Abstract
Beginning January 1, 2000, Medicare extended coverage of immunosuppression medications from 3-years to lifetime based on age >65 years or disability. Using USRDS data for Medicare-insured recipients of kidney transplants between July 1995 and December 2000, we identified four Cohorts of Medicare-insured kidney transplant recipients. Patients in Cohort 1 were individuals who were both eligible and received lifetime-coverage. Patients in Cohort 2 would have been eligible, but their three-year coverage expired before lifetime-coverage was available. Patients in Cohort 3 were ineligible for lifetime-coverage because of youth or lack of disability. Patients in Cohort 4 were transplanted 1996–1996 and were ineligible for lifetime-coverage. Incomes were categorized by ZIP-code median household income from census data.
Lifetime-extension of Medicare immunosuppression was associated with improved allograft survival among low-income transplant recipients in the sense that the previously existing income-related disparities in graft survival in Cohort 2 were not apparent in Cohort 1. Ineligible individuals served as a control group; the income-related disparities in graft survival observed in the early Cohort 4 persisted in more recent Cohort 3. Multivariate proportional-hazards models confirmed these findings.
Future work should evaluate the cost-effectiveness of these coverage increases, as well as that of benefits extensions to broader patient groups.
Keywords: Medicare, insurance, outcomes, kidney graft survival, immunosuppression
Introduction
Patients with end-stage renal disease require renal replacement therapy through dialysis or kidney transplantation. In 1973, Medicare implemented lifetime-coverage of maintenance dialysis after a ninety-day waiting period [1]. Since the advent of cyclosporine, kidney transplantation has both improved quality of life and conferred a survival advantage when compared to long-term dialysis [2, 3]. To sustain allograft function, transplant recipients must take immunosuppressive medications for the life of the allograft. The high costs of these medications pose financial burdens, particularly among lower income recipients, that may lead to non-compliance and premature graft failure [4, 5]. An understanding of the relationships between patient access to immunosuppression benefits and graft outcomes is critical to the formulation of prudent reimbursement policies.
While patients with end stage renal disease became eligible for Medicare in 1972, the details of transplant patients' eligibility have changed over the years (Appendix Table). Since 1978, transplant recipients not eligible for Medicare because of their age or disability, have had their Medicare eligibility limited to three years post-transplant. Medicare's coverage of 80% of the costs of maintenance immunosuppression (IS) pharmaceuticals began in 1986, at which time only the first year after transplantation was covered. Between 1993 and 1995, Medicare gradually extended IS coverage to three years after transplant for all recipients. This policy change provided one quasi-experiment for assessing the impact of Medicare's immunosuppression benefits on graft survival. We previously demonstrated that during the years when Medicare's immunosuppression benefits expired after one-year, graft survival after one year among patients in the lowest three income quartiles fell below that of patients in the highest income group[5]. However during years with three-years of IS coverage, no disparities in income-related graft survival were observed. That income-related disparities seem to have been removed by the additional two-years of immunosuppression coverage was an initial indication that low income patient outcomes were adversely affected (compared to high income patients) by the expiration of coverage.
PL 106–113 (Medicare, Medicaid, and SCHIP Balanced Budget Refinement Act of 1999) and the Medicare Beneficiary Improvements and Protection Act sections of PL 106–554 (the Consolidated Appropriations Act of 2000) provided a second policy change that facilitates a retrospective analysis. In combination, these laws effectively extended lifetime-IS coverage to two groups of patients whose three-year immunosuppression coverage would have otherwise expired at the end of 1999. Transplant recipients aged 65 years or older on January 1, 2000 and those eligible for Medicare because they received Social Security Disability Insurance (SSDI) received this lifetime IS benefit. These two groups together represent 55 percent of the total transplants in 2002. Transplant recipients younger than age 65 when their three-year Medicare immunosuppression coverage expired and ineligible for SSDI received no additional coverage.
