Abstract
College students are highly susceptible to the H1N1 virus, yet previous studies suggest that college students perceive themselves at low risk for the flu. We surveyed 514 undergraduates to assess their perceptions of H1N1 flu risk and opinions about flu vaccines. A third of respondents stated that they were not at risk of getting the H1N1 flu because they were young. Responses indicated a distrust of the safety and effectiveness of influenza vaccinations; only 15.8% of participants planned on receiving H1N1 vaccination. Top reasons for refusing the H1N1 vaccine included questioning vaccine safety and effectiveness, and concerns about potential serious and/or benign side effects. Top reasons for H1N1 vaccination acceptance included receiving a doctor recommendation for the vaccine, having previously gotten a seasonal vaccine, and being at high-risk for influenza. Our findings suggest that college students are inaccurate in assessing their risk level and are unlikely to seek vaccinations.
Keywords: H1N1 influenza, influenza vaccination, college students, flu risk perception
An outbreak of a novel strain of influenza (H1N1) reached pandemic status in spring of 2009. The first batches of a vaccine for the new H1N1 strain were released in October of 2009 [1]. We had the unique opportunity to study students’ risk perceptions in a university setting during this period of extensive media coverage and heightened vigilance due to the H1N1 pandemic. College students are more susceptible to the H1N1 virus due to close living conditions in residence halls [2], social contact in and out of the classroom [3-5], and the fact that younger people are more likely to get the H1N1 flu [1,6]. While vaccination is an effective strategy to reduce influenza cases [7], influenza vaccination rates prior to the pandemic were typically low among college students [8].
Vaccinations against influenza are effective. Vaccination is associated with significant reductions in doctor visits, better school performance, and less days of missed class/work for college students [7]. Thus, immunization provides the best preventative strategy against the influenza virus [1,9]. Despite this, even the most effective vaccine is ineffective if people are not willing to get themselves vaccinated [10]. Unfortunately, the general public is distrustful of pandemic flu vaccines [11].
Multiple studies have shown that a motivation for flu vaccine refusal of a novel flu vaccine is fear of side effects [12-15]. Many people also believe that the vaccination will not be effective [12,14,16] or that the novel vaccines have not received adequate testing [13,15] and may be harmful and weaken the immune system [16]. Still others are unconcerned about the flu and simply do not want the vaccine [12,14]. Vaccine acceptance is generally driven by self-perceived risk; if people feel that they are low risk, they are unlikely to receive flu vaccinations [17]. By contrast, people who are receptive to flu vaccinations are likely to be so because they want protection for themselves and their families [12-14] and flu vaccine acceptance is correlated with beliefs about vaccine effectiveness and safety [15,16]. In addition, flu vaccination acceptance is increased when one has been advised to by a doctor or other health authority [2,13,14,18]. Demographic variables are also related to vaccination acceptance, with older age and chronic illness being predictors [7,10,12,14,18,19].
College students are at particular risk for H1N1 influenza. During a pandemic, universities are threatened by the possibility of rapid influenza transmission because of their large young adult population and close social contact [1,4,5]. Students living in on-campus residences are at even higher risk of becoming ill due to close proximity living conditions [2]. Data based on laboratory-confirmed cases of H1N1 flu suggest higher infection rates in younger age groups [6], and people under the age of 25 were one of the key groups recommended by the CDC to receive the 2009 H1N1 vaccine [1].
In the present study, we surveyed undergraduate college students on their perceptions of their H1N1 flu risk and their attitudes regarding vaccinations. Given the heightened media activity during the H1N1 pandemic of 2009, we wished to determine rates of likelihood to receive vaccinations and major reasons for vaccine refusal in this at risk group.
Method
Participants
514 adults (245 males, 268 females, 1 declined to report gender) between the ages of 18 and 48 (mean age = 20.0 years, SD = 4.0) participated in this study. The study took place at Northern Kentucky University (NKU) during the peak of the H1N1 2009 pandemic (October to December). Self-reported racial-ethnic make-up included 466 Caucasians, 27 African-Americans, 4 Hispanics, 4 Asians, and 13 who reported “other”. 112 participants lived on campus, while 400 lived off campus. Participants were recruited from an introductory psychology course and received partial course credit for their participation. In the psychology department, 820 students were eligible to participate in this survey, resulting in a 63% response rate. All volunteers provided informed consent prior to participating and the NKU IRB approved this study.
NKU has a population of over 15,000 students. The first NKU student tested positive for H1N1 influenza on August 31, 2009. By November, NKU had recorded 36 confirmed cases and 22 probable cases of H1N1 influenza. Updated information was posted on the NKU website homepage including influenza information, preventative and avoidant strategies, and the current number of confirmed and probable cases on the NKU campus. The H1N1 nasal mist vaccine was available on campus in October and the H1N1 injection vaccine was available in December.
Materials and Procedure
H1N1 Flu Information Questionnaire
This 50-item questionnaire provided a measure of college students’ knowledge of the H1N1 flu, vaccination history, plans to receive vaccinations and reasoning, and perceptions of flu risk. Participants respond to yes/no questions and questions on a 7-point Likert scale ranging from “not at all” to “very much.” These questions were partly derived from a previous survey [20] and questions specific to college students were added as necessary.
Procedure
Individuals viewed web-based announcements describing this study and volunteers were informed that the study purpose was to examine the opinions of college students about risks of the flu. The 50-question web-based survey was anonymous.
Criterion Measures and Data Analyses
College students’ perceptions of flu risk, opinions about flu vaccines, general health habits and other related questions were examined using Mann-Whitney tests for non-parametric data. SPSS 17.0 was used to conduct all analyses with alpha level set at .05.
Results
For all participants, 54.3% of respondents felt that they had control over their flu risk because they engaged in various protective behaviors (e.g., washing hands often). 29.4% said they would still attend classes or exams, even if they became sick with the flu. 51.6% said they were not concerned about getting the H1N1 virus. Further, 72.8% of respondents believed they were not at risk for becoming seriously ill if they developed the H1N1 flu. For those students who felt they were not at risk for getting the H1N1 flu, top reasons for belief in decreased risk included that they were healthy (50%) and that they take precautions (e.g., using hand sanitizer) (41.1%). 32.5% of respondents between ages 18 and 24 felt that they were not at risk of getting the H1N1 flu because they were young.
Regarding H1N1 vaccination, of all participants, 15.8% reported that they were planning on getting an H1N1 vaccine, 53.1% reported that they were not planning on getting an H1N1 vaccine, and 31.1% reported that they were still undecided as to whether or not they were getting an H1N1 vaccine. Table 1 illustrates that participants who had received a recommendation from a doctor to get a flu vaccination were significantly more likely to get the H1N1 vaccination, z = -5.30, p < .001. In addition, individuals who had received a seasonal influenza vaccine