Abstract
Pre- or postexposure treatments against the filoviral hemorrhagic fevers are currently not available for human use. We evaluated, in a guinea pig model, the immunogenic potential of Kunjin virus (KUN)–derived replicons as a vaccine candidate against Ebola virus (EBOV). Virus like particles (VLPs) containing KUN replicons expressing EBOV wild-type glycoprotein GP, membrane anchor-truncated GP (GP/Ctr), and mutated GP (D637L) with enhanced shedding capacity were generated and assayed for their protective efficacy. Immunization with KUN VLPs expressing full-length wild-type and D637L-mutated GPs but not membrane anchor–truncated GP induced dose-dependent protection against a challenge of a lethal dose of recombinant guinea pig-adapted EBOV. The surviving animals showed complete clearance of the virus. Our results demonstrate the potential for KUN replicon vectors as vaccine candidates against EBOV infection.
Ebola virus (EBOV) belongs to the genus Ebolavirus in the Filoviridae family, negative-strand RNA viruses responsible for severe hemorrhagic fever in human and nonhuman primates. In the field, establishment of strict quarantine measures preventing further human-to-human transmission is still the sole manner to fight the spread of infection. Several vaccine candidates have been developed, including some relying on the immunity induced by immunogens present on virus like particles (VLPs) produced in mammalian or insect cells [1, 2] or produced by plasmid DNA [3]. On the other hand, vaccines based on replicating viruses have also been developed including attenuated recombinant EBOV [4–9]. In the majority of vaccine candidates against EBOV, the surface glycoprotein GP was chosen as the immunogen because it is the only viral protein displayed at the surface of virions and virus-infected cells. The GP of EBOV is a type I glycoprotein synthesized from GP-gene specific mRNAs edited by the viral polymerase [10, 11]. GP possesses multiple N- and O-linked glycans and constitutes 2 disulfide-linked subunits, GP1 and GP2, which form trimeric spikes that decorate the surface of virus particles [12, 13]. Despite particular properties such as the presence of an immunosuppressive peptide [14] and the ability to mask some of its own epitopes, this protein appears to be the best immunogen to mount a protective immune response against EBOV [14, 15].
Flavivirus Kunjin (KUN) is an Australian subtype of West Nile virus [16] that is substantially less pathogenic than North American strains of West Nile virus. KUN replicons were the first reported flavivirus replicons, constructed by deleting the majority of the region coding for structural genes. To produce VLPs containing encapsidated KUN replicons, a tetracycline-inducible cell line expressing KUN structural genes C, prM and E was recently developed [17]. KUN VLPs can infect and deliver replicon RNA into most mammalian cell types, including dendritic cells, where replicon RNA initiates self-amplification without displaying significant cytopathic effects. The deleted structural genes in the replicon RNA can be replaced by vaccine immunogen, which is then expressed to high levels owing to the self-replicating nature of the replicon RNA [18]. RNA replication occurs exclusively in the cytoplasm, which avoids any issues associated with genome integration. Moreover, self-limited single-round infection provides an additional safety measure. KUN replicon–based vaccine candidates have shown promising results with immunogens derived from human immunodeficiency virus and papillomavirus [19, 20]. Here, we report the use of VLPs containing KUN replicons expressing different versions of EBOV GP for inducing protection in guinea pigs against a lethal challenge from guinea pig–adapted EBOV.
