Abstract
Objective
To characterize pelvic floor injury after vaginal childbirth with serial MRI.
Methods
3T MR images were obtained early (1-month) and late (7-months) after childbirth in 19 women with risk factors for pelvic floor injury. All received multiplanar intermediate-weighted sequences and 11 had fluid sensitive sequences. MR images were evaluated for levator edema and tears, and pubic abnormalities.
Results
Three had unilateral high-grade tears, three had unilateral low grade tears, one had bilateral high and low-grade tears of the levator ani muscles. All tears were focal at the pubis. Levator edema was present in all on initial imaging and resolved at follow-up. Six had bone marrow edema; five with fracture line. None showed a pattern indicating nerve damage separate from muscle tears.
Conclusion
MRI showed focal levator ani muscle tears at the pubis with bone marrow edema and fracture in patients at risk for pelvic floor injury.
Introduction
It is well established that visible loss in the pubic portion of the levator ani muscles occurs in 10 to 20% of primiparous women after vaginal childbirth, in contrast to nulliparous women where no such abnormalities are found [1, 2]. Tremendous deformation occurs during childbirth with certain levator ani muscle fibers stretching up to 3.3 times their normal length[3] . Women with known pelvic organ prolapse are more likely (53% vs. 16% for normal controls) to show this same pattern of levator ani injury [4]. Competing hypotheses about injury mechanism are unresolved and include 1) excessive muscle stretch [3] vs. 2) nerve injury [5] vs. 3) compression from the baby’s head resulting in ischemia and reperfusion injury [6].
The ability to test these hypotheses rests on advancements in imaging that allows assessment for soft tissue injury with high spatial and contrast resolution. For example, edema as a sign of trauma can be observed as increased signal intensity on MR images when fluid sensitive scanning techniques are used. The anatomical tissue involved and imaging pattern (“focal or diffuse” and “normal or abnormal tissue architecture”) can indicate injury extent and location of injury. Accurate assessment of pelvic floor injury may help explain patient symptoms and potentially guide future treatment options.
In this study, we imaged women that had risk factors for levator ani injury during vaginal childbirth approximately 1 month and 7 months post partum with MRI to assess for pelvic floor abnormalities. We tested the hypotheses that signal changes would be observed in the levator ani consistent with 1) muscle stretch injury with tear, 2) major nerve injury and/or, 3) compression-related injury.
Materials and Methods
Institutional Review Board approval was obtained. Birth records were reviewed to identify women with possible pelvic floor injury after their first vaginal childbirth. Risk criteria included forceps or vacuum delivery, anal sphincter laceration, prolonged second stage of labor [2], precipitous delivery or shoulder dystocia [7]. Women were invited prior to hospital discharge to be telephoned for full screening. Informed consent was obtained and participants were compensated for their time.
The women were studied by MRI early after childbirth (mean ± SD: 29.4 ± 8.7 days after birth) and again around 7 months (mean 207.9 ±14.3 days after birth). The initial imaging time point was selected to allow resolution of non-specific soft tissue edema related to childbirth. The second time point was selected because healing was expected to be complete by then. MR imaging (3 Tesla, Philips Achieva, Philips Medical Systems, The Netherlands; 8 channel cardiac coil positioned over the pelvis) included coronal, axial, and sagittal proton density–weighted (TR/TE = 2100–2500/30 msec) sequences (field-of-view = 20 cm; 256 × 25 matrix, number of signal averages 2; and slice thickness/gap = 4 mm/1 mm). For the last 11 participants additional 2 mm sections with 0.2 mm gap in the axial and coronal planes were obtained with proton density-weighted sequences (TR/TE = 2100–2500/30) and with either proton density-weighted fat saturation (TR/TE = 2355/30) or STIR (TR/TE = 5987/60) sequences (FOV = 18cm, 256 × 256 matrix, number of signal averages 2). No intravenous contrast was given.
The MRI studies were reviewed, using the standard monitor of the PACS system, by two board-certified radiologists (CB, JJ) with fellowship-training in musculoskeletal imaging with differences resolved by consensus. They assessed both the levator ani and adjacent osseous structures blinded to obstetric factors.
