Abstract
Study Aim
This study sought to determine whether premorbid child and family functioning accounts for or moderates group differences in postconcussive symptoms following mild traumatic brain injury (TBI) in childhood.
Methods
This prospective, longitudinal cohort study recruited 8- to 15-year-old children, 186 with mild TBI and 99 with orthopedic injuries (OI), from consecutive emergency department admissions. Parents and children rated postconcussive symptoms within 3 weeks of injury and at 1, 3, and 12 months post injury. Parents also provided retrospective ratings of pre-injury symptoms, as well as of premorbid child behavioral adjustment, overall family functioning, and other stressors and resources in the family environment.
Results
Children with mild TBI reported more postconcussive symptoms than those with OI, as did their parents, although premorbid child behavioral adjustment and symptoms also were significant predictors of postconcussive symptoms. Group differences in somatic symptoms as reported by parents were more pronounced among children from families that were higher functioning and had more environmental resources.
Discussion
Mild TBI during childhood results in more postconcussive symptoms than OI, even after children’s premorbid adjustment is taken into account. Counter to expectations, postconcussive symptoms following mild TBI may actually be more apparent among children from higher-functioning families with greater resources.
Keywords: Postconcussive, mild head injury, children, premorbid, moderator
1. Introduction
Mild traumatic brain injuries (TBI) are extremely common in children and adolescents. In the United States, more than a half million youth under the age of 15 years sustain TBI that require hospital-based medical care each year, and the vast majority of these injuries are mild in severity (Bazarian et al., 2005; Faul et al., 2010). Even if only a small proportion of children with mild TBI suffer persistent negative outcomes, then mild TBI is a serious public health problem.
Past reviews have suggested that mild TBI have little short- or long-term effect on children (Carroll et al., 2004b; Satz et al., 1997). However, most previous studies of mild TBI have assessed outcomes using standardized tests of cognitive abilities or broad-based ratings of behavioral adjustment. Only a few studies have focused specifically on post-concussive symptoms. Post-concussive symptoms are subjective somatic, cognitive, and emotional problems that are embodied in the diagnostic criteria for post-concussion syndrome in the International Classification of Diseases (ICD-10; World Health Organization, 1992), as well as in the research criteria for post-concussional disorder in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 1994). Both parents and children frequently report post-concussive symptoms following mild TBI (Barlow et al., 2010; Fay et al., 2003; Mittenberg et al., 1997; Ponsford et al., 1999; Taylor et al., 2010; Yeates et al., 1999, 2009), although the symptoms can occur in the absence of objective evidence of brain injury such as abnormal neuroimaging findings or deficits on standardized cognitive testing (Asarnow et al., 1995; Bijur et al., 1990; Satz, 2001).
These apparently contradictory findings have engendered ongoing controversy about the etiology of post-concussive symptoms. The controversy is often framed in terms of “psychogenesis versus physiogenesis” (Alexander, 1997; Bigler, 2008; Lishman, 1988; McKinlay, 2009). The former position holds that post-concussive symptoms can be accounted for by factors other than the injury itself, such as premorbid child or family functioning, post-injury coping or expectations, or outright malingering (Binder, 1986). In contrast, arguments for physiogenesis rest on experimental studies of non-human animals and clinical research with humans suggesting that mild TBI can result in acute neuropathology and abnormalities in brain function (Giza & Hovda, 2001) and that the occurrence of post-concussive symptoms after mild TBI may be associated with deficits on standardized cognitive testing and abnormalities on neuroimaging (Levin et al., 2008; Wilde et al., 2008). Despite the apparent conflict, these competing explanations are not mutually exclusive (Kashluba et al., 2008; Ponsford et al., 2000). Research is needed to identify both injury and non-injury related factors that predict the risk of persistent post-concussive symptoms (Satz, 2001; Yeates, 2010).
We recently completed a prospective, longitudinal study intended to clarify the outcomes of mild TBI in children (Yeates & Taylor, 2005). The study focused specifically on post-concussive symptoms and was designed to address the methodological shortcomings of previous research (Carroll et al., 2004a; Dikmen & Levin, 1993; Yeates, 2010). Participants were recruited from consecutive admissions to emergency departments at two large children’s hospitals, and included children with mild TBI or with orthopedic injuries (OI). Mild TBI were defined based on specific inclusion and exclusion criteria encompassing a range of severity (Williams et al., 1990). The inclusion of the OI group controlled for premorbid factors associated with an increased risk of traumatic injury, as well as for the experience of acute medical care. Children and parents provided ratings of post-concussive symptoms at an initial assessment within 3 weeks of injury, and again at 1, 3, and 12 months post injury. They also provided retrospective ratings of pre-injury symptoms at the initial assessment.
In several recent papers, we have shown that children with complicated mild TBI, as indexed by neuroimaging abnormalities, loss of consciousness, and other indicators of severity (e.g., hospitalization, associated injuries, acute mental status changes), display different trajectories of post-concussive symptoms across time than children with uncomplicated mild TBI or OI not involving the head (Taylor et al., 2010; Yeates et al., 2009). Somatic and cognitive symptoms show distinct post-injury trajectories, which are moderated by children’s cognitive ability (Fay et al., 2009) and coping skills (Woodrome et al., 2011), as well as by demographic factors such as age at injury and socioeconomic status (Taylor et al., 2010). However, we have not specifically examined the role of premorbid child and family functioning as potential predictors of post-concussive symptoms.
