Abstract
Background
N-acetylcysteine (NAC), an antidote for acetaminophen poisoning, might benefit patients with non-acetaminophen related acute liver failure.
Methods
In a prospective, double-blind trial, acute liver failure patients without clinical or historical evidence of acetaminophen overdose were stratified by site and coma grade and randomly assigned to groups that were given NAC or placebo (dextrose) infusion for 72 hours. The primary outcome was overall survival at 3 weeks. Secondary outcomes included transplant-free survival and rate of transplantation.
Results
A total of 173 patients received NAC (n=81) or placebo (n=92). Overall survival at 3 weeks was 70% for patients given NAC and 66% for patients given placebo (one-sided p=0.283). Transplant-free survival was significantly better for NAC patients (40%) than for those given placebo (27%; one-sided p=0.043). The benefits of transplant-free survival appeared to be confined to the 114 patients with coma grade I–II who received NAC (52% compared with 30% for placebo; one-sided p=0.010); transplant-free survival for the 59 patients with coma grade III–IV was 9% in those given NAC and 22% in those given placebo (one-sided p=0.912). The transplantation rate was lower in the NAC group but not significantly different between groups (32% vs. 45%; p=0.093). Intravenous NAC was generally well tolerated; only nausea and vomiting occurred significantly more frequently in the NAC group (14% vs. 4%; p=0.031).
Conclusions
Intravenous NAC improves transplant-free survival in patients with early stage non-acetaminophen related acute liver failure. Patients with advanced coma grades do not benefit from NAC and typically require emergency liver transplantation. (ClinicalTrials.gov number NCT00004467)
Acute liver failure is a relatively rare syndrome associated with a high mortality and frequent need for liver transplantation. Since the 1950s, trials of therapies to limit further damage or improve hepatic regeneration have failed to show evidence of benefit.1–6 In recent years, acetaminophen poisoning, either intentional or unintentional, has become the most common etiology of acute liver failure identified both in Europe and in the United States.7 When given within the first 24 hours after ingestion, N-acetylcysteine (NAC) can effectively prevent or minimize liver damage due to acetaminophen, even after massive overdoses,.8–10
Treatment with NAC may benefit patients with other forms of acute liver failure,11 either by improving systemic hemodynamics, tissue oxygen delivery,12–16 or via other favorable effects on the acutely injured liver.17,18 No clinical trials using NAC for patients with non-acetaminophen acute liver failure have been performed.19 In 1998, the Acute Liver Failure Study Group, funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health (NIH), began a registry at 24 participating sites around the United States to better characterize and understand mechanisms of acute liver failure. A prospective, randomized, double blind placebo controlled trial of NAC for cases of acute liver failure not due to acetaminophen was initiated in late 1998, ending in 2006. This paper summarizes the outcomes of this trial.
METHODS
Objective
The primary outcome measure for this trial was the overall number of patients surviving at 3 weeks following study admission; our research hypothesis was that patients receiving NAC would have a significantly higher overall survival than those receiving the placebo. The secondary outcome measures were the number of patients surviving without transplantation and the number of patients undergoing transplantation at three weeks following study admission. Our research hypothesis for transplant-free survival was that patients receiving NAC would demonstrate higher rates of transplant-free survival. The research hypothesis for transplantation did not specify a direction. Because of the extensive experience with NAC for acetaminophen-related liver failure, our original protocol specified the use of one-sided tests for overall survival and transplant-free survival, since it seemed very unlikely that NAC would harm patients in this setting.
Study Population
Detailed prospective data as well as serum, tissue and DNA were collected on all cases of acute liver failure meeting study criteria beginning in January 1998. Eligibility for the registry included age 18 years old or greater, evidence of acute liver failure (any degree of encephalopathy and coagulopathy: international normalized ratio [INR] ≥1.5) due to an illness of less than 24 weeks duration. Medical histories, clinical and laboratory findings were recorded on case report forms through death, transplantation or three weeks following study admission and at long-term follow-up visits one and two years following study entry.
Eligibility requirements were the same for both the NAC trial and registry with the following exceptions. Patients were excluded from the NAC trial for known or suspected acetaminophen overdose, if they had previously received NAC or if they were determined to have hepatic ischemia (shock liver), liver failure due to pregnancy or cancer. Patients with refractory hypotension, septic shock, and those expected to undergo transplantation imminently (i.e., in less than 8 hours), or those >70 years old were also excluded. Since all participants were, by definition, encephalopathic, informed consent was obtained from next of kin. The study was approved by the institutional review boards at all participating centers.
Study Design
Randomization was stratified by the standard hepatic encephalopathy (coma) categories (I–II versus III–IV),20 and by site with a blocking factor of 4. The site pharmacist received the randomization list prepared by the biostatistician (JSR); all study personnel (except the two biostatisticians, LSH and JSR) remained blinded throughout the study. After consent was obtained, patients were weighed and coma grade was determined so that the site pharmacist could randomize the patient and prepare the medication.
Response to treatment was carefully recorded, including vital signs, progression of coma grade and use of other supportive measures such as mannitol, need for intubation, rise in intracranial pressure in patients with an intra-cranial monitor inserted, and assessment of adverse events. All other aspects of care conformed to standard of care at each study site, all of which were liver transplant centers during the study except for one site, which had ready transplantation access nearby.
Study Medication
Following randomization, infusion of either 5% dextrose (placebo) or 5% dextrose with N-acetylcysteine (Acetadote®, Cumberland Pharmaceuticals, Nashville, TN) was begun, with an initial loading dose of 150 mg/kg/hr of NAC over one hour, followed by 12.5 mg/kg/hour for 4 hours, then continuous infusions of 6.25 mg/kg NAC for the remaining 67 hours.
