Abstract
Lower extremity amputation not only limits mobility, but also increases the risk of knee osteoarthritis of the intact limb. Dynamic walking models of non-amputees suggest that pushing-off from the trailing limb can reduce collision forces on the leading limb. These collision forces may determine the peak knee external adduction moment (EAM), which has been linked to the development of knee OA in the general population. We therefore hypothesized that greater prosthetic push-off would lead to reduced loading and knee EAM of the intact limb in unilateral transtibial amputees.
Seven unilateral transtibial amputees were studied during gait under three prosthetic foot conditions that were intended to vary push-off. Prosthetic foot-ankle push-off work, intact limb knee EAM and ground reaction impulses for both limbs during step-to-step transition were measured.
Overall, trailing limb prosthetic push-off work was negatively correlated with leading intact limb 1st peak knee EAM (slope = −0.72 +/− 0.22; p=0.011). Prosthetic push-off work and 1st peak intact knee EAM varied significantly with foot type. The prosthetic foot condition with the least push-off demonstrated the largest knee EAM, which was reduced by 26% with the prosthetic foot producing the most push-off. Trailing prosthetic limb push-off impulse was negatively correlated with leading intact limb loading impulse (slope = −0.34 +/− 0.14; p=.001), which may help explain how prosthetic limb push-off can affect intact limb loading.
Prosthetic feet that perform more prosthetic push-off appear to be associated with a reduction in 1st peak intact knee EAM, and their use could potentially reduce the risk and burden of knee osteoarthritis in this population.
Introduction
Approximately one million people in the United States are living with lower extremity amputation and this number is projected to more than double by the year 2050 1. Lower extremity amputation not only limits mobility, but also predisposes individuals to painful secondary impairments that can result in additive disability. Knee osteoarthritis (OA) of the intact limb is one such secondary impairment 2, 3. Intact limb knee pain in unilateral lower extremity amputees is reported to be twice as common 3, and the prevalence of symptomatic knee OA 17 times higher than in age-matched non-amputees 2. Imaging studies have also confirmed the increased prevalence of intact limb, knee degenerative changes when compared with control populations 4, 5. While transtibial amputees (TTAs) are more likely to develop knee pain in their intact limb, they are five times less likely to develop knee pain in their amputated limb than a control population 3. Since TTAs are known to load their intact limb to a greater extent than their prosthetic limb during gait 6, the marked asymmetry in knee pain and degeneration suggests that mechanical loading factors are likely an important contributor to the increased incidence in this population. It is possible that this loading asymmetry might be associated with specific mechanical characteristics of the prosthetic limb and therefore might be reduced by improving these characteristics.
Although mechanical loading factors have not been extensively studied in the amputee population, there is a foundation of literature that has demonstrated the importance of the peak knee external adduction moment (EAM) during walking on the development of knee joint degenerative changes in the general population 7–13. In particular, the first of the two EAM peaks during stance phase has been reported to be associated with increased knee OA severity 14. The factors that modify knee EAM in the intact limb of amputees have not been studied to date.
One potential explanation for increased mechanical loading in the intact limb is reduced prosthetic limb push-off power and ground reaction forces seen with conventional prosthetic feet 15. Dynamic walking models and experimental studies of non-amputees suggest that pushing off from the trailing limb can reduce the collision of the leading limb with the ground 16–20. During the transition from one stance leg to the next, the velocity of the body center of mass must change from a forward-and-down direction to a forward-and-up direction 16. This redirection is due to the ground reaction impulse (the integral of ground reaction forces) across the step-to-step transition period, roughly corresponding to double support 16 (Figure 1A). If the trailing prosthetic limb produces a reduced push-off, the leading intact limb must perform a greater share of the center of mass velocity redirection, thus increasing the ground reaction loading impulse on the leading limb. This is expected to result in greater loading of the intact limb, and hence greater knee EAM. Prosthetic feet that improve push-off could therefore potentially reduce intact limb loading, and specifically peak knee EAM during early stance.
