Abstract
Purpose
This study evaluated the potential use of the computed tomography indices (CTI) on cone beam CT (CBCT) images for an assessment of the bone mineral density (BMD) in postmenopausal osteoporotic women.
Materials and Methods
Twenty-one postmenopausal osteoporotic women and 21 postmenopausal healthy women were enrolled as the subjects. The BMD of the lumbar vertebrae and femur were calculated by dual energy X-ray absorptiometry (DXA) using a DXA scanner. The CBCT images were obtained from the unilateral mental foramen region using a PSR-9000N™ Dental CT system. The axial, sagittal, and coronal images were reconstructed from the block images using OnDemend3D™. The new term "CTI" on CBCT images was proposed. The relationship between the CT measurements and BMDs were assessed and the intra-observer agreement was determined.
Results
There were significant differences between the normal and osteoporotic groups in the computed tomography mandibular index superior (CTI(S)), computed tomography mandibular index inferior (CTI(I)), and computed tomography cortical index (CTCI). On the other hand, there was no difference between the groups in the computed tomography mental index (CTMI: inferior cortical width).
Conclusion
CTI(S), CTI(I), and CTCI on the CBCT images can be used to assess the osteoporotic women.
Keywords: Cone-Beam Computed Tomography, Osteoporosis, Bone Density
Introduction
Osteoporosis is a systemic disease characterized by a low bone mass, deterioration of the bone structure and increased bone fragility.1 Bone loss occurs with aging after approximately 30 years. In particular, the rate of bone loss increases after menopause in women. In women there is a period of bone loss for 5-10 years post menopause. After this period the rate of bone loss declines at a more gradual rate.2
Dental radiographs are used widely in the adult population. Therefore, dental radiographs may offer an opportunity as a screening tool for osteoporosis.1,3,4 Jaw bone density can be assessed using intraoral radiographs,3 panoramic radiographs,4,5 cone beam CT (CBCT),6 quantitative CT (QCT),7,8 and dual energy X-ray absorptiometry (DXA).9-11
DXA is known as the most accurate clinical method for identifying those with low bone mineral density (BMD).9-11 BMD in the mandible is positively correlated with that in the lumbar spine and femoral neck in osteoporosis.10,11 Taguchi et al12 observed a significant correlation between the mandibular cortical measurements and vertebral BMD measured by DXA.
Panoramic mandibular index (PMI) on panoramic radiograph has been used to assess the mandibular bone quality.4,5 Measurement of the cortical width and a subjective assessment of cortical porosity on panoramic radiographs are methods used previously to diagnose osteoporosis.5,12 Klemetti et al5 reported that the linear correlation of the PMI with the BMD values was weak. Drozdzowska13 demonstrated that the efficacy of the panoramic-based mandibular indices in the diagnosis of osteoporosis was low to moderate. On the other hand, Horner and Devlin14 and Taguchi et al12,15 reported that the mandibular cortical index (MCI) was a useful method for osteoporosis screening.
On the other hand, there was no report on the use of the computed tomography indices (CTI) on CBCT images to evaluate the mandibular bone quality. This study was examined the potential use of CTI on the CBCT images for an assessment of the BMD in postmenopausal osteoporotic women.
Materials and Methods
Twenty-one postmenopausal osteoporotic Korean women between the ages of 55 and 72 (mean: 66.0) and 21 postmenopausal healthy women between the ages of 55 and 80 (mean: 60.0) were enrolled as the subjects in this study. The exclusion criteria were metabolic bone diseases such as hyper-, hypoparathyroidism, diabetes, osteomalacia, thyrotoxicosis, and renal disease. Informed consent was obtained from the patients who participated in this study on osteoporosis.
Evaluation of bone mineral density
The BMD (T score, Korean) of the lumbar vertebrae (L1-L3) and femur by DXA using a DXA scanner (Hologic Discovery QDR®, Hologic Inc, Bedford, MA, USA) were calculated. The height and weight were measured at the time of DXA scanning. The subjects with a T score value ≤-2.5 at both the lumbar and femoral neck were classified as osteoporotic, and a T score value ≥-1.0 was classified as normal.
