Abstract
Objective
To examine the effect of the transition to adulthood on financial and non-financial barriers to care in youth with asthma.
Study design
With National Health Interview Survey data from 2000 to 2005, we examined delays and unmet needs because of financial and non-financial barriers, evaluating the effect of adolescent (age, 12–17 years; n = 1539) versus young adult age (age, 18–24 years; N = 833), controlling for insurance, usual source of care, and sociodemographic characteristics. We also simulated the effects of providing public insurance to uninsured patients and a usual source of care to patients Without one.
Results
More young adults than adolescents encountered financial barriers resulting in delays (18.6% versus 8%, P < .05) and unmet needs (26.6% versus 11.4%, P < .05), although delays caused by non-financial barriers were similar (17.3% versus 14.9%, P = not significant). In logistic models young adults were more likely than adolescents to report delays (odds ratio [OR], 1.45; 95% CI, 1.02–2.08) and unmet needs (OR, 1.8; 95% CI, 1.29–2.52) caused by financial barriers.
Conclusions
Delays and unmet needs for care caused by financial reasons are significantly higher for young adults than they are for adolescents with asthma.
Assuring uninterrupted access to care for youth with chronic conditions as they age into adulthood is a priority issue for policy makers and clinicians.1–4 Despite increasing attention, it appears that few adolescents are receiving services to foster a successful transition.5 Considerable attention has been directed toward the role of insurance and having a usual source of care in assuring access to health care services for young adults.6–10 Becoming an adult dramatically reduces an individual's eligibility for public health insurance programs, such as Medicaid, and it also marks a time when a young adult may no longer be eligible as a dependent in a family's private health insurance plan. As a result of these issues, adults aged 19 to 24 years have the lowest rates of health insurance coverage of any age group in the United States.11 Many youth age out of pediatric care or move away, finding themselves without care or changing their source of care. Although most adolescents with special health care needs have a usual source of care, many young adults, even those with disabilities, do not.12 Finding an adult-oriented health care provider for youth during the transition is frequently identified as a barrier to care.13
We could find no studies that focus on the unmet needs and access to care for youth with asthma as they transition to adulthood. This lack of attention is striking for 2 reasons. First, asthma is among the most prevalent serious chronic conditions. Second, the need for ongoing primary care and asthma-specific monitoring is highlighted in current practice guidelines.14 The purpose of this analysis is 3-fold: First, we examine health care access in adolescents and young adults with asthma; second, we model whether young adults with asthma are more likely than adolescents with asthma to experience delays and unmet needs for care because of financial and non-financial barriers net of health insurance coverage, having a usual source of care, and other sociodemographic characteristics; and finally, we simulate a counter-factual situation in which all adolescents and young adults with asthma who are uninsured are actually enrolled in public health insurance coverage and those without a usual source of care are provided with one to estimate the impact of these access barriers on unmet need due.
METHODS
Data Source and Study Population
We used public use data from the National Health Interview Survey (NHIS) for these analyses.15 The NHIS is an annual household survey conducted by the National Center for Health Statistics (NCHS) to provide data on the health and health care use of the non-institutionalized US population. Data from the years 2000 to 2005 were pooled to form a sample of 26,597 adolescents (age, 12–17 years) and 19,998 young adults (age, 18–24). The NHIS is comprises several component questionnaires. For these analyses, we included data from the person, household, sample child, and sample adult questionnaires. The respondents for the adolescents were most often a knowledgeable adult in the household, whereas young adults generally responded for themselves. Response rates range between 79% and 81% for the sample child survey (adolescents) and between 69% and 74% for the adult samples across the individual years of the surveys. Sample weights provided by the NCHS account for non-response and allow for generalization from the sample to the overall US population.
The study population for these analyses is adolescents and young adults who report having asthma. Subjects were identified as having asthma by an affirmative response to both questions: “Have you (the subject) ever been told by a doctor or other health professional that you had asthma?” and “During the past 12 months, have you had an episode of asthma or an asthma attack?” Together these questions identify those adolescents and young adults with asthma for whom ongoing medical care is particularly important.