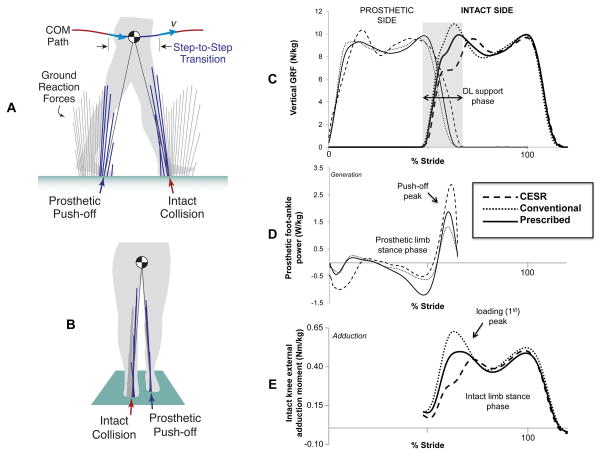
Figure 1.
Conceptual diagrams demonstrating the prosthetic and intact side ground reaction forces associated with the step-to-step transition (A, B) and graphic display of subject average vertical ground reaction force (C), prosthetic foot-ankle power (D), and intact knee external adduction moment (E), across the gait cycle for each prosthetic foot condition. (A) Sagittal view: the body center of mass (COM) is redirected during the step-to-step transition, as a result of forces applied by both legs against the ground (indicated by lines originating at center of pressure points throughout the gait cycle from a representative trial). (B) Coronal view: the ground reaction force is directed medial to the knee joint center of rotation essentially throughout stance phase leading to an external adduction moment. (C) Push-off and loading impulses were defined as the area under the vertical ground reaction force curves during double limb support. Prosthetic limb push-off impulse was negatively correlated with intact limb loading impulse. There was also a negative correlation between prosthetic foot-ankle push-off work (D) and intact limb 1st (loading) peak knee external adduction moment (E).
The goal of this study was to determine whether the amount of push-off from a prosthetic foot affects intact knee EAM during gait in unilateral TTAs. We studied three prosthetic foot conditions that we expected to be associated with varying amounts of prosthetic push-off. We hypothesized that greater prosthetic push-off would lead to reduced loading, and hence reduced knee EAM, during early stance phase of the intact limb.
Methods
We tested for differences in limb loading during gait in unilateral TTAs. We examined variations in prosthetic foot-ankle push-off work including those that occurred systematically due to the type of foot (by applying three different prosthetic foot conditions), as well as those that occurred spontaneously as a result of gait variability. We then tested whether increases in push-off work, whether systematic or spontaneous, was associated with reductions in intact limb loading and knee EAM.
In order to explore the potential mechanistic connection between these two clinically relevant variables, we also subdivided the relationship between prosthetic foot-ankle push-off work and intact knee EAM into the following three paired relationships: First, push-off impulse from the prosthetic limb should increase with prosthetic push-off work, because pushing off causes a change in COM velocity, which entails a change in both momentum and kinetic energy, and therefore involve both impulse and work 16, 21. Second, the intact limb loading impulse should decrease linearly with push-off impulse, because the two must sum to redirect the COM velocity by a relatively fixed amount dictated by the particular gait 21, which we assume to be relatively fixed within each trial. Third, the intact limb peak EAM is expected to increase in proportion to the loading impulse. This is because the ground reaction loading impulse is the integral sum of ground reaction forces during double support, and the ground reaction force is the primary determinant of the EAM (assuming a relatively fixed moment arm of the ground reaction force relative to the knee joint center). To assess this flow of logic, we tested for correlation for each of the expected relationships. The measurements consisted of kinematics and kinetics of overground walking, according to the procedures detailed below.
Subjects
Seven unilateral TTA subjects participated in the study. They were recruited through bulletin board advertisements and a local amputee clinic, and all signed informed consent prior to participation as approved by the Institutional Review Board. Inclusion criteria consisted of the following: being between the ages of 18 and 80; having used a prosthesis for at least two years and wearing the prosthesis at least eight hours per day; self-report of being at least a moderately active community ambulator; being able to walk without the use of upper extremity aids; not having a history of falls within the previous 6 months; being free from neurological deficits and underlying musculoskeletal disorders that might affect gait characteristics.
