) = 10.51, p = 0.11; CFI = 0.99; RMSEA= 0.06, CI = 0.00 to 0.13; SRMR = 0.03 (Figure 1). This model included a latent intercept with all paths set to 1 and a latent rate of change in which paths were set as 0, λ, λ, 1 for T1 through T4 respectively. The paths for the latent slope indicated that fear increased throughout the course of the task from T1 (M = 4.02) to T4 (M = 6.64) (Figure 2).
Figure 1.
The upper model presents the best fitting growth curve for T1 to T4 of the pretreatment BAT. The lower model presents the best fitting growth curve for T1 to T5 of the pretreatment BAT. = p < 0.001.
Figure 2.
Change trajectory as predicted by latent linear and quadratic growth terms for BAT fear ratings at pretreatment and posttreatment
A follow up model was fitted to the data to assess how anxiety changed from confrontation with the audience to peak anxiety during the speech (T5). A latent growth model best fit the data, χ2 (11) = 16.48, p = 0.12; CFI = 0.96; RMSEA= 0.06, CI = 0.00 to 0.13; SRMR = 0.04. Across the entire task, 67% of the total change in fear occurred between T1 (M = 4.02) and T3 (M = 5.88), 21% between T3 and T4 (M = 6.64), and 12% between T4 and T5 (M = 6.85) (Figure 2). Although mean anxiety ratings increased at each time point, this model suggested that the rate of change in anxiety differed across the phases. The rate of change was highest during the anticipation phase, declining somewhat from the anticipation to the confrontation phase, and also from the confrontation (T4) to the peak level of anxiety during the speech (T5).
Posttreatment BAT
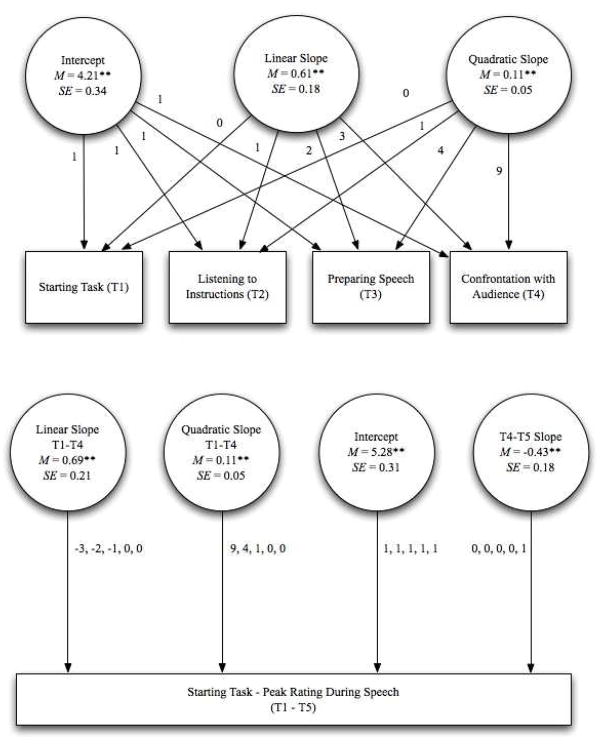
For posttreatment, a linear growth model was fitted to the data that included a latent factor for intercept and a latent factor for linear change from T1–T4. The model did not fit the data well: χ2 (8) = 15.31, p < 0.05; CFI = 0.94; RMSEA= 0.13, CI = 0.00 to 0.21; SRMR = 0.10. Several additional models were fitted with a quadratic growth model demonstrating the best fit T1–T4, χ2 (6) = 6.14, p = 0.41; CFI = 0.99; RMSEA= 0.02, CI = 0.00 to 0.18; SRMR = 0.05. This model suggested that the rate at which anxiety changed over the course of the task increased from the start of the task (T1) to the confrontation with the audience (T4) (Figure 2).