The overall purpose of the current study, therefore, was to determine whether the relationship between mild TBI and post-concussive symptoms is accounted for or moderated by premorbid child and family functioning. At the initial assessment, parents provided ratings of children’s premorbid behavioral adjustment, as well as their pre-injury symptoms. Parents also provided retrospective ratings of overall family functioning and other stressors and resources in the family environment. Based on previous research showing that premorbid child and family functioning moderates the psychosocial outcomes of moderate to severe TBI (Taylor et al., 2002; Yeates et al., 1997), we hypothesized that differences between the mild TBI and OI groups in post-concussive symptoms would be larger among children with poorer premorbid functioning than among those with better functioning. A secondary hypothesis was that the moderating effects of premorbid child and family functioning would be most apparent in children with complicated mild TBI, as indexed by loss of consciousness.
2. Methods
2.1. Participants
All children from 8 to 15 years of age who presented to the Emergency Departments of Nationwide Children’s Hospital in Columbus, Ohio, USA, and Rainbow Babies and Children’s Hospital in Cleveland, Ohio, USA, with head trauma or orthopedic trauma were screened on a daily basis to determine if they met criteria for participation. Children were included in the mild TBI group if they sustained a blunt head trauma and displayed at least one of the following indications of concussion: an observed loss of consciousness of no longer than 30 minutes; a Glasgow Coma Scale (Teasdale & Jennett, 1974) score of 13 or 14; or reports by medical personnel of at least two of the following acute signs and symptoms of concussion: persistent post-traumatic amnesia (PTA), transient neurological deficits, recurrent vomiting, nausea, headache, diplopia, dizziness, disorientation, and other mental status changes. Children were excluded from the mild TBI group if they displayed delayed neurological deterioration, but not if they required hospitalization or demonstrated intracranial lesions or skull fractures on acute computerized tomography.
Inclusion criteria for the OI group consisted of upper or lower extremity fractures that were associated with an Abbreviated Injury Scale (AIS; American Association for the Advancement of Automotive Medicine, 1990) score of 3 or less. The AIS is a widely-used scoring system that assesses the severity of injuries to specific anatomic regions on a scale of 1 to 6. Children were excluded from the OI group if they displayed any evidence of head injury or symptoms of concussion.
Additional exclusion criteria for children in both groups included: (a) any injury that required surgical or neurosurgical intervention; (b) any associated injury with an AIS score greater than 3; (c) any injury that interfered with neuropsychological testing (e.g., fracture of preferred upper extremity); (d) hypoxia, hypotension, or shock associated with the injury; (e) ethanol or drug ingestion involved with the injury; (f) documented history of previous head trauma requiring medical treatment; (g) premorbid neurological disorder or mental retardation; (h) any injury resulting from child abuse or assault; (i) history of severe psychiatric disorder requiring hospitalization; or (j) any medical contraindication to magnetic resonance imaging (MRI). Children were not excluded for premorbid learning difficulties or attention problems. The mild TBI and OI groups did not differ on retrospective parent ratings of premorbid school performance or attention problems.
Among children meeting inclusion criteria, participation rates were 35% in the OI group and 48% in the mild TBI group. Participants and non-participants did not differ in age, sex, ethnic/racial minority status, or in census tract measures of socioeconomic status (i.e., mean family income, percentage of minority heads of household, and percentage of households below the poverty line).
The final sample included 186 children with mild TBI and 99 children with OI. The groups did not differ in age at injury, sex, ethnic/racial minority status, socioeconomic status, post-acute intellectual functioning, or parents’ retrospective ratings of premorbid symptoms (see Table 1). The mild TBI group displayed greater overall injury severity as measured by the Modified Injury Severity Scale, which is an overall index derived from AIS scores, calculated as the sum of the squares of the three most severely injured body areas (Osler, Bakker, & Long, 1997). However, when the contribution of the head injury to MISS scores was omitted, the OI group had the highest mean score. Recreational and sports-related injuries were the most common cause of injury (57% of mild TBI, 62% of OI), with falls the second leading cause (20% of mild TBI, 21% of OI). Transportation-related injuries accounted for significantly more cases of mild TBI (17%) than OI (3%).
Table 1.
Demographic and Clinical Characteristics of Participants
| Variable | OI | Mild TBI without LOC |
Mild TBI with LOC |
|---|---|---|---|
| n | 99 | 112 | 74 |
| Years of age at injury (M, SD) | 11.76 (2.23) | 11.83 (2.23) | 12.15 (2.20) |
| Male (n, %) | 64 (65%) | 75 (67%) | 57 (77%) |
| Caucasian (n, %) | 64 (65%) | 80 (71%) | 52 (70%) |
| Socioeconomic status1 (M, SD) | −0.09 (1.15) | −0.02 (0.87) | 0.15 (0.97) |
| Modified Injury Severity Scale (M, SD)* | 3.25 (1.52) | 3.33 (3.49) | 6.58 (5.23) |
| Glasgow Coma Scale < 15 (n, %) | NA | 13 (12%) | 11 (15%) |
| Intracranial abnormality on MRI (n, %) | NA | 16 (14%) | 17 (24%) |
| WASI IQ score at initial post-injury assessment (M, SD) | 98.90 (15.09) | 99.37 (13.67) | 100.09 (14.16) |
| Premorbid total PCS-I score (M, SD) | 1.13 (2.06) | 1.04 (1.35) | 1.19 (1.68) |
| Premorbid HBI cognitive symptoms score (M, SD) | 10.92 (7.59) | 11.73 (7.78) | 11.23 (7.59) |
| Premorbid HBI somatic symptoms score (M, SD) | 2.46 (3.16) | 3.53 (3.43) | 3.14 (3.23) |
TBI = Traumatic Brain Injury; OI = Orthopedic Injury; LOC = Loss of consciousness; MRI = Magnetic Resonance Imaging; post-concussive symptoms = Post-concussive symptoms; WASI = Wechsler Abbreviated Scale of Intelligence; PCS-I = Postconcussive Symptom Interview; HBI = Health and Behavior Inventory.