National data are now available to allow study of income-related disparities in five-year transplant outcomes among the first cohort potentially eligible for life-time immunosuppression benefits under the new Medicare rules. The current study explored linked records from the United States Renal Data System (USRDS) and the United States Census to describe the relationship between income and allograft survival over five years post-transplant, before and after the new Medicare rules. Our primary objective was to assess whether the latest expansion of Medicare coverage might also have reduced the previously existing income-related disparities in kidney allograft survival among patients eligible for long-term immunosuppression benefits.
Methods
Study Sample
Kidney transplant recipients were identified from historical data collected by the USRDS that incorporated information from the Organ Procurement and Transplantation Network (OPTN) registry and Medicare billing claims. The sample was limited to recipients of deceased donor organs primarily insured by Medicare. We defined patients with primary Medicare coverage as meeting two criteria: having at least $5,000 in institutional claims during the first 90 days and having at least $50 in physician/supplier claims during the first year following transplantation [5]. Recipients who had prior failed kidney transplants and recipients of multi-organ transplants were excluded.
The impact of Medicare's extended IS coverage was estimated by comparing outcomes among four cohorts defined by potential eligibility for the lifetime-IS coverage and actual transplant dates (Table 1). Cohort 1 included patients who were both “eligible” (over 65 at the expiration of the 3 years coverage or disabled) for the lifetime-coverage and who received their transplant in 1997 or later. Patients in Cohort 1 were the only group that actually received lifetime-coverage. Patients in Cohort 2 would have been “eligible” for the lifetime IS coverage, but were transplanted too early to receive it. Their three-year coverage expired before the new Medicare laws went into effect. Patients in Cohort 3 were transplanted recently enough (after 1996) to have IS coverage through 1/1/2000, but were “ineligible” for lifetime coverage because of their youth and lack of disability. Patients in Cohort 4 were both “ineligible” for lifetime-coverage and were transplanted too early.
Table 1.
Definitions of the Four Study Cohorts
| Reasons for Medicare Eligibility on 1/1/2000 | Transplant Date | |
|---|---|---|
| 1995 to 1996 | 1997 to 2000 | |
| Over 65 or Disabled | Cohort 2: “Eligible” but did not get lifetime coverage because their 3 years of immunosuppression coverage ended before 1/1/2000 | Cohort 1: “Eligible” and received lifetime - immunosuppression coverage after 1/1/2000 |
| End Stage Renal Disease, but younger than 65 and not disabled | Cohort 4: “Ineligible” | Cohort 3: “Ineligible” |
“Disability” is defined empirically as “unemployed due to disability” in the USRDS data set.
Estimated Income
To provide a proxy measure of each recipient's income, median household income according to the ZIP code in the 2000 US Census [6] was merged to the ZIP code of each patient's residence at transplant recorded in the USRDS. We were able to match income information to 6,780 (96.5%) of the 7,028 Medicare-financed, deceased donor kidney recipients sampled from transplants in 1995–1996, and to 17,810 (97.3%) of the 18,299 patients sampled in 1997–2000. Income quartile for each person in the study was determined by the quartile of the median family income of the recipient's ZIP code. The proportion of college-educated in each participant's ZIP code was considered as an additional measure of socioeconomic status apart from that associated with income category and race.
Outcome Measures
The primary outcome was renal allograft survival over five years, censored for death, as reported as a failure event or return to dialysis in the USRDS. Dates of death were as reported by the USRDS.
Statistical Analysis
We demonstrated the apparent impact of the Medicare's extended IS coverage both with Kaplan-Meier plots and with multivariate Cox Proportional Hazards regression estimates. Kaplan-Meier plots provide a graphical representation of income-related disparities between the highest and lowest quartiles over the five years post-transplant. These disparities were visually and statistically (log-rank test, P<0.05) apparent in the absence of Medicare's coverage of maintenance IS medications. The disparities were not apparent in the presence IS coverage. Observations were censored at the earliest of the following events: loss to follow-up, five years post-transplant, death, or end of study (December 31, 2005).