The levator ani were assessed for tear by recording absence of the muscle fibers in at least one 4 mm section or two or more adjacent 2 mm sections in both axial and coronal planes. Each side of the muscle was graded separately. Subtle tears were defined as equivocal muscle fibers loss. Low-grade partial tears were defined muscle fiber loss less than 50%. High-grade tears were greater than 50% fiber loss, while complete tears were only noted if no residual fibers remained in either the axial or coronal planes for the entire thickness of the pubic portion of the levator ani. This standard musculoskeletal radiology grading system for tears is a minor adaptation from previous publications on the levator ani, which relied on investigators outside of the musculoskeletal field, [1, 4].
The levator ani muscles were also evaluated for fluid signal on MR images, defined as increased or isointense signal in comparison to other visible musculature. The location of the increase signal was also described as diffuse or focal, and if focal the location was noted.
Presence of increased signal within the pubic bone compared to the ischial tuberosity was also recorded on either proton density-weighted fat saturation or STIR MR images in the last 11 women. Presence and location of the bone marrow increased signal and that of the fracture line (linear low signal on MRI) were noted.
The MRI data were summarized as simple counts of observations on type and severity levels of injury and recovery from injury. Patient records were reviewed for additional clinical information.
Results
A total of 19 women were recruited with a mean age of 28 years (range; 22 – 35). Participants demonstrated obstetrical factors of anal sphincter laceration (n = 13), lengthy second stage of labor (n = 4), precipitous delivery (n = 1), and infant shoulder dystocia (n= 1). Although vacuum/forceps assisted delivery has been identified as a risk factor for levator ani injury [1] we were unable to recruit participants with this particular risk factor. All 19 women completed the initial MRI (one month after delivery) and 16 completed the follow-up MRI (7 months after delivery).
Of the 19 women, 53% (10/19) had no tear (Fig. 1), 16% (3/19) had high-grade tear on one side and contralateral subtle tear (Fig. 2), 11% (2/19) had low-grade tear and contralateral subtle tear (Fig. 3), 5% (1/19) had high-grade tear and contralateral low-grade tear, 5% (1/19) had low-grade tear and no contralateral tear, 5% (1/19) had bilateral subtle tears, and 5% (1/19) had subtle tear and no contralateral tear. All tears were located in the anterior fibers at or near their insertion along the posterior cortex of the pubis.
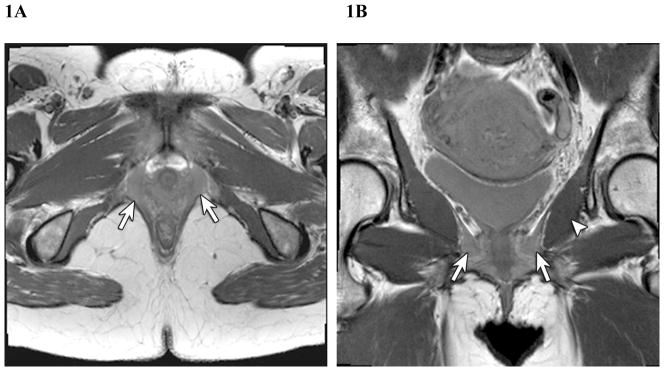
Fig. 1.
33-year-old woman 3 weeks after delivery with no tears but bilateral levator ani muscle edema (arrows) seen on proton density-weighted sequences in the axial (1A) and coronal (1B) planes. Note normal obturator internus muscle signal (arrowhead).