MATERIALS AND METHODS
Construction of KUN Replicons Expressing EBOV GP
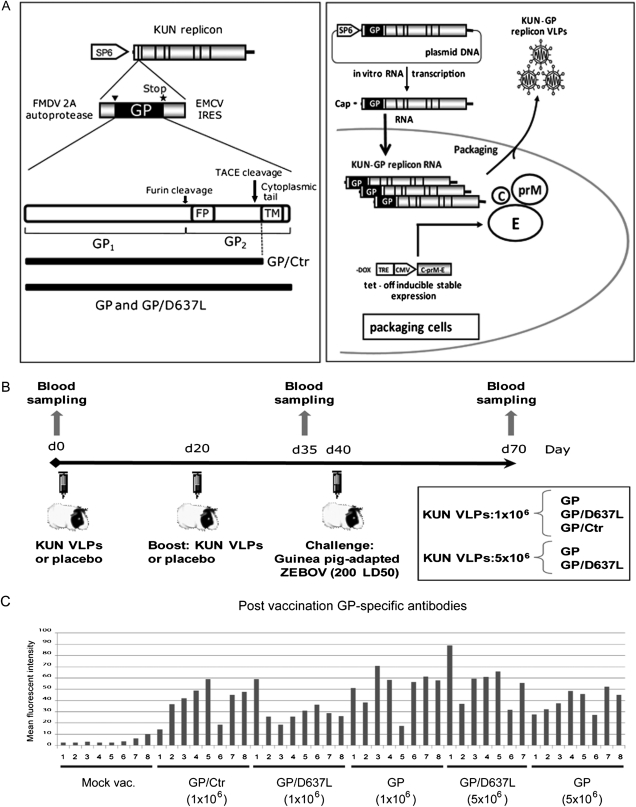
The sequence encoding full-length wild-type GP of Zaire EBOV strain Mayinga was amplified by polymerase chain reaction (PCR) from pGem-EBOV/GP [21] and cloned into the SP6 promoter-based KUN replicon vector SP6KUNrep5, which contains the FMDV 2A autoprotease upstream and the EMCV IRES downstream of the insertion site [22] (Figure 1A). The D637L mutant of GP displays a TACE cleavage site similar to the one observed in the interleukin (IL)–6 receptor (“LPVQ”). This mutation led to a better cleavability of GP by TACE, thus resulting in an enhanced GP shedding [23]. (Figure 1A) The mutant was generated by PCR mutagenesis with appropriate primers and then cloned into SP6KUNrep5. The replicon encoding GP/Ctr was generated by PCR mutagenesis by introducing a translation termination codon upstream of the region coding for the transmembrane anchor. The resulting GP lacks the last 25 codons and thus represents a truncated, membrane anchor–less version of the full-length GP released into the culture medium in a soluble form (Figure 1A).
Figure 1.
Immunization of guinea pigs with KUN-GP replicon virus like particles (VLPs) elicits an anti-GP antibody response. A, KUN replicon system for generating an Ebola virus (EBOV) vaccine candidate. Left panel, Schematic representation of the KUN-GP replicon. The KUN replicon vector SP6KUNrep5 contains the foot-and-mouth disease virus 2A autoprotease (FMDV 2A) sequence upstream and the encephalomyelocarditis virus internal ribosomal entry site (EMCV IRES) sequence downstream of the insertion site, to allow the release of the native product translated from the inserted gene. The GP/D637L construct containing a single aminoacid substitution (D637L) at the TACE cleavage site and the membrane anchor–truncated GP/Ctr construct are illustrated. The transmembrane anchor (TM), cytoplasmic tail, fusion peptide (FP), furin, and TACE cleavage sites are indicated. Right panel, Generation of KUN-GP replicon VLPs. KUN-GP replicon RNA was transcribed in vitro by SP6 RNA polymerase from linearised SP6KUNrep5-GP plasmid DNA and electroporated into the tetKUNCprME BHK packaging cell line inducibly expressing KUN structural genes C, prM, and E. VLPs containing encapsidated KUN-GP replicon RNA were collected from the culture medium of electroporated cells at various times after electroporation and their titers determined on Vero cells, as described elsewhere [24]. B, Vaccination and challenge protocols. Groups of 8 Dunkin Hartley guinea pigs were vaccinated twice with a 20-day interval with placebo, 1 × 106 KUN VLPs (GP, GP/D637L, and GP/Ctr), or 5 × 106 VLPs (GP and GP/D637L). Animals were challenged at day 40 with 200 LD50s of guinea pig-adapted recombinant Zaire EBOV and kept for 30 days. C, Induction of anti-GP–specific antibodies. The presence of anti-GP–specific antibodies was analyzed by flow cytometry on HEK293T cells transfected with pEBOVGP-IRES2-GFP. Serum samples were diluted 1:100. Alexa 555–labeled anti-guinea pig immunoglobulin (Ig) Gs were used as secondary antibodies. The graphs display the raw mean fluorescence intensity measured for each serum, and the numbers 1–8 correspond to the identification number of guinea pigs in each group.