Socioeconomic status was assessed by averaging sample z scores for years of maternal education, median family income for census tract, and the Duncan Socioeconomic Index, which is a measure of occupational prestige.
Groups differ significantly, p < .05.
2.2. Procedure and Attrition
The research was approved by the appropriate institutional review boards, and informed parental consent and child assent were obtained in writing prior to participation. Children who met all inclusion/exclusion criteria and whose parents agreed to participate were scheduled for an initial assessment no later than 3 weeks post injury, with 80% completed between 1 and 2 weeks post injury (M = 11.35 days, SD = 3.42). Parents and children rated current post-concussive symptoms at the initial assessment and again at 1, 3, and 12 months post injury. At the initial assessment, parents also completed a retrospective report of pre-injury symptoms, prior to reporting current symptoms, as well as retrospective ratings of children’s premorbid behavioral adjustment. Parents also provided retrospective ratings of overall family functioning and other stressors and resources in the family environment. Additionally, children with mild TBI completed standardized testing of cognitive skills, as well as MRI of the brain.
Of 285 children who completed the initial assessment, 280 (98%) completed the assessment at 1-month post injury, 268 (94%) completed the 3-month assessment, and 253 (89%) completed the 12-month assessment. The groups did not differ in the proportion of missed assessments. At each assessment, children who did and did not return did not display any significant differences in demographic or clinical variables (i.e., SES, age at injury, severity of injury, or initial post-concussive symptoms), except for the 12 month assessment, when children who did not return had lower SES and were more likely to be of minority race.
2.3. Measures
2.3.1. Child behavioral adjustment
Children’s behavioral adjustment was assessed using the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001). The CBCL is a well-known rating scale that was standardized on a large sample of community and clinic-referred children. It has demonstrated satisfactory reliability and validity in previous research. For the current study, behavioral adjustment was measured using the total T score from the CBCL.
2.3.2. Family functioning
Family functioning was assessed using the 12-item General Functioning subscale of the McMaster Family Assessment Device (FAD-GF, Byles et al., 1988; Miller et al., 1985). The measure has shown satisfactory reliability and validity in previous research (Byles et al., 1988; Miller et al., 1985) and is related to outcomes of childhood TBI (Yeates et al., 1997). For this study, the scores from the General Functioning Scale were standardized across the entire sample (m = 0, sd = 1). Consistent with the scaling of the original scores, higher scores reflect worse family functioning.
Family functioning was also assessed using the Life Stressors and Social Resources Inventory—Adult Form (LISRES-A; Moos & Moos, 1988). The LISRES-A (Moos et al., 1989) is an interview measure that generates standard scores for stressors and resources across a variety of domains. It has demonstrated satisfactory reliability and validity in prior research (Wade et al., 1996). For the current study, we averaged standard scores across domains to provide global measures of family stressors and resources. Child stressor and resource subscales were omitted because they included ratings of behavior and were potentially confounded with the measures of premorbid child behavioral adjustment. The negative life events stressor subscale was omitted because it was potentially confounded with injury severity.
2.3.3. Post-concussive symptoms
Post-concussive symptoms were assessed using two measures, the Postconcussive Symptom Interview (PCS-I; Mittenberg et al., 1997) and the Health and Behavior Inventory (HBI; Yeates et al., 1999). The parent and child forms of both measures are worded slightly differently to be age-appropriate and to reflect first- versus third-person perspectives. The PCS-I is administered orally, and asks children and their parents to report the presence or absence of 15 postconcussive symptoms over the past week. The symptoms include cognitive (e.g., “Have you had any trouble paying attention in the last week?”), somatic (e.g., “Have you been tired a lot in the last week?”), and emotional difficulties (e.g., “Have you felt cranky in the last week?”) similar to those listed in the research diagnostic criteria for postconcussional disorder in the DSM-IV (American Psychiatric Association, 1994) and for postconcussion syndrome in the ICD-10 (World Health Organization, 1993). The total number of symptoms was used as a dependent measure, and displayed satisfactory internal consistency at each of the four assessments (Cronbach’s alpha from .78 to .82 for parents’ ratings and from .70 to .77 for children’s ratings).
The HBI is a 50-item self report questionnaire that includes a variety of cognitive, somatic, emotional, and behavioral symptoms. The questionnaire requires parents and children to rate the frequency of occurrence of each symptom over the past week on a four point scale, ranging from “never” to “often”. Total scores for cognitive (e.g., “I have trouble paying attention.”) and somatic (e.g., “I have headaches.”) symptom dimensions were used as dependent measures, based on a factor analytic study showing substantial agreement between parents and children for those dimensions (Ayr et al., 2009). Total scores for each dimension displayed satisfactory internal consistency across all four assessments (Cronbach’s alpha from .83 to .95 for parents’ ratings and from .86 to .91 for children’s ratings).