Experimental protocol and instrumentation
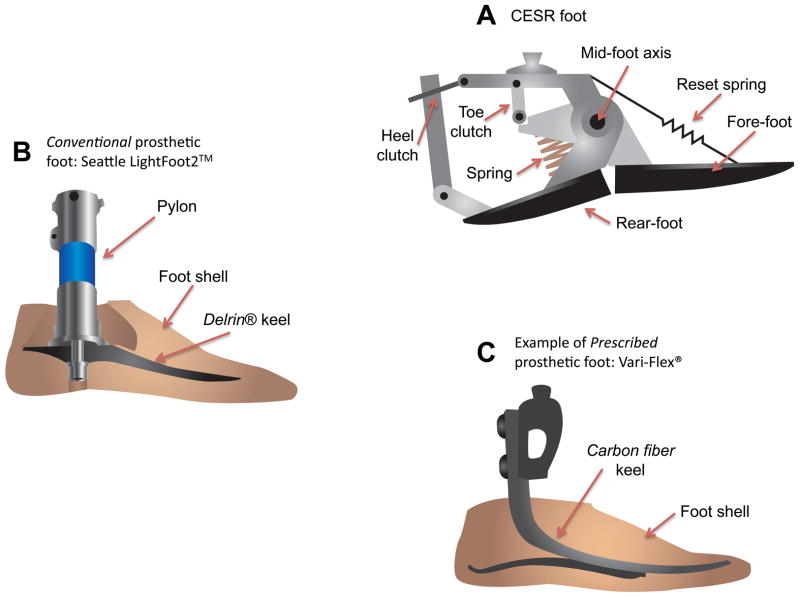
Subjects were tested under three prosthetic foot conditions in a randomized order in this within-subjects design: (1) the prototype Controlled Energy Storage and Return (CESR) prosthetic foot 22 (Figure 2A); (2) a conventional prosthetic foot (Conventional) (Figure 2B ); (3) the subject’s currently prescribed prosthetic foot (Prescribed) (Figure 2C). The CESR foot is an energy recycling foot that is designed to increase prosthetic ankle push-off as compared to conventional prosthetic feet. It is intended to store and capture energy in a spring at foot strike. This energy is stored until later in stance phase, when a latch opens, transferring the spring energy into plantarflexion push-off. The CESR foot has been shown to increase push-off impulse and to almost double peak positive prosthetic foot-ankle push-off power compared to a conventional prosthetic foot in non-amputees wearing a fixed-ankle simulator boot 22. The Conventional foot was a Seattle LightFoot2TM (Seattle Systems; Poulsbo, Washington) that has a Delrin keel with some elastic qualities. We included a Prescribed prosthetic foot condition in order to represent the prosthetic foot that was previously selected by a clinician with the goal of optimizing function for each individual subject.
Figure 2.
Schematic diagrams of the three prosthetic foot types used in the study. The Controlled energy storage and return (CESR) foot (A), the Conventional foot (B), and an example of a Prescribed foot (C).
Subjects were given an acclimation period on two different days, and returned on a third day for data collection. They practiced walking overground and on a treadmill using the conventional and prescribed feet for approximately 10 to 20 minutes and for approximately 45 minutes or until the patient felt comfortable with the CESR foot. Subjects were given additional acclimation time with the CESR foot due to its novel design and function. Data collection occurred on a separate day from the acclimation sessions to avoid the effects of fatigue. Prosthetic alignment was adjusted by the same experienced prosthetist for all conditions. All trials were at a walking speed of approximately 1.14 m/s, which is a typical walking speed for transtibial amputees 23, 24.
Data collection and processing
Kinematic and ground reaction force data were measured while subjects walked overground across force plates embedded along a 10-meter walkway. Gait kinematics were collected with a 12-camera motion capture system (Vicon, Centennial, CO) sampled at 120 Hz. Thirty-five 14 mm reflective markers were placed on each subject at locations consistent with a modified Vicon Plug-in-Gait full-body model. All prosthetic foot conditions included a prosthetic heel marker, a toe marker, and a marker at the distal end of the rigid shank, mirroring placement on the intact limb. Anthropometric measurements were taken for each individual according to the Vicon Plug-in-Gait requirements for static and dynamic modeling. Ground reaction forces were collected with 2 Bertec force plates (Columbus, OH) and 2 AMTI force plates (Watertown, MA) sampled at 1200 Hz.