Production of VLPs
VLPs containing KUN replicons were generated by transfecting the corresponding replicon RNAs produced in vitro into the packaging cell line tetKUNCprME [24] and harvesting culture supernatants at various times after transfection (Figure 1A). The VLP titers were determined on Vero cells, as described elsewhere [24]. GP expression was analyzed by Western blot using anti-GP monoclonal antibodies.
Vaccination
Female, 3-week-old Dunkin-Hartley guinea pigs (Harlan NL) were injected intraperitonealy with 1 × 106 or 5 × 106 KUN-GP VLPs. Control guinea pigs were mock-inoculated with phosphate-buffered saline. Guinea pigs received boosters 20 days after initial vaccination with an intraperitoneal injection of the same doses of VLPs. Samples of blood were collected from each guinea pig before the immunization (day 0), 5 days before the challenge with EBOV (day 35), and during euthanasia (day 70 for survivors). Animals were challenged at day 40 with 200 lethal doses, 50% (LD50s) of recombinant guinea pig-adapted EBOV [25]. After the challenge, animals were monitored daily during an additional 30 days (Figure 1B).
Flow Cytometry
Detection of GP antibodies was performed as described in Tamura et al [26]. Briefly, HEK293T cells were transfected with pEBOVGP-IRES2-GFP, a plasmid permitting expression of EBOV GP and eGFP from a single bicistronic mRNA, using Exgen 500 (Euromedex) in accordance with the manufacturer’s instructions. Twenty-four hours after transfection, cells were harvested and incubated with guinea pig sera (dilution, 1:100) and, subsequently, with anti-guinea pig immunoglobulin (Ig) G labeled with Alexa 555 (Molecular Probes). Mean fluorescent intensity was measured (555 nm channel) on GP/GFP-expressing cells. For detection of anti-NP antibodies, phCMV-EBOV/NP–transfected cells were treated with the BD cytofix/cytoperm kit in accordance with the manufacturer’s instruction. The cells were subsequently incubated with sera from vaccinated guinea pigs and anti–guinea pig IgG labeled with FITC (dilution 1:150) (Abcam).
Histological Examination
After necropsy, guinea pig organs were immersed in 4% paraformaledehyde and incubated for 15 days in accordance with the Bio Safety Level 4 bio-safety procedures. Organs were then embedded in paraffin (Anipath, Laennec Medicine Faculty), and microtome slices were counterstained with hematoxilin. Immunostaining of the organs was performed using anti-EBOV VP40 antibodies.
RESULTS AND DISCUSSION
Generation and Characterization of KUN-based Vaccine Candidates
Three KUN-based replicon vectors encoding wild-type EBOV GP, GP/D637L, and membrane anchor–truncated GP/Ctr (Figure 1A, left panel) were constructed and used to generate KUN VLPs in a packaging cell line (Figure 1A, right panel), as described elsewhere [24]. Replicon RNA expressing full-length wild-type GP induced a substantial cytopathogenic effect when transfected into packaging cells causing a reduction in VLP production and secretion. Two other replicons expressing mutated GPs were less cytopathic and led to somewhat improved VLP production (data not shown). GPs expression was confirmed for each replicon construct by Western blot using anti-GP monoclonal antibodies (data not shown). Indeed, the cytopathic effects induced by GP expression were in agreement with recent publications revealing that EBOV GP is able to mask or shield cellular surface proteins, including cellular integrins [15]. Masking of cellular integrins prevents their function, thus leading to rounding and detachment of the cells from the culture plastic. An enhanced shedding of GP from the cell surface induced by mutation at the TACE cleavage site (D637L) was previously shown to reduce GP presence on the plasma membrane, thus diminishing its cytopathogenic effects [24]. Earlier, it was also shown that truncation of the GP transmembrane anchor results in reduced cytopathogenicity, as explained by efficient secretion of truncated GP from the cells [27].