We used Cox Proportional Hazards regressions to examine the importance of access to IS benefits on graft survival in a model that controlled for a number of potential confounding factors. For reasons discussed in the Results section, the sample for this analysis included all study participants who survived with graft function to the second transplant anniversary. In the simple model without other significant confounding factors, risk ratios were estimated for variables representing: (a) the lowest quartile of recipient income; (b) exposure to year 2000 Medicare legislation based on transplant in 1997–2000 (regardless of characteristics qualifying for extended benefits); (c) characteristics conferring eligibility for extended immunosuppression benefits in the year 2000 legislation (regardless of year of transplant); and (d) the presence of all three factors together (the lowest income quartile, transplantation in 1997–2000, and eligibility characteristics. The full model included these same four variables and all confounding factors found to be significant (forward stepwise procedure with P<0.05) drawn from a list of recipient, donor and transplant factors as reported by the OPTN.
Results
Sample and baseline characteristics
We identified 35,030 patients who received kidney transplants from July 1995 to December 2000 with Medicare as the primary payer. Of these, 24,590 patients (73%) met complete enrollment criteria as first, single organ, deceased donor transplant recipients with sufficient ZIP Code data to be matched to the Census. Characteristics of each of the four Cohorts based on transplantation date and the presence of traits conferring eligibility for life-time immunosuppression by year 2000 legislation are shown in Table 2.
Table 2.
Baseline characteristics of the study samples according to patient characteristics defining eligibility for extended immunosuppression benefits and era of transplantation.*
| Variable | Eligibles, 1995–96 (N=3209) | Eligibles, 1997–2000 (N=8693) | P-value† | Ineligibles, 1995–96 (N=3571) | Ineligibles, 1997–2000 (N=9117) | P-value† |
|---|---|---|---|---|---|---|
| Recipient traits | ||||||
| Mean Age (years) | 51.34 | 53.21 | <0.001 | 42.91 | 43.71 | 0.001 |
| Male sex | 62.32 | 61.23 | 0.277 | 61.64 | 59.44 | 0.023 |
| Black race | 29.04 | 31.52 | 0.009 | 32.99 | 34.58 | 0.088 |
| College educated | 19.76 | 25.38 | <0.001 | 25.38 | 19.27 | <0.001 |
| Income quartile (Q) | ||||||
| Q1 | 26.77 | 26.08 | 0.448 | 24.67 | 26.08 | 0.102 |
| Q2 | 26.15 | 24.38 | 0.047 | 23.77 | 24.38 | 0.472 |
| Q3 | 24.49 | 24.24 | 0.774 | 23.41 | 24.24 | 0.325 |
| Q4 | 22.59 | 25.29 | 0.002 | 28.14 | 25.29 | 0.001 |
| Panel-reactive antibody >50% | 4.02 | 4.23 | 0.606 | 4.76 | 4.73 | 0.937 |
| Donor Traits | ||||||
| Age (years) | 36.12 | 37.49 | <0.001 | 34.50 | 35.62 | 0.002 |
| Male sex | 59.08 | 57.58 | 0.139 | 58.30 | 58.46 | 0.870 |
| Black race | 10.63 | 10.79 | 0.798 | 12.91 | 12.30 | 0.346 |
| Transplant factors | ||||||
| Number of HLA mismatches | 3.18 | 3.37 | <0.001 | 3.28 | 3.43 | <0.001 |
| Donor-recipient | ||||||
| CMV sero-pairing | ||||||
| Negative/negative | 11.44 | 9.06 | <0.001 | 12.80 | 10.69 | <0.001 |
| Negative/positive | 24.09 | 22.45 | 0.060 | 21.51 | 19.96 | 0.052 |
| Positive/negative | 17.67 | 12.70 | <0.001 | 20.33 | 15.81 | <0.001 |
| Positive/positive | 39.98 | 42.41 | 0.017 | 34.92 | 36.77 | 0.052 |
| Discharge immunosuppression | ||||||
| Cyclosporine | 64.38 | 60.06 | <0.001 | 61.72 | 58.73 | 0.002 |
| Tacrolimus | 9.26 | 27.87 | <0.001 | 8.01 | 27.00 | <0.001 |
| MMF | 37.21 | 71.47 | <0.001 | 36.07 | 68.62 | <0.001 |
| Delayed graft function | 32.02 | 38.17 | <0.001 | 27.53 | 35.92 | <0.001 |
Numbers are percentages unless otherwise noted. CMV, cytomegalovirus; HLA, human leukocyte antigen; MMF, mycophenolate mofetil.
