Abstract
Purpose
The purpose of this study was to present the clinical features of a case series of osteomas in the craniofacial region and to compare them with those described in the dental literatures.
Materials and Methods
A retrospective study of 18 patients diagnosed with osteomas in the craniofacial region was performed. The age, gender, location, symptoms, and the radiological findings were recorded.
Results
There were 13 women and 5 men from 18 years to 69 years of age (mean age, 42±27 years). Fourteen osteomas were found in the mandible (78%), two in frontal sinus, one in sphenoid bone, and one in maxilla.
Conclusion
Osteomas are benign tumors composed of mature compact bone or cancellous bone. They are essentially restricted to the craniofacial skeleton and rarely, if ever, are diagnosed in other bones.
Keywords: Osteoma, Jaw, Paranasal Sinuses
Introduction
Osteoma is a benign tumor composed of mature compact bone or cancellous bone. This tumor is essentially restricted to the craniofacial skeleton and rarely, if ever, is diagnosed in other bones.1,2 The mandible and paranasal sinuses are the most commonly affected sites in the maxillofacial region.3-5 In some countries the prevalence of the osteoma is about 1% of all patients in the ear, nose and throat (ENT) clinics.2 Clinically, this neoplasm may be silent for years without any symptoms and diagnosed only when it becomes large enough or observed coincidentally during radiological investigations.3,5 Osteoma of the jaws may arise on the surface of the bone, as a polypoid or sessile mass (periosteal osteoma), or it may be located in the medullary bone (endosteal osteoma).1
The etiology of osteoma is still unclear.1,3 Osteoma is a solitary lesion occurring predominantly in the skull and many authors suggested that most osteomas in the maxillofacial areas were reactive bone hyperplasia or advanced ossifications.2 Furlaneto et al6 contended that none of the proposed hypotheses related to the etiology of these lesions has been proven. The growth of the tumor is caused by the activity of either the periosteum or the endosteum. It can also be called central, peripheral, or extraskeletal.7 Peripheral osteoma is defined by centrifugal growth from the periosteum, while central osteomas arise centripetally from the endosteum.7,8 Although osteoma is essentially tumor of the craniofacial bone and rarely affects the extragnathal skeleton, cases of osteomas arising within soft tissue such as the bulk of skeletal muscles have been reported.5,9-11
The purpose of this article is to present the clinical features of a case series of osteomas occurring in the craniofacial region and to compare them with those described in dental literatures.3
Materials and Methods
A retrospective study of the patients diagnosed with osteomas in the craniofacial region between 2004 and 2011 at Pusan National University Dental Hospital was performed. The following data were retrieved from the clinical records, the radiographic examination and the histologic analysis: age, gender, location, symptoms, type of osteoma, and treatment.
Results
There were 13 women and 5 men from 18 years to 69 years of age (mean age, 42±27 years). Fourteen (78%) osteomas were found in the mandible (Figs. 1-7), two in frontal sinus, one in sphenoid bone (Fig. 8), and one in maxilla (Fig. 9). Table 1 shows the clinical features of the osteomas. There were minor symptoms such as difficulties in chewing associated with the location of the large osteomas in mandibular condyle (Figs. 6 and 7) and the lingual side of the mandibular body (Figs. 2 and 3). Large osteomas located buccally caused some degree of facial swelling and asymmetry (Figs. 4 and 5). However, there was no headache caused by frontal sinus osteomas and the patients declined to be operated on. All the cases except for two osteomas located in the frontal sinus were confirmed by means of histological examination.
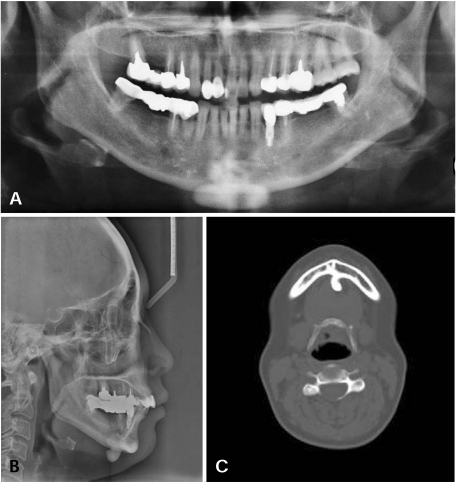
Fig. 1.