A second model that included the peak rating of anxiety during the course of the speech (T5) was fitted to the data. Several models were fitted to the data including latent quadratic, cubic, and quartic factors, with all yielding poor fit statistics. The group means suggested that anxiety increased from T1 (M = 4.28) to T4 (M = 5.42) and then decreased from T4 to T5 (M = 4.97). To address this directional change in slope, a spline or piecewise, model was used (Meredith & Tisak, 1990). A piecewise model allows for two different slopes to be estimated when the rate of change is expected to vary across two distinct periods. A piecewise latent growth model was fitted to the data that included the best fitting quadratic model for T1 – T4, and a slope for T4 – T5. Paths from the intercept to the indicators were set to one, paths from the linear slope for the first portion were initially set to −3, −2, −1, 0, 0, paths from the quadratic slope to the first portion were set to 9, 4, 1, 0. 0. and paths for the second portion were set to 0, 0, 0, 0, 1. The intercept represented the point in time when all slopes were 0, which corresponded to T4 in this model. This model demonstrated excellent fit with the data, χ2 (8) = 5.88, p = 0.41; CFI = 0.99; RMSEA = 0.02, CI = 0.00 to 0.13; SRMR = 0.04. These findings suggested that fear increased from T1 to T4 (linear slopeT1–T4 = 0.69, p < 0.01; quadratic slopeT1–T4 = 0.11, p < 0.05) but decreased from T4 to T5 (slopeT4–T5 = −0.43, p < 0.05) (Figure 3).
Figure 3.
The upper model presents the best fitting growth curve for T1 to T4 of the posttreatment BAT. The lower model presents the best fitting growth curve for T1 to T5 of the posttreatment BAT. For the lower model, the values next to each path represent the values of the paths corresponding to Times T1–T5. ** = p < 0.001.
An additional model was fitted in which treatment type, VRE & EGT, was included with paths predicting latent intercept, slope for T1 – T4, and slope for T4 – T5. This model significantly reduced fit, suggesting that the patterns of SUDs ratings did not differ across VRE and EGT.
Pretreatment and Posttreatment Comparison
Finally, a series of 2 × 2 (Time × Treatment Type) ANOVAs were conducted to compare changes from pretreatment to posttreatment for each of the five assessment points across the diagnostic categories (Table 1). A bonferroni correction was applied to these analyses to account for number of analyses that were conducted with a p < 0.01 being required for significance. Using this criterion, there were no significant Time × Treatment Type interactions across the time points suggesting that changes from pretreatment to posttreatment at each point did not vary across treatments. There was a main effect for time at T3 (F (1, 40) = 6.85, p < 0.01, η2 = 0.15) and T5 (F (1, 40) = 17.25, p < 0.01, η2 = 0.31), but no main effect of time for other time points. The length of the speeches in minutes was compared across pretreatment and posttreatment BATs with a repeated measures t-test. The results indicated that posttreatment BAT speeches were significantly longer (MPost = 7.01, SD = 2.76) than pretreatment BAT speeches (MPre = 4.75, SD = 2.78), t (50) = −2.58, p < 0.01, d = 0.51.
Table 1.
Pretreatment and Posttreatment SUDs ratings for Speech Task.
| Prior to Listening Instructions (T1) | Listening to Instructions (T2) | Preparing Speech (T3) | In front of audience (T4) | During Speech (T5) | ||
|---|---|---|---|---|---|---|
| Pretreatment | M | a4.02 | a5.04 | a5.88 | a6.64 | a6.85 |
| N = 51 | SD | 2.42 | 2.48 | 2.25 | 2.66 | 2.74 |
|
| ||||||
| Posttreatment | M | a4.28 | a4.53 | b4.79 | a5.42 | b4.97 |
| N = 51 | SD | 2.40 | 2.45 | 2.42 | 2.30 | 2.22 |
Subscripts indicate significant differences within each column at p < 0.01.