Patient defined as eligible for life-time immunosuppression benefits were age ≥62 at time of transplant (and thus ≥65 at the three-year anniversary) or unemployed due to disability, regardless of time of transplant
P-value from Chi-square test or t-test comparisons of differences in trait distribution among eligible and ineligible patients within the indicated transplant era.
Kaplan-Meier Analysis: Patients “Eligible” for Medicare's Lifetime Benefit
The hypothesis that Medicare's lifetime IS coverage eliminated otherwise existing income-related disparities in graft survival is graphically supported by the 5-year Kaplan-Meier plots of graft survival. Among Cohort 2, the “eligible” individuals transplanted too early to receive the lifetime benefit, no substantial income-related disparities in graft survival were apparent through 1000 days (Figure 1). However, significant graft survival differences at the end of the 5th year post-transplant were apparent. Graft survival among the lowest income quartile (53.5%) was 5.44 percentage points lower than the graft survival among the highest income quartiles (58.96%), P=0.039. The 5.4% absolute difference in graft survival represents a 10.1% increase in the relative graft failure rate after 5 years.
Figure 1.
Kaplan-Meier Estimates of 5-year Graft Survival Among Medicare-extension “Eligible” Graft Recipients Stratified by Income Level and Era of Transplantation.
A) Patients who received Medicare's lifetime coverage (Cohort 1).
B) Patients transplanted too soon to qualify for Medicare's lifetime-coverage (Cohort 2). There was no difference in 5-year graft survival between the highest income quartile (Q4) shown in blue and the lowest income quartile (Q1) shown in black when patients received lifetime coverage but better allograft survival among higher income recipients when lifetime-coverage was not available, P=0.039.
In contrast, no income-related disparities existed among the “eligible” individuals transplanted recently enough to receive the lifetime coverage (Cohort 1). Five-year graft survival ranged from 59.07% for the second lowest income quartile to 60.00% for the highest income quartile, P=0.64.
Notably, the statistically significant income-related disparity in graft survival in Cohort 2 began during the third year post-transplant, during which Medicare's immunosuppression coverage was still available. First, income related differences in graft survival among Cohort 2 were not significantly different at either two or 3 years post transplant. But while the income-related differences in five-year graft survival were significant among the two-year survivors (76.3% versus 69.1%, P=0.003), they were not significantly different among the three-year survivors (81.0% versus 77.7%, p=0.166).