Radiographic images of case I (46/F). The osteoma is located at the lingual surface of mandibular symphysis. A. Panoramic image. B. Lateral cephalometric image. C. Axial CT image.
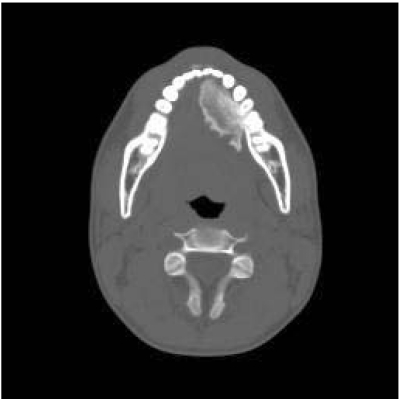
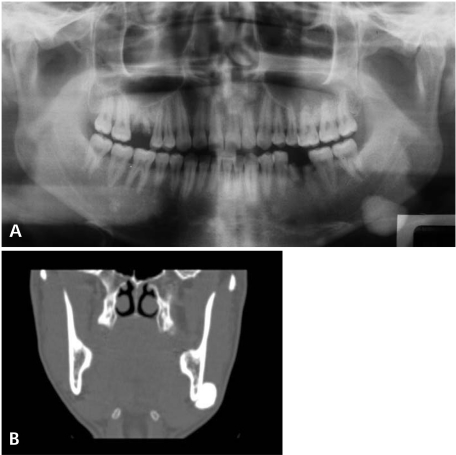
Fig. 7.
A. Panoramic image of case XIV (56/F) shows the osteoma located at the anterior surface of mandibular condyle. B. Axial CT image.
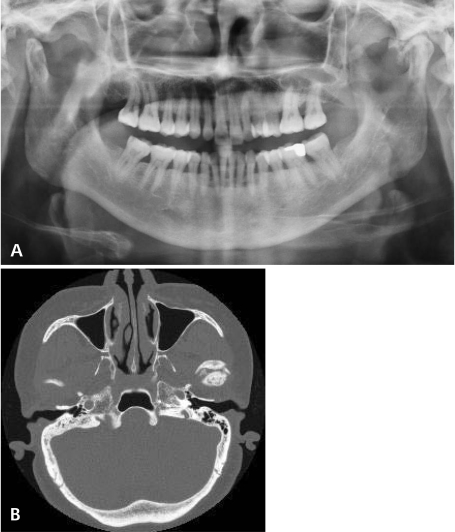
Fig. 8.
A. Panoramic view of case XV (43/F) shows the osteoma located at the infra- and supra-temporal fossa of sphenoid bone. B. Axial CT image. C. Coronal CT image.
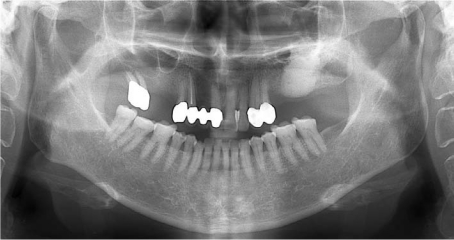
Fig. 9.
Panoramic image of case XVI (69/F) shows the osteoma located at the center of left palate without any buccopalatal expansion.
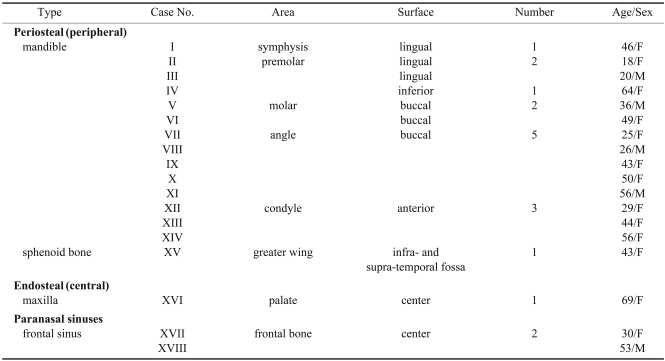
Table 1.
Clinical features of osteoma cases in this study
Fig. 6.
Panoramic image of case XIII (44F) shows the osteoma located at the anterior surface of mandibular condyle.