2.4. Data Analysis
Analyses of post-concussive symptoms across the four assessments (initial assessment and 1-, 3-, and 12-month follow-ups) were conducted using general linear mixed model analysis. Separate analyses were done for each measure of post-concussive symptoms as rated by parents and children. Predictors in the primary analytic models included group membership (indexed by two dummy variables, one comparing children with mild TBI and LOC to the OI group and another comparing the children with mild TBI but no LOC with the OI group) and time since injury (modeled in terms of both linear and quadratic change). Sex, race, socioeconomic status, and age at injury were included as covariates. The measure of preinjury symptoms corresponding to the measure of post-concussive symptoms in each particular analysis was also included as a covariate in analyses of parent-reported post-concussive symptoms; thus the dependent measures in those analyses reflect changes in symptoms relative to pre-injury levels. To explore potential moderating effects of premorbid child and family functioning on group differences, the models also included the CBCL total T score, FAD GF z score, and LISRES-A stressors and resources standard scores as predictors, as well as their interactions with group, time since injury, and group X time since injury.
After fitting an initial model, we reduced model complexity to achieve the most parsimonious model. We followed an iterative process, eliminating predictors for which the F tests for fixed effects were not significant, starting with three-way interactions, and then re-estimating the model before examining lower-level interactions and, finally, main effects. For any significant interaction, all of the main effects and lower-level interactions upon which the significant interaction was based were retained in the model. To control for Type I error, we applied a family-wise alpha for the parent and child measures of post-concussive symptoms, with alpha set at .0167 for each of the three parent measures and for each of the three child measures. Unstandardized beta weights and standard errors (SE’s) for significant main or simple effects provide estimates of effect size.
3. Results
3.1. Parent Ratings of Post-Concussive Symptoms
The results of analyses of parent ratings of post-concussive symptoms are summarized in Table 2, which presents significant effects for each measure of postconcussive symptoms. Children with mild TBI and LOC displayed significantly more symptoms than those in the OI group according to parent ratings on the PCS-I. Children with mild TBI but no LOC also displayed more symptoms than the OI group, but the difference was not significant after Bonferroni correction, t(285) = 2.36, p = .019. Although group differences lessened across time, the group X time since injury interaction was not significant after Bonferroni correction, F(4,285) = 2.92, p = 0.022. Group differences did not vary as a function of either children’s premorbid behavioral adjustment or premorbid family functioning. Additional predictors of higher parent ratings on the PCS-I included more premorbid symptoms, poorer premorbid behavioral adjustment, and female sex.
Table 2.
Results of Mixed Models Analysis of Parent-Rated Measures of PCS: Significant Effects
| Measure | Effect | Estimate | SE | Df | t | p |
|---|---|---|---|---|---|---|
| PCS Count | Premorbid PCS rating | 0.37 | 0.07 | 284 | 5.05 | <.001 |
| Sex | 0.64 | 0.24 | 282 | 2.70 | .007 | |
| Premorbid adjustment (CBCL) | 0.67 | 0.12 | 282 | 5.68 | <.001 | |
| Time since injury (linear) | −6.32 | 0.93 | 316 | −6.81 | <.001 | |
| Time since injury (quadratic) | 4.74 | 0.79 | 315 | 5.97 | <.001 | |
| Mild TBI with LOC vs OI | 1.00 | 0.28 | 282 | 3.52 | <.001 | |
| Group [F(2, 283) = 6.48, p = .002] | ||||||
| Cognitive PCS | Premorbid PCS rating | 0.62 | 0.04 | 281 | 15.30 | <.001 |
| Premorbid adjustment (CBCL) | 1.05 | 0.28 | 283 | 3.72 | <.001 | |
| Time since injury (linear) | 7.58 | 2.23 | 313 | 3.40 | <.001 | |
| Time since injury (quadratic) | −7.14 | 1.97 | 311 | −3.63 | <.001 | |
| Mild TBI with LOC vs OI | 2.74 | 0.63 | 285 | 4.32 | <.001 | |
| Group [F(2, 285) = 9.44, p < .001] | ||||||
| Somatic PCS | Premorbid rating | 0.41 | 0.05 | 278 | 8.22 | <.001 |
| Premorbid adjustment (CBCL) | 0.55 | 0.16 | 284 | 3.50 | <.001 | |
| Mild TBI with LOC vs OI | 3.01 | 0.70 | 315 | 4.33 | <.001 | |
| Mild TBI without LOC vs OI | 2.36 | 0.63 | 322 | 3.76 | <.001 | |
| Mild TBI with LOC vs OI X Time (linear) | −10.35 | 4.16 | 337 | −2.48 | .013 | |
| Group [F(2, 316) = 11.23, p < .001] | ||||||
| Group X Time [F(4, 300) = 5.03, p < .001)] | ||||||
| Group X FAD-GF [F(2, 278) = 6.20, p = .002)] | ||||||
| Group X LISRES-A Resources [F(2, 289) = 6.74, p = .001)] | ||||||
TBI = Traumatic Brain Injury; OI = Orthopedic Injury; LOC = Loss of consciousness; PCS = Postconcussive symptoms; FAD-GF = Family Assessment Device General Functioning Scale; LISRES-A = Life Stressors and Social Resources Inventory—Adult Form
Parent ratings of cognitive symptoms on the HBI followed a similar pattern. Specifically, the overall group main effect was significant. The mild TBI group with LOC displayed significantly more cognitive symptoms than the OI group across time, but the contrast between the mild TBI group without LOC and the OI group was not significant. More premorbid symptoms and poorer premorbid behavioral adjustment were again significantly associated with higher parent ratings. However, premorbid child and family functioning did not moderate group differences.