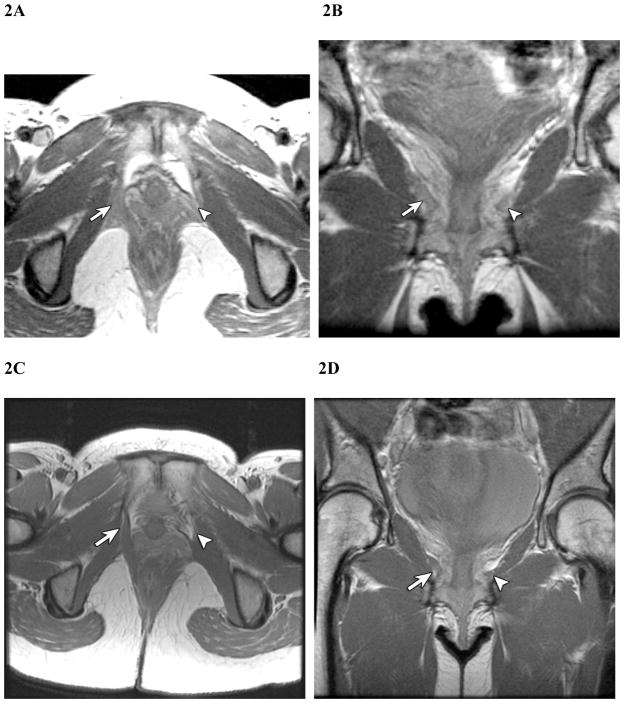
Fig. 2.
35-year-old woman 3 weeks (A, axial and B, coronal) and 6 months (C,D) after delivery with high grade left levator ani tear (arrowhead) and contralateral subtle right levator ani tear (arrow). Note interval decreased edema of levator ani muscles on proton density-weighted images (TR/TE, 4,000/30).
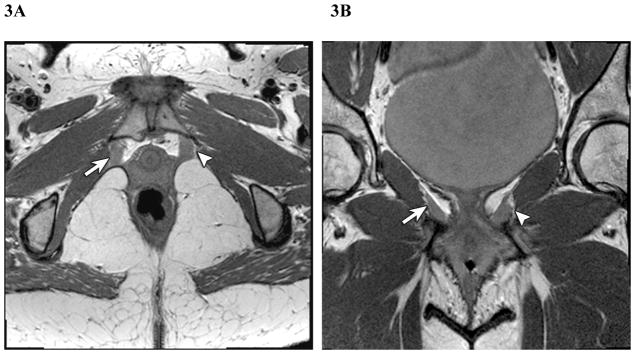
Fig 3.
35-year-old woman 3 weeks after delivery with low grade right levator ani tear (arrow) and subtle left levator ani tear (arrowhead) in the axial (3A) and coronal (3B) planes.
Of the 16 women with follow-up MRI, two showed interval resolution of the MRI findings; neither one had high-grade tears in the early scan. The remaining muscle tears were more conspicuous on the follow-up MRI studies. In all other subjects with tears, there was no change in the MRI grading between initial and follow-up MRI.
With regard to levator ani signal intensity, 100% (19/19) of patients imaged had foci of increased signal in the levator ani relative to the adjacent obturator internus on the initial MRI (Fig. 1) with the highest signal seen in the anterior fibers. The obturator internus muscle did not show increased signal relative to other muscles in the region. Of the 16 women with follow-up MRI, all had resolution of the increased signal involving the levator ani.