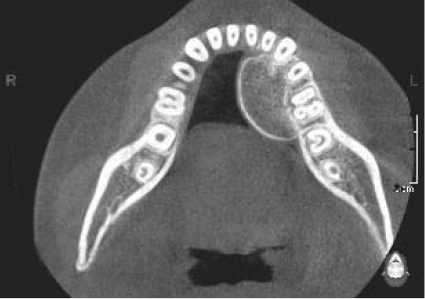
Fig. 2.
Axial CT image of case II (18/F) shows the osteoma located at the lingual surface of mandibular premolar area.
Fig. 3.
Axial CT image of case III (20/M) shows the osteoma located at the lingual surface of mandibular premolar area.
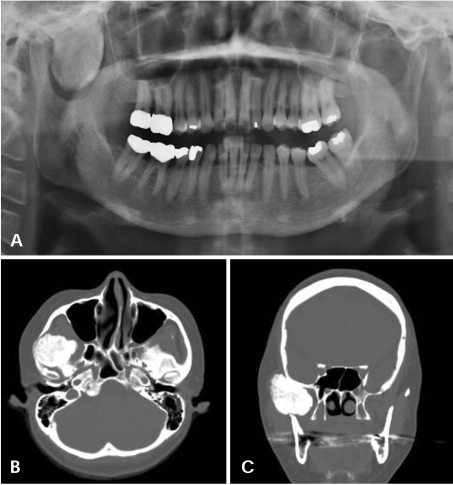
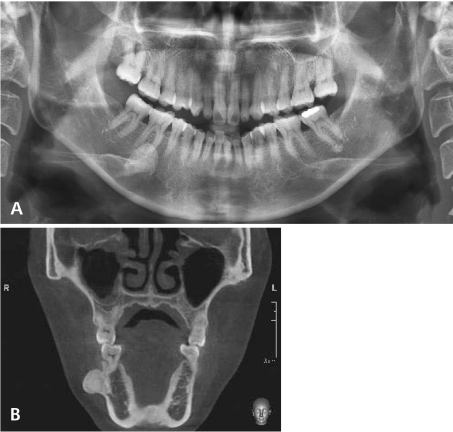
Fig. 4.
A. Panoramic image of case VI (49/F) shows the osteoma located at the buccal surface of mandibular molar area. B. Coronal CT image.
Fig. 5.
A. Panoramic image of case VIII (26/M) shows the osteoma located at the buccal surface of mandibular angle area. B. Coronal CT image.
Discussion
There is controversy whether osteoma represents true neoplasm, and not all lesions designated as an osteoma may represent a single entity. Some likely represent the end stage of an injury or inflammatory process or the end stage of a hamartomatous process such as fibrous dysplasia. The common palatal and mandibular tori and buccal exostosis are not considered to represent osteomas, although they are histologically identical to osteoma.1 In this study, the osteoma found in the left part of palate (case XVI) had the previous history of inflammation before the development of the osteoma. Also there were two cases of osteomas located at the mandibular tori area (case II and III), however the size was large enough to be considered as osteomas, though the ages of these two patients were younger than those of the rest of the patients.
The most common gnathic locations of the osteomas are the posterior body of the mandible or the condyle.1 In this study, 10 cases of the 14 mandibular osteomas occurred in the mandibular body or angle area, and 3 cases occurred in the condyle. Condylar osteomas are considered by some to be a true neoplasm, whereas others designate them as hyperostoses.1 Osteomas occurring in the condylar process can be classified into two types according to their pattern of proliferation: those that proliferate and cause replacement of the condyle by the osteoma and those that form a pedunculated or osseous mass on the condyle or neck of the mandible.3 However in this study, one condylar osteoma (case XIV) revealed rather irregular and quite atypical shape giving the false impression of synovial chondromatosis.
Osteoma is the most common benign tumor of the paranasal sinus. Its incidence is between 0.014% and 0.43%.12 It usually grows slowly. However, it may extend to the surrounding structures and cause severe intracranial or orbital complications.4 Larrea-Oyarbide et al,3 Sayan et al,7 and Longo et al.11 reported that the most frequently affected paranasal sinus of osteoma was the frontal, followed by the maxillary, ethmoidal, and sphenoidal sinuses. Though turbinate osteoma is very rare, some cases have been reported in literature.4,13-15 Osteomas arising in the paranasal sinuses may cause such symptoms as sinusitis, headache, or ophthalomologic manifestations,1 however in this study, the frontal sinus osteomas were found incidentally.