Study Outcomes
The primary outcome of the trial was overall survival at three weeks after randomization. To obtain long-term outcomes, we used information gathered by the sites, in addition to the original study data set, censored 365 days after study admission. Secondary outcomes specified in the protocol were transplant-free survival and transplant rate. Two additional secondary outcomes also listed in the original protocol were length of hospital stay and a composite of the number of organ systems failing, utilizing specific definitions for hepatic encephalopathy, evidence for cerebral edema, use of vasopressor or ventilatory support, serum creatinine level (≥300 μM/L) or bacteremia. Data were reviewed twice yearly by a Data and Safety Monitoring Board and three interim analyses were performed, after 57, 113 and 170 patients had been enrolled.
Sample Size
Based on our own pre-study data, overall survival for non-acetaminophen related ALF in the United States at the start of the trial was estimated at 57%.1 Assuming overall survival (combining transplant-free plus transplanted and alive) of 57% (25%+32%) in the placebo arm and a predicted improvement in overall survival to 75% in the treated arm (45%+30%), 170 patients were targeted for enrollment to achieve 80% power (likelihood of rejecting the hypothesis of equal response rates) with a one-sided test of proportions at the 0.05 significance level.
Statistical analyses were based on the intention-to-treat principle and involved all randomized patients except for nine who represented protocol violations (see below).
Statistical Analysis
Univariate analyses were performed for patient demographic and illness characteristics at baseline for descriptive purposes and to determine their possible influences on the primary and secondary outcomes using χ2 or Fisher’s Exact test, and independent group Student’s t-test or Mann-Whitney U test as indicated. Additional analyses were performed on the baseline measures to separately compare the entire consented group, the placebo group and the group of eligible patients who were not consented.
The primary outcome, patients who survived (with or without transplant) versus those who died, and two of the secondary outcomes, patients (a) who survived without transplantation versus those dead or transplanted and (b) those transplanted versus not transplanted, were compared for the two treatment groups using χ2 analysis, Breslow-Day homogeneity of odds ratio test and the Mantel-Hanszel Common Odds Ratio tests. Results are presented using percentages and 95 percent confidence intervals (95% CI). As stated in the protocol, both overall survival and transplant-free survival were one-sided tests with the research hypothesis stated as the NAC group is expected to have higher or equal proportions of survival and transplant-free survival than the placebo group.
Three separate Kaplan-Meier models were developed for the primary/secondary measures censored at one year testing for group differences using the log rank test. A single measure was defined to combine treatment group and coma category into one variable: NAC I–II, NAC III–IV, placebo I–II, and placebo III–IV.
The statistical packages used to analyze the data were SPSS V16 and SAS V 9.1. Assumptions of all statistical tests were examined (normality, homogeneity of variance, etc.); since most variables were non-normally distributed, non-parametric analyses were used to analyze the data. Unless otherwise noted, all statistical tests were two-sided and p < 0.05 was considered significant. No corrections to the p-values were made for multiple comparisons.
RESULTS
Study Population
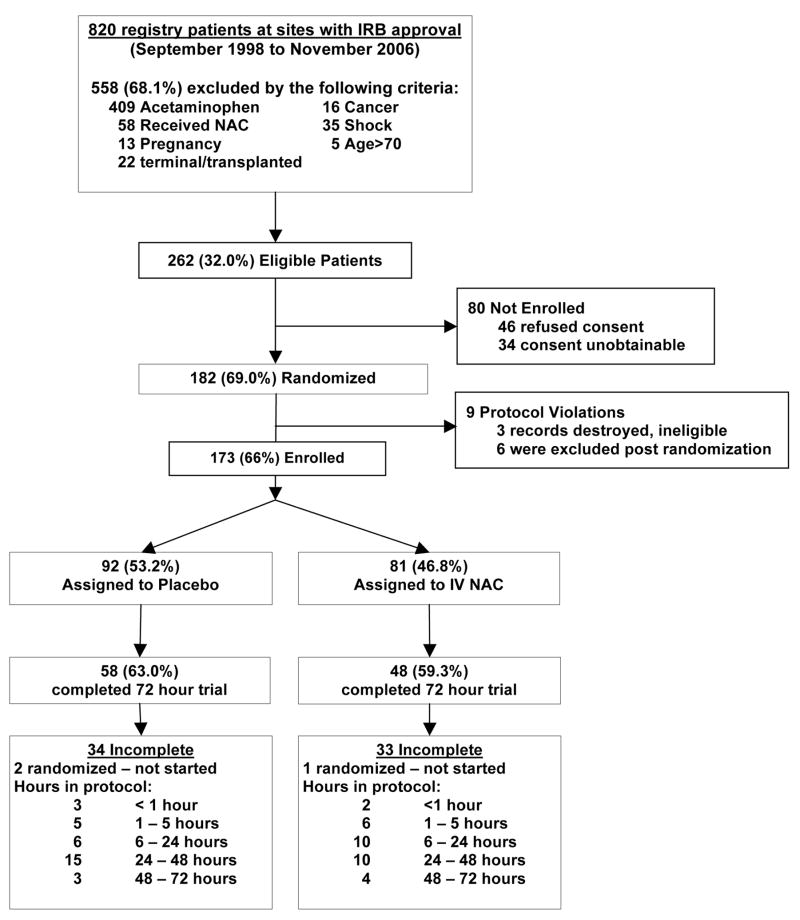
Among 820 eligible patients at sites with IRB approval, 558 (68%) met exclusion criteria (Figure 1). Of the remaining 262 patients, 89 were excluded either because consent was refused (46), was unobtainable (34) or, after randomization, because of protocol violations (9). The 9 protocol violations included inadvertent enrollment of two prisoners who were removed from consideration once their status was recognized, one patient for whom all hospital records were lost, 4 who met exclusion criteria but were mistakenly offered participation in the study, one patient who underwent transplantation before the first dose of NAC was administered and one patient who was withdrawn because the trial solution turned pink in the intravenous bottle. This harmless dye reaction was considered by the site investigator at the time as evidence of possible bacterial contamination; the patient was withdrawn and given open label medication. Data on the first 3 protocol violations were not available. For the latter group, 2 of the 6 were slated to, or did, receive NAC.
Figure 1.
Study design. A total of 820 patients were screened, leading to 173 patients enrolled in the final study.