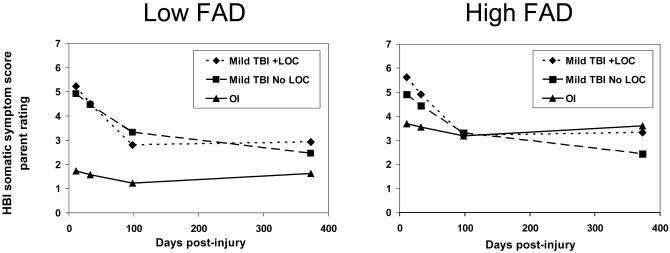
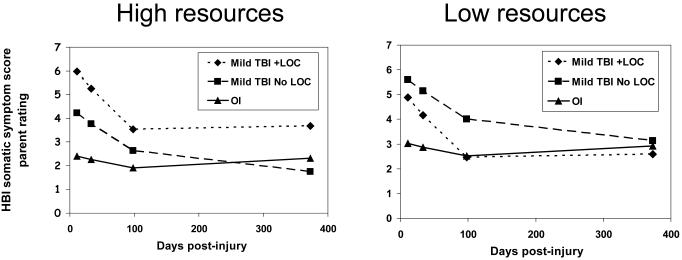
In contrast to the previous findings, the analysis of parent ratings of somatic symptoms on the HBI showed evidence of moderation of group differences by premorbid family functioning. Specifically, the group X FAD General Functioning scale interaction was significant, as was the group X LISRES-A resources scale interaction. To illustrate the interactions, somatic symptom scores were estimated at low and high levels of family functioning (or resources) (i.e., 1 standard deviation above vs 1 standard deviation below the overall sample mean for the respective measure of the family environment). As Figures 1 and 2 show, better family functioning and more family resources were associated with larger group differences in somatic symptoms than poorer family functioning or fewer resources. This was true for both mild TBI groups when family functioning was treated as the moderator, but only for children with mild TBI and LOC when family resources were considered. In addition to these interactions, the interaction of group X time since injury was significant, because group differences in somatic symptoms declined over time. Finally, more premorbid symptoms and poorer premorbid behavioral adjustment were also significant predictors of more post-injury somatic symptoms.
Figure 1.
Estimated means for parent ratings of somatic symptoms on the HBI as a function of family functioning (modeled at FAD scores +1 and −1 SD from grand sample mean).
Figure 2.
Estimated means for parent ratings of somatic symptoms on the HBI as a function of family functioning (modeled at LISRES-A total resources scores +1 and −1 SD from grand sample mean).
3.2. Child Ratings of Post-Concussive Symptoms
The results of analyses of children’s self-ratings of post-concussive symptoms are summarized in Table 2. The analyses revealed significant interactions of group X time since injury (i.e., linear slope) for both total symptom counts on the PCS-I and somatic symptom ratings on the HBI. In both cases, children in the mild TBI groups, both with and without LOC, reported significantly more symptoms than children in the OI group at the initial assessment and 1-month follow-up, but not at the 3- and 12-month follow-ups. Poorer premorbid behavioral adjustment and female sex were significant predictors of both total symptom counts on the PCS-I and somatic symptom ratings on the HBI, but premorbid child and family functioning did not moderate group differences.
Higher child self-ratings of cognitive symptoms on the HBI were related to poorer premorbid behavioral adjustment and lower SES. Neither the main effect for group nor the group X time since injury interaction was significant, and premorbid child and family functioning did not moderate group differences.
4. Discussion
The current study confirms that children with mild TBI, particularly those characterized by LOC, demonstrate significant post-concussive symptoms as compared to children with OI, even when premorbid child and family adjustment are taken into account. Children with mild TBI showed significant post-injury increases in both somatic and cognitive symptoms, although somatic symptoms tended to resolve over time, while cognitive symptoms persisted as much as 12 months post-injury. Consistent with previous reports based on the larger parent study (Taylor et al, 2010), both parents and children reported group differences in somatic symptoms, whereas only parents reported differences in cognitive symptoms. Thus, the findings provide support for a robust association between mild TBI and postconcussive symptoms that cannot be accounted for entirely by premorbid functioning.
Although group differences were robust, children’s premorbid symptoms and overall behavioral adjustment also were significant predictors of postconcussive symptoms, as was female sex. These findings are consistent with previous research showing that premorbid factors should be taken into consideration when evaluating the effects of mild TBI in children and adolescents (Ponsford, 1999). Premorbid factors not only help account for post-injury functioning, but may also be associated with the propensity to be injured in the first place (McKinlay et al., 2009). Thus, comparison groups in studies of pediatric mild TBI should be composed of children with other injuries, rather than healthy children, to avoid inaccurate attribution of group differences in post-injury functioning to mild TBI (Asarnow et al., 1995; Yeates, 2010).
Contrary to expectations, the findings provide only limited evidence for moderation of the effects of mild TBI by premorbid child or family functioning. Group differences did not vary in any instance as a function of premorbid child behavioral adjustment. Group differences in parent reports of somatic symptoms were moderated by family factors, but the direction of the interaction was opposite to expectations, such that group differences were more pronounced in the presence of better family functioning and more family resources. This finding runs counter to previous research among children with severe TBI showing that the effects of TBI are exacerbated in the face of poorer premorbid child and family functioning (Taylor et al., 2002; Yeates et al., 1997). The current findings have several potential explanations: Family adversity may obscure the effects of mild TBI for parents, making them less likely to perceive increased postconcussive symptoms; parents of children from higher-functioning families with more resources may be more attentive or sensitive to changes in their children’s health, making them more likely to perceive increased symptoms following mild TBI; children from higher-functioning families with more resources may be more sensitive to the effects of mild TBI, perhaps because they face higher demands or expectations in their daily environment or are more closely monitored; or the effects of mild TBI may be masked by other, more powerful causes of cognitive and somatic symptoms among children from lower-functioning families or those with lower resources.