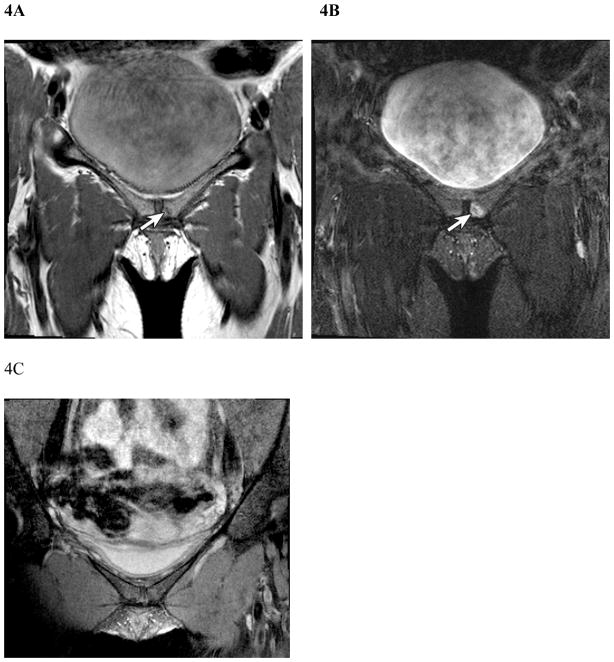
With regard to pubis abnormalities, 55% (6/11) of participants imaged with fat saturation or STIR sequences had focal bone marrow edema along the posterior cortex on the initial MRI, bilateral in 33% (2/6) and unilateral in 67% (4/6). Of the two participants with bilateral bone marrow edema, LA tears were graded as low-grade and no tear in one subject, and high-grade and subtle tear in the other subject. Of the four participants with unilateral bone marrow edema, one had a high grade tear on the contralateral side, the others had subtle or low grade tears on one or both sides. Fracture lines involving the subcortical regions of the pubis were identified in 46% (5/11) of subjects; the fracture lines were unilateral in four and bilateral in one subject (Fig. 4). All of the fractures resolved by late scan. On follow-up MRI, there was interval resolution of bone marrow edema in 83% (5/6) of the participants who had bone marrow edema on the initial MRI.
Fig 4.
28-year-old woman 4 weeks after delivery with a subcortical fracture along the left posterior pubic cortex (arrows) with proton density-weighted sequence (4A) and same plane with proton density-weighted fat saturated sequence (4B). Note resolution of fracture line in 4C at 6 months after delivery.
Clinical symptoms were compared between those with normal MRI results (10), those with high grade tears (4), and those with low grade or subtle tears (5). No patients in any group described pelvic pain. Bowel dysfunction was present in one patient who had no levator ani tear. Urinary leakage was present in three subjects, one with normal MRI, one with high grade tear, and one with low grade tear.
Discussion
In this study, certain women at higher risk for levator ani injury demonstrated: 1) levator ani muscle fibers torn from their origin at the pubic bone, 2) focal levator ani edema, 3) focal bone marrow edema, and 4) pubic bone fracture. These injury indicators occurred uniquely or in conjunction with each other. There were no indicators of a primary neurological or simple compression injury.
The location of abnormalities focally at the pubis on MRI, often in association with bone marrow edema, supports tear of the pubic portion of the levator ani fibers as the primary injury mechanism for pelvic floor injury after vaginal delivery. This pattern of muscle tearing occurs in the same region as the muscle defects seen in women with pelvic organ prolapse [4] and is predicted by computer-simulated models of vaginal birth [3]. Muscles in general are most vulnerable to tears at the myotendinous junction [8, 9]. Tearing at the myotendinous junction is readily demonstrated by MRI where findings correlate with degree of tissue damage [9, 10]. In contrast, none of the participants showed signal intensity changes to the obturator internus muscle or increased edema in the fat adjacent to the obturator internus, as would be indicative of primary crush injury.
There are a number of findings that suggest nerve injury may not be the primary mechanism of pubic levator ani trauma in our participants. Traumatic neuropathy, shown in other non-birth related musculoskeletal injuries, is seen with muscle changes 5 days after nerve injury [11]. No anatomically intact levator ani demonstrated a pattern of diffuse increased signal intensity throughout the muscle on early MR images and then volume loss on final scan, as would be expected if denervation were the primary injury mechanism. If severe nerve damage had occurred one could expect diffuse atrophy or possibly fatty infiltration when observed on late, compared to early, MR scans throughout all muscles previously innervated [10, 11]. The soft tissue trauma that results in most any muscle fiber tear logically could involves nerve injury as well. Further investigation in a larger patient population is needed to resolve the possible injury mechanisms.
Of interest is the distribution of levator ani and pubis abnormalities on MRI in our participants. Bone marrow edema of the pubis was identified bilaterally in two participants and in a unilateral distribution in four. A subcortical fracture line was seen in five of these six participants with no clear association to grade or side of levator ani tear. Given the small sample size, further investigation with a larger population is needed to fully characterize location of marrow edema and fracture, association with specific levator ani tear site and grade, as well as association with other clinical findings.