Measures
Outcome variables
Subjects were classified as having delayed care because of financial barriers when during the previous 12 months he or she had delayed seeking medical care because of concerns about its affordability. Similarly, an unmet need because of a financial barrier was identified when during the previous 12 months the respondent indicated that he or she had failed to receive needed medical care or prescription medication because of being unable to afford it. Delayed care because of a non-financial barrier was identified by a positive response to any of 5 questions about having delayed care because of being unable to get through on the phone, being able to get an appointment soon enough, having to wait too long to see the doctor, the office not being open at convenient time, or not having transportation.
Predictor variables
The predictor variables are derived from the extensive theoretical and empirical literature about access to care.16–18 The primary predictor of interest was whether the subject was an adolescent or young adult. We chose the age of 18 to differentiate the 2 groups because it represents the age of majority status, and it is also the time when eligibility rules for insurance coverage begin to change. We tested our findings about the sensitivity of this choice of age. Insurance status was categorized as having public or private insurance or being uninsured. A usual source of care was identified as a place where the subject usually goes when he/she is sick or needs advice about health and that this place is a clinic, office, or outpatient department. Health status was dichotomized into “at least very good health” for ease of interpretation from a 5-category reported health status measure. Race/ethnicity and poverty status (≤200% of the federal poverty level versus >200% of the federal poverty level) were categorized by NCHS. When data were missing for poverty status or Hispanic origin, the NCHS-imputed values were used.
Analyses
We generated descriptive statistics and bivariate comparisons in the form of frequencies and proportions of adolescents and young adults. We ran logistic regression models to assess the association between being an adolescent or young adult and each dependent variable and included health insurance coverage, having a usual source of care, health status, and other demographic variables as important control variables. Finally, we simulated the hypothetical impact of providing public health insurance coverage to respondents who reported being uninsured and having a usual source of care to respondents without one on each outcome variable while adjusting for the other measured potential confounders. We used the coefficients from the logistic regression models to calculate the predicted probability of each outcome for each individual. Then for the subjects without health insurance, we recalculated their predicted probability for each outcome as if they had insurance. We also completed the same procedure for subjects not having a usual source of care. In these simulations, all other characteristics of the persons (eg, poverty, race, sex) remain unchanged. The sample mean for the predicted probabilities in each situation (using observed insurance status or the simulated status) is the population rate for the outcome. This form of counterfactual modeling provides the predicted population effects of an intervention. In contrast, the odds ratio (OR) from a logistic regression provides an estimate of the effect of a characteristic for an subject with otherwise “average” characteristics. A large or small OR may represent a powerful effect for an individual, but in the case in which the characteristic is rare, any intervention that changes the characteristic may have a very small population effect. Thus, these simulations complement the typically presented regression results. Simulations were conducted only for the outcomes associated with financial barriers because the results of the logistic regression caused by non-financial barriers demonstrated no significant contribution of age.19 All analyses were conducted with STATA software version 9.1 (College Station, TX), applying sample weights and using procedures to adjust for the complex sample design.20 This study was approved by the institutional review board at the University of Minnesota.
RESULTS
Overall, 5.7% of adolescents (95% CI, 5.4–6.1) and 4.2% of young adults (95% CI, 3.8–4.5) were identified as having asthma, with an episode or attack in the previous 12 months. The lower prevalence found in young adults is caused primarily by a rate in young adult men that is much lower than that in adolescent boys (3.2 % versus 6.2 %; P < .05). In female subjects, the rate of asthma did not differ significantly between the young adults and adolescents (5.2 % versus 5.3 %; P = not significant). These findings are consistent with the recognized natural history of asthma.21 Young adults with asthma were much more likely than adolescents with asthma to be uninsured (26.7 % versus 7.9 %; P < .05) and to lack a usual source of care (19.9 % versus 5.2%; P < .05; Table I).
Table 1.