Thus, 173 patients comprised the final study group (Table 1), 92 randomized to receive placebo and 81 to receive NAC. The imbalance in size of study groups was related to the randomization process whereby patients were stratified by site and coma grade (I–II vs. III–IV); not all sites reached a balance point on the randomization lists. During the course of the trial, the project biostatisticians verified the accurate use of the randomization scheme with the site pharmacist before each DSMB meeting. The majority of patients enrolled comprised four etiologies: drug-induced liver injury (DILI, n=45), autoimmune hepatitis (AIH, n=26), hepatitis B (HBV, n=37) and indeterminate (n=41). Patient numbers were reasonably well balanced between the placebo and treatment group within each etiology. The characteristics of the patients in the two groups were similar at enrollment (Table 1), except that the placebo group had longer median duration between jaundice and encephalopathy than the treated group (12 vs. 7 days, p=0.026) and a higher percentage of females (p=0.004). The 80 unconsented patients did not differ from the enrolled group (n=173) or the placebo group (n=92), except for lower median alanine aminotransferase (ALT) values than either comparison group (both p < 0.001, results not shown). Patients were enrolled at 22 sites over the period of the study, with 12 sites enrolling 8 or more patients (overall range 1–19). Five sites enrolled ≤3 patients.
Table 1.
Baseline characteristics at enrollment by treatment group.
| Placebo | NAC | χ2 | |||||
|---|---|---|---|---|---|---|---|
| Categorical variables | % of n=92 | 95% CI | % of n=81 | 95% CI | p-value | ||
| Gender (female) | 68% | 58% – 79% | 47% | 35% – 58% | 0.004 | ||
| Race (Caucasian) | 55% | 45% – 66% | 56% | 44% – 67% | 0.987 | ||
| Admit coma grade I–II | 62% | 51% – 72% | 73% | 63% – 83% | 0.129 | ||
|
| |||||||
| Continuous variables | N | Median | Range | N | Median | Range | Mann-Whitney p-value |
|
| |||||||
| Age (years) | 92 | 40.5 | 18 – 71 | 81 | 42 | 17 – 69 | 0.682 |
| Weight (kg) | 92 | 74.4 | 45 – 138 | 81 | 81 | 38 – 178 | 0.066 |
| Symptom to Coma (days) | 91 | 17 | 0 – 69 | 80 | 15 | 0 – 117 | 0.346 |
| Jaundice to Coma (days) | 86 | 12 | 0 – 65 | 75 | 7 | 0 – 153 | 0.026 |
| Bilirubin (mg/dL) | 92 | 20.3 | 0.7 – 62.4 | 81 | 22.3 | 0.7 – 51.5 | 0.645 |
| Creatinine (mg/dL) | 92 | 1.0 | 0.5 – 9.5 | 81 | 1.3 | 0.2 – 6.6 | 0.341 |
| INR | 92 | 2.9 | 1.1 – 14 | 81 | 2.4 | 1.4 – 20.1 | 0.258 |
| ALT (IU/L) | 90 | 756.5 | 31 – 13100 | 79 | 999 | 13 – 10153 | 0.304 |
| MELD | 92 | 33 | 19 – 49 | 81 | 32 | 12 – 57 | 0.673 |
No differences were observed between the two groups except in the time from jaundice to coma and in gender.
Overall, 58 (63%) in the placebo and 48 (59%) in the NAC arm completed 72 hours of therapy (Figure 1), and the majority (138/173, 80%) of patients received at least 24 hours of treatment. Reasons for early discontinuation included death or withdrawal of support (n=17), transplantation (n=36) or side effects possibly due to the drug (5 total, 4 thought to be due to NAC).
Study outcomes
Overall survival at 3 weeks was 70% (95% CI=60%, 81%, n=81) for NAC and 66% (95% CI=56%, 77%, n=92) for placebo (one-sided p=0.283; Table 2). However, transplant-free survival was significantly higher at 40% (95% CI=28%, 51%, n=81) in the treatment group as compared to 27% for placebo (95% CI=18%, 37%, n=92, one-sided p=0.043). When examining transplant-free survival by coma category at randomization (I–II vs. III–IV), the largest difference was observed in patients with coma grade I–II: 52% (95% CI=38%, 65%, n=58) survived in the NAC group as compared to 30% (95% CI=17%, 43%, n=56) in the placebo group (one-sided p=0.010). This was not the case for coma III–IV patients where transplant-free survival was only 9% (95% CI=0%, 22%, n=23) with NAC vs. 22% (95% CI=7%, 37%, n=36) with placebo (one-sided p=0.912). The odds ratios comparing the treatment groups for transplant-free survival were 2.46 (95% CI= 1.14, 5.30) for coma category I–II and 0.33 (95% CI=0.06, 1.74) for coma category III–IV; that is, patients in coma category I–II receiving NAC were 2.46 times more likely to survive than those in the placebo group, while those with advanced coma (III–IV) receiving NAC were only 0.33 (95% CI=0.06, 1.74) times as likely to survive as those in the placebo group (Breslow-Day χ2 (1)=5.11, p=0.012). Overall transplantation rates were 32% (95% CI= 21%, 43%, n=81) for NAC vs. 45% (95% CI= 34%, 55%, n=92) for placebo, p=0.093.
Table 2.