The current study has several potential limitations. Recruitment rates for the mild TBI and OI groups were both below 50%, and may therefore limit the generalizability of the results. Relatively greater attrition of children of lower SES and ethnic minority status may also have reduced generalizability. However, non-participants did not differ from participants demographically, SES and minority status were taken into account in data analyses, and the mixed model analyses incorporated all available data, including that collected from children who missed later assessments. An additional limitation of the study is that information regarding children’s premorbid status was determined by retrospective ratings, and could potentially be biased for this reason. Although biases related to retrospective recall cannot be avoided completely, we believe that post-injury parent ratings are valid because they were obtained shortly after the injury, minimizing demands on retrospective recall. The mild TBI and OI groups did not differ on any retrospective measure of pre-injury functioning, suggesting that parents in the mild TBI group were able to distinguish pre- and post-injury symptoms and were not minimizing any premorbid difficulties their children might have had. A further weakness is the lack of a non-injury comparison group (Satz et al., 1997). An uninjured comparison group would help clarify the child and family premorbid characteristics associated with minor traumatic injuries in general, and provide a benchmark against which to compare post-injury symptoms in both the mild TBI and OI groups (Light et al., 1998).
Future research is needed to further delineate the effects of both injury and non-injury related factors, and their interactions, on postconcussive symptoms in children with mild TBI. Although the current findings reflect robust group differences that are related to injury severity, more information is needed regarding the nature of the underlying brain injury sufficient to result in postconcussive symptoms. Advanced neuroimaging techniques, such as susceptibility-weighted and diffusion tensor imaging, may provide quantitative indices of injury that may serve as biomarkers of brain injury (Ashwal et al., 2010). At the same time, the role of factors besides brain injury in accounting for persistent postconcussive symptoms also deserves attention. We have shown that children’s age (Taylor et al., 2010), premorbid intellectual functioning and behavioral adjustment (Fay et al., 2009), and coping skills (Woodrome et al., 2011), as well as SES and family functioning, help account for or moderate the effects of mild TBI; however, other factors, such as pain, motivation, and symptom exaggeration, warrant further study. The ongoing study of injury and non-injury related factors as predictors of outcomes will not only yield a deeper scientific understanding of mild TBI, but also improve methods for clinically identifying mild TBI and monitoring their sequelae and provide guidance in developing treatment approaches to preventing or ameliorating persistent postconcussive symptoms.
Yeates highlights.
We asked if premorbid function predicts postconcussive symptoms after pediatric mild TBI.
We studied postconcussive symptoms in children with mild TBI and orthopedic injuries.
Premorbid function is a predictor, but mild TBI still accounts for postconcussive symptoms.
Somatic symptoms are higher in children from higher functioning families with more resources.
Children from higher-functioning families may be more vulnerable to mild TBI.
Table 3.
Results of Mixed Models Analysis of Self-Rated Measures of PCS: Significant Effects
| Measure | Effect | Estimate | SE | Df | t | p |
|---|---|---|---|---|---|---|
| PCS Count | Sex | 1.14 | 0.29 | 281 | 3.94 | <.001 |
| Premorbid adjustment (CBCL) | 0.72 | 0.13 | 283 | 5.60 | <.001 | |
| Mild TBI with LOC vs OI | 1.81 | 0.44 | 295 | 4.08 | <.001 | |
| Mild TBI without LOC vs OI | 1.00 | 0.40 | 295 | 2.52 | .012 | |
| Mild TBI with LOC vs OI X Time (linear) | −7.52 | 2.56 | 308 | −2.94 | .004 | |
| Mild TBI with LOC vs OI X Time (quadratic) | 6.10 | 2.24 | 306 | 2.72 | .007 | |
| Group [F(2, 283) = 6.48, p = .002] | ||||||
| Group X Time (linear) [F(2, 310) = 4.45, p = .013] | ||||||
| Cognitive PCS | Socioeconomic status | −0.94 | 0.39 | 279 | −2.43 | .016 |
| Premorbid adjustment (CBCL) | 1.67 | 0.33 | 283 | 5.01 | <.001 | |
| Somatic PCS | Sex | 1.70 | 0.57 | 281 | 2.98 | .003 |
| Premorbid adjustment (CBCL) | 0.89 | 0.25 | 283 | 3.54 | <.001 | |
| Mild TBI with LOC vs OI | 3.54 | 0.85 | 291 | 4.16 | <.001 | |
| Mild TBI with LOC vs OI X Time (linear) | −13.89 | 4.17 | 300 | −3.33 | .001 | |
| Mild TBI with LOC vs OI X Time (quadratic) | 11.58 | 3.66 | 299 | 3.16 | .002 | |
| Group [F(2, 290) = 8.69 p < .001] | ||||||
| Group X Time (linear) [F(2, 301) = 5.56, p = .004] | ||||||
| Group X Time (quadratic) [F(2, 301) = 5.06, p = .007] | ||||||
TBI = Traumatic Brain Injury; OI = Orthopedic Injury; LOC = Loss of consciousness; PCS = Postconcussive symptoms.
Acknowledgements
This work was supported by grants HD44099 and HD39834 from the National Institutes of Health to the first author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest that require disclosure.