Characteristics of adolescents and young adults with asthma in the United States, 2000 to 2005
| Adolescents (n = 1,539) |
Young adults (n = 833) |
|||
|---|---|---|---|---|
| % | (SE) | % | (SE) | |
| Sex | ||||
| Female | 45.1% | (1.6) | 62.9% | (2.2) |
| Race/Ethnicity | ||||
| Hispanic | 13.9% | (1) | 9.4% | (1.1) |
| Caucasian, non-Hispanic | 63.9% | (1.4) | 72% | (1.9) |
| Black,non-Hispanic | 18.3% | (1.2) | 14.4% | (1.4) |
| Other, non-Hispanic | 3.9% | (0.6) | 4.2% | (0.9) |
| Region | ||||
| Northeast | 19.9% | (1.2) | 20.1% | (2.1) |
| Midwest | 24.1% | (1.5) | 29.2% | (2.1) |
| South | 34.7% | (1.5) | 31.5% | (2.1) |
| West | 21.3% | (1.4) | 19.1% | (1.6) |
| Reported health status | ||||
| Excellent or very good | 62.4% | (1.4) | 56.1% | (2) |
| Good, fair, or poor | 37.6% | (1.4) | 43.9% | (2) |
| Poverty level | ||||
| <200% | 39.7% | (1.6) | 48.7% | (2.3) |
| Usual source of care | ||||
| No | 5.2% | (0.7) | 19.9% | (1.7) |
| Health insurance | ||||
| Public | 24.9% | (1.5) | 16.6% | (2.3) |
| Private | 67.1% | (1.9) | 56.8% | (1.9) |
| Not covered | 7.9% | (0.9) | 26.7% | (1.9) |
Source: National Health Interview Survey.
Pooled data from 2000–2005.
Adolescent age, 12–17 years; young adults age, 18–24 years.
Sample n is unweighted; percentages are weighted, and SE reflects complex sampling design.
The bivariate relationships between the outcomes, age category, insurance coverage, having a usual source of care, and sociodemographic characteristics for youth with asthma are presented in Table II (available at www.jpeds.com). Delays and unmet needs for care caused by financial barriers were reported more frequently for young adults than for adolescents, and delays caused by non-financial barriers were not significantly different in age categories. Young adults were more likely to experience financial barriers resulting in either delays or unmet needs for care than were adolescents across all predictors and sociodemographic categories. An attenuated pattern was observed for delayed care caused by non-financial barriers.
Table II.
Characteristics of adolescents and young adults with asthma by reason for delayed or unmet needs for care for youth with asthma in the United States, 2000 to 2005
| % reporting delays because of financial barriers |
% reporting unmet need because of financial barriers |
% reporting delays because of non-financial barriers |
||||
|---|---|---|---|---|---|---|
| Adolescents % (SE) | Young adults % (SE) | Adolescents % (SE) | Young adults % (SE) | Adolescents % (SE) | Young adults % (SE) | |
| Overall | 8% (0.9) | 18.6% (1.6)* | 11.4%(l) | 26.6% (1.9)* | 14.9% (1.2) | 17.3% (1.5) |
| Sex | ||||||
| Female | 9% (1.4) | 18.8% (1.9)* | 12.7% (1.6) | 28.7% (2.3)* | 15.2% (1.6) | 19.9% (2.1) |
| Male | 7.1% (1.1) | 18.3% (2.8)* | 10.2% (1.2) | 23.3% (3.2)* | 14.6% (1.6) | 13% (2.5) |