A minimum of six successful overground trials was collected for each condition. Trials were defined as successful if they met the following two criteria: (1) walking speed was within the range of 1.14 ± 0.11 m/s as measured by a timing light system and (2) at least two sequential foot strikes occurred on separate force plates. All gait data were filtered with Vicon’s Woltring quintic spline algorithm with a mean-square-error value of 20, prior to computing 3D inverse dynamics using the Vicon Plug-In-Gait dynamic model, and subsequently using a low pass 25 Hz 3rd order Butterworth filter after the calculation of joint moments and powers.
Prosthetic limb push-off impulse and intact limb loading impulse were calculated by integrating the ground reaction force under the trailing prosthetic limb and the leading intact limb respectively, over the double support phase. Coronal knee moments (adduction and abduction moments) were calculated using a standard inverse dynamics approach, and the magnitude of the 1st and 2nd peaks of the intact knee EAM were quantified. Prosthetic foot-ankle power was calculated as the sum of translational and rotational power performed on the distal shank 25–27, where the former was defined as the dot product of the ground reaction force and translational velocity at the lateral malleolus ankle marker, and the latter as the dot product of the joint moment about the lateral malleolus and the angular velocity of the shank. This method captures the net behavior of the foot and does not assume a rigid-body model of the prosthesis with a fixed joint center of rotation as is necessary with standard inverse dynamics. Inverse dynamics may not accurately account for energy storage, dissipation and return28 in prosthetic feet which have a deformable foot-ankle segment rather than a fixed axis of rotation. Prosthetic foot-ankle push-off work was defined as the integral of positive power generated during the final phase of stance (approximately 50–60% of the gait cycle). All quantities were normalized to body mass.
Statistical Analysis
Paired associations were tested using linear mixed effects regression, applied across all of the steps recorded from each subject. The primary test was between trailing limb push-off work and leading limb knee EAM. Secondary tests were performed between prosthetic foot-ankle push-off work and push-off (trailing prosthetic limb) impulse, between push-off impulse and loading (intact leading limb) impulse, and between loading (intact leading limb) impulse and the same limb’s knee EAM. The first variable of each pair acted as the independent fixed effect, and the second as the dependent variable, with subject and subject by independent variable interactions as random effects. Results from these tests were summarized as slopes +/− standard errors.
The relationship between intact knee peak EAM and prosthetic foot condition was assessed using linear mixed effects regression. Peak intact knee EAM was the dependent variable, foot condition was the independent variable and subject and subject by foot condition were modeled as random effects. Overall significance (P<.05) across all foot conditions was assessed first, and if significant, pair-wise comparisons among the three foot conditions were then tested for significance using linear contrasts (P<.017, applying Bonferroni’s correction). The same procedure was used to determine the association between prosthetic peak foot-ankle power or push-off work and foot condition. All analyses were carried out using R 2.9.0 software (R Foundation for Statistical Computing, Vienna, Austria).
Results
Seven male unilateral transtibial amputee subjects (mean +/− SD age: 52.3 ± 12 yrs; Weight: 80.9 ± 9.9 kg; Height: 1.85 ± 0.05 m) were studied while walking overground. All subjects had a traumatic etiology of amputation. Table 1 describes the Prescribed prosthetic feet as well as the socket suspension type for each subject. All subjects wore patellar tendon-bearing design sockets and used a gel liner interface. All amputees had a dynamic elastic response type of Prescribed prosthetic foot.
Table 1.
Prescribed prosthetic foot and suspension mechanism for each subject.
| Prescribed prosthetic foot | Suspension mechanism | |
|---|---|---|
| Subject 1 | FS1000 (1) | pin lock |
| Subject 2 | Renegade (1) with rotator (4) | pin lock |
| Subject 3 | Ceterus (2) | suction |
| Subject 4 | Seattle Carbon LightFoot 2 (3) | pin lock |
| Subject 5 | Flex Foot (2) | pin lock |
| Subject 6 | Luxon Max (4) | pin lock |
| Subject 7 | Vari-flex (2) | pin lock |
Freedom Innovation Inc; Irvine, California;
Ossur, Reykjavik, Iceland;
Seattle Systems; Poulsbo, Washington;
Otto Bock, Duderstadt, Germany
Overall, there was a statistically significant negative correlation between trailing limb prosthetic foot-ankle push-off work and leading intact limb 1st peak knee EAM (slope = −0.72 +/− 0.22; P=.011). For the proposed subdivided relationships, there was a significant correlation between prosthetic foot-ankle push-off work and trailing prosthetic limb push-off impulse (slope = 0.88 +/− 0.18; P=.002); trailing limb push-off impulse was negatively correlated with leading intact limb loading impulse (Figure 1C) (slope = −0.34 +/− 0.14; P=.001); and there was a trend toward a correlation between leading limb impulse and 1st peak intact knee EAM (slope = 0.25 +/− 0.17; P=.14).