CBCT images
CBCT images were obtained from the unilateral mental foramen region using a PSR-9000N™ Dental CT system (Asahi Roentgen Ind Co Ltd, Kyoto, Japan) at 80 kV, 10 mA, 30 seconds, and the pixel size was 0.15 mm. The axial, sagittal, and coronal images were reconstructed from the block images using OnDemend3D™ (Cybermed Inc, Seoul, Korea).
One oral and maxillofacial radiologist with 13 years of experience performed the measurements on a LCD monitor with resolution of 1,280×1,024. The measurements were repeated after 2 weeks.
CBCT measurements
The terms "CTI(S)", "CTI(I)", "CTMI", and "CTCI" on CBCT images were used in the present study. They were modified Ledgerton's classification16 on panoramic images.
CTI(S): computed tomography mandibular index (superior), which was the ratio of the inferior cortical width to the distance from the superior margin of the mental foramen to the inferior border of the mandible
CTI(S)=W/S
CTI(I): computed tomography mandibular index (inferior), which was the ratio of the inferior cortical width to the distance from the inferior margin of the mental foramen to the inferior border of the mandible
CTI(I)=W/I
CTMI: computed tomography mental index, which was the inferior cortical width of the mandible
CTMI=W
CTCI: computed tomography cortical index, which was the type of the inferior mandibular cortex
CTCI : Type 1, 2 and 3
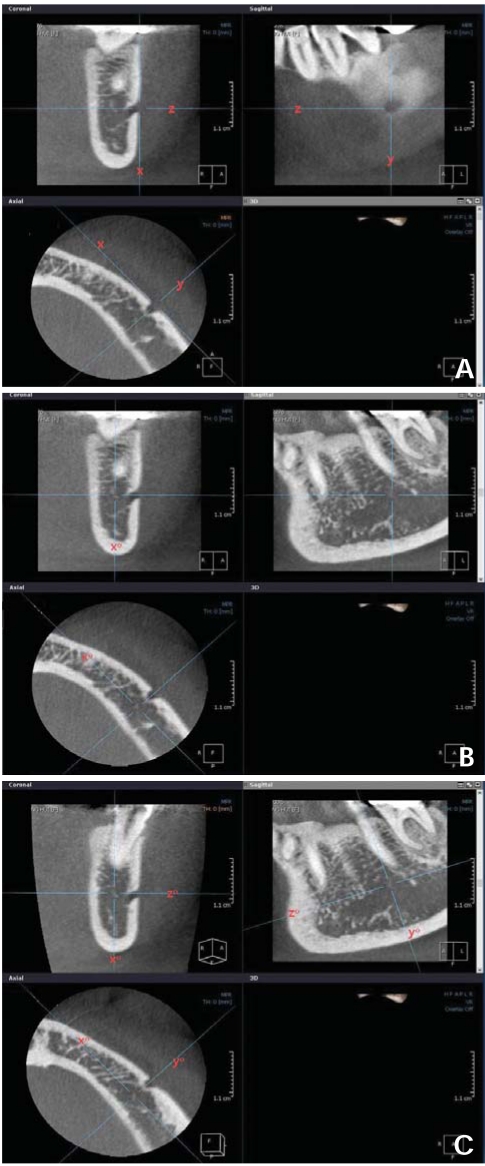
On the axial image, an antero-posterior tangent line "x" was drawn, and line "y" and "z" were drawn perpendicular to line "x" through the center of the mental foramen, then these lines became perpendicular mutually (Fig. 1A). On the coronal image, line "x" was moved to line "x°", the bisecting position of the bucco-lingual dimension of the mandibular body (Fig. 1B). On the sagittal image, line "z" was moved to line "z°", parallel position with the mandibular inferior border of the mandible, then line "y" corresponds with line "y°", perpendicular line "z°" at the same time (Fig. 1C).
Fig. 1.
A. On the axial image, an antero-posterior tangent line "x" is drawn, and line "y" and "z" are drawn perpendicular to line "x" through the center of the mental foramen, then these lines become perpendicular mutually. B. On the coronal image, line "x" is moved to line "x°", the bisecting position of the bucco-lingual dimension of the mandibular body. C. On the sagittal image, line "z" is moved to line "z°", parallel position with the mandibular inferior border of the mandible, then line "y" corresponds with line "y°", perpendicular line "z°" at the same time.