Immunization of Guinea Pigs With KUN-GP VLPs Induces GP-Specific Antibodies
Dunkin Hartley guinea pigs were vaccinated with KUN VLPs expressing either full-length wild-type GP, GP/D637L, or GP/Ctr, twice, with either 1 × 106 or 5 × 106 KUN VLPs per animal at a 20-day interval, respectively (Figure 1B). To monitor the antibody response, blood samples were collected from animals before the first immunization (day 0), 5 days before the challenge with EBOV (day 35), and at the end point of the experiment (day 70 for survivors or at the time of euthanasia). Presence of GP-specific antibodies in animals was assayed by flow cytometry using HEK293T cells expressing EBOV GP. Mean fluorescent intensity was used to estimate the levels of the GP-specific antibodies. As shown in Figure 1C, all guinea pigs vaccinated with KUN VLP constructs expressing either wild-type GP or GP/D637L displayed the presence of GP-specific antibodies. Overall, these results demonstrate that vaccination with KUN replicons induces an anti-GP–specific antibody response; however, the magnitude of the response varied between animals.
Immunization of Guinea Pigs With KUN VLPs Expressing EBOV GP Protects Animals From Lethal Challenge
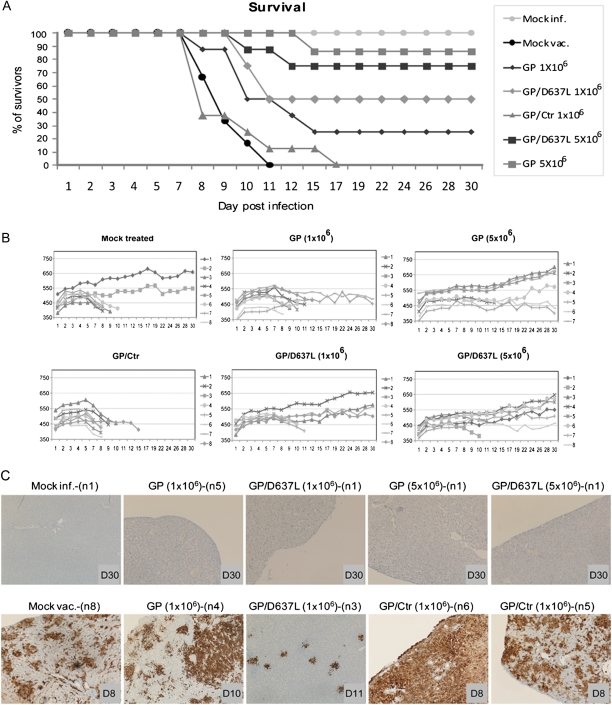
To evaluate the protective efficacy of the KUN replicons expressing EBOV GP, guinea pigs vaccinated with different KUN VLP constructs were infected with 200 LD50s of guinea pig–adapted recombinant EBOV [25]. Control animals died of infection 8 ± 0.82 (mean value +/− SD) days after challenge with EBOV (Figure 2A). Both KUN replicon VLPs expressing wild-type and D637L-mutated full-length GP provided an intermediate level of protection when a low dose was used for the vaccination (1 × 106 infectious VLPs). VLPs expressing wild-type GP protected 25% of animals (Figure 2A), with the mean time to death delayed to 9.83 ± 2.19 days. KUN- GP/D637L VLPs appeared to be more efficient at this immunization dose and protected 50% of the animals, with the mean time to death delayed to 9.5 ± 0.57 days (Figure 2A). The protective efficacy correlated well with the gain in body weight (Figure 2B). It is noteworthy that all animals challenged with EBOV (survivors and those that reached the ethical end point and were euthanized) showed the presence of anti-NP–specific antibodies that served as a control for EBOV infection (data not shown). Remarkably, when a higher vaccination dose was used (5 × 106), VLPs encoding wild-type and D637L-mutated full-length GP demonstrated a significant increase in protection, with >75% of animals surviving the challenge (Figure 2A). It should be mentioned, however, that those that survived the infection showed a delay in body weight increase (Figure 2B). The delay in most cases lasted for a few days, after which the animals started to gain weight, resembling mock-infected controls at the end of the experiment. Some animals appeared to suffer more from damage caused by infection. Although macroscopic observations did not reveal signs of disease, such as stress or reduced mobility, these animals did not gain weight until the end of the experiment. Surprisingly, immunization with VLPs expressing GP/Ctr (Figure 2A) did not elicit any protection, with the time to death ranging from 7 to 14 days (mean, 8.37 ± 2.54). These results suggested that soluble, nonmembrane-associated GP had low if any efficacy in mounting a protective response against EBOV.