| Race/Ethnicity | ||||||
| Hispanic | 8.4% (2.2) | 13.5% (3.3) | 17.1% (2.7) | 24.1% (4) | 19.6% (3) | 15.1% (3.1) |
| Caucasian, non-Hispanic | 7.3% (1.1) | 19.1% (2)* | 10.1%(1.1) | 26.8% (2.4)* | 14.5% (1.5) | 17.5% (2) |
| Black,non-Hispanic | 10.5% (2.2) | 19.9% (4.2)* | 12.9% (2.5) | 30.1% (5)* | 12.9% (2.4) | 16.8% (3.7) |
| Other, non-Hispanic | 6.2% (4.4) | 17.1% (7.1)* | 3.9% (2.8) | 15.7% (9.3) | 13.3% (5.9) | 20.5% (6.7) |
| Region | ||||||
| Northeast | 7% (1.8) | 10.8% (2.5) | 8.5% (2.2) | 15.0% (3.3) | 9.6% (2.3) | 12.3% (3.5) |
| Midwest | 7.1% (2) | 16.2% (2.5)* | 10.7% (2.2) | 27.9% (3.7)* | 15.3% (2.6) | 17.2% (2.8) |
| South | 9.3% (1.4) | 24.6% (3.5)* | 15.5% (1.9) | 34.3% (3.9)* | 15% (1.8) | 21.3% (3) |
| West | 7.7% (2.1) | 20.7% (3.1)* | 8% (1.6) | 24.6% (3.6)* | 19.1% (2.6) | 16.1% (3) |
| Reported health status | ||||||
| Excellent/very good | 4.6% (0.9) | 14.6% (1.9)* | 7.5% (1) | 20.9% (2.3)* | 12.5% (1.4) | 15% (2.1) |
| Good, fair, or poor | 13.6% (1.8) | 23.6% (2.6)* | 17.8% (2) | 34% (2.9)* | 18.8% (2) | 20.2% (2.3) |
| Poverty level | ||||||
| Under 200% | 12.1% (1.8) | 26% (2.5)* | 18.9% (1.9) | 32.6% (2.8)* | 21.6% (2.3) | 16.3% (2.5) |
| At or over 200% | 5.3% (0.8) | 11.3% (1.9)* | 6.4% (1.1) | 20.8% (2.5)* | 10.4% (1.2) | 16.3% (1.8) |
| Usual source of care | ||||||
| No | 23.9% (5.1) | 39.2% (4.1)* | 30.5% (5.9) | 49.1% (4.1)* | 19.1% (5.2) | 15.5% (3) |
| Yes | 7.1% (0.9) | 13.6% (1.6)* | 10.3% (1) | 21.3% (2)* | 14.6% (1.2) | 18.2% (1.8) |
| Health insurance | ||||||
| Public | 8.1 (1.8) | 16.1 (3.8)* | 18.4 (2.2) | 27.8 (4.8) | 23.2 (2.8) | 17.5 (3.6) |
| Private | 4.7 (0.8) | 10.5 (1.5)* | 6.1 (0.9) | 14.6 (1.9)* | 11.7 (1.4) | 16.6 (2.2) |
| Not covered | 35.4 (5.7) | 38.1 (3.9) | 33.9 (5.3) | 52.1 (4)* | 15.7 (4.1) | 18.8 (2.7) |
Source: National Health Interview Survey.
Pooled data from 2000–2005.
Adolescents age 12–17 years, young adults age 18–24 years.
Sample percentages are weighted and SE reflects complex sampling design.
Comparison between adolescents and young adults P < .05 by logistic regression.
The independent effects of age, insurance coverage, having a usual source of care, and the sociodemographic characteristics on each of the outcomes were evaluated with logistic regression (Table III). Young adults were more likely to report delays and unmet needs in care because of financial barriers than were adolescents after controlling for other significant predictors of access, including insurance, having a usual source of care, health status, and sociodemographic characteristics. In the model evaluating delays caused by non-financial barriers neither age, insurance, or having a usual source of care was significantly associated with the outcome. Using an alternative age cutoff point did not substantially alter our findings.
Table III.