Prosthetic foot-ankle work and peak power varied significantly with foot type (Figure 1D). On average, the CESR foot performed 68% more push-off work than the Prescribed foot, and 137% more than the Conventional foot (Table 2).
Table 2.
Mean (SD) of peak prosthetic ankle power, prosthetic push-off work, and peak intact knee external adduction moment (EAM) by prosthetic foot condition.
| CESR | Conventional | Prescribed | P-value | |
|---|---|---|---|---|
| Peak prosthetic foot- ankle power (W/kg) | 3.20 (0.72) | 1.35 (0.31) | 1.90 (0.53) | .0004abc |
| Prosthetic push-off work (J/kg) | 0.27 (0.04) | 0.11 (0.03) | 0.15 (0.04) | <.0001abc |
| 1st Peak intact knee EAM (Nm/kg) | .451 (.144) | .608 (.169) | .509 (.132) | .015ab |
| 2nd Peak intact knee EAM (Nm/kg) | .483 (.158) | .497 (.143) | .466 (.146) | .054 |
Significant pairwise difference between CESR and Conventional (P<.017)
Significant pairwise difference between Prescribed and Conventional (P<.017)
Significant pairwise difference between CESR and Prescribed (p<.017)
Consistent with prior studies 7, 8, 14, the knee EAM throughout the stance phase has a typical two-peak shape similar to that seen in graphs of the vertical ground reaction force during walking 8. The 1st peak intact knee EAM varied significantly by prosthetic foot condition (Figure 1E). Specifically, both CESR and Prescribed showed a significantly reduced mean 1st peak knee EAM compared with Conventional (Table 2). First peak knee EAM in the CESR condition appeared less than that of the Prescribed condition on average, however this difference did not achieve statistical significance (P=.077). There were no significant differences in mean 2nd peak EAM across foot type.
Discussion
In this study we investigated the effects of three different prosthetic foot conditions on the intact knee EAM in unilateral transtibial amputees, a population with a high prevalence of knee OA. Our aim was to explore the effects of prosthetic foot-ankle push-off on the mechanical loading of the intact knee. In support of our hypothesis, we found that increased prosthetic foot-ankle push-off work was associated with a reduction in intact knee 1st peak EAM. Examining each prosthetic foot individually, the one with the largest magnitude push-off work, the CESR, was associated with the lowest intact knee 1st peak knee EAM. The foot with the least push-off work, the Conventional, was associated with the largest intact knee 1st peak knee EAM.
We propose the following potential chain of mechanisms to explain the association found between prosthetic foot-ankle push-off work and 1st peak intact knee EAM: Ankle push-off work constitutes the largest joint contribution to terminal stance push-off 29, and dynamic walking models demonstrate that the push-off impulse causes a change in COM velocity and hence kinetic energy, with the change in energy determining the amount of push-off work 21. We observed a positive correlation between push-off work and impulse. Similarly, models show that trailing limb push-off impulse can reduce leading limb loading impulse during the transition between one stance limb to the next 16–20; consistent with these models we found that trailing prosthetic limb push-off impulse was negatively correlated with leading intact limb loading impulse. Lastly we found a trend toward a relationship between leading limb loading impulse and leading limb 1st peak knee EAM. This is likely because the loading impulse is the integral of ground reaction forces that make up an important component of the knee EAM. Of course, correlation does not prove causation, and these proposed mechanisms deserve further study.