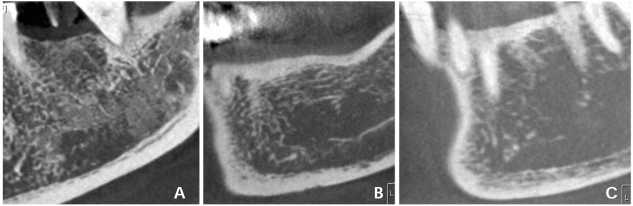
On the coronal image, the distance "S" from the superior margin of the mental foramen to the inferior border of the mandible was measured (Fig. 2A). Distance "I" was measured from the inferior margin of the mental foramen to the inferior border of the mandible (Fig. 2B). And inferior cortical width (W) was measured (Fig. 2C).
Fig. 2.
A. Distance "S" from the superior margin of the mental foramen to the inferior border of the mandible is measured on coronal image. B. Distance "I" is measured from the inferior margin of the mental foramen to the inferior border of the mandible. C. Inferior cortical width (W) of the mandible is measured.
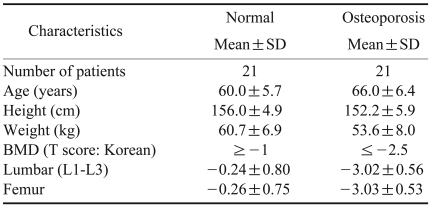
The types of the inferior mandibular cortex were subjectively classified as follows:
Type 1: the cortical endosteal margin appears even and regular (Fig. 3A)
Fig. 3.
The types of the inferior mandibular cortex are subjectively classified as follows. A. Type 1: the cortical endosteal margin appears even and regular. B. Type 2: the endosteal margin appears semilunar defects or 1 to 2 layers of cortical endosteal residues. C. Type 3: the cortical layer has numerous (>3) endosteal residues and is clearly porous.
Type 2: the endosteal margin shows semilunar defects or 1 to 2 layers of cortical endosteal residues (Fig. 3B)
Type 3: the cortical layer has numerous (>3) endosteal residues and is clearly porous (Fig. 3C)
Statistical analysis
The relationships between the CTI(S), CTI(I), CTCI, and BMDs were assessed using a t-test. The CTMI was determined by linear regression analysis, and the intra-observer agreement was examined using the Pearson's correlation coefficient and Spearman's rho on SPSS 16.0 (SPSS Inc, Chicago, IL, USA) for Windows.
Results
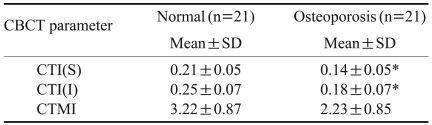
Table 1 lists the characteristics of the study subjects. A total number of 42 women were enrolled in this study. The mean age of the study population was 60.0 (SD 5.7) years in the normal group and 66.0 (SD 6.4) years in the osteoporosis group. The mean height and weight were 156.0 cm, 60.7 kg in the normal group and 152.2 cm and 53.6 kg in the osteoporosis group. The mean lumbar and femur BMD scores were respectively -0.24 and -0.26 in the normal group and -3.02 and -3.03 in the osteoporosis group.
Table 1.
Characteristics of the study subjects
Table 2 lists the mean values of the computed tomography parameters on the CBCT images. The mean values of the CTI(S) and CTI(I) were 0.21 and 0.25 in the normal group, and 0.14, 0.18 in the osteoporosis group. The mean value of the CTMI was 3.22 in the normal group, and 2.23 in the osteoporosis group. There were significant differences between the normal and osteoporosis groups in the CTI(S) and CTI(I) (P<0.05). On the other hand, there was no correlation between the groups in the CTMI (P>0.05).
Table 2.
Mean values of the computed tomography parameters on cone beam computed tomography (CBCT) image
*: significant at the 0.05 level t-test (2-tailed), CTI(S): computed tomography mandibular index (superior), CTI(I): computed tomography mandibular index (inferior), CTMI: computed tomography mental index (inferior cortical width)
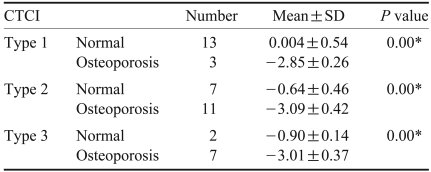
Table 3 lists the ability of CTCI to differentiate osteoporosis from normal on the CBCT images. The mean values of the Type 1, 2 and 3 were respectively 0.004, -0.64, -0.90 in the normal group, and -2.85, -3.09 and -3.01 in the osteoporosis group. There was a significant difference in the CTCI between the groups (P<0.05).