Figure 2.
Immunization of guinea pigs with KUN-GP replicon virus like particles (VLPs) protects them from lethal challenge with Ebola virus (EBOV). A, Survival rate for each vaccinated group of guinea pigs. Guinea pigs were challenged with 200 LD50s of recombinant guinea pig-adapted EBOV. After the challenge animals were monitored daily during 30 days. Animals reaching the ethical end point were euthanized in accordance with regulations of the ethics committee. The percentages of surviving animals per group of animals are shown. B, Kinetics of animal body weight gain on challenge with EBOV. Animal body weight was measured during the challenge experiment on the days indicated. In the group of mock-vaccinated animals 2 guinea pigs (n1 and n2) were mock-infected, and 6 guinea pigs were challenged with EBOV. The x-axis represents the number of days after challenge, and the y-axis represents the weight in grams. C, Immunohistological analysis of the necropsy samples. The names of the KUN-GP replicon VLPs, the vaccination dose, and the individual numbers of the animals are indicated, as well as the day of sampling after infection (labeled as D). Liver samples were embedded in paraffin, and microtome slices were counterstained with hematoxilin. Immunostaining of the organs was performed using anti-VP40 EBOV–specific antibodies. The top row shows liver histology sections without any trace of VP40 antigen from mock-infected and surviving animals. The bottom row displays liver sections from animals that died of EBOV infection that all display antigen: either a low antigen level (GP/D637L -1 × 106—animal n3) or a high antigen level (GP-Ctr (1 × 106)—animals n5 and n6).
Animals surviving the challenge were euthanized and necropsied 30 days after infection. An immuno-histological analysis of the necropsy samples using anti-VP40 antibodies revealed clearance of virus from the livers of survivors (Figure 2C). Remarkably, those animals that had been vaccinated with KUN replicons expressing full-length GP but that did not survive the infection appeared to be capable of reducing virus replication. In these animals, virus spread was somewhat limited, comparison with the massive and widely disseminated appearance of virus-infected areas in mock-vaccinated controls. Curiously, animals vaccinated with replicons expressing truncated GP (GP/Ctr) demonstrated somewhat more acute signs of infection than did the mock-vaccinated guinea pigs; this correlated with the lack of protection by this VLP construct and development of stronger cachexia than in the other animal groups. The nature of this phenomenon is not yet well defined and will require further analysis. It can be speculated that soluble C-terminal-truncated GP expressed from KUN GP/Ctr and the membrane-bound GP synthesized from 2 other replicons could be different in the spectrum of induced anti-GP specific antibodies. Appearance of GP-specific antibodies mediating virus entry enhancement [28] or formation of immune complexes in the absence of a strong cell-mediated immunity could serve as possible explanations for the lack of the protection afforded by this KUN VLP.
In conclusion, we demonstrated—to our knowledge, for the first time—the ability of KUN replicons expressing full-length EBOV GP to protect guinea pigs from lethal EBOV infection. Adjustments of vaccine dose and vaccination protocols will likely result in more effective protection. The self-limited, single-round infection nature of KUN replicons combined with their capacity to elicit effective protection will provide unique safety standards for this candidate in vaccine development.