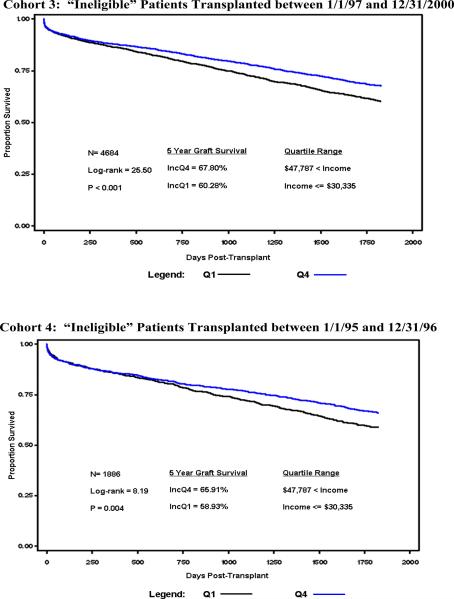
Kaplan Meier Analysis: Patients “Ineligible” for Medicare's Lifetime Benefit
Supporting our hypothesis, those patients ineligible for the lifetime benefit (Cohort 4) saw no reduction in the income-related disparities in graft survival. As with the “eligible” patients, there were income-related disparities in five-year graft survival before the policy change, (Figure 2). Five-year graft survival ranged from 58.9% for the lowest quartile to 65.9% for the highest income quartile, P=0.004. Importantly, income-related disparities continued among “ineligible” individuals after the policy change despite transplantation in a later era (Cohort 3). Five-year graft survival for the highest quartile was 67.8%, compared to was 60.3%, P<0.001 for the lowest quartile.
Figure 2.
Kaplan-Meier Estimates of 5-Year Graft Survival Among “Ineligible” Patients Stratified by Income Level and Era of Transplantation.
A) Patients transplanted after 1996 but ineligible for lifetime-coverage (Cohort 3).
B) Patients transplanted too soon to qualify for Medicare's lifetime coverage AND who were ineligible for lifetime coverage (Cohort 4).
The lifetime-coverage “ineligible” patients in the highest income quartile (Q4) shown in blue had better 5-year graft survival compared to those in the lowest quartile (Q1) shown in black whether they were in the early era, P<0.001, or later era, P=0.004.
The differences in income-related graft survival appeared before Medicare's immunosuppression coverage expired at the end of three years which was similar to the “eligible” Cohort before the benefits extension. Five-year graft survival among two-year survivors ranged from 75.2% in the lowest income quartiles to 81.0% in the highest quartile, P=0.001. Five-year graft survival among three-year survivors showed less variability, ranging from 81.9% in the lowest income quartile to 85.0% in the highest income quartile, P=0.13.
Multivariable Regression
Cox's regression analysis of graft survival at five years among two-year survivors demonstrated independent associations of both lower recipient income and “eligibility” with increased risk of graft loss (Table 2). In a simpler model without any variable representing donor, recipient or transplant characteristics, deceased donor transplant recipients in the lowest-income quartile (median household incomes by ZIP Code <$ 30,335) had a 36.2% additional relative increase in risk of graft failure when compared to those in the highest quartile (median household incomes by ZIP code > $47,787), P<0.001. When compared with “ineligible” individuals, “eligible” patients had a 31.6% additional higher risk of graft failure, P<0.001. Overall, the risk of graft failure did not differ significantly among transplants performed in 1997–2000 compared to those performed in 1995–1996, P=0.72. Low income individuals who were eligible for Medicare's immunosuppression coverage and who were transplanted during the years in which Medicare actually provided the lifetime immunosuppression coverage, Cohort 2, had 21.2% incremental reduction in the relative risk of graft failure compared to otherwise been expected, P=0.003. This risk reduction quantifies the estimated benefit of Medicare's lifetime immunosuppression extension in reducing income-related disparities in graft outcomes. In support, the joint hazard ratio that combined the effect of low income (Income Q1) with the effect of the extended IS coverage (IncomeQ1*Eligible*Post1997) was not significantly different from 1.00, P=0.29.
In the multivariate Cox proportional hazards model with adjustments for significant donor, recipient, and transplant characteristics, extended immunosuppression correlated with a 19.4%, P=0.009 incremental reduction in graft failures (Table 2). This compared to the 18.2%, P=0.003, greater graft failure associated with low income and the 20%, P=0.002, higher graft failure among “eligible” individuals. Controlling for transplants after 1997 was insignificant, P=0.57. Since the product of the “Income Q1” and the “IncomeQ1*Eligible*Post1997” hazard ratio was insignificantly different from 1.0, P=0.51, we concluded that Medicare's lifetime coverage of immunosuppression medications appears to have offset the income-related disparities in graft survival.