Table 3.
Ability of computed tomography cortical index (CTCI) to differentiate osteoporosis from normal on cone beam computed tomography image
*: correlation is significant at the 0.05 level t-test (2-tailed)
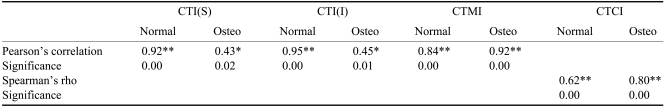
Table 4 lists the intra-observer agreement in the assessment of the CTI. The Pearson's correlation coefficients were respectively 0.92, 0.95, and 0.84 in the normal group, and 0.43, 0.45, and 0.92 in the osteoporosis group. The value of the Spearman's rho was 0.62 in the normal group, and 0.80 in the osteoporosis group. The intra-observer agreement showed a significant correlation for all parameters (P<0.05).
Table 4.
Intra-observer agreement in the assessment of the computed tomography indices (CTI) by Pearson's correlation coefficient and Spearman's rho
**: correlation is significant at the 0.01 level (2-tailed), *: 0.05 level, Osteo: osteoporosis, CTI(S): computed tomography mandibular index (superior), CTI(I): computed tomography mandibular index (inferior), CTMI: computed tomography mental index (inferior cortical width), CTCI: computed tomography cortical index
Discussion
This study examined the potential use of the CTI on CBCT images in diagnosis of osteoporosis in women.
Early diagnosis through bone density measurements allows proper management of osteoporosis to decrease the risk of fracture and disability. Many studies3,17,18 have examined the methods for detecting individuals with a low BMD at an early stage. Some investigators have investigated whether dental radiographs could play a role in the detection of individuals with osteoporosis.3-8 A basic requirement for this would be that the bone mass in the jaw might be related to that of other skeletal sites in which osteoporosis was a significant problem.
DXA, a well-established means of measuring the BMD in the spine and femoral neck, is the most reliable method to examine the bone density in the mandible.9-11 Adams19 reported that the precision of DXA of the spine ranged from 0.5 to 1%, whereas DXA of the femoral neck was 2-5%. Horner et al11 demonstrated that BMD measurements of the mandible showed a significant correlation with those of the lumbar vertebra and femoral neck. Taguchi et al8 reported the significant correlations between the mandibular BMDs using QCT and lumbar and femoral neck BMDs measured by DXA.
In the present study, DXA was used as the gold standard for the BMD measurements in the lumbar and femoral neck. The World Health Organization (WHO) set the threshold for the diagnosis of osteoporosis at a BMD of 2.5 or more standard deviations below the young normal reference measurements.
Some studies18,20,21 regarding the PMI on panoramic radiographs have been performed. Benson et al20 first suggested the PMI on a panoramic image. Watson et al21 reported that there was no difference in the mean PMI between normal and osteoporotic women. Klemetti et al22 stated that the PMI should not be used to assess the patient's status regarding osteoporosis.
On the other hand, the results of the present study on the CBCT images showed that the CTI(S) and CTI(I) was significantly different between the normal and osteoporotic groups (P<0.05). This result was contrary to those reported by Watson et al21 and Klemetti et al22 on the panoramic images.
Devlin et al23 demonstrated that the mandibular cortical width had better efficacy in detecting osteoporosis on a panoramic radiograph than the mandibular cortical index. There was no evidence for any benefit associated with combining the two measurements to detect osteoporosis. They insisted that only those with the thinnest mandibular cortices (≤3 mm) should be referred for a further osteoporosis investigation, because this group had the highest likelihood of osteoporosis. Horner et al24 found that a thinning of the mandibular cortex below 3 mm at the mental foramen on a panoramic radiograph was associated with a low skeletal mass (or osteopenia) at the spine or femoral neck.
Our results on the CBCT images showed no significant difference in CTMI between the normal and osteoporotic groups, which was contrary to those of earlier studies23,24 on the panoramic images.