Regression results of models predicting delays and unmet needs for care for youth with asthma: 2000 to 2005
| Delayed care because of financial barriers |
Unmet needs because of financial barriers |
Delayed care because of non-financial barriers |
|
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | |||
| Adolescent | Reference | Reference | Reference |
| Young adult | 1.45* (1.02–2.08) | 1.8* (1.29–2.52) | 1.13 (0.82–1.54) |
| Insurance | |||
| Uninsured | Reference | Reference | Reference |
| Public | 0.23* (0.13–0.29) | 0.37* (0.24–0.58) | 0.86 (0.56–1.33) |
| Private | 0.24* (0.15–0.39) | 0.19* (0.13–0.29) | 0.86 (0.56–1.33) |
| Usual source of care | |||
| No | Reference | Reference | Reference |
| Yes | 0.41* (0.26–0.66) | 0.41* (0.28–0.61) | 1.16 (0.71–1.92) |
| Sex | |||
| Female | Reference | Reference | Reference |
| Male | 0.71* (0.51–0.99) | 0.62* (0.45–0.85) | 0.8 (0.59–1.09) |
| Race/Ethnicity | |||
| Caucasian, non-Hispanic | Reference | Reference | Reference |
| Black, non-Hispanic | 0.73 (0.45 1.18) | 0.69 (0.44 1.08) | 0.72 (0.49–1.07) |
| Hispanic | 0.58 (0.34–1.01) | 0.96 (0.65–1.41) | 0.92 (0.7–1.4) |
| Other, non-Hispanic | 0.51 (0.18–1.43) | 0.26* (0.18–1.43) | 0.92 (0.5–1.71) |
| Poverty status | |||
| ≥200% | Reference | Reference | Reference |
| <200% | 2.1* (1.42–3.13) | 1.47* (1.03–2.08) | 1.47* (1.05–2.05) |
| Health status | |||
| Excellent/very good | Reference | Reference | Reference |
| Good/fair/poor | 1.91* (1.36–2.68) | 1.74* (1.26–2.39) | l.34* (l.0l–l.76) |
Source: National Health Interview Survey Pooled data from 2000–2005 adjusted for sample design and sample weights.Actual sample for regressions = 2,352.
O Rs (P < .05) represent the odds of reporting each outcome compared to the odds for the reference category for that variable and reflect the effect all other variables shown as well as region of country.
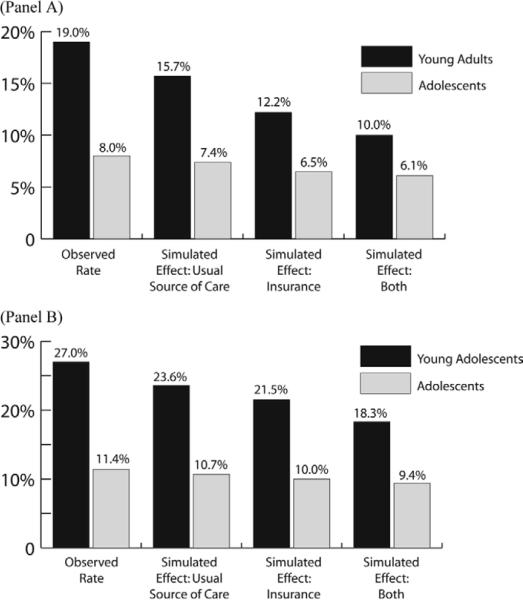
Results of the simulations of providing either public health insurance to subjects who report being uninsured or assuring a usual source of care to subjects reporting being without one are shown in the Figure. These simulations demonstrate the effect of changes in the population rates of unmet needs and delays in care that might be observed could such a change in access factors be achieved. For example, the observed rate of unmet needs caused by financial barriers in this sample of young adults is 27.1%; with the scenario of no one being uninsured (all uninsured persons are switched to having public coverage) and everyone having a usual source of care, the predicted rate of unmet needs would be 18.3%. Even if insurance and a usual source of care could be assured for all young adults, the predicted rates of unmet needs and delays in care for the young adults would still notably exceed those of adolescents.
Figure.
Simulated effects of providing insurance, usual source of care, or both on delays in care (A) and unmet needs (B).
DISCUSSION
The results of these analyses demonstrate that young adults with asthma have rates of delay in receiving care and unmet needs for care because of financial barriers that significantly exceed those of adolescents. Young adults with asthma are more likely to lack health insurance or a usual source of care than are adolescents, explaining part, but not all, of the difference in rates of delays and unmet needs. Aging into adulthood, independent of whether one has insurance or not, accounts for a component of the high rate of delays and unmet needs, although the mechanism is not elucidated by this analysis.