Discussion
Socioeconomic disadvantages, including low incomes, are associated with inferior health outcomes. At least a portion of income-related outcome disparities are thought to be driven by differential access to healthcare and medications. In the current study we examined whether the recent extension of Medicare immunosuppression benefits from three years to lifetime among kidney transplant recipients aged ≥65 years or disabled attenuated income-associated differences in long-term renal allograft survival.
We found that prior to enactment of Medicare's expansion of immunosuppression coverage, absolute decrements in five-year renal allograft survival among low- compared to high-income Medicare beneficiaries ranged from 5.4% in the elderly and disabled patients to 7.0% among the younger and non-disabled cohort. After enactment of the benefits extension, the discrepancy in graft survival persisted in the ineligible young and non-disabled, such that the five-year graft survival was 7.5% less among low versus high-income groups. In contrast, among patients eligible for lifetime immunosuppression benefits under the expanded policy, the five-year graft survival of the low income category was nearly equivalent to that of the high-income group.
These results are congruent with our prior study which used similar methodology to investigate the impact of extension of Medicare immunosuppression coverage from one-year to three-years regardless of patient characteristics [5]. In that analysis we found that low income was associated with a significant absolute 3.9% reduction in three-year graft survival when immunosuppression benefits expired after one-year, but that extension of benefits to three years for all Medicare-insured transplant recipients attenuated this disparity to a non-significant difference of <1%. After adjustment for potentially confounding recipient, donor and transplant characteristics, the expanded immunosuppression benefits were associated with a relative reduction in graft failure rates of 21%–27% in both the previous and in the present study. Only the introduction of cyclosporine in the 1980's has had as profound an impact on 3 and 5 year kidney transplant outcomes [7].
In both our current and earlier studies, income-related disparities in graft survival began to appear before Medicare's coverage of immunosuppression medications expired. In fact and as explained above, the income-related disparities at five years are only significant among patients with at least 2-year graft survival, not among patients with grafts that survived 3-years. While we have no information to test the hypothesis, we attribute this phenomenon the “hoarding behavior” patients might undertake as they see that the end of Medicare's immunosuppression coverage is approaching. Patients who put some of the immunosuppression medications aside to be used after Medicare's coverage has expired are effectively increasing noncompliance before the coverage expiration and therefore increasing their risk of graft failure.
Other studies have identified associations between low patient income and adverse outcomes in end-stage renal disease and transplantation. In a study conducted prior to the implementation of any Medicare reimbursement policy for maintenance immunosuppression, the need for financial assistance at the time of transplantation correlated with more than twice the incidence of return to dialysis after one year and five years compared to patients of “adequate” income in a mostly white transplant population [8]. In a registry analysis of 4,471 patients transplanted in the United States in 1990, patients with an estimated household income less-than or equal-to 20% below the federal poverty level had an absolute 10% decrement in 10-year graft survival compared to the most affluent kidney transplant recipients, but this was not independent of race in a multivariable regression model [9]. In a study of veterans whom receive medications without cost, African American race was an independent factor for poor transplant outcomes even when adjusted for a wide variety of donor and recipient factors. Income was not considered [10].
Maintenance of transplant function is the central goal of post-transplantation care. Kidney transplant loss increases the risk of multi-systemic complications including myocardial infarction, congestive heart failure, and death [11–13]. Thus, allograft failure is a catastrophic event in the life of a transplant recipient that incurs substantial human costs. The possibility of preventing allograft loss among financially disadvantaged patients supports the need for reimbursement policies to consider the impact of benefit extensions among broader segments of the transplanted population.