Overall survival and transplant-free survival for treatment groups stratified by coma category at randomization at 21 days of follow-up.
| Outcome | Coma Category at Randomization | Treatment Group | Treatment Group by Outcome for each Coma Category | Overall Treatment Group by Outcome | Breslow-Day | ||
|---|---|---|---|---|---|---|---|
| Placebo | NAC | One sided p-value | One sided p-value | One sided p-value | Odds Ratio (NAC/Placebo) | ||
|
Overall Survival | |||||||
| 21 Days | I – II | 75%, n=56 | 79%, n=58 | 0.292 | 0.283 | 0.262 | 1.28 |
| 63% – 87% | 68% – 91% | 0.53 – 3.07 | |||||
|
|
|
||||||
| III – IV | 53%, n=36 | 48%, n=23 | 0.645 | 0.82 | |||
| 35% – 70% | 25% – 70% | 0.29 – 2.34 | |||||
|
| |||||||
| Total | 66%, n=92 | 70%, n=81 | |||||
| 56% – 77% | 60% – 81% | ||||||
|
| |||||||
|
Transplant-free Survival | |||||||
| 21 Days | I – II | 30%, n=56 | 52%, n=58 | 0.010 | 0.043 | 0.012 | 2.46 |
| 17% – 43% | 38% – 65% | 1.14 – 5.30 | |||||
|
|
|
||||||
| III – IV | 22%, n=36 | 9%, n=23 | 0.912 | 0.33 | |||
| 7% – 37% | 0% – 22% | 0.06 – 1.74 | |||||
|
| |||||||
| Total | 27%, n=92 | 40% n=81 | |||||
| 18% – 37% | 28% – 51% | ||||||
Survival Analysis
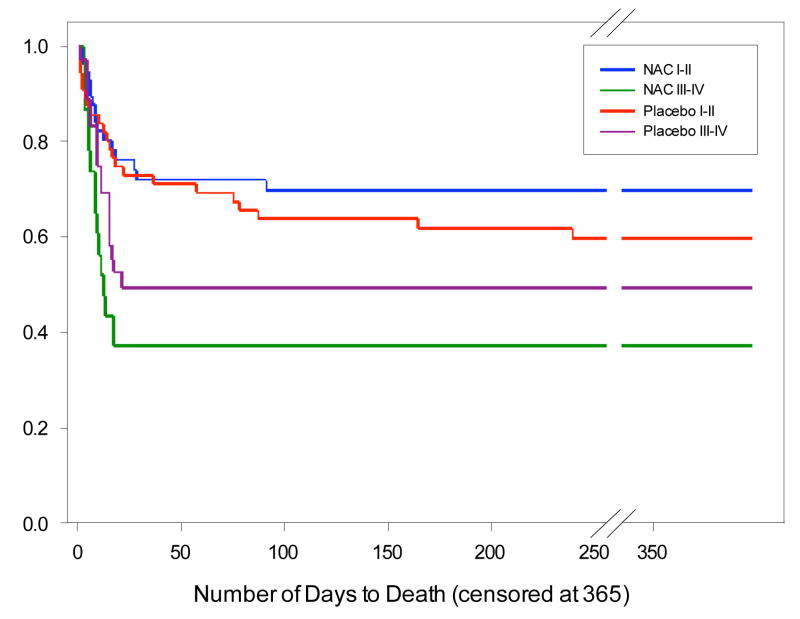
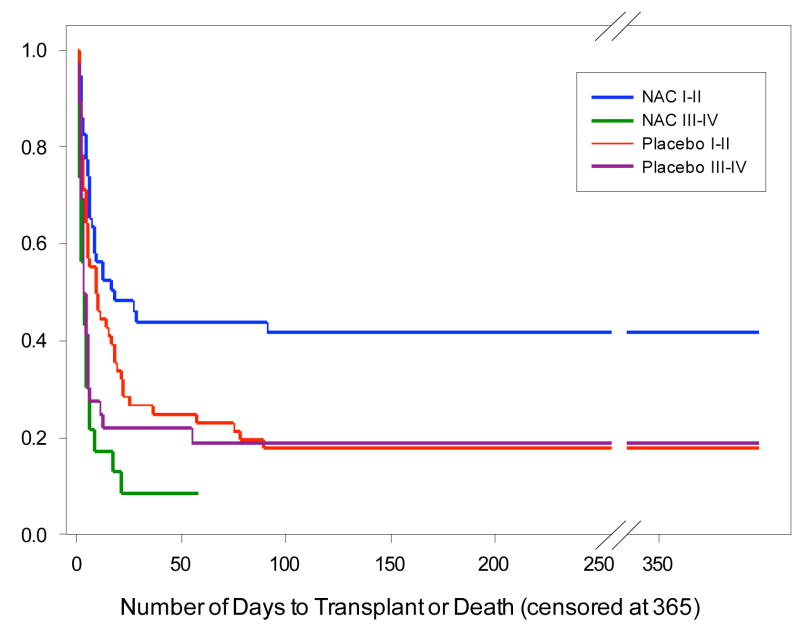
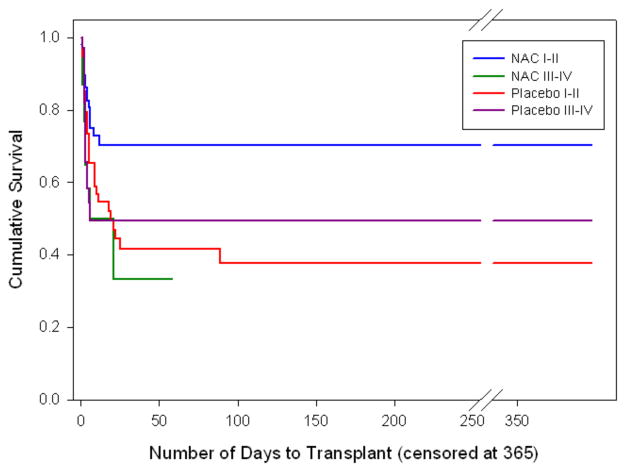
Treatment group/coma category was found to have significantly different survival times using the Log Rank Test (p=0.007; Figure 2). Patients in the NAC I–II group were found to have significantly longer survival than Placebo III–IV (p = 0.012) and NAC III–IV (p = 0.002), but not Placebo I–II (p =0.350). For the secondary outcome of survival without transplant, treatment group/coma category was significantly different (p=0.001; Figure 3). Patients in the NAC coma category I–II group were found to have significantly longer transplant-free survival time than the other three groups (largest p = 0.017). For the other secondary outcome, transplantation, treatment group/coma category was found to be significant (p = 0.025). Patients in the NAC coma category I–II group were found to have a significantly longer time to transplantation than the other three groups (largest p = 0.032). In a sub-analysis of the primary and secondary outcomes for patients receiving ≥ 4 hours or ≥ 24 hours infusion, the results were similar to those reported (results not shown).