Taguchi et al12 demonstrated that the cortical measurements detected on the panoramic images might be useful for identifying younger postmenopausal women with a low BMD or osteoporosis. They found that the sensitivity and specificity for diagnosing the spinal osteoporosis was 86.8% and 63.6%, respectively in normal postmenopausal women with cortical erosion on the panoramic image. They suggested that dentists should be able to refer postmenopausal women with suspected spinal osteoporosis for bone densitometry based on the panoramic radiographs. On the other hand, Drozdxowska13 reported that the efficacy of the panoramic-based mandibular indices in diagnosing osteopenia/osteoporosis was low to moderate. These results showed a significant relationship between the cortical erosion and the BMD (P<0.05), which corresponded to those reported by Taguchi et al.12
The intra-observer agreement of the present study showed a significant correlation in the CTI(S), CTI(I), and CTCI, however there was no correlation in the CTMI on the CBCT images.
The limitations of this study included the small sample size. Further studies with a larger sample and examination of the relationship between the CTI in patients with systemic diseases and BMDs are requested.
In conclusion, this study suggests that CTI(S), CTI(I), and CTCI on CBCT images can be used to assess the osteoporotic women.
References
- 1.Verheij JG, Geraets WG, van der Stelt PF, Horner K, Lindh C, Nicopoulou-Karayianni K, et al. Prediction of osteoporosis with dental radiographs and age. Dentomaxillofac Radiol. 2009;38:431–437. doi: 10.1259/dmfr/55502190. [DOI] [PubMed] [Google Scholar]
- 2.White SC. Oral radiographic predictors of osteoporosis. Dentomaxillofac Radiol. 2002;31:84–92. doi: 10.1038/sj.dmfr.4600674. [DOI] [PubMed] [Google Scholar]
- 3.Nackaerts O, Jacobs R, Devlin H, Pavitt S, Bleyen E, Yan B, et al. Osteoporosis detection using intraoral densitometry. Dentomaxillofac Radiol. 2008;37:282–287. doi: 10.1259/dmfr/30424604. [DOI] [PubMed] [Google Scholar]
- 4.Kim JY, Nah KS, Jung YH. Comparison of panorama radiomorphometric indices of the mandible in normal and osteoporotic women. Korean J Oral Maxillofac Radiol. 2004;34:69–74. [Google Scholar]
- 5.Klemetti E, Kolmakov S, Heiskanen P, Vainio P, Lassila V. Panoramic mandibular index and bone mineral densities in postmenopausal women. Oral Surg Oral Med Oral Pathol. 1993;75:774–779. doi: 10.1016/0030-4220(93)90438-a. [DOI] [PubMed] [Google Scholar]
- 6.Hua Y, Nackaerts O, Duyck J, Maes F, Jacobs R. Bone quality assessment based on cone beam computed tomography imaging. Clin Oral Implants Res. 2009;20:767–771. doi: 10.1111/j.1600-0501.2008.01677.x. [DOI] [PubMed] [Google Scholar]
- 7.Lindh C, Nilsson M, Klinge B, Petersson A. Quantitative computed tomography of trabecular bone in the mandible. Dentomaxillofac Radiol. 1996;25:146–150. doi: 10.1259/dmfr.25.3.9084263. [DOI] [PubMed] [Google Scholar]
- 8.Taguchi A, Tanimoto K, Suei Y, Ohama K, Wada T. Relationship between the mandibular and lumbar vertebral bone mineral density at different postmenopausal stages. Dentomaxillofac Radiol. 1996;25:130–135. doi: 10.1259/dmfr.25.3.9084261. [DOI] [PubMed] [Google Scholar]
- 9.Horner K, Karayianni K, Mitsea A, Berkas L, Mastoris M, Jacobs R, et al. The mandibular cortex on radiographs as a tool for osteoporosis risk assessment: the OSTEODENT project. J Clin Densitom. 2007;10:138–146. doi: 10.1016/j.jocd.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Karayianni K, Horner K, Mitsea A, Berkas L, Mastoris M, Jacobs R, et al. Accuracy in osteoporosis diagnosis of a combination of mandibular cortical width measurement on dental panoramic radiographs and a clinical risk index (OSIRIS): the OSTEODENT project. Bone. 2007;40:223–229. doi: 10.1016/j.bone.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 11.Horner K, Devlin H, Alsop CW, Hodgkinson IM, Adams JE. Mandibular bone mineral density as a predictor of skeletal osteoporosis. Br J Radiol. 1996;69:1019–1025. doi: 10.1259/0007-1285-69-827-1019. [DOI] [PubMed] [Google Scholar]
