Abstract
The emergence of Reston ebolavirus (REBOV) in domestic swine in the Philippines has caused a renewed interest in REBOV pathogenicity. Here, the use of different rodent species as animal disease models for REBOV was investigated. BALB/c and STAT1−/− mice, Hartley guinea pigs, and Syrian hamsters were inoculated intraperitoneally with REBOV strain Pennsylvania or Reston08-A. Although virus replication occurred in guinea pigs, hamsters, and STAT1−/− mice, progression to disease was only observed in STAT1−/− mice. Moreover, REBOV Pennsylvania was more pathogenic than REBOV Reston08-A in this model. Thus, STAT1−/− mice may be used for research of REBOV pathogenicity and intervention strategies.
Reston ebolavirus (REBOV) is one of the members of the genus Ebolavirus in the Filoviridae family and was discovered in 1989 in cynomolgus macaques imported into the United States from the Philippines [1]. Subsequent epizootics of REBOV infection in 1990, 1992, and 1996 in nonhuman primate quarantine facilities in the United States and Italy were also traced back to import of cynomolgus macaques from the same facility in the Philippines which had been reported to host REBOV infected animals several times [2–5]. In 2008, REBOV was detected in domestic swine in the Philippines that were also experiencing porcine reproductive and respiratory syndrome virus infection [6]. These outbreaks of REBOV infection in nonhuman primates and swine highlight the zoonotic potential of this virus. In addition, although REBOV has not yet been associated with disease in humans, it is capable of infecting humans as shown by the presence of antibodies against REBOV in people in close contact with infected macaques and swine [6–8], suggesting that sufficient adaptation might render REBOV more pathogenic in humans. However, research is hampered by the fact that the only available disease model described for REBOV is the cynomolgus macaque [9, 10]; experimental inoculation of mice lacking the interferon α/β receptor with REBOV has been described, but no disease was observed in these animals [11].
In this study, we assessed several rodent models, BALB/c mouse (Mus musculus), Hartley guinea pig (Cavia porcellus), Syrian hamster (Mesocricetus auratus), and STAT1−/− mouse (Mus musculus), which lack the signal transducer and activator of transcription 1 [12], for their use as REBOV disease models. We used 2 different REBOV strains, Pennsylvania, isolated from cynomolgus macaques during a REBOV outbreak in the United States in 1989, and Reston08-A, isolated from a domestic pig during a REBOV outbreak in the Philippines in 2008. Animal experiments were approved by the Institutional Animal Care and Use Committee and performed by certified staff in an Association for Assessment and Accreditation of Laboratory Animal Care–approved biosafety level 4 facility.
Two groups of 12 6–8-week-old female BALB/c mice (Harlan Laboratories), Hartley guinea pigs (Charles River Laboratories), Syrian hamsters (Harlan Laboratories), and STAT1−/− mice (Taconic) were housed in isolation units and inoculated intraperitoneally with 105 focus-forming units (FFUs) of REBOV Pennsylvania or Reston08-A virus; 4 animals of each species were mock-inoculated. Animals were monitored for clinical signs and weighed daily. On days 2 and 5 after inoculation, 4 animals from each group of 12 were euthanized, and blood, lungs, spleens, livers, and kidneys were harvested and nasal and oropharyngeal swabs were collected. Remaining animals were euthanized on day 14 after inoculation and sampled like the animals euthanized on days 2 and 5 after inoculation.
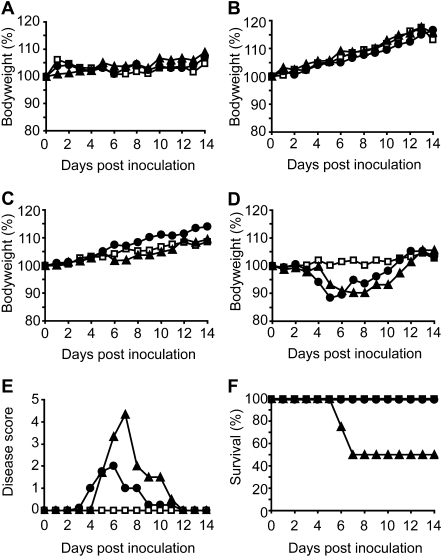
BALB/c mice, Hartley guinea pigs, and Syrian hamsters showed no clinical signs or weight loss upon inoculation with REBOV strains Pennsylvania or Reston08-A (Figure 1, A–C). In contrast, STAT1−/− mice showed severe clinical signs upon inoculation with both viruses, such as ruffled fur, lethargy, and weight loss. The maximum weight loss for Reston08-A–inoculated STAT1−/− mice was 12% on day 5 after inoculation, followed by recovery starting on day 6; the maximum weight loss in STAT1-/- mice inoculated with REBOV Pennsylvania was ∼10%, but it lasted from day 6 through day 8 (Figure 1D). The severity of disease was scored daily (with 0 for no signs of disease and 7 for death); the mean disease scores of REBOV Pennsylvania–inoculated STAT1-/- mice and Reston08-A–inoculated STAT1-/-mice are plotted in Figure 1E. The first onset of clinical signs was observed in the Reston08-A–inoculated STAT1-/- mice on day 4 after inoculation; the REBOV Pennsylvania–inoculated STAT1-/- mice showed signs starting on day 5.