Peak knee EAM is an indicator of the knee joint loading that has been associated with knee OA 7–13. Knee OA affects the medial tibiofemoral compartment 10 times more commonly than the lateral compartment 30, and the ground reaction force vector falls medial to the knee for the majority of stance phase resulting in an EAM 31 (Figure 1B). In our study CESR reduced 1st peak intact knee EAM by 26% and Prescribed reduced the value by 16%, when compared to Conventional. Changes on the order of even 5–7% of peak knee EAM have been argued to be clinically significant in prior study assessing the effect of lateral wedge insoles on a population with knee OA 32.
The first peak in EAM is considered to be more important in association with the pathomechanics of knee OA14 due to being usually larger in magnitude7, 8, 14 and having a steeper rate of rise 33. If prosthetic foot-ankle push-off work affects contralateral knee loading, one would expect that effect to be seen at the 1st (loading) peak rather than at the 2nd peak. Consistent with this hypothesis, we found a significantly larger change in the 1st peak EAM by prosthetic foot condition. However, while the CESR foot provided significantly greater foot-ankle push-off than the Prescribed foot, the associated reduction in 1st peak intact knee EAM did not reach statistical significance. The lack of significance may be due to the less controlled nature of the Prescribed foot condition (which differed with each subject), or to the much greater accommodation time that subjects had with that foot. It may also suggest that other prosthetic design factors, for example foot length or timing of energy release, may be important as well. Future study is therefore warranted to explore these other prosthetic factors that may influence the mechanical loading conditions of the intact knee.
While commercially available dynamic elastic response prosthetic feet are unable to match intact ankle peak push-off power, the prototype CESR foot has been shown to restore push-off power to nearly normal values in non-amputee subjects walking with a fixed-ankle simulator boot 22. In the current investigation, TTA subjects demonstrated a greater than doubling of peak prosthetic foot-ankle push-off work for the CESR compared to Conventional condition, as well as greater push-off impulse. The Prescribed condition also demonstrated a significantly greater prosthetic foot-ankle push-off work relative to the Conventional, albeit a smaller increase than the CESR. This finding was expected given that all of the prosthetic feet in the Prescribed condition are commercially categorized as dynamic elastic response feet while the Seattle LightFoot2TM (Conventional) may have more limited energy return capabilities 34.
There are several potential limitations to this study, including a relatively small number of subjects. This could have led to type two error in not finding a statistically significant difference in 1st peak intact knee EAM between CESR and Prescribed foot conditions. However, the within-subjects design minimizes other potentially confounding variables to which a between-subjects design may be more prone. But it does not address the limited accommodation time of the CESR and Conventional prosthetic foot conditions.
While similar accommodation times have been used in prior study 22, there is no definitive literature to our knowledge examining the effect of various accommodation times when comparing different prosthetic feet. The Prescribed condition may therefore have had an advantage since these were the feet used by subjects prior to participation in the study. Although these limitations may affect the ability to detect the hypothesized effects, they appear not to reduce the overall relationship observed between prosthetic push-off work and intact knee EAM. Similarly, differences in other variables such as walking speed, double support duration, and COM displacement between foot conditions would be unlikely to affect the overall relationship we observed.
In conclusion, prosthetic foot characteristics have a significant effect on the intact knee EAM during gait in unilateral TTAs. Specifically, feet that perform more prosthetic foot-ankle push-off appear to be associated with a reduction in intact knee 1st peak EAM, and their use may therefore reduce the risk and burden of knee osteoarthritis in this population. Future study is warranted to explore other prosthetic foot factors that may also be contributing to this difference in intact knee loading conditions. Studying the effects of prosthetic foot design on the loading conditions associated with knee OA offers a clinically relevant prevention strategy to this common secondary disability in lower extremity amputees.