- 12.Taguchi A, Tsuda M, Ohtsuka M, Kodama I, Sanada M, Nakamoto T, et al. Use of dental panoramic radiographs in identifying younger postmenopausal women with osteoporosis. Osteoporos Int. 2006;17:387–394. doi: 10.1007/s00198-005-2029-7. [DOI] [PubMed] [Google Scholar]
- 13.Drozdzowska B, Pluskiewicz W, Tarnawska B. Panoramic-based mandibular indices in relation to mandibular bone mineral density and skeletal status assessed by dual energy X-ray absorptiometry and quantitative ultrasound. Dentomaxillofac Radiol. 2002;31:361–367. doi: 10.1038/sj.dmfr.4600729. [DOI] [PubMed] [Google Scholar]
- 14.Horner K, Devlin H. The relationship between two indices of mandibular bone quality and bone mineral density measured by dual energy X-ray absorptiometry. Dentomaxillofac Radiol. 1998;27:17–21. doi: 10.1038/sj.dmfr.4600307. [DOI] [PubMed] [Google Scholar]
- 15.Taguchi A, Suei Y, Ohtsuka M, Otani K, Tanimoto K, Ohtaki M. Usefulness of panoramic radiography in the diagnosis of postmenopausal osteoporosis in women. Width and morphology of inferior cortex of the mandible. Dentomaxillofac Radiol. 1996;25:263–267. doi: 10.1259/dmfr.25.5.9161180. [DOI] [PubMed] [Google Scholar]
- 16.Ledgerton D, Horner K, Devlin H, Worthington H. Panoramic mandibular index as a radiomorphometric tool: an assessment of precision. Dentomaxillofac Radiol. 1997;26:95–100. doi: 10.1038/sj.dmfr.4600215. [DOI] [PubMed] [Google Scholar]
- 17.Horner K, Allen P, Graham J, Jacobs R, Boonen S, Pavitt S, et al. The relationship between the OSTEODENT index and hip fracture risk assessment using FRAX. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:243–249. doi: 10.1016/j.tripleo.2010.03.035. [DOI] [PubMed] [Google Scholar]
- 18.Taguchi A, Suei Y, Sanada M, Ohtsuka M, Nakamoto T, Sumida H, et al. Validation of dental panoramic radiography measures for identifying postmenopausal women with spinal osteoporosis. AJR Am J Roentgenol. 2004;183:1755–1760. doi: 10.2214/ajr.183.6.01831755. [DOI] [PubMed] [Google Scholar]
- 19.Adams JE. Osteoporosis and bone mineral densitometry. Curr Opin Radiol. 1992;4:11–20. [PubMed] [Google Scholar]
- 20.Benson BW, Prihoda TJ, Glass BJ. Variations in adult cortical bone mass as measured by a panoramic mandibular index. Oral Surg Oral Med Oral Pathol. 1991;71:349–356. doi: 10.1016/0030-4220(91)90314-3. [DOI] [PubMed] [Google Scholar]
- 21.Watson EL, Katz RV, Adelezzi R, Gift HC, Dunn SM. The measurement of mandibular cortical bone height in osteoporotic vs. non-osteoporotic postmenopausal women. Spec Care Dentist. 1995;15:124–128. doi: 10.1111/j.1754-4505.1995.tb00494.x. [DOI] [PubMed] [Google Scholar]
- 22.Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Scand J Dent Res. 1994;102:68–72. doi: 10.1111/j.1600-0722.1994.tb01156.x. [DOI] [PubMed] [Google Scholar]
- 23.Devlin H, Karayianni K, Mitsea A, Jacobs R, Lindh C, van der Stelt P, et al. Diagnosing osteoporosis by using dental panoramic radiographs: The OSTEODENT project. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:821–828. doi: 10.1016/j.tripleo.2006.12.027. [DOI] [PubMed] [Google Scholar]
- 24.Horner K, Devlin H. The relationship between mandibular bone mineral density and panoramic radiographic measurements. J Dent. 1998;26:337–343. doi: 10.1016/s0300-5712(97)00020-1. [DOI] [PubMed] [Google Scholar]