Figure 2.
Kaplan-Meier curve for each group (treatment by coma category) was used to show overall survival to 365 days. In separate analyses, patients in the NAC I–II group demonstrated significantly higher survival than either Placebo III–IV (p = 0.012) or NAC III–IV (p = 0.002). Number of patients with censored data prior to 365 days: 14 in NAC I–II, 5 in NAC III–IV, 12 in Placebo I–II, 7 in Placebo III–IV.
Figure 3.
Kaplan-Meier curves for each group (treatment by coma category) showing transplant-free survival to 365 days. Patients in the NAC I–II group demonstrated significantly higher transplant-free survival than the other three groups (largest p = 0.017). Number of patients with censored data prior to 365 days: 10 in NAC I–II, 2 in NAC III–IV, 5 in Placebo I–II, 2 in Placebo III–IV. Note: 2 patients in the NAC III–IV group were censored, one at day34 and the other at day 58.
When overall and transplant-free survival were considered within each of the four largest etiologic groups, patients with DILI or hepatitis B showed improved outcomes compared to those with AIH or indeterminate etiologies (Table 4). For example, transplant-free survival for DILI patients was 58% (95% CI=33%, 83%) for those receiving NAC compared to 27% (95% CI=8%, 46%) for those receiving placebo, and was 40% (95% CI=19%, 61%) for NAC vs. 17% (95% CI=0%, 42%) for placebo for HBV patients. Since the numbers in each group were small, we did not draw conclusions or calculate significance, based on these analyses.
Table 4.
Overall and transplant-free survival according to etiology. Percentage, n and 95% CI.
| Overall Survival | Transplant-free survival | |||
|---|---|---|---|---|
| Etiology | Placebo | NAC | Placebo | NAC |
| DILI | 65%, n=26 | 79%, n=19 | 27%, n=26 | 58%, n=19 |
|
| ||||
| N=45 | 45% – 86% | 58% – 100% | 8% – 46% | 33% – 83% |
|
| ||||
| AIH | 67%, n=15 | 64%, n=11 | 27%, n=15 | 9%, n=11 |
| N=26 | 34% – 94% | 31% – 97% | 1% – 52% | 0% – 31% |
|
| ||||
| HBV | 50%, n=12 | 76%, n=25 | 17%, n=12 | 40%, n=25 |
| N=37 | 18% – 83% | 57% – 95% | 0% – 42% | 19% – 61% |
|
| ||||
| Indeterminate | 69%, n=26 | 60%, n=15 | 23%, n=26 | 40%, n=15 |
| N=41 | 50% – 89% | 32% – 88% | 5% – 41% | 12% – 68% |
DILI – Drug induced liver injury; AIH – autoimmune hepatitis; HBV – hepatitis B virus. Patients with DILI or HBV appeared to have improved overall and transplant-free survival when compared to those with AIH or indeterminate ALF.
Use of acetaminophen
To determine if unrecognized acetaminophen toxicity might have caused some of the indeterminate cases, sera from 113 patients (those with available samples) were analyzed after the conclusion of the trial using a highly sensitive and specific assay for acetaminophen adducts in serum.21,22 Three patients in each treatment group had adduct levels strongly implicating high-dose acetaminophen ingestions. A re-analysis excluding these 6 cases showed no difference in outcomes or percentage survival for the two treatment groups.
Length of hospital stay, number of organ systems failing
In comparing length of hospital stay among survivors, a trend was observed for NAC-treated patients to have shorter hospital stays (median 9 vs. 13 days (p=0.056). Comparison of organ system failure(s) between the two treatment groups failed to demonstrate individual (or total group) significant differences (Supplemental Table 1). This appears to relate to the small number of defined organ failure events occurring during the immediate study period. Progression or regression of encephalopathy between the two treatment groups appeared to be similar.
Adverse Events
Adverse events were equal between the groups (Supplemental Table 2); side effects were minimal with no differences in incidence except for nausea and vomiting, present in 14% (95% CI= 6%, 22%, n=81) of NAC treated patients and 4% (95% CI=0%, 9%, n=92) of placebo patients (p=0.031). Although bronchospasm has been reported with NAC, only one patient in each treatment group experienced this symptom.
DISCUSSION
There is no established treatment for non-acetaminophen acute liver failure other than liver transplantation. Our study suggests that transplant-free survival was improved by N-acetylcysteine. However, this improvement in survival was primarily observed in those with early stage hepatic encephalopathy: among those with coma grade I–II at admission, 52% receiving NAC survived without transplantation vs. 30% survival for those who received placebo. This finding was supported by the survival analyses (Figures 2 and 3).
Advanced coma grade patients showed no benefit from NAC but represented a smaller patient group, half the size of the early coma grade group. Within the advanced coma group, 10% died or were withdrawn from care while still on study medication, 50% died or underwent transplantation by 4 days and nearly 90% achieved these outcomes by 3 weeks. Among the 100 study patients of all grades listed for transplantation, 67 received a graft, 30 (45%) within 48 hours of study initiation. Twenty one of 59 advanced coma grade patients (36% overall, 57% of those listed) received a transplant by day 4, compared to 23/114 (20% overall, 37% of those listed) with early coma grades, confirming that coma grade at admission determines outcome, and, more specifically, whether a transplant will be obtained and utilized in rapid fashion. Only 4 additional patients in the advanced coma group were transplanted after day 4, vs. 19 additional grafts for those with early grade encephalopathy. The majority of patients recovered after transplantation, although short-term survival was slightly decreased when compared to patients with chronic liver disease.23 Thus, high early mortality, rapid transplantation and excellent early post-transplant survival rates appeared more likely than any possible medical therapy to affect overall survival for those with advanced coma grades. By contrast, patients with early hepatic encephalopathy only reached the 50% outcome point by 10 days. There appeared to be additional benefit beyond three weeks in that the differences between the treatment/coma categories observed during the initial 21 days were more significantly different at 365 days. The apparent benefit for those with early encephalopathy suggests that NAC treatment, to affect outcome, must be instituted early in the course of disease.