Our study is limited by the use of ZIP code median family income as a surrogate for individual recipient's income. However, resulting misclassification of individuals would be expected to be random and to bias the estimates of effects toward a null result, thereby weakening rather than confounding our observed findings. Further, we considered the availability of Medicare insurance benefits as a proxy measure of benefits utilization. The availability of other forms of insurance to some patients may underestimate the improvement in graft survival experienced among the subset that would be otherwise uninsured.
In conclusion, we found that lifetime extension of Medicare immunosuppression benefits is associated with attenuation of the disadvantages in allograft survival among low-income transplant recipients eligible for these benefits. Future work should evaluate the cost-effectiveness of these coverage increases and the implications of similar policy in other population segments aside from elderly and disabled patients. These and other analyses could benefit greatly from patient-specific information about income and/or employment in the USRDS data set.
Table 3.
Cox's regression analysis of deceased-donor graft survival at five years among two-year survivors (N= 9,320).
| Baseline Model | ||||
|---|---|---|---|---|
| Variable | Hazard Ratio | 95% Confidence Limits | P | |
| Income Q1 | 1.362 | 1.230 | 1.508 | <0.0001 |
| Eligible | 1.316 | 1.185 | 1.461 | <0.0001 |
| Post 1997 | 1.019 | 0.918 | 1.131 | 0.7202 |
| Income Q1*Eligible*Post 1997 | 0.788 | 0.675 | 0.921 | 0.0026 |
| Model Including Donor, Recipient, and Transplant Characteristics | ||||
|---|---|---|---|---|
| Variable | Hazard Ratio | 95% Confidence Limits | P | |
| Income Q1 | 1.182 | 1.057 | 1.322 | 0.0034 |
| Eligible | 1.200 | 1.069 | 1.348 | 0.0020 |
| Post 1997 | 1.033 | 0.925 | 1.153 | 0.5653 |
| Income Q1*Eligible*Post 1997 | 0.806 | 0.687 | 0.947 | 0.0086 |
| Black recipient | 1.639 | 1.489 | 1.804 | <0.0001 |
| College-educated recipient | 0.816 | 0.732 | 0.909 | 0.0002 |
| Male donor | 0.867 | 0.794 | 0.947 | 0.0016 |
| CMV donor +/ recipient + | 1.111 | 1.014 | 1.216 | 0.0232 |
| CMV donor +/ recipient − | 1.120 | 1.007 | 1.245 | 0.0365 |
| Tacrolimus at discharge | 0.837 | 0.748 | 0.937 | 0.0020 |
| Delayed graft function | 1.268 | 1.156 | 1.390 | <0.0001 |
CMV, cytomegalovirus; Q, quartile
Variables found to be insignificant in the regression included: recipient sex, body mass index, and panel-reactive antibody >50%; donor race, body mass index; number of HLA mismatches, CMV donor −/ recipient + sero-pairing; discharge cyclosporine, and discharge MMF.
Acknowledgments
The authors are indebted to the USRDS for their data. The interpretation and reporting of the data supplied by the USRDS are the responsibility of the authors and should in no way be seen as reflecting the official policy or interpretation of the U.S. government.
Portions of this work were supported by grants to the University of New Hampshire from Hoffman LaRoche, Inc. (2006), and from the Digestive and Kidney Diseases (NIDDK), DK59585 (2002 to 2004). D.C.B. received support from a grant from the NIDDK, P30DK079333. K.L.L. received support from a grant from the NIDDK, K08DK073036.
Funding Sources: Portions of this work were supported by grants to the University of New Hampshire from Hoffman LaRoche, Inc. (2006), and from the Digestive and Kidney Diseases (NIDDK), DK59585 (2002 to 2004). D.C.B. received support from a grant from the NIDDK, P30DK079333. K.L.L. received support from a grant from the NIDDK, K08DK073036.
Footnotes
Disclosures: No author has a commercial association that would pose a conflict of interest.