Discussion
The findings of the current study are consistent with theoretical descriptions of the manner in which anxiety changes in anticipation of and during a feared social situation for individuals diagnosed with social phobia (Clark & Wells, 1995; Rapee & Heimberg, 1997). Specifically, results showed that during a pretreatment BAT, anxiety sharply increased during the anticipation phase (88% change) and continued to increase during the performance phase, though less dramatically (12% change). This finding is consistent with previous research utilizing multiple ratings for a BAT across anticipation and performance phases (Coles & Heimberg, 2000; Heimberg, et al., 1990), and with imaging research that indicates increased brain and autonomic activity in anticipation of a speech (Davidson, Marshall, Tomarken, & Henriques, 2000). Results from the current study also show that a different pattern of anxiety ratings emerges following treatment. During the posttreatment BAT, anxiety increased during the anticipation phase, but decreased by a small, albeit significant, amount during the performance phase. The confrontation phase was shown to be the peak point of anxiety during the posttreatment BAT, but not during the pretreatment BAT.
Several significant methodological limitations deserve mention. The current study relied on a single item self report measure, SUDs ratings, to assess anxiety during the course of the task. Such measures are prone to increased measurement error. Furthermore, the current study used a single retrospective rating of fear for the duration of the 10-minute performance phase. Other studies using a BAT task included several ratings during the performance phase (Coles & Heimberg, 2000; Heimberg, et al., 1990). As such, the manner in which anxiety changed during the performance phase of the BAT could not be fully explored. Additional work is needed to more fully determine how anxiety changes during the performance phase. It is possible that anxiety has a single peak during or shortly after the confrontation phase. Alternatively, anxiety could have multiple peaks during the course of the speech.
Researchers are encouraged to replicate the findings of the current study using a multi method assessment approach (Brewer & Hunter, 1989). First, using a multi-item measure to assess state anxiety, such as the State Trait Anxiety Inventory-STATE (STAI; Spielberg, 1984) or State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA; Gros, Antony, Simms, & McCabe, 2007) would be an improvement over the single-item SUDS ratings used in the present study. In addition to self report measures, measures of physiological arousal, and behavioral observations should be used to obtain more accurate assessments of social anxiety during the course of the BAT. Such assessment tools should be used throughout the entire duration of the BAT so that multiple measures of anxiety are taken during the course of the anticipation phase. Care should be taken to preserve the ecological validity of the anticipation and confrontation phases by limiting the participant’s contact with the observers before the speech. Behavioral coders could observe the participant during the anticipation phase through a two way mirror or provide ratings based on a video recording. The use of a more comprehensive assessment battery would also allow for the use of a stronger analytic strategy in which a latent factor of social anxiety is created from the self report, physiological, and behavioral measures (Courvoisier, Nussbeck, Eid, Geiser, & Cole, 2008). The latent factors would then be included as the indicators of the slope and intercept for the growth curve model. This approach would allow for a more accurate portrayal of changes in social anxiety during the course of the BAT by substantially reducing measurement error.
The association between self-report, physiological, and behavioral measures of anxiety are of interest. Prior work has shown that behavioral and self report measures can have weak associations with physiological arousal in public speaking tasks (Westenberg, et al., 2009). These findings should be replicated with such measures to better understand physiological changes during the anticipation, confrontation, and performance phases.
Exposure treatments for social phobia typically emphasize anxiety during the performance portion of social interactions (Heimberg, et al., 1990; Hofmann, 1999). For example, participants are asked to engage in conversations, speak to an audience, or attend social functions (e.g. parties). The findings of the current study suggest that conducting exposure to target anticipatory anxiety and anxiety during confrontation may also be useful in order to prevent the escalation of anxiety and reduce the amount of anxiety experienced during the actual situation. Prior work examining the influence of anticipatory processing on social phobia symptoms during public speaking has advocated for similar approaches to be integrated into treatment packages (Hinrichsen & Clark, 2003). Although anxiety during the confrontation phase was lower at posttreatment than pretreatment, this difference was not significant. Providing additional exposures to the confrontation phase represents a potential method by which to further enhance social phobia treatments. VRE provides an excellent means for such an approach because of the ease with which the confrontation phase can be recreated.