The overall survival of 66% for the placebo group was 9% higher than the 57% we had predicted. Although the overall registry includes equal numbers of patients in coma grade I–II vs. III–IV, and we had predicted equal enrollment of early and late coma grade patients, as noted above, twice as many patients with early coma grades were enrolled in the study (66% (114) with coma grade I–II vs. 35% (59) with coma grade III–IV). We did not specifically target the early coma grades for enrollment; however, we excluded those considered pre-terminal or about to undergo liver transplantation. Although the apparent improved overall survival for placebo subjects in all coma grades is likely related to the over-representation of early coma grades, improvement in overall survival during the trial period for other reasons, such as improved intensive care, might also play a role.
Establishing prognosis in non-acetaminophen acute liver failure has proven difficult and is confounded by transplantation, since this ‘rescue’ intervention, which affected 40% of our patients, does not allow the true outcome (death or recovery) to occur. We predicted that NAC therapy might benefit patients undergoing transplantation but could not demonstrate this. Since short-term outcomes of transplantation hinge on many other factors, such as organ quality and availability, it seems unlikely, in retrospect, that a short-term pre-transplant medical therapy would make much difference. The main prognostic factors in 3-week survival for the overall group using multivariate analyses were coma grade and INR at admission to study; these important variables have been previously noted and used by others.24
The study groups were well balanced in terms of age, gender, weight and etiology. While the placebo patients had a longer apparent duration of illness, the groups were well matched in all other parameters including Model for End-stage Liver Disease (MELD) scores.25–27 The imbalance in numbers enrolled in the two groups reflected the randomization scheme which took into account site as well as coma grade using a blocking factor of 4, and did not appear to affect the balance in each group.
Of note, there were relatively similar numbers of patients (26 to 45) among the four main etiologies: DILI, autoimmune hepatitis, hepatitis B and indeterminate. There was a trend for improved overall and transplant-free outcomes among the DILI and hepatitis B patients and for less favorable overall outcomes among those with AIH or indeterminate etiology.
The study occurred over nearly 8 years despite the large number of study sites because of the difficulties encountered with enrollment in this already-rare condition: it was necessary to choose only the subgroup that were unrelated to acetaminophen which represents less than half of all ALF in the United States7, then to identify next of kin in a timely fashion, help them understand both the data registry and the nature of the trial so that informed consent could be obtained. The urgent nature of the study setting and the simultaneous consideration of transplantation often distracted attention from the study. In the early years, competing trials of liver assist devices and, later, availability of intravenous NAC (Acetadote®; FDA approved for acetaminophen poisoning in 2003) also confounded enrollment. Among our registry, 58 non-acetaminophen patients received NAC prior to consideration for study enrollment despite the lack of evidence regarding its efficacy.
Examining the evolution to secondary end points disclosed a trend toward shorter hospital stays but no other differences between the two treatment groups, possibly reflecting that few of our specified outcomes (such as use of mannitol, intubation) were reached during treatment. There were no changes in mean arterial pressure or urine output during NAC infusion; however, pulmonary artery catheters or other hemodynamic measurements were not mandated by the study and were rarely used. A recent retrospective study using historical controls in pediatric acute liver failure not due to acetaminophen showed improved transplant-free survival and shorter hospital stays with NAC.28
Nausea and vomiting were the only symptoms more frequent in the treatment than the placebo group. Along with its excellent safety profile, NAC is easy to administer, does not require intensive care and can be given in community hospitals.
In summary, a significantly improved transplant-free survival at 3 weeks and at one year was observed with the use of N-acetylcysteine for the treatment of non-acetaminophen related acute liver failure, the benefit being confined to those with early hepatic encephalopathy. Extrapolating NAC efficacy to patients with less severe liver injury (e.g., coagulopathy without encephalopathy) cannot be made from our study since all study patients were required to exhibit some degree of encephalopathy at enrollment. Use of NAC should not be a substitute for early referral to a transplant center for any patient demonstrating evidence of coagulopathy (prolonged INR), regardless of whether encephalopathy is present, since referral ensures that these critically ill patients can undergo urgent transplantation, should it be needed. Based on the present study and its generally favorable safety profile, intravenous NAC should be considered for patients with early stage non-acetaminophen acute liver failure. Additional studies are needed to determine the optimal dose and duration of NAC therapy, predictors of response and the physiologic basis for these improved outcomes.
Supplementary Material
Figure 4.
Kaplan-Meier curves for each group (treatment by coma category) showing number of days to transplantation to 365 days. Patients in the NAC I–II group demonstrated significantly longer time to transplantation than the other three groups (largest p = 0.032). Number of patients with censored data prior to 365 days: 10 in NAC I–II, 2 in NAC III–IV, 5 in Placebo I–II, 3 in Placebo III–IV. Note: 2 patients in the NAC III–IV group were censored, one at day34 and the other at day 58.
Table 3.
Transplantation rate for treatment groups stratified by coma category at randomization at 21 days follow-up.