6. References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2001. [Google Scholar]
- Alexander MP. Minor traumatic brain injury: A review of physiogenesis and psychogenesis. Seminars in Clinical Neuropsychiatry. 1997;2:177–187. doi: 10.1053/SCNP00200177. [DOI] [PubMed] [Google Scholar]
- American Association for Automotive Medicine . The Abbreviated Injury Scale (AIS)-1990 Revision. American Association for Automotive Medicine; Des Plaines: 1990. [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th Ed. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Asarnow RF, Satz P, Light R, Zaucha K, Lewis R, McCleary C. The UCLA study of mild head injury in children and adolescents. In: Michel ME, Broman S, editors. Traumatic head injury in children. Oxford University Press; New York: 1995. pp. 117–146. [Google Scholar]
- Ashwal S, Tong KA, Obenaus A, Holshouser BA. Advanced neuroimaging techniques in children with traumatic brain injury. In: Anderson VA, Yeates KO, editors. Pediatric traumatic brain injury: New frontiers in clinical and translational research. Cambridge University Press; New York: 2010. pp. 68–93. [Google Scholar]
- Ayr LK, Yeates KO, Taylor HG, Browne M. Dimensions of post-concussive symptoms in children with mild traumatic brain injuries. Journal of the International Neuropsychological Society. 2009;15:19–30. doi: 10.1017/S1355617708090188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow KM, Crawford S, Stevenson A, Sandhu SS, Belanger F, Dewey D. A prospective epidemiological study of post-concussion syndrome in pediatric mild traumatic brain injury. Pediatrics. 2011;126:e374–e381. doi: 10.1542/peds.2009-0925. [DOI] [PubMed] [Google Scholar]
- Bazarian JJ, McClung J, Shah MN, Cheng YT, Flesher W, Kraus J. Mild traumatic brain injury in the United States, 1998-2000. Brain Injury. 2005;19:85–91. doi: 10.1080/02699050410001720158. [DOI] [PubMed] [Google Scholar]
- Bigler ED. Neuropsychology and clinical neuroscience of persistent post-concussive syndrome. Journal of the International Neuropsychological Society. 2008;14:1–22. doi: 10.1017/S135561770808017X. [DOI] [PubMed] [Google Scholar]
- Bijur PE, Haslum M. Cognitive, behavioral, and motoric sequelae of mild head injury in a national birth cohort. In: Broman S, Michel ME, editors. Traumatic head injury in children. Oxford University Press; 1995. pp. 147–164. [Google Scholar]
- Binder LM. Persisting symptoms after mild head injury: A review of the postconcussive syndrome. Journal of Clinical and Experimental Neuropsychology. 1986;8:323–346. doi: 10.1080/01688638608401325. [DOI] [PubMed] [Google Scholar]
- Byles J, Byrne C, Boyle MH, Oxford OR. Ontario Child Health Study: Reliability and validity of the General Functioning Scale of the McMaster Family Assessment Device. Family Process. 1988;27:97–104. doi: 10.1111/j.1545-5300.1988.00097.x. [DOI] [PubMed] [Google Scholar]
- Carroll LJ, Cassidy JD, Holm L, Kraus J, Coronado VG. Methodological issues and research recommendations for mild traumatic brain injury: The WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine. 2004a;(Suppl. 43):113–125. doi: 10.1080/16501960410023877. [DOI] [PubMed] [Google Scholar]
- Carroll LJ, Cassidy JD, Peloso PM, Borg J, von Holst H, Holm L, Paniak C, Pépin M. Prognosis for mild traumatic brain injury: Results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. Journal of Rehabilitation Medicine. 2004b;(Suppl. 43):84–105. doi: 10.1080/16501960410023859. [DOI] [PubMed] [Google Scholar]
- Dikmen SS, Levin HS. Methodological issues in the study of mild head injury. Journal of Head Trauma Rehabilitation. 1993;8:30–37. [Google Scholar]
- Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002-2006. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; Atlanta, GA: 2010. [Google Scholar]
- Fay GC, Jaffe KM, Polissar NL, Liao S, Martin KM, Shurtleff HA, Rivara JB, Winn JR. Mild pediatric traumatic brain injury: A cohort study. Archives of Physical Medicine and Rehabilitation. 1993;74:895–901. [PubMed] [Google Scholar]
- Fay TB, Yeates KO, Taylor HG, Bangert B, Dietrich A, Nuss KE, Rusin J, Wright M. Cognitive reserve as a moderator of postconcussive symptoms in children with complicated and uncomplicated mild traumatic brain injury. Journal of the International Neuropsychological Society. 2009;16:94–105. doi: 10.1017/S1355617709991007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giza CC, Hovda DA. The neurometabolic cascade of concussion. Journal of Athletic Training. 2001;36:228–235. [PMC free article] [PubMed] [Google Scholar]
- Kashluba S, Paniak C, Casey JE. Persistent symptoms associated with factors identified by the WHO Task Force on Mild Traumatic Brain Injury. The Clinical Neuropsychologist. 2008;22:195–208. doi: 10.1080/13854040701263655. [DOI] [PubMed] [Google Scholar]
- Levin HS, Hanten G, Roberson G, Li X, Ewing-Cobbs L, Dennis M, Chapman S, Max JE, Hunter J, Schachar R, Luerssen TG, Swank P. Prediction of cognitive sequelae based on abnormal computed tomography findings in children following mild traumatic brain injury. Journal of Neurosurgery: Pediatrics. 2008;1:461–470. doi: 10.3171/PED/2008/1/6/461. [DOI] [PubMed] [Google Scholar]
- Light R, Asarnow R, Satz P, Zucha K, McCleary C, Lewis R. Mild closed-head injury in children and adolescents: Behavior problems and academic outcomes. Journal of Consulting and Clinical Psychology. 1998;66:1023–1029. doi: 10.1037//0022-006x.66.6.1023. [DOI] [PubMed] [Google Scholar]