Acknowledgments
This work was supported by the U.S. Department of Veterans Affairs, Office of Research and Development Rehabilitation, R&D Program (Grants A4372R and A4843C). Additionally, Dr. Morgenroth’s work was supported by the Rehabilitation Medicine Scientist Training Program and the NIH (grant K12 HD001097). Statistical analyses were performed by Jane B. Shofer, MS. Prosthetic adjustments were performed by Wayne Biggs, CPO.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422–9. doi: 10.1016/j.apmr.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Struyf PA, van Heugten CM, Hitters MW, Smeets RJ. The prevalence of osteoarthritis of the intact hip and knee among traumatic leg amputees. Arch Phys Med Rehabil. 2009;90(3):440–6. doi: 10.1016/j.apmr.2008.08.220. [DOI] [PubMed] [Google Scholar]
- 3.Norvell DC, Czerniecki JM, Reiber GE, Maynard C, Pecoraro JA, Weiss NS. The prevalence of knee pain and symptomatic knee osteoarthritis among veteran traumatic amputees and nonamputees. Arch Phys Med Rehabil. 2005;86(3):487–93. doi: 10.1016/j.apmr.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 4.Lemaire ED, Fisher FR. Osteoarthritis and elderly amputee gait. Arch Phys Med Rehabil. 1994;75(10):1094–9. doi: 10.1016/0003-9993(94)90084-1. [DOI] [PubMed] [Google Scholar]
- 5.Hungerford D, Cockin J. Fate of the retained lower limb joints in second World War amputees. J Bone Joint Surg. 1975;57(1):111. [Google Scholar]
- 6.Gailey R, Allen K, Castles J, Kucharik J, Roeder M. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45(1):15–29. doi: 10.1682/jrrd.2006.11.0147. [DOI] [PubMed] [Google Scholar]
- 7.Baliunas AJ, Hurwitz DE, Ryals AB, Karrar A, Case JP, Block JA, et al. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage. 2002;10(7):573–9. doi: 10.1053/joca.2002.0797. [DOI] [PubMed] [Google Scholar]
- 8.Hurwitz DE, Ryals AB, Case JP, Block JA, Andriacchi TP. The knee adduction moment during gait in subjects with knee osteoarthritis is more closely correlated with static alignment than radiographic disease severity, toe out angle and pain. J Orthop Res. 2002;20(1):101–7. doi: 10.1016/S0736-0266(01)00081-X. [DOI] [PubMed] [Google Scholar]
- 9.Hurwitz DE, Sumner DR, Andriacchi TP, Sugar DA. Dynamic knee loads during gait predict proximal tibial bone distribution. J Biomech. 1998;31(5):423–30. doi: 10.1016/s0021-9290(98)00028-1. [DOI] [PubMed] [Google Scholar]
- 10.Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9(1):113–9. doi: 10.1002/jor.1100090114. [DOI] [PubMed] [Google Scholar]
- 11.Sharma L, Hurwitz DE, Thonar EJ, Sum JA, Lenz ME, Dunlop DD, et al. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 1998;41(7):1233–40. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 12.Wada M, Maezawa Y, Baba H, Shimada S, Sasaki S, Nose Y. Relationships among bone mineral densities, static alignment and dynamic load in patients with medial compartment knee osteoarthritis. Rheumatology (Oxford) 2001;40(5):499–505. doi: 10.1093/rheumatology/40.5.499. [DOI] [PubMed] [Google Scholar]
- 13.Foroughi N, Smith R, Vanwanseele B. The association of external knee adduction moment with biomechanical variables in osteoarthritis: a systematic review. Knee. 2009;16(5):303–9. doi: 10.1016/j.knee.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Mundermann A, Dyrby CO, Andriacchi TP. Secondary gait changes in patients with medial compartment knee osteoarthritis: increased load at the ankle, knee, and hip during walking. Arthritis Rheum. 2005;52(9):2835–44. doi: 10.1002/art.21262. [DOI] [PubMed] [Google Scholar]
- 15.Winter DA, Sienko SE. Biomechanics of below-knee amputee gait. J Biomech. 1988;21(5):361–7. doi: 10.1016/0021-9290(88)90142-x. [DOI] [PubMed] [Google Scholar]