Other authors have demonstrated the high rates of being uninsured in young adults and specifically in those with chronic conditions.7,9,12 Exactly why so many young adults lack insurance coverage is not completely elucidated, but likely represents a combination of factors, including the possibility of aging out of family dependent coverage or Medicaid/SCHIP eligibility and being employed in jobs that do not offer health insurance. The simulation of providing public health insurance coverage to subjects who were uninsured demonstrates the potential impact that insurance coverage can have for this group. Expansion of public coverage eligibility to young adults with chronic conditions is 1 of several policy options available to increase health care access in young adults with chronic conditions. Recent evaluations of providing insurance to children with asthma through the SCHIP program have demonstrated a substantial positive effect of access and quality of asthma-specific care.22 Several states are experimenting with other options to ensure coverage, ranging from expanding age limits on eligibility for family coverage to mandating coverage for all. Effects of these programs and others should be monitored specifically to assess their impact on access to care for young adults.
Insurance coverage alone, however, is unlikely to be the full answer to the issue of access to and appropriate use of care for youth in the transition to adulthood. Exactly what factors, other than health insurance, account for the high rates of delay and unmet needs remains unclear. The literature on health care transitions provides little in the way of in-depth description of this problem, and we are left to rely on theory and conjecture. Do young adults continue to be seen in child-oriented health care settings? One analysis of discharges from children's hospitals demonstrated that services for adults make up a small proportion of the overall services provided, but the number of adults cared for in pediatric hospitals increased between 1994 and 1999.23 Little else is known about the care-seeking behaviors of young adults, especially those with childhood-onset chronic conditions. When care is not sought in pediatric settings, is it sought in adult settings? Are these young adults “dropping out” and not seeking care? The analysis presented here only demonstrates that, from these young adults' perspectives, they are not receiving the care that they need from the health care system, pediatric or adult-oriented.
There are a number of important limitations to the conclusions that can be drawn from these analyses. First, we compared adolescents and young adults who report having asthma. The proportion of young adult men with asthma was significantly lower than that of adolescent boys. Several factors could account for this difference, including respondent bias or the natural history of the condition. If the lower proportion represents the natural history of the condition, as the literature suggests, the results are unbiased.21 Furthermore, we were limited in our ability to fully adjust for differences in the severity of asthma between the adolescent group and young adult group as a reason for differences in the rates of unmet needs. We included self-reported and proxy-reported health status to capture such potential bias. These analyses rely on parent and self-report of asthma and delays and unmet needs. Clearly, not all delays and unmet needs pose the same threat to the health of these adolescents and young adults, and subjects may differ in their recognition of, and willingness to report, delays and unmet needs and level of severity that triggers an attempt to get care. Finally, we used cross-sectional data and are limited in our ability to assess causality.
To improve access to care for young adults with chronic conditions, policy that encourages health insurance coverage and eliminates interruptions in having an identified source of care are likely to have a major impact. Additionally, preparing adolescents with asthma for the transition to adult care, and preparation of the pediatric and adult-oriented systems to provide developmentally appropriate care will be necessary to address this issue.
Acknowledgments
Supported by the Agency for Healthcare Research and Quality and the Vikings Children's Foundation.