Figure 1.
Weight loss, disease score, and survival upon inoculation of different rodent species with Reston ebolavirus. BALB/c mice (A), Hartley guinea pigs (B), Syrian hamsters (C), and STAT1−/− mice (D) were inoculated intraperitoneally with Dulbecco modified Eagle medium (squares), 105 focus-forming units (FFUs) of Reston ebolavirus strain Pennsylvania (triangles), or 105 FFUs of strain Reston08-A (circles) and weighed daily. The mean body weight per group was calculated as the percentage of weight at the start of the experiment. In STAT1−/− mice, severity of disease was scored daily (0, no symptoms; 1, ruffled fur; 2, ruffled fur and weight loss of <5%; 3, ruffled fur, hunched posture, and weight loss of >5%; 4, ruffled fur, hunched posture, and weight loss of >10%; 5, ruffled fur, hunched posture, and weight loss of >15% or paralysis of limbs; 6, ruffled fur, hunched posture, and weight loss of >20% or paralysis of limbs; 7, death; euthanasia was performed at a score of ≥5). Mean disease scores were calculated (E). Survival of STAT1−/− mice was calculated as the percentage of animals surviving after the 5 day post inoculation necropsies (F).
Disease scores of the REBOV Pennsylvania–inoculated STAT1−/− mice were higher and clinical signs lasted longer than those of the Reston08-A–inoculated mice. On day 5 after inoculation, 1 of the REBOV Pennsylvania–inoculated STAT1−/− mice succumbed to the infection; of the remaining 4 mice, 1 died on day 6 after inoculation and 1 died on day 7 after inoculation (Figure 1F). All of the Reston08-A–inoculated STAT1−/− mice recovered after initial disease symptoms and survived the infection. Recovery in the surviving REBOV Pennsylvania–inoculated STAT1−/− mice seemed somewhat slower than in the Reston08-A–inoculated mice; however, surviving STAT1-/- mice had completely recovered from the infection by day 12 after inoculation, as indicated by regained body weight. Taken together, the lethality of the REBOV Pennsylvania strain in STAT1−/− mice combined with its higher disease score, prolonged weight loss, and delayed recovery, as compared with the Reston08-A virus, suggest that the REBOV Pennsylvania virus has a more pathogenic phenotype than Reston08-A.