Study limitations include selection bias as only those participants at risk for pelvic floor injury were included; however, imaging of this population allowed us a larger pool of injuries to characterize. Lack of a control group is another relative limitation, although the normal appearance the levator ani muscle in nulliparous women has been described [1]. Another limitation is lack of standard of reference for grading of levator ani tears on MRI in the radiology literature. We attempted to strengthen the study by applying the principles of muscle imaging with MRI to the levator ani, using fluid sensitive scans in the last 11 women, and consensus interpretation by experienced musculoskeletal radiologists. Our current imaging protocol now consists of the following parameters: coronal, axial, and sagittal proton density weighted images (TR/TE, 2,107/30; slice thickness, 4 mm; gap, 1 mm) and coronal and axial proton density–weighted images (TR/TE, 2,107/30; slice thickness, 2 mm; gap, 0.2 mm) with and without fat saturation.
In summary, this study supports the value of utilizing musculoskeletal imaging techniques and the hypothesis that the primary mechanism of pelvic floor injury with childbirth is levator ani muscle tear at the pubic bone as shown on MRI. Further investigation using a larger patient population is needed to confirm these preliminary results.
Acknowledgments
*Supported by the National Institute of Health grant: R21 HD049818 P50HD044406
References
- 1.DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101:46–53. doi: 10.1016/s0029-7844(02)02465-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005;106:707–712. doi: 10.1097/01.AOG.0000178779.62181.01. [DOI] [PubMed] [Google Scholar]
- 3.Lien KC, Mooney B, DeLancey JO, Ashton-Miller JA. Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol. 2004;103:31–40. doi: 10.1097/01.AOG.0000109207.22354.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeLancey JO, Morgan DM, Fenner DE, et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol. 2007;109:295–302. doi: 10.1097/01.AOG.0000250901.57095.ba. [DOI] [PubMed] [Google Scholar]
- 5.Weidner AC, Jamison MG, Branham V, South MM, Borawski KM, Romero AA. Neuropathic injury to the levator ani occurs in 1 in 4 primiparous women. Am J Obstet Gynecol. 2006;195:1851–1856. doi: 10.1016/j.ajog.2006.06.062. [DOI] [PubMed] [Google Scholar]
- 6.Conner E, Margulies R, Liu M, Smilen SW, Porges RF, Kwon C. Vaginal delivery and serum markers of ischemia/reperfusion injury. Int J Gynaecol Obstet. 2006;94:96–102. doi: 10.1016/j.ijgo.2006.04.039. [DOI] [PubMed] [Google Scholar]
- 7.Kearney R, Miller JM, Ashton-Miller JA, DeLancey JO. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet Gynecol. 2006;107:144–149. doi: 10.1097/01.AOG.0000194063.63206.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benjamin M, Toumi H, Ralphs JR, Bydder G, Best TM, Milz S. Where tendons and ligaments meet bone: attachment sites ('entheses') in relation to exercise and/or mechanical load. J Anat. 2006;208:471–490. doi: 10.1111/j.1469-7580.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Connell DA, Schneider-Kolsky ME, Hoving JL, et al. Longitudinal study comparing sonographic and MRI assessments of acute and healing hamstring injuries. AJR Am J Roentgenol. 2004;183:975–984. doi: 10.2214/ajr.183.4.1830975. [DOI] [PubMed] [Google Scholar]
- 10.May DA, Disler DG, Jones EA, Balkissoon AA, Manaster BJ. Abnormal signal intensity in skeletal muscle at MR imaging: patterns, pearls, and pitfalls. Radiographics. 2000;20(Spec No):S295–315. doi: 10.1148/radiographics.20.suppl_1.g00oc18s295. [DOI] [PubMed] [Google Scholar]
- 11.Bendszus M, Stoll G. Technology insight: visualizing peripheral nerve injury using MRI. Nat Clin Pract Neurol. 2005;1:45–53. doi: 10.1038/ncpneuro0017. [DOI] [PubMed] [Google Scholar]