Glossary
- NHIS
National Health Interview Survey
- NCHS
National Center for Health Statistics
- OR
Odds ratio
REFERENCES
- 1.Freed GL, Hudson EJ. Transitioning children with chronic diseases to adult care: current knowledge, practices, and directions. J Pediatr. 2006;148:824–7. doi: 10.1016/j.jpeds.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 2.MCHB . Achieving success for all: children and youth with special health care needs: a 10-year action plan to accompany healthy people 2010. Maternal and Child Health Bureau; Washington, DC: 2001. [Google Scholar]
- 3.American Academy of Pediatrics A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110:1304–6. [PubMed] [Google Scholar]
- 4.Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the society for adolescent medicine. J Adolesc Health. 2003;33:309–11. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- 5.Scal P, Ireland M. Provision of services to foster transition to adulthood for youth with special health care needs. Pediatrics. 2005;115:1607–12. doi: 10.1542/peds.2004-0458. [DOI] [PubMed] [Google Scholar]
- 6.Zuvekas S, Weinick R. Changes in access to care, 1977–1996: the role of health insurance. Health Serv Res. 1999;34(1 pt 2):271–9. [PMC free article] [PubMed] [Google Scholar]
- 7.White PH. Access to health care: health insurance considerations for young adults with special health care needs/disabilities. Pediatrics. 2002;110:1328–35. [PubMed] [Google Scholar]
- 8.Newacheck PW, Wong ST, Galbraith AA, Hung Y-Y. Adolescent health care expenditures: a descriptive profile. J Adolesc Health. 2003;32(6 Suppl 1):3–11. doi: 10.1016/s1054-139x(03)00064-8. [DOI] [PubMed] [Google Scholar]
- 9.Fishman E. Aging out of coverage: young adults with special health needs. Health Aff. 2001;20:254–66. doi: 10.1377/hlthaff.20.6.254. [DOI] [PubMed] [Google Scholar]
- 10.Callahan ST, Cooper WO. Gender and uninsurance among young adults in the United States. Pediatrics. 2004;113:291–7. doi: 10.1542/peds.113.2.291. [DOI] [PubMed] [Google Scholar]
- 11.Collins S, Schoen C, Tenney K, Doty MM, Ho A. Why young adults become uninsured and how new policies can help. The Commonwealth Fund; New York, NY: 2005. Rite of passage? Report no. 649. [PubMed] [Google Scholar]
- 12.Callahan ST, Cooper W. Access to health care for young adults with disabling chronic conditions. Arch Pediatr Adolesc Med. 2006;160:178–82. doi: 10.1001/archpedi.160.2.178. [DOI] [PubMed] [Google Scholar]
- 13.Scal P. Transition for youth with chronic conditions: primary care physicians' approaches. Pediatrics. 2002;110:1315–21. [PubMed] [Google Scholar]
- 14.National Heart, Lung, and Blood Institute . Guidelines for the diagnosis and management of asthma. National Institutes of Health; Bethesda, Md: 1997. Report no. 97–4051. [PubMed] [Google Scholar]
- 15.Botman S, Moore T, Moriarity C, Parsons V. Design and estimation for the National Health Interview Survey 1995–2004. National Center for Health Statistics; Hyattsville, Md: 2000. [Google Scholar]
- 16.Newacheck P, Hughes D, Hung Y, Wong S, Stoddard J. The unmet health needs of America's children. Pediatrics. 2000;105:989–97. [PubMed] [Google Scholar]
- 17.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter. J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 18.Callahan ST, Cooper WO. Access to health care for young adults with disabling chronic conditions. Arch Pediatr Adolesc Med. 2006;160:178–82. doi: 10.1001/archpedi.160.2.178. [DOI] [PubMed] [Google Scholar]
- 19.Graubard B, Korn E. Predictive margins with survey data. Biometrics. 1999;55:652–9. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- 20.Minnesota Population Center and State Health Access Data Assistance Center . Integrated health interview survey. version 1.0 University of Minnesota; Minneapolis: 2007. [Google Scholar]
- 21.Guilbert T, Krawiec M. Natural history of asthma. Pediatr Clin North Am. 2003;50:523–8. doi: 10.1016/s0031-3955(03)00044-0. [DOI] [PubMed] [Google Scholar]
- 22.Szilagyi PG, Dick AW, Klein JD, Shone LP, Zwanziger J, Bajorska A, et al. Improved asthma care after enrollment in the state children's health insurance program in New York. Pediatrics. 2006;117:486–96. doi: 10.1542/peds.2005-0340. [DOI] [PubMed] [Google Scholar]
- 23.Goodman DM, Mendez E, Throop C, Ogata ES. Adult survivors of pediatric illness: the impact on pediatric hospitals. Pediatrics. 2002;110:583–9. doi: 10.1542/peds.110.3.583. [DOI] [PubMed] [Google Scholar]