Funding
This work was supported by INSERM, France, and grants from the National Institute of Health (R21 AI 53579), Agence Nationale de la Recherche (ANR-07-MIME-006-01), and Fondation pour la Recherche Médicale en France (FRM DMI20091117323)
Acknowledgments
We are grateful to A. Dorier, T. Poumaroux and the Valbex team for the BSL2 animal facility experiments; G. Mercier, L. Thevenet and D. Moukouanga (BSL4 animal facility) and N. Gadot (Anipath) for providing excellent technical support; and R. Buckland for helpful discussions.
References
- 1.Warfield KL, Swenson DL, Negley DL, Schmaljohn AL, Aman MJ, Bavari S. Marburg virus-like particles protect guinea pigs from lethal Marburg virus infection. Vaccine. 2004;22:3495–502. doi: 10.1016/j.vaccine.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 2.Warfield KL, Swenson DL, Olinger GG, et al. Ebola virus inactivation with preservation of antigenic and structural integrity by a photoinducible alkylating agent. J Infect Dis. 2007;196(Suppl 2):S276–83. doi: 10.1086/520605. [DOI] [PubMed] [Google Scholar]
- 3.Dery M, Bausch DG. A DNA vaccine for the prevention of Ebola virus infection. Curr Opin Mol Ther. 2008;10:285–93. [PubMed] [Google Scholar]
- 4.Sullivan NJ, Sanchez A, Rollin PE, Yang ZY, Nabel GJ. Development of a preventive vaccine for Ebola virus infection in primates. Nature. 2000;408:605–9. doi: 10.1038/35046108. [DOI] [PubMed] [Google Scholar]
- 5.Jones SM, Feldmann H, Stroher U, et al. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med. 2005;11:786–90. doi: 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- 6.Bukreyev A, Yang L, Zaki SR, et al. A single intranasal inoculation with a paramyxovirus-vectored vaccine protects guinea pigs against a lethal-dose Ebola virus challenge. J Virol. 2006;80:2267–79. doi: 10.1128/JVI.80.5.2267-2279.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pushko P, Bray M, Ludwig GV, et al. Recombinant RNA replicons derived from attenuated Venezuelan equine encephalitis virus protect guinea pigs and mice from Ebola hemorrhagic fever virus. Vaccine. 2000;19:142–53. doi: 10.1016/s0264-410x(00)00113-4. [DOI] [PubMed] [Google Scholar]
- 8.Halfmann P, Ebihara H, Marzi A, et al. Replication-deficient ebolavirus as a vaccine candidate. J Virol. 2009;83:3810–5. doi: 10.1128/JVI.00074-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prins KC, Delpeut S, Leung DW, et al. Mutations abrogating VP35 interaction with double-stranded RNA render Ebola virus avirulent in guinea pigs. J Virol. 2010;84:3004–15. doi: 10.1128/JVI.02459-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Volchkov VE, Volchkova VA, Muhlberger E, et al. Recovery of infectious Ebola virus from complementary DNA: RNA editing of the GP gene and viral cytotoxicity. Science. 2001;291:1965–9. doi: 10.1126/science.1057269. [DOI] [PubMed] [Google Scholar]
- 11.Volchkov VE, Becker S, Volchkova VA, et al. GP mRNA of Ebola virus is edited by the Ebola virus polymerase and by T7 and vaccinia virus polymerases. Virology. 1995;214:421–30. doi: 10.1006/viro.1995.0052. [DOI] [PubMed] [Google Scholar]
- 12.Feldmann H, Volchkov VE, Volchkova VA, Stroher U, Klenk HD. Biosynthesis and role of filoviral glycoproteins. J Gen Virol. 2001;82:2839–48. doi: 10.1099/0022-1317-82-12-2839. [DOI] [PubMed] [Google Scholar]
- 13.Volchkov VE, Feldmann H, Volchkova VA, Klenk HD. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci U S A. 1998;95:5762–7. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volchkov VE, Blinov VM, Netesov SV. The envelope glycoprotein of Ebola virus contains an immunosuppressive-like domain similar to oncogenic retroviruses. FEBS Lett. 1992;305:181–4. doi: 10.1016/0014-5793(92)80662-z. [DOI] [PubMed] [Google Scholar]