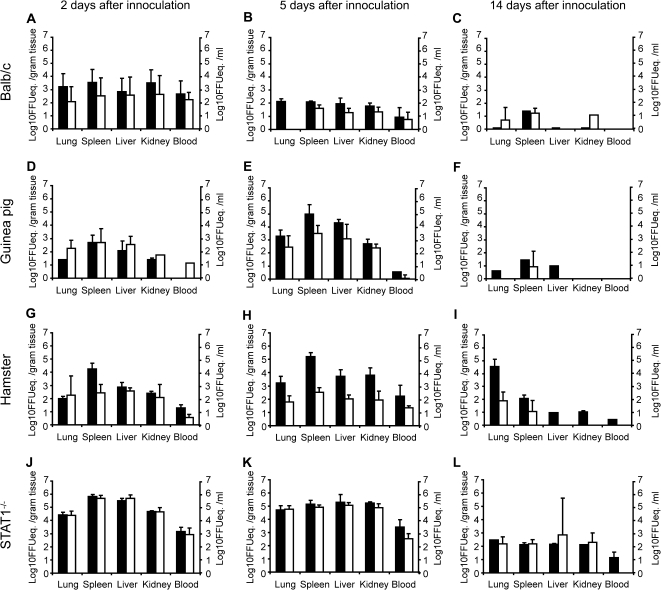
Lung, spleen, liver, and kidney samples obtained from animals on days 2, 5, and 14 after inoculation were homogenized using a TissueLyzer II (Qiagen), and RNA was extracted from 30-mg tissue samples using a RNeasy Mini Kit (Qiagen) according to instructions of the manufacturer. RNA was extracted from blood and from nasal and oropharyngeal swabs using the QIAamp Viral RNA Mini Kit (Qiagen). All samples were analyzed for the presence of viral RNA by use of a 2-step real-time reverse-transcription polymerase chain reaction (PCR) with Taqman reverse transcription reagents (Applied Biosystems) and Taqman Universal Master Mix II (Applied Biosystems) according to the instructions of the manufacturer (primer and probe sequences are available on request); FFU equivalents were calculated for positive samples by running a standard curve of a titered virus stock in parallel with all real-time PCRs. Nasal and oropharyngeal swabs of all animals were negative (data not shown). In BALB/c mice, FFU equivalents were highest on day 2 after inoculation, with lower FFU equivalents and fewer animals testing positive on day 5 than on day 2 after inoculation and progressively less on day 14 after inoculation, although viral RNA could still be detected in all animals at this time (Figure 2, A–C). Thus, the possibility cannot be excluded that the positive PCR data are derived from residual RNA in tissues rather than from active replication of virus in these animals. In guinea pigs and hamsters, FFU equivalents in lung, spleen, liver, and kidney samples on day 2 after inoculation were comparable to those found in BALB/c mice (Figure 2, D–G); however, FFU equivalents in these animals increased between days 2 and 5 after inoculation, suggesting that the virus replicated in these animals. On day 5 after inoculation, REBOV Pennsylvania FFU equivalents were higher than those of Reston08-A in inoculated guinea pigs and hamsters (Figure 2, E–H). On day 14 after inoculation, viral RNA could no longer be detected in 3 of 4 guinea pigs and 2 of 4 hamsters inoculated with Reston08-A, compared with only 1 guinea pig and none of the hamsters that cleared the REBOV Pennsylvania virus by that time (Figure 2, F–I). Interestingly, in the lungs of all 4 hamsters inoculated with REBOV Pennsylvania, FFU equivalents remained high up to day 14 after inoculation. In STAT1−/− mice, FFU equivalents were ∼100-fold higher on days 2 and 5 after inoculation than in the other 3 animal species (Figure 2, J–K), in line with the severe disease observed in these animals. Unlike in guinea pigs and hamsters, no differences in FFU equivalents in STAT1−/− mice were detected between the 2 viruses on days 2 and 5 after inoculation, despite the fact that REBOV Pennsylvania seemed more virulent in these animals than Reston08-A virus, based on clinical signs and survival data. On day 14 after inoculation, low levels of RNA of both viruses could still be detected in all tissues, except for the blood of Reston08-A infected animals. Reston08-A virus inoculated animals, (Figure 2L).
Figure 2.
Focus-forming unit equivalents (FFUeq) in Reston ebolavirus–inoculated rodent species. On days 2 (left panels), 5 (middle panels), and 14 (right panels) after inoculation, 4 BALB/c mice (A–C), 4 Hartley guinea pigs (D–F), 4 Syrian golden hamsters (G–I), and 4 STAT1−/− mice (J–L) inoculated with Reston ebolavirus strain Pennsylvania (black bars) or Reston08-A (white bars) were euthanized and lungs, spleens, livers, kidneys, and blood samples were assayed for the presence of viral RNA. Focus-forming unit equivalents of positive samples were calculated per gram tissue for lung, spleen, liver, and kidney samples or per milliliter for blood samples. Geometric mean titers were calculated; error bars indicate standard deviation.
The detection of REBOV in domestic swine in the Philippines in 2008 was unprecedented in several ways: it was the first time an Ebola virus was detected in a domestic animal species, and 3 genetically distinct REBOV viruses were isolated from 2 geographical locations [6], suggesting independent introductions of different REBOV strains into the Philippine swine population or a prolonged, but undetected, circulation in swine of this virus. This extension of known host species for REBOV and the potential of sustained pig-to-pig transmission raise the concern for the emergence of REBOV in and adaptation of REBOV to other domestic animal species or humans. The detection of REBOV in swine highlights the need for livestock and wildlife surveillance and to explore the potential natural host in areas where the virus is endemic. Moreover, it emphasizes the need for small animal models to study the molecular basis of the pathogenesis of REBOV and the ability of this virus to acquire enhanced pathogenicity.