- 16.Adamczyk PG, Kuo AD. Redirection of center-of-mass velocity during the step-to-step transition of human walking. J Exp Biol. 2009;212(Pt 16):2668–78. doi: 10.1242/jeb.027581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donelan JM, Kram R, Kuo AD. Mechanical work for step-to-step transitions is a major determinant of the metabolic cost of human walking. J Exp Biol. 2002;205(Pt 23):3717–27. doi: 10.1242/jeb.205.23.3717. [DOI] [PubMed] [Google Scholar]
- 18.Donelan JM, Kram R, Kuo AD. Simultaneous positive and negative external mechanical work in human walking. J Biomech. 2002;35(1):117–24. doi: 10.1016/s0021-9290(01)00169-5. [DOI] [PubMed] [Google Scholar]
- 19.Kuo AD. The six determinants of gait and the inverted pendulum analogy: A dynamic walking perspective. Hum Mov Sci. 2007;26(4):617–56. doi: 10.1016/j.humov.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Kuo AD, Donelan JM, Ruina A. Energetic consequences of walking like an inverted pendulum: step-to-step transitions. Exerc Sport Sci Rev. 2005;33(2):88–97. doi: 10.1097/00003677-200504000-00006. [DOI] [PubMed] [Google Scholar]
- 21.Kuo AD. Energetics of actively powered locomotion using the simplest walking model. J Biomech Eng. 2002;124(1):113–20. doi: 10.1115/1.1427703. [DOI] [PubMed] [Google Scholar]
- 22.Collins SH, Kuo AD. Recycling energy to restore impaired ankle function during human walking. PLoS One. 5(2):e9307. doi: 10.1371/journal.pone.0009307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torburn L, Perry J, Ayyappa E, Shanfield SL. Below-knee amputee gait with dynamic elastic response prosthetic feet: a pilot study. J Rehabil Res Dev. 1990;27(4):369–84. doi: 10.1682/jrrd.1990.10.0369. [DOI] [PubMed] [Google Scholar]
- 24.Robinson JL, Smidt GL, Arora JS. Accelerographic, temporal, and distance gait factors in below-knee amputees. Phys Ther. 1977;57(8):898–904. doi: 10.1093/ptj/57.8.898. [DOI] [PubMed] [Google Scholar]
- 25.Prince FWD, Sjonnesen G, Wheeldon RK. A new technique for the calculation of the energy stored, dissipated, and recovered in different ankle-foot prostheses. IEEE T Rehabil Eng. 1994;2:247–55. [Google Scholar]
- 26.Robertson DG, Winter DA. Mechanical energy generation, absorption and transfer amongst segments during walking. J Biomech. 1980;13(10):845–54. doi: 10.1016/0021-9290(80)90172-4. [DOI] [PubMed] [Google Scholar]
- 27.Caldwell GE, Forrester LW. Estimates of mechanical work and energy transfers: demonstration of a rigid body power model of the recovery leg in gait. Med Sci Sports Exerc. 1992;24(12):1396–412. [PubMed] [Google Scholar]
- 28.Geil MD, Parnianpour M, Quesada P, Berme N, Simon S. Comparison of methods for the calculation of energy storage and return in a dynamic elastic response prosthesis. J Biomech. 2000;33(12):1745–50. doi: 10.1016/s0021-9290(00)00102-0. [DOI] [PubMed] [Google Scholar]
- 29.Winter D. The Biomechanics and Motor Control of Human Gait: Normal, Elderly and Pathologic. Waterloo: Waterloo Biomechanics; 1991. [Google Scholar]
- 30.Ahlback S. Acta Radiol Diagn (Stockh) Suppl 277. 1968. Osteoarthrosis of the knee. A radiographic investigation; pp. 7–72. [PubMed] [Google Scholar]
- 31.Andriacchi TP. Dynamics of knee malalignment. Orthop Clin North Am. 1994;25(3):395–403. [PubMed] [Google Scholar]
- 32.Kerrigan DC, Lelas JL, Goggins J, Merriman GJ, Kaplan RJ, Felson DT. Effectiveness of a lateral-wedge insole on knee varus torque in patients with knee osteoarthritis. Arch Phys Med Rehabil. 2002;83(7):889–93. doi: 10.1053/apmr.2002.33225. [DOI] [PubMed] [Google Scholar]
- 33.Lloyd CH, Stanhope SJ, Davis IS, Royer TD. Strength asymmetry and osteoarthritis risk factors in unilateral trans-tibial, amputee gait. Gait Posture. 2010;32(3):296–300. doi: 10.1016/j.gaitpost.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Gitter A, Czerniecki JM, DeGroot DM. Biomechanical analysis of the influence of prosthetic feet on below-knee amputee walking. Am J Phys Med Rehabil. 1991;70(3):142–8. doi: 10.1097/00002060-199106000-00006. [DOI] [PubMed] [Google Scholar]