| Outcome | Coma Category at Randomization | Treatment Group | Treatment Group by Outcome for each Coma Category | Overall Treatment Group by Outcome | Breslow-Day | ||
|---|---|---|---|---|---|---|---|
| Placebo | NAC | p-value | p-value | p-value | Odds Ratio (NAC/Placebo) | ||
|
Transplanted | |||||||
| 21 Days | I – II | 46%, n=56 | 28%, n=58 | .037 | 0.093 | 0.180 | 0.44 |
| 32% – 60% | 15% – 40% | 0.20 – .96 | |||||
|
|
|
||||||
| III – IV | 42%, n=36 | 43%, n=23 | .891 | 1.08 | |||
| 24% – 59% | 21% – 66% | 0.37 – 3.10 | |||||
|
| |||||||
| Total | 45%, n=92 | 32%, n=81 | |||||
| 34% – 55% | 21% – 43% | ||||||
Acknowledgments
*Members and institutions participating in the Acute Liver Failure Study Group 1998–2006: W.M. Lee, MD (Principal Investigator), George A. Ostapowicz, MD, Frank V. Schiødt, MD, Julie Polson, MD, University of Texas Southwestern, Dallas, TX; Anne M. Larson, MD, University of Washington, Seattle, WA; Timothy Davern, MD, University of California, San Francisco, CA; Michael Schilsky, MD, Mount Sinai School of Medicine, NY, NY; Timothy McCashland, MD, University of Nebraska, Omaha, NE; J. Eileen Hay, MBBS, Mayo Clinic, Rochester, MN; Natalie Murray, MD, Baylor University Medical Center, Dallas, TX; A. Obaid S. Shaikh, MD, University of Pittsburgh, Pittsburgh, PA; Andres Blei, MD, Northwestern University, Chicago, IL; Atif Zaman, MD, University of Oregon, Portland, OR; Steven H.B. Han, MD, University of California, Los Angeles, CA; Robert Fontana, MD, University of Michigan, Ann Arbor, MI; Brendan McGuire, MD, University of Alabama, Birmingham, AL; Ray Chung, MD, Massachusetts General Hospital, Boston, MA; Alastair Smith, MB, ChB, Duke University Medical Center, Durham, NC; Robert Brown, MD, Cornell/Columbia University, NY, NY; Jeffrey Crippin, MD, Washington University, St Louis, MO; Edwin Harrison, Mayo Clinic, Scottsdale, AZ; Adrian Reuben, MBBS, Medical University of South Carolina, Charleston, SC; Santiago Munoz, MD, Albert Einstein Medical Center, Philadelphia, PA; Rajender Reddy, MD, University of Pennsylvania, Philadelphia, PA; R. Todd Stravitz, MD, Virginia Commonwealth University, Richmond, VA; Lorenzo Rossaro, MD, University of California Davis, Sacramento, CA; Raj Satyanarayana, MD, Mayo Clinic, Jacksonville, FL; and Tarek Hassanein, MD, University of California, San Diego, CA. The University of Texas Southwestern Administrative Group included Grace Samuel, Ezmina Lalani, Carla Pezzia, and Corron Sanders, PhD and the Statistics and Data Management Group included, Joan Reisch, PhD, Linda Hynan, PhD, Janet P. Smith, Joe W. Webster, and Mechelle Murry. We further acknowledge all the coordinators from the study sites who participated in this study. We dedicate this paper to Andres T. Blei, our friend and colleague. Andy was a passionate contributor to the work of the ALF Study Group for nearly 12 years.
The support of the following grants is gratefully acknowledged: R-03 DK52827, R-01 DK58369, U-01 DK58369 from NIDDK, NIH, and FD-R-001661 from the Orphan Products Division, United States Food and Drug Administration (FDA). Additional funding provided by the Stephen Tips Fund of the Northwestern Medical Foundation and the Jeanne Roberts and Rollin and Mary Ella King Funds of the Southwestern Medical Foundation. This study was performed under IND # 56925, filed with the FDA. The N-acetylcysteine used in the trial was supplied initially by Apothecon/Geneva Pharmaceuticals, a division of Bristol Myers Squibb, and, after April 2003, by Cumberland Pharmaceuticals, Nashville, TN. No additional support, data analysis or input of any kind was provided by these companies.
Footnotes
There are no conflicts of interest to disclose. The statistical analysis of the entire data sets pertaining to efficacy (specifically primary and major secondary efficacy endpoints) and safety (specifically, serious adverse events as defined in federal guidelines) have been independently confirmed by a biostatistician who is not employed by the corporate entity. The corresponding author had full access to all of the data and takes full responsibility for the veracity of the data and analysis. This is a randomized clinical trial (ClinicalTrials.gov number NCT00004467)
The Data and Safety Monitoring Board for the trial included Michael W. Fried, Chair, University of North Carolina, Chapel Hill; Edward Geehan, Georgetown University, Washington, DC: Lewis Tepperman, New York University; Caroline Riely, University of Tennessee, Memphis; Patrick Northup, University of Virginia, Charlottesville; Prashant Pandya, VA Medical Center, Kansas City, MO; Aynar Unalp-Arida, Johns Hopkins University, Baltimore, MD:
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lee WM. Medical Progress: Acute liver failure. N Engl J Med. 1993;329:1862–72. doi: 10.1056/NEJM199312163292508. [DOI] [PubMed] [Google Scholar]
- 2.Polson J, Lee WM. American Association for the Study of Liver Disease Position Paper: The management of acute liver failure. Hepatology. 2005;41:1179–97. doi: 10.1002/hep.20703. [DOI] [PubMed] [Google Scholar]
- 3.Rakela J, Mosley JW, Edwards VM, Govindarajan S, Alpert E. A double-blinded, randomized trial of hydrocortisone in acute hepatic failure. The Acute Hepatic Failure Study Group. Dig Dis Sci. 1991;36:1223–28. doi: 10.1007/BF01307513. [DOI] [PubMed] [Google Scholar]
- 4.Rake MO, Flute PT, Shilkin KB, Lewis ML, Winch J, Williams R. Early and intensive therapy of intravascular coagulation in acute liver failure. Lancet. 1971;ii:1215–18. doi: 10.1016/s0140-6736(71)90540-x. [DOI] [PubMed] [Google Scholar]