The absence of disease manifestation (in BALB/c mice, Hartley guinea pigs, and Syrian hamsters) and perhaps even replication (in BALB/c mice) makes these animals interesting models as they may resemble the situation in humans, among whom REBOV-induced disease has so far not been observed. The replication of REBOV in guinea pigs and hamsters also creates the possibility of adapting REBOV to these hosts, similar to the adaptation of Zaire ebolavirus to mice and guinea pigs [13, 14], possibly resulting in a disease manifestation similar to that observed in cynomolgus macaques and thus an opportunity to study REBOV disease in guinea pigs or hamsters.
Besides the cynomolgus macaque, in which REBOV causes severe and often lethal hemorrhagic disease [9, 10], the STAT1−/− mouse is currently the only small animal model in which severe disease is observed upon REBOV infection, making it an attractive model to study pathogenesis or antiviral therapy. The fact that REBOV, especially the REBOV Pennsylvania strain, causes severe disease in STAT1−/− mice indicates that the early innate immune response is a major determinant of pathogenicity of REBOV in vivo.
We observed a difference in pathogenicity in STAT1−/− mice between the REBOV Pennsylvania and Reston08-A strains, where the Pennsylvania virus displayed a more pathogenic phenotype. Whether the decreased pathogenicity of the Reston08-A virus is due to circulation of the virus in pigs or in its natural reservoir is currently not clear. In total, there are 105 amino acid differences between strains Pennsylvania and Reston08-A [6], with 32 amino acid differences in the glycoprotein (reviewed in [15]), which mediates viral entry into the host cell and is also an important determinant of pathogenicity of Ebola viruses.
The STAT1−/− mouse model described here can be used to further investigate the determinants of the difference in pathogenicity between REBOV Pennsylvania, Reston08-A, and other REBOV strains of interest. Moreover, the STAT1−/− mouse model will be helpful to assess potential prophylactic and therapeutic intervention strategies, such as vaccination and antiviral therapies. There are drawbacks to using STAT1−/− mice in these studies. First of all, STAT1−/− mice lack an important component of the interferon α/β and interferon γ signaling cascade. Nonetheless, these mice have been used successfully for testing vaccines against monkeypox virus and rotavirus [16, 17] and for testing of antivirals against monkeypox virus and Crimean-Congo hemorrhagic fever virus [16, 18]. Second, mouse models of Ebola virus infection have shown relatively poor predictability of vaccine efficacy in a nonhuman primate model. However, the STAT1−/− mouse model described here is currently the only alternative disease model for studying REBOV infection.
Funding
This work was supported by the Division of Intramural Research of the National Institute of Allergy and Infectious Diseases, National Institutes of Health.
Acknowledgments
We thank William White at the Foreign Animal Disease Diagnostic Laboratory of the United States Department of Agriculture (Plum Island, NY) and Stuart Nichol and Pierre Rollin at the Special Pathogens Branch of the Centers for Disease Control and Prevention (Atlanta, GA) for providing REBOV strain Reston08-A. We thank Rachel Lacasse, Lisa Kercher, David Safronetz, Andrea Marzi and Friederike Feldmann (Division of Intramural Research, National Institute of Allergy and Infectious Diseases, National Institutes of Health) for assistance in the high-containment laboratory.