- Lishman WA. Physiogenesis and psychogenesis in the post-concussion syndrome. British Journal of Psychiatry. 1988;153:460–469. doi: 10.1192/bjp.153.4.460. [DOI] [PubMed] [Google Scholar]
- McKinlay A. Controversies and outcomes associated with mild traumatic brain injury in childhood and adolescence. Child: care, health, and development. 2009;36:3–21. doi: 10.1111/j.1365-2214.2009.01006.x. [DOI] [PubMed] [Google Scholar]
- McKinlay A, Kyonka EGE, Grace RC, Horwood LJ, Fergusson DM, MacFarlane MR. An investigation of the pre-injury risk factors associated with children who experience traumatic brain injury. Injury Prevention. 2009;16:31–35. doi: 10.1136/ip.2009.022483. [DOI] [PubMed] [Google Scholar]
- Miller IW, Bishop DS, Epstein NB, Keitner GI. The McMaster Family Assessment Device: Reliability and validity. Journal of Marital and Family Therapy. 1985;11:345–356. [Google Scholar]
- Mittenberg W, Wittner MS, Miller LJ. Postconcussion syndrome occurs in children. Neuropsychology. 1997;11:447–452. doi: 10.1037//0894-4105.11.3.447. [DOI] [PubMed] [Google Scholar]
- Moos RH, Fenn CB, Billings AG, Moos BI. Assessing life stressors and social resources: Applications to alcoholic patients. Journal of Substance Abuse. 1989;1:135–152. doi: 10.1016/s0899-3289(88)80017-8. [DOI] [PubMed] [Google Scholar]
- Osler T, Bakker SP, Long WA. A modification of the injury severity score that both improves accuracy and simplifies scoring. Journal of Trauma. 1997;43:922–925. doi: 10.1097/00005373-199712000-00009. [DOI] [PubMed] [Google Scholar]
- Ponsford J, Willmott C, Rothwell A, Cameron P, Ayton G, Nelms R, Curran C, Ng KT. Cognitive and behavioral outcomes following mild traumatic head injury in children. Journal of Head Trauma Rehabilitation. 1999;14:360–372. doi: 10.1097/00001199-199908000-00005. [DOI] [PubMed] [Google Scholar]
- Ponsford J, Willmott C, Rothwell A, Cameron P, Kelly A-M, Nelms R, Curran C, Ng K. Factors influencing outcome following mild traumatic brain injury in adults. Journal of the International Neuropsychological Society. 2000;6:568–579. doi: 10.1017/s1355617700655066. [DOI] [PubMed] [Google Scholar]
- Satz P. Mild head injury in children and adolescents. Current Directions in Psychological Science. 2001;10:106–109. [Google Scholar]
- Satz P, Zaucha K, McCleary C, Light R, Asarnow R. Mild head injury in children and adolescents: A review of studies (1970-1995) Psychological Bulletin. 1997;122:107–131. doi: 10.1037/0033-2909.122.2.107. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Dietrich A, Nuss K, Wright M, Rusin J, Bangert B, Yeates KO. Post-concussive symptoms in children with mild traumatic brain injury. Neuropsychology. 2010;24:148–159. doi: 10.1037/a0018112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich M. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Teasdale G, Jennett B. Assessment of coma and impaired consciousness: A practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- Wade S, Taylor HG, Drotar D, Stancin T, Yeates KO. Childhood traumatic brain injury: Initial impact on the family. Journal of Learning Disabilities. 1996;29:652–661. doi: 10.1177/002221949602900609. [DOI] [PubMed] [Google Scholar]
- Wilde EA, McCauley SR, Hunger JV, Bigler ED, Levin HS. Diffusion tensor imaging of acute mild traumatic brain injury in adolescents. Neurology. 2008;70:948–955. doi: 10.1212/01.wnl.0000305961.68029.54. [DOI] [PubMed] [Google Scholar]
- Williams DH, Levin HS, Eisenberg HM. Mild head injury classification. Neurosurgery. 1990;27:422–428. doi: 10.1097/00006123-199009000-00014. [DOI] [PubMed] [Google Scholar]
- Woodrome SE, Yeates KO, Taylor HG, Rusin J, Bangert B, Dietrich A, Nuss KE, Wright M. Coping strategies as a predictor of post-concussive symptoms in children with mild traumatic brain injury versus mild orthopedic injury. Journal of the International Neuropsychological Society. 2011;17:317–326. doi: 10.1017/S1355617710001700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. World Health Organization; Geneva: 1992. [Google Scholar]
- Yeates KO. Mild traumatic brain injury and postconcussive symptoms in children and adolescents. Journal of the International Neuropsychological Society. 2010;16:953–960. doi: 10.1017/S1355617710000986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeates KO, Luria J, Bartkowski H, Rusin J, Martin L, Bigler ED. Post-concussive symptoms in children with mild closed-head injuries. Journal of Head Trauma Rehabilitation. 1999;14:337–350. doi: 10.1097/00001199-199908000-00003. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG. Neurobehavioural outcomes of mild head injury in children and adolescents. Pediatric Rehabilitation. 2005;8:5–16. doi: 10.1080/13638490400011199. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Drotar D, Wade SL, Klein S, Stancin T, Schatschneider C. Pre-injury family environment as a determinant of recovery from traumatic brain injuries in school-age children. Journal of the International Neuropsychological Society. 1997;3:617–630. [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Rusin J, Bangert B, Dietrich A, Nuss K, Wright M, Nagin DS, Jones BL. Longitudinal trajectories of post-concussive symptoms in children with mild traumatic brain injuries and their relationship to acute clinical status. Pediatrics. 2009;123:735–743. doi: 10.1542/peds.2008-1056. [DOI] [PMC free article] [PubMed] [Google Scholar]