- 5.Harrison PM, Hughes RD, Forbes A, Portmann B, Alexander GJM, Williams R. Failure of insulin and glucagon infusions to stimulate liver regeneration in fulminant hepatic failure. J Hepatol. 1990;10:332–36. doi: 10.1016/0168-8278(90)90141-d. [DOI] [PubMed] [Google Scholar]
- 6.Sinclair SB, Levy GA. Treatment of fulminant viral hepatic failure with prostaglandin E. A preliminary report. Dig Dis Sci. 1991;36:791–800. doi: 10.1007/BF01311239. [DOI] [PubMed] [Google Scholar]
- 7.Ostapowicz GA, Fontana RJ, Schiødt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med. 2002;137:945–54. doi: 10.7326/0003-4819-137-12-200212170-00007. [DOI] [PubMed] [Google Scholar]
- 8.Prescott LF, Critchley JA. The treatment of acetaminophen poisoning. Annu Rev Pharmacol Toxicol. 1983;23:87–101. doi: 10.1146/annurev.pa.23.040183.000511. [DOI] [PubMed] [Google Scholar]
- 9.Hamlyn AN, Douglas AP, James O. The spectrum of paracetamol (acetaminophen) overdose: clinical and epidemiological studies. Postgrad Med J. 1978;54:400–04. doi: 10.1136/pgmj.54.632.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rumack BH. Acetaminophen overdose in young children. Am J Dis Child. 1984;138:428–33. doi: 10.1001/archpedi.1984.02140430006003. [DOI] [PubMed] [Google Scholar]
- 11.Makin AJ, Wendon J, Williams R. A 7-year experience of severe acetaminophen-induced hepatotoxicity (1987–1993) Gastroenterology. 1995;109:1907–16. doi: 10.1016/0016-5085(95)90758-0. [DOI] [PubMed] [Google Scholar]
- 12.Harrison PM, Wendon JA, Gimson AE, Alexander GJ, Williams R. Improvement by acetylcysteine of hemodynamics and oxygen transport in fulminant hepatic failure. N Engl J Med. 1991;324:1852–7. doi: 10.1056/NEJM199106273242604. [DOI] [PubMed] [Google Scholar]
- 13.Walsh TS, Hopton P, Philips BJ, Mackenzie SJ, Lee A. The effect of N-acetylcysteine on oxygen transport and uptake in patients with fulminant hepatic failure. Hepatology. 1998;27:1332–40. doi: 10.1002/hep.510270520. [DOI] [PubMed] [Google Scholar]
- 14.Rank N, Michel C, Haertel C, Lenhart A, Welte M, Meier-Hellmann A, Spies C. N-acetylcysteine increases liver blood flow and improves liver function in septic shock patients: Results of a prospective, randomized, double-blind study. Crit Care Med. 2000;28:3799–3807. doi: 10.1097/00003246-200012000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Schneider J, Lutun P, Boudjema K, Wolf P, Tempé J-D. In vivo evidence of enhanced guanylyl cyclase activation during the hyperdynamic circulation of acute liver failure. Hepatology. 1994;19:38–44. [PubMed] [Google Scholar]
- 16.Alonso A, Lau J, Jaber BL, Weintraub A, Sarnak MJ. Prevention of radiocontrast nephropathy with N-acetylcysteine in patients with chronic kidney disease: a meta-analysis of randomized, controlled trials. Am J Kidney Dis. 2004;43:1–9. doi: 10.1053/j.ajkd.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 17.Zwingmann C, Bilodeau M. Metabolic insights into the hepatoprotective effect of N-acetylcysteine in mouse liver. Hepatology. 2006;443:454–63. doi: 10.1002/hep.21075. [DOI] [PubMed] [Google Scholar]
- 18.Hein OV, Ohring R, Schilling A, et al. N-acetylcysteine decreases lactate signal intensities in liver tissue and improves liver function in septic shock patients, as shown by magnetic resonance spectroscopy: extended case report. Crit Care. 2004;8:R66–R71. doi: 10.1186/cc2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sklar GE, Subramaniam M. Acetylcysteine treatment for non-acetaminophen-induced acute liver failure. Ann Pharmacother. 2004;38:498–500. doi: 10.1345/aph.1D209. [DOI] [PubMed] [Google Scholar]
- 20.Trey C, Davidson CS. The management of fulminant hepatic failure. In: Popper H, Schaffner F, editors. Progress in liver diseases. New York: Grune & Stratton; 1970. pp. 282–98. [PubMed] [Google Scholar]
- 21.Davern TJ, II, James LP, Hinson JA, et al. Measurement of serum acetaminophen-protein adducts in patients with acute liver failure. Gastroenterology. 2006;130:687–94. doi: 10.1053/j.gastro.2006.01.033. [DOI] [PubMed] [Google Scholar]
- 22.James LP, Alonso EM, Hynan LS, et al. Detection of acetaminophen-protein adducts in children with acute liver failure of indeterminate cause. Pediatrics. 2006;118:676–81. doi: 10.1542/peds.2006-0069. [DOI] [PubMed] [Google Scholar]
- 23.O’Grady J, Alexander GJM, Hayllar KM, Williams R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology. 1989;97:439–45. doi: 10.1016/0016-5085(89)90081-4. [DOI] [PubMed] [Google Scholar]
- 24.Wiesner R, Edwards E, Freeman R, et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–96. doi: 10.1053/gast.2003.50016. [DOI] [PubMed] [Google Scholar]
- 25.Kremers WK, van IJperen M, Kim WR, et al. MELD score as a predictor of pre-transplant and posttransplant survival in OPTN/UNOS status 1 patients. Hepatology. 2004;39:764–69. doi: 10.1002/hep.20083. [DOI] [PubMed] [Google Scholar]
- 26.Zaman MB, Hoti E, Qasim A, et al. MELD score as a prognostic model for listing acute liver failure patients for liver transplantation. Transplant Proc. 2006;38:2097–98. doi: 10.1016/j.transproceed.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Katoonizadeh A, Decaestecker J, Wilmer A, et al. MELD score to predict outcome in adult patients with non-acetaminophen induced acute liver failure. Liver Int. 2007;27:329–34. doi: 10.1111/j.1478-3231.2006.01429.x. [DOI] [PubMed] [Google Scholar]
- 28.Kortsalioudaki C, Taylor RM, Cheeseman P, Bansal S, Mieli-Vergani G, Dhawan A. Safety and efficacy of N-acetylcysteine in children with non-acetaminophen-induced acute liver failure. Liver Transpl. 2008;14:25–30. doi: 10.1002/lt.21246. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.