References
- 1.Jahrling PB, Geisbert TW, Dalgard DW, et al. Preliminary report: isolation of Ebola virus from monkeys imported to USA. Lancet. 1990;335:502–5. doi: 10.1016/0140-6736(90)90737-p. [DOI] [PubMed] [Google Scholar]
- 2.Miranda ME, Ksiazek TG, Retuya TJ, et al. Epidemiology of Ebola (subtype Reston) virus in the Philippines, 1996. J Infect Dis. 1999;179(suppl 1):S115–9. doi: 10.1086/514314. [DOI] [PubMed] [Google Scholar]
- 3.Hayes CG, Burans JP, Ksiazek TG, et al. Outbreak of fatal illness among captive macaques in the Philippines caused by an Ebola-related filovirus. Am J Trop Med Hyg. 1992;46:664–71. doi: 10.4269/ajtmh.1992.46.664. [DOI] [PubMed] [Google Scholar]
- 4.Rollin PE, Williams RJ, Bressler DS, et al. Ebola (subtype Reston) virus among quarantined nonhuman primates recently imported from the Philippines to the United States. J Infect Dis. 1999;179(suppl 1):S108–14. doi: 10.1086/514303. [DOI] [PubMed] [Google Scholar]
- 5.Viral haemorrhagic fever in imported monkeys. Wkly Epidemiol Rec. 1992;67:142–3. [PubMed] [Google Scholar]
- 6.Barrette RW, Metwally SA, Rowland JM, et al. Discovery of swine as a host for the Reston ebolavirus. Science. 2009;325:204–6. doi: 10.1126/science.1172705. [DOI] [PubMed] [Google Scholar]
- 7.Miranda ME, White ME, Dayrit MM, Hayes CG, Ksiazek TG, Burans JP. Seroepidemiological study of filovirus related to Ebola in the Philippines. Lancet. 1991;337:425–6. doi: 10.1016/0140-6736(91)91199-5. [DOI] [PubMed] [Google Scholar]
- 8.Miller RK, Baumgardner JY, Armstrong CW, et al. Update: filovirus infections among persons with occupational exposure to nonhuman primates. MMWR Morb Mortal Wkly Rep. 1990;39:266–7. 273. [PubMed] [Google Scholar]
- 9.Jahrling PB, Geisbert TW, Jaax NK, Hanes MA, Ksiazek TG, Peters CJ. Experimental infection of cynomolgus macaques with Ebola-Reston filoviruses from the 1989–1990 U.S. epizootic. Arch Virol Suppl. 1996;11:115–34. doi: 10.1007/978-3-7091-7482-1_11. [DOI] [PubMed] [Google Scholar]
- 10.Fisher-Hoch SP, Brammer TL, Trappier SG, et al. Pathogenic potential of filoviruses: role of geographic origin of primate host and virus strain. J Infect Dis. 1992;166:753–63. doi: 10.1093/infdis/166.4.753. [DOI] [PubMed] [Google Scholar]
- 11.Bray M. The role of the type I interferon response in the resistance of mice to filovirus infection. J Gen Virol. 2001;82:1365–73. doi: 10.1099/0022-1317-82-6-1365. [DOI] [PubMed] [Google Scholar]
- 12.Durbin JE, Hackenmiller R, Simon MC, Levy DE. Targeted disruption of the mouse Stat1 gene results in compromised innate immunity to viral disease. Cell. 1996;84:443–50. doi: 10.1016/s0092-8674(00)81289-1. [DOI] [PubMed] [Google Scholar]
- 13.Bray M, Davis K, Geisbert T, Schmaljohn C, Huggins J. A mouse model for evaluation of prophylaxis and therapy of Ebola hemorrhagic fever. J Infect Dis. 1998;178:651–61. doi: 10.1086/515386. [DOI] [PubMed] [Google Scholar]
- 14.Volchkov VE, Chepurnov AA, Volchkova VA, Ternovoj VA, Klenk HD. Molecular characterization of guinea pig-adapted variants of Ebola virus. Virology. 2000;277:147–55. doi: 10.1006/viro.2000.0572. [DOI] [PubMed] [Google Scholar]
- 15.Zampieri CA, Sullivan NJ, Nabel GJ. Immunopathology of highly virulent pathogens: insights from Ebola virus. Nat Immunol. 2007;8:1159–64. doi: 10.1038/ni1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stabenow J, Buller RM, Schriewer J, West C, Sagartz JE, Parker S. A mouse model of lethal infection for evaluating prophylactics and therapeutics against Monkeypox virus. J Virol. 2010;84:3909–20. doi: 10.1128/JVI.02012-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vancott JL, McNeal MM, Choi AH, Ward RL. The role of interferons in rotavirus infections and protection. J Interferon Cytokine Res. 2003;23:163–70. doi: 10.1089/107999003321532501. [DOI] [PubMed] [Google Scholar]
- 18.Bente DA, Alimonti JB, Shieh WJ, et al. Pathogenesis and immune response of Crimean-Congo hemorrhagic fever virus in a STAT-1 knockout mouse model. J Virol. 2010;84:11089–100. doi: 10.1128/JVI.01383-10. [DOI] [PMC free article] [PubMed] [Google Scholar]