Footnotes
This study was supported by Pusan National University Hospital Grant.
References
- 1.Neville BW, Damm DD, Allen CM, Bouquot JE. Oral and maxillofacial pathology. 2nd ed. Philadelphia: WB Saunders Co; 2002. pp. 566–567. [Google Scholar]
- 2.Piattelli A, Scarano A, Di Alberti L, Piattelli M. Osteoma of the mandible. A case report. Acta Stomatol Belg. 1995;92:13–16. [PubMed] [Google Scholar]
- 3.Larrea-Oyarbide N, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Osteomas of the craniofacial region. Review of 106 cases. J Oral Pathol Med. 2008;37:38–42. doi: 10.1111/j.1600-0714.2007.00590.x. [DOI] [PubMed] [Google Scholar]
- 4.Kutluhan A, Salviz M, Bozdemir K, Deger HM, Culha I, Ozveren MF. Middle turbinate osteoma extending into anterior cranial fossa. Auris Nasus Larynx. 2009;36:702–704. doi: 10.1016/j.anl.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 5.Ogbureke KU, Nashed MN, Ayoub AF. Huge peripheral osteoma of the mandible: a case report and review of the literature. Pathol Res Pract. 2007;203:185–188. doi: 10.1016/j.prp.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Furlaneto EC, Rocha JR, Heitz C. Osteoma of the zygomatic arch - report of a case. Int J Oral Maxillofac Surg. 2004;33:310–311. doi: 10.1006/ijom.2002.0468. [DOI] [PubMed] [Google Scholar]
- 7.Sayan NB, Uçok C, Karasu HA, Günhan O. Peripheral osteoma of the oral and maxillofacial region: a study of 35 new cases. J Oral Maxillofac Surg. 2002;60:1299–1301. doi: 10.1053/joms.2002.35727. [DOI] [PubMed] [Google Scholar]
- 8.Kashima K, Rahman OI, Sakoda S, Shiba R. Unusual peripheral osteoma of the mandible: report of 2 cases. J Oral Maxillofac Surg. 2000;58:911–913. doi: 10.1053/joms.2000.8223. [DOI] [PubMed] [Google Scholar]
- 9.Bodner L, Gatot A, Sion-Vardy N, Fliss DM. Peripheral osteoma of the mandibular ascending ramus. J Oral Maxillofac Surg. 1998;56:1446–1449. doi: 10.1016/s0278-2391(98)90414-1. [DOI] [PubMed] [Google Scholar]
- 10.Ertas U, Tozoglu S. Uncommon peripheral osteoma of the mandible: report of two cases. J Contemp Dent Pract. 2003;4:98–104. [PubMed] [Google Scholar]
- 11.Longo F, Califano L, De Maria G, Ciccarelli R. Solitary osteoma of the mandibular ramus: report of a case. J Oral Maxillofac Surg. 2001;59:698–700. doi: 10.1053/joms.2001.23408. [DOI] [PubMed] [Google Scholar]
- 12.Eller R, Sillers M. Common fibro-osseous lesions of the paranasal sinuses. Otolaryngol Clin North Am. 2006;39:585–600. doi: 10.1016/j.otc.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 13.Viswanatha B. Middle turbinate osteoma. Indian J Otolaryngol Head Neck Surg. 2008;60:266–268. doi: 10.1007/s12070-008-0090-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin CJ, Lin YS, Kang BH. Middle turbinate osteoma presenting with ipsilateral facial pain, epiphora, and nasal obstruction. Otolaryngol Head Neck Surg. 2003;128:282–283. doi: 10.1067/mhn.2003.29. [DOI] [PubMed] [Google Scholar]
- 15.Ishimaru T. Superior turbinate osteoma: A case report. Auris Nasus Larynx. 2005;32:291–293. doi: 10.1016/j.anl.2005.03.004. [DOI] [PubMed] [Google Scholar]