Abstract
Steven-Johnson syndrome is a common condition characterised by erythematous target lesions on the skin and involvement of the oral mucosa, genitals and conjunctivae. It has been documented as one of the extra-pulmonary manifestations of Mycoplasma pneumoniae infection. Recently, there has been several documentation of an incomplete presentation of this syndrome – without the typical rash but with mucosal, conjunctival and genital involvement. Our case illustrates that the incomplete Steven-Johnson syndrome may present with oral mucosal and conjunctival involvement alone without skin or genital involvement. This important clinical diagnosis should not be missed due to its atypical presentation. Treatment of Steven-Johnson syndrome remains supportive along with treating the underlying infection if recognised.
Background
Steven-Johnson syndrome is often characterised by erythematous target lesions on the skin with oral mucosa, conjunctivae and genital involvement. Atypical presentation of this syndrome associated with Mycoplasma pneumoniae can present in adults without the typical skin or genital involvement. This atypical presentation should not be missed and it is important for clinicians to recognise, correctly diagnose and treat this clinical condition.
Case presentation
A 19-year-old male was admitted to the emergency admissions unit with a 1 week history of shortness of breath, productive cough, nausea and central pleuritic chest pain. He had been started on amoxicillin by his general practitioner a few days before admission to the hospital for a presumed community acquired pneumonia.
On examination, he was febrile (37.9°C), tachycardic (110 bpm) and hypoxic (SaO2 90%, pO2 7.31 on room air). Chest examination revealed few scattered expiratory wheeze but no crackles. Initial chest x-ray showed no focal lung consolidation.
The differential diagnoses at this stage included early pneumonia and pulmonary embolism. He was started on intravenous co-amoxiclav and treatment dose dalteparin. His CURB-65 score was one (no signs of confusion, urea: 7.1 mmol/l, respiratory rate: 25 per min and blood pressure: 108/62). According to the trust guidelines, macrolides were not indicated at this stage. CT pulmonary angiogram was negative for pulmonary embolus but revealed bilateral diffuse, patchy ground glass opacification and tree in bud nodularity in keeping with early infection. Treatment dose dalteparin was discontinued.
The following morning, he developed multiple painful ulcers, with yellow exudates throughout his mouth. These spread onto the palate, lips and tongue and caused him to have difficulty swallowing (figure 1). Later in the day, we noted conjunctival involvement as his left conjunctiva was hyperaemic with purulent discharge. No lesions elsewhere were noted and, in particular, examination of the genitalia was normal. These lesions were considered to be characteristic of Stevens-Johnson syndrome.
Figure 1.
Painful oral ulcerations.
He had a repeat chest x-ray which showed a more prominent perihilar bronchial wall thickening and patchy air space changes in the left lower lobe in keeping with infection (figure 2). Oral erythromycin was added for severe pneumonia.
Figure 2.
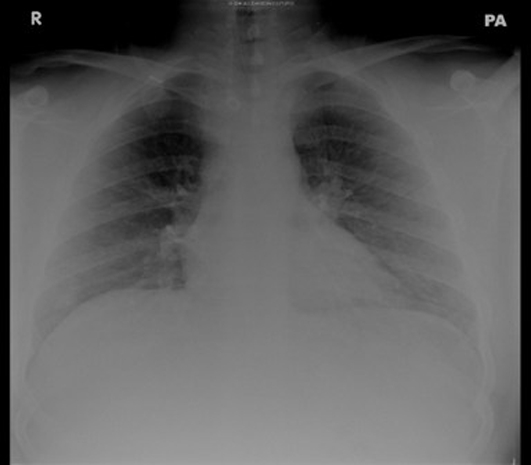
Chest x-ray after 48 h of admission.
Investigations
PCR tests for Herpes simplex and Varicella zoster viruses, urinary antigen for Legionella pneumophila and serum antibody for HIV were negative. Gram staining of material from the oral ulcers was also negative.
Because of the presentation with atypical pneumonia in combination with Stevens-Johnson syndrome, mycoplasma serology tests were taken in the acute phase which showed M pneumoniae complement fixation test titre >512 and the M pneumoniae agglutination test was positive which confirmed the diagnosis. Convalescent serum sample were taken 9 days postacute phase was consistent with recent M pneumoniae infection. The current British Thoracic Society guidelines recommend PCR of sputum and respiratory secretions, but this test was not available and we had to rely on serology and clinical diagnosis.
Treatment
Erythromycin was added to co-amoxiclav to broaden antibiotic cover.
Outcome and follow-up
The patient made a clinical improvement and was discharged home to complete a 2 week course of antibiotics. He was reviewed in the general medical outpatient clinic 4 weeks postdischarge and has made a full recovery.
Discussion
Stevens-Johnson syndrome has been well-documented as an extra-pulmonary manifestation of M pneumoniae infections. Stevens-Johnson syndrome was first described in 1922 and is characterised by erythematous target lesions on the skin and involvement of the oral mucosa, genitals and conjunctivae.1 Several cases have reported incomplete atypical presentations of Stevens-Johnson syndrome, primarily in children,2–4 which lack the typical rash, but retain oral, ocular and genital manifestations.5 Our case illustrates that incomplete presentation of this syndrome can occur with only oral mucosa and conjunctival lesions alone, without skin or genital involvement. Treatment of Stevens-Johnson syndrome remains supportive along with treating the underlying infection if recognised.
Learning points.
-
▶
Steven-Johnson syndrome is a well-documented extra-pulmonary manifestation of M pneumoniae infections.
-
▶
Atypical Steven-Johnson syndrome can present with only oral mucosa and conjunctival lesions alone, without the characteristic erythematous target skin lesions or genital involvement.
-
▶
Treatment of Steven-Johnson syndrome remains supportive along with treating the underlying pathology.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Stevens AM, Johnson FC. A new eruptive fever associated with stomatitis and ophthalmia; report of two cases in children. Am J Dis Child 1922;24:526–33 [Google Scholar]
- 2.Vanfleteren I, Van Gysel D, De Brandt C. Stevens-Johnson syndrome: a diagnostic challenge in the absence of skin lesions. Pediatr Dermatol 2003;20:52–6 [DOI] [PubMed] [Google Scholar]
- 3.Ravin KA, Rappaport LD, Zuckerbraun NS, et al. Mycoplasma pneumoniae and atypical Stevens-Johnson syndrome: a case series. Pediatrics 2007;119:e1002–5 [DOI] [PubMed] [Google Scholar]
- 4.Bullen LK, Zenel JA. Visual diagnosis: a 15-year-old female who has cough, rash, and painful swallow. Pediatr Rev 2005;26:176–81 [DOI] [PubMed] [Google Scholar]
- 5.Hillebrand-Haverkort ME, Budding AE, bij de Vaate LA, et al. Mycoplasma pneumoniae infection with incomplete Stevens-Johnson syndrome. Lancet Infect Dis 2008;8:586–7 [DOI] [PubMed] [Google Scholar]