References
- [1].Rettig RA. Implementing the end-stage renal disease program of Medicare. Santa Monica, CA: [Accessed August 16, 2006]. Rand Report R-2505-HCFA/HEW, 1980. (at http://www.rand.org/pubs/reports/2005/R2505.pdf.) [Google Scholar]
- [2].Evans RW, Manninen DL, Garrison LP, Jr., Hart LG, Blagg CR, Gutman RA, et al. The quality of life of patients with end-stage renal disease. The New England Journal of Medicine. 1985;312:553–9. doi: 10.1056/NEJM198502283120905. [DOI] [PubMed] [Google Scholar]
- [3].Eggers PW. Effect of transplantation on the Medicare end-stage renal disease program. The New England Journal of Medicine. 1988;318:223–9. doi: 10.1056/NEJM198801283180406. [DOI] [PubMed] [Google Scholar]
- [4].Kasiske BL, Cohen D, Lucey MR, Neylan JF. Payment for immunosuppression after organ transplantation. American Society of Transplantation. JAMA. 2000;283:2445–50. doi: 10.1001/jama.283.18.2445. [DOI] [PubMed] [Google Scholar]
- [5].Woodward RS, Schnitzler MA, Lowell JA, Spitznagel EL, Brennan DC. Effect of extended coverage of immunosuppressive medications by medicare on the survival of cadaveric renal transplants. American Journal of Transplantation. 2001;1:69–73. doi: 10.1034/j.1600-6143.2001.010113.x. [DOI] [PubMed] [Google Scholar]
- [6].United States Census Bureau [Accessed September 27, 2006];Census 2000 Summary File 3. at http://www.factfinder.census.gov.
- [7].Hariharan S, Johnson CP, Bresnahan BA, Taranto SE, McIntosh MJ, Stablein D. Improved graft survival after renal transplantation in the United States, 1988 to 1996. The New England Journal of Medicine. 2000;342:605–12. doi: 10.1056/NEJM200003023420901. [DOI] [PubMed] [Google Scholar]
- [8].Kalil RS, Heim-Duthoy KL, Kasiske BL. Patients with a low income have reduced renal allograft survival. Am J Kidney Dis. 1992;20:63–9. doi: 10.1016/s0272-6386(12)80318-0. [DOI] [PubMed] [Google Scholar]
- [9].Press R, Carrasquillo O, Nickolas T, Radhakrishnan J, Shea S, Barr RG. Race/ethnicity, poverty status, and renal transplant outcomes. Transplantation. 2005;80:917–24. doi: 10.1097/01.tp.0000173379.53347.31. [DOI] [PubMed] [Google Scholar]
- [10].Chakkera HA, O'Hare AM, Johansen KL, Hynes D, Stroupe K, Colin PM, et al. Influence of race on kidney transplant outcomes within and outside the Department of Veterans Affairs. J Am Soc Nephrol. 2005;16:269–77. doi: 10.1681/ASN.2004040333. [DOI] [PubMed] [Google Scholar]
- [11].Lentine KL, Brennan DC, Schnitzler MA. Incidence and predictors of myocardial infarction after kidney transplantation. J Am Soc Nephrol. 2005;16:496–506. doi: 10.1681/ASN.2004070580. [DOI] [PubMed] [Google Scholar]
- [12].Lentine KL, Schnitzler MA, Abbott KC, Li L, Burroughs TE, Irish W, et al. De novo congestive heart failure after kidney transplantation: a common condition with poor prognostic implications. Am J Kidney Dis. 2005;46:720–33. doi: 10.1053/j.ajkd.2005.06.019. [DOI] [PubMed] [Google Scholar]
- [13].Rao PS, Schaubel DE, Jia X, Li S, Port FK, Saran R. Survival on dialysis post-kidney transplant failure: results from the Scientific Registry of Transplant Recipients. Am J Kidney Dis. 2007;49:294–300. doi: 10.1053/j.ajkd.2006.11.022. [DOI] [PubMed] [Google Scholar]