- 15.Reynard O, Borowiak M, Volchkova VA, Delpeut S, Mateo M, Volchkov VE. Ebolavirus glycoprotein GP masks both its own epitopes and the presence of cellular surface proteins. J Virol. 2009;83:9596–601. doi: 10.1128/JVI.00784-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mackenzie JSRWA, M. W. Service encyclopedia of arthropod-transmitted infections of man and domesticated animals. Oxford: Oxford University Press; 2001. [Google Scholar]
- 17.Harvey TJ, Liu WJ, Wang XJ, et al. Tetracycline-inducible packaging cell line for production of flavivirus replicon particles. J Virol. 2004;78:531–8. doi: 10.1128/JVI.78.1.531-538.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pijlman GP, Suhrbier A, Khromykh AA. Kunjin virus replicons: an RNA-based, non-cytopathic viral vector system for protein production, vaccine and gene therapy applications. Expert Opin Biol Ther. 2006;6:135–45. doi: 10.1517/14712598.6.2.135. [DOI] [PubMed] [Google Scholar]
- 19.Harvey TJ, Anraku I, Linedale R, et al. Kunjin virus replicon vectors for human immunodeficiency virus vaccine development. J Virol. 2003;77:7796–803. doi: 10.1128/JVI.77.14.7796-7803.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kent SJ, De Rose R, Mokhonov VV, et al. Evaluation of recombinant Kunjin replicon SIV vaccines for protective efficacy in macaques. Virology. 2008;374:528–34. doi: 10.1016/j.virol.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 21.Sanchez A, Kiley MP, Holloway BP, Auperin DD. Sequence analysis of the Ebola virus genome: organization, genetic elements, and comparison with the genome of Marburg virus. Virus Res. 1993;29:215–40. doi: 10.1016/0168-1702(93)90063-s. [DOI] [PubMed] [Google Scholar]
- 22.Hoang-Le D, Smeenk L, Anraku I, et al. A Kunjin replicon vector encoding granulocyte macrophage colony-stimulating factor for intra-tumoral gene therapy. Gene Ther. 2009;16:190–9. doi: 10.1038/gt.2008.169. [DOI] [PubMed] [Google Scholar]
- 23.Dolnik O, Volchkova V, Garten W, et al. Ectodomain shedding of the glycoprotein GP of Ebola virus. Embo J. 2004;23:2175–84. doi: 10.1038/sj.emboj.7600219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khromykh AA, Varnavski AN, Westaway EG. Encapsidation of the flavivirus kunjin replicon RNA by using a complementation system providing Kunjin virus structural proteins in trans. J Virol. 1998;72:5967–77. doi: 10.1128/jvi.72.7.5967-5977.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volchkov VE, Chepurnov AA, Volchkova VA, Ternovoj VA, Klenk HD. Molecular characterization of guinea pig-adapted variants of Ebola virus. Virology. 2000;277:147–55. doi: 10.1006/viro.2000.0572. [DOI] [PubMed] [Google Scholar]
- 26.Tamura T, Chiba J. Production of antibodies against multipass membrane proteins expressed in human tumor cells using dendritic cell immunization. J Biomed Biotechnol. 2009;2009:673098. doi: 10.1155/2009/673098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takada A, Watanabe S, Ito H, Okazaki K, Kida H, Kawaoka Y. Downregulation of beta1 integrins by Ebola virus glycoprotein: implication for virus entry. Virology. 2000;278:20–6. doi: 10.1006/viro.2000.0601. [DOI] [PubMed] [Google Scholar]
- 28.Takada A, Feldmann H, Ksiazek TG, Kawaoka Y. Antibody-dependent enhancement of Ebola virus infection. J Virol. 2003;77:7539–44. doi: 10.1128/JVI.77.13.7539-7544.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]