Anticipatory processing also has been shown to be associated with post event processing, a ruminative component of social phobia (Mellings & Alden, 2000), which is also associated with poorer treatment response (Price & Anderson, 2011). As such, treatment for social phobia may benefit from expanding the focus of treatment to include both anticipatory and post event periods. Additional research using BATs may benefit from expanding the scope of the feared situation to include additional measurements from before and after these experiences. Viewing the BAT in such a manner could lead to a better understanding of how cognitive processes, anxiety, and physiological arousal interact with one another. The increased use of mobile applications in healthcare could provide an excellent means to obtain naturalistic cognitive, behavioral, and physiological ratings from before and after a social experience (Kazdin & Blase, 2011).
The full integration of anticipatory phases into exposure for social phobia presents a number of challenges to exposure therapists. First, the strength of associations for extinction learning have been shown to be highly dependent upon context (Bouton, Westbrook, Corcoran, & Maren, 2006). Anxiety that has been established in a novel anticipatory context may carry over into a performance context for which extinction has occurred. For example, a student may experience a significant amount of anxiety during a presentation in class despite having completed exposures for this event because she chose to prepare for the speech in the library (novel anticipatory context) as opposed to her dorm room (familiar anticipatory context). Therapists and patients should work together to identify salient contexts that the person is likely to encounter leading up to an event to allow for more comprehensive exposures. Technologies such as VRE and mobile devices may be helpful treatment modalities, as the therapist can access an anticipation phase across a variety of contexts, and (especially in the case of VRE) easily repeat such anticipatory contexts.
Safety behaviors are another interesting construct to consider across anticipatory and performance phases of encounters with feared stimuli. Safety behaviors are maladaptive coping strategies that are used to ineffectively reduce anxiety when encountering a feared stimulus (Wells, et al., 1996). This definition implies that safety behaviors occur during the performance phase (Salkovskis, 1991), and treatments have focused on minimizing them at this time (Otto, et al., 2005). The current study demonstrated that anxiety increased significantly during the anticipation phase for the event, and so research should begin to examine the role of safety behaviors during this period. It may be difficult to distinguish between safety behaviors and adaptive preparatory strategies in preparation for an event because “pep talks” or prespeech rituals are common. It is unknown whether these behaviors serve as a distraction from anticipatory anxiety during an exposure and thus undermine overall treatment response, or if they are adaptive in reducing the overall experience of anxiety. Future research is needed to identify safety behaviors that occur in anticipation of an event, the effect that these behaviors have on the experience of anxiety throughout the event, and the effect that these behaviors have on treatment response.
The results also indicated that fear during the preparation of the speech (T3) and during the speech (T5) were significantly lower at posttreatment as compared to pretreatment. The significant difference in ratings at the conclusion of the speech is consistent with prior work demonstrating that CBT is effective at reducing fear ratings during a BAT following treatment for social phobia (Heimberg, et al., 1990; Heimberg, et al., 1998; Rapee, et al., 2009). Whereas Heimberg et al. (1990) found significant decreases from pretreatment to posttreatment at every time point, the results of the current study show differences at only 2 time points. This may be due to a slightly smaller sample size in the current study. Another difference is that the Heimberg study used an individually tailored BAT, whereas the current study used a standardized speech task. Prior research recommends personalized stimulus situaions for BATs (Chiauzzi, Heimberg, Becker, & Gansler, 1985). Although the standardized speech task was sure to be personally relevant for each participant (as inclusion criteria required self-report of public speaking as a primary fear), the speech task itself was not personalized for each participant.
The current study had additional limitations. The overall sample size for the current study was relatively small for latent growth curve analyses. Future studies that use larger clinical samples with a control group should replicate the results to provide additional support for the current findings. Finally, the current study did not include a posttreatment BAT from a no treatment control condition. As such, the extent that differences in the observed pattern of anxiety ratings across pretreatment and posttreatment BATs were solely attributed to treatment cannot be determined. These findings should be replicated with a no treatment comparison condition at posttreatment to verify that the change in anxiety is due to treatment. Finally, the audience at the posttreatment BAT was larger (2–3 members) than it was at the pretreatment BAT (1 member). Future work should attempt to recreate the speech environment as accurately as possible for pretreatment and posttreatment speeches.
The current study focused exclusively on public speaking fears, and thus it is not known whether the pattern of anxious responding found in the current study is characteristic for other types of social situations. This line of inquiry is important because a recent review (Blöte, Kint, Miers, & Westenberg, 2009) questioned the utility of speech tasks for assessing social phobia symptoms, and suggested that public speaking anxiety may be a specific subtype of social phobia. Additional research is needed to determine how anxiety changes before and after treatment for other social situations.
Despite the limitations of the current study, the results provide the first empirical investigation of the manner in which anxiety changes during the anticipation, confrontation, and performance phases of a public speaking event before and after treatment for social phobia. Additional research is needed to better understand how the anticipation phase can be incorporated into exposure based interventions and how doing so will further the treatment process.
Research Highlights.
Fear increased during the anticipation phase and peaked during confrontation prior to treatment.
Feared remained at an elevated level during the speech prior to treatment.
Fear increased to a lesser extent during the anticipation after treatment.
Fear peaked during confrontation after treatment
Fear decreased during performance after treatment.
Acknowledgments
The research described in this paper was supported in part by grants to the first author from the American Psychological Association and Georgia State University and the NIMH R42 MH 60506-02 grant awarded to the second author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson PL, Zimand E, Hodges LF, Rothbaurn BO. Cognitive behavioral therapy for public-speaking anxiety using virtual reality for exposure. Depression and Anxiety. 2005;22:156–158. doi: 10.1002/da.20090. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and statistical manual of mental disorders. 4. American Psychiatric Publishing, Inc; 2000. Text Revision. [Google Scholar]
- Becker RE, Heimberg RG. Assessment of social skills. In: Bellack AS, Hersen M, editors. Behavioral assessment: A practical handbook. 3. Elmsford, NY US: Pergamon Press; 1988. pp. 365–395. [Google Scholar]
- Behnke RR, Sawyer CR. Milestones of anticipatory public speaking anxiety. Communication Education. 1999;48:165–172. [Google Scholar]
- Beidel DC, Rao PA, Scharfstein L, Wong N, Alfano CA. Social skills and social phobia: An investigation of DSM-IV subtypes. Behaviour Research and Therapy. 2010;48:992–1001. doi: 10.1016/j.brat.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidel DC, Turner SM, Jacob RG, Cooley MR. Assessment of social phobia: Reliability of an impromptu speech task. Journal of Anxiety Disorders. 1989;3:149–158. [Google Scholar]
- Bellack AS. Recurrent problems in the behavioral assessment of social skill. Behaviour Research and Therapy. 1983;21:29–41. [Google Scholar]
- Blöte AW, Kint MJW, Miers AC, Westenberg PM. The relation between public speaking anxiety and social anxiety: A review. Journal of Anxiety Disorders. 2009;23:305–313. doi: 10.1016/j.janxdis.2008.11.007. [DOI] [PubMed] [Google Scholar]
- Bouton M, Westbrook R, Corcoran K, Maren S. Contextual and temporal modulation of extinction: behavioral and biological mechanisms. Biological Psychiatry. 2006;60:352–360. doi: 10.1016/j.biopsych.2005.12.015. [DOI] [PubMed] [Google Scholar]
- Brewer J, Hunter A. Multimethod research: A synthesis of styles. Sage Publications, Inc; 1989. [Google Scholar]
- Brown M, Stopa L. Does anticipation help or hinder performance in a subsequent speech? Behavioural and Cognitive Psychotherapy. 2007;35:133–147. [Google Scholar]
- Chiauzzi E, Heimberg R, Becker R, Gansler D. Personalized versus standard role plays in the assessment of depressed patients’ social skill. Journal of Psychopathology and Behavioral Assessment. 1985;7:121–133. [Google Scholar]
- Clark DM, Wells A. A cognitive model of social phobia. In: Heimberg RG, Liebowitz MR, editors. Social phobia: Diagnosis, assessment, and treatment. Guilford Press; 1995. pp. 69–93. [Google Scholar]
- Coles ME, Heimberg RG. Patterns of anxious arousal during exposure to feared situations in individuals with social phobia. Behaviour Research and Therapy. 2000;38:405–424. doi: 10.1016/s0005-7967(99)00092-3. [DOI] [PubMed] [Google Scholar]
- Courvoisier DS, Nussbeck FW, Eid M, Geiser C, Cole DA. Analyzing the convergent and discriminant validity of states and traits: Development and applications of multimethod latent state-trait models. Psychological assessment. 2008;20:270. doi: 10.1037/a0012812. [DOI] [PubMed] [Google Scholar]
- Craske MG, Kircanski K, Zelikowsky M, Mystkowski J, Chowdhury N, Baker A. Optimizing inhibitory learning during exposure therapy. Behaviour Research and Therapy. 2008;46:5–27. doi: 10.1016/j.brat.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Marshall JR, Tomarken AJ, Henriques JB. While a phobic waits: Regional brain electrical and autonomic activity in social phobics during anticipation of public speaking. Biological Psychiatry. 2000;47:85–95. doi: 10.1016/s0006-3223(99)00222-x. [DOI] [PubMed] [Google Scholar]
- Fairbank JA, Keane TM. Flooding for combat-related stress disorders: Assessment of anxiety reduction across traumatic memories. Behavior Therapy. 1982;13:499–510. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. Structured clinical interview for the DSM-IV-TR axis 1 disorders. New York: Biometrics Research Department; 2002. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Gros DF, Antony MM, Simms LJ, McCabe RE. Psychometric properties of the State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA): Comparison to the State-Trait Anxiety Inventory (STAI) Psychological assessment. 2007;19:369. doi: 10.1037/1040-3590.19.4.369. [DOI] [PubMed] [Google Scholar]
- Heimberg RG, Dodge CS, Hope DA, Kennedy CR. Cognitive behavioral group treatment for social phobia: Comparison with a credible placebo control. Cognitive Therapy and Research. 1990;14:1–23. [Google Scholar]
- Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, Holt CS, Welkowitz LA, Juster HR, Campeas R, Bruch MA, Cloitre M, Fallon B, Klein DF. Cognitive behavioral group therapy vs phenelzine therapy for social phobia: 12-week outcome. Archives of General Psychiatry. 1998;55:1133–1141. doi: 10.1001/archpsyc.55.12.1133. [DOI] [PubMed] [Google Scholar]
- Hinrichsen H, Clark D. Anticipatory processing in social anxiety: two pilot studies. Journal of Behavior Therapy and Experimental Psychiatry. 2003;34:205–218. doi: 10.1016/S0005-7916(03)00050-8. [DOI] [PubMed] [Google Scholar]
- Hofmann SG. Unpublished treatment manual. Boston University; 1999. Behavior group therapy for social phobia. [Google Scholar]
- Hofmann SG. Cognitive Mediation of Treatment Change in Social Phobia. Journal of Consulting and Clinical Psychology. 2004;72:392–399. doi: 10.1037/0022-006X.72.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kazdin AE, Blase SL. Rebooting Psychotherapy Research and Practice to Reduce the Burden of Mental Illness. Perspectives on Psychological Science. 2011;6:21–37. doi: 10.1177/1745691610393527. [DOI] [PubMed] [Google Scholar]
- Levin AP, Saoud JB, Strauman T, Gorman JM. Responses of ‘generalized’ and ‘discrete’ social phobics during public speaking. Journal of Anxiety Disorders. 1993;7:207–221. [Google Scholar]
- McNeil DW, Ries BJ, Turk CL. Behavioral assessment: Self-report, physiology, and overt behavior. In: Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, editors. Social phobia: Diagnosis, assessment, and treatment. New York, NY US: Guilford Press; 1995. pp. 202–231. [Google Scholar]
- Mellings T, Alden LE. Cognitive processes in social anxiety: The effects of self-focus, rumination and anticipatory processing. Behaviour Research and Therapy. 2000;38:243–257. doi: 10.1016/s0005-7967(99)00040-6. [DOI] [PubMed] [Google Scholar]
- Meredith W, Tisak J. Latent curve analysis. Psychometrika. 1990;55:107–122. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 5. Los Angeles, CA: 2007. [Google Scholar]
- Otto MW, Smits JAJ, Reese HE. Combined Psychotherapy and Pharmacotherapy for Mood and Anxiety Disorders in Adults: Review and Analysis. Clinical Psychology: Science and Practice. 2005;12:72–86. [Google Scholar]
- Price M, Anderson PL. The impact of cognitive behavioral therapy on post event processing among those with social anxiety disorder. Behaviour Research and Therapy. 2011;49:132–137. doi: 10.1016/j.brat.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapee RM, Gaston JE, Abbott MJ. Testing the efficacy of theoretically derived improvements in the treatment of social phobia. Journal of Consulting and Clinical Psychology. 2009;77:317–327. doi: 10.1037/a0014800. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997;35:741–756. doi: 10.1016/s0005-7967(97)00022-3. [DOI] [PubMed] [Google Scholar]
- Rowe MK, Craske MG. Effects of varied-stimulus exposure training on fear reduction and return of fear. Behaviour Research and Therapy. 1998;36:719–734. doi: 10.1016/s0005-7967(97)10017-1. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM. The importance of behaviour in the maintenance of anxiety and panic: A cognitive account. Behavioural and Cognitive Psychotherapy. 1991;19:6–19. [Google Scholar]
- Spielberg C. State-Trait Anxiety Inventory: a comprehensive bibliography. 1984. State-trait anxiety inventory: a comprehensive bibliography. [Google Scholar]
- Tillfors M, Furmark T, Marteinsdottir I, Fredrikson M. Cerebral blood flow during anticipation of public speaking in social phobia: a PET study. Biological Psychiatry. 2002;52:1113–1119. doi: 10.1016/s0006-3223(02)01396-3. [DOI] [PubMed] [Google Scholar]
- Turner SM, Beidel DC, Jacob RG. Social phobia: A comparison of behavior therapy and atenolol. Journal of Consulting and Clinical Psychology. 1994;62:350. doi: 10.1037//0022-006x.62.2.350. [DOI] [PubMed] [Google Scholar]
- Vassilopoulos SP. Coping strategies and anticipatory processing in high and low socially anxious individuals. Journal of Anxiety Disorders. 2008;22:98–107. doi: 10.1016/j.janxdis.2007.01.010. [DOI] [PubMed] [Google Scholar]
- Wells A, Clark DM, Salkovskis P, Ludgate J, Hackmann A, Gelder M. Social phobia: The role of in-situation safety behaviors in maintaining anxiety and negative beliefs*. Behavior Therapy. 1996;26:153–161. doi: 10.1016/j.beth.2016.08.010. [DOI] [PubMed] [Google Scholar]
- Westenberg CL, Miers AC, Sumter SR, Kallen VL, van Pelt J, Blöte AW. A prepared speech in front of a pre-recorded audience: Subjective, physiological, and neuroendocrine responses to the Leiden Public Speaking Task. Biological Psychology. 2009;82:116–124. doi: 10.1016/j.biopsycho.2009.06.005. [DOI] [PubMed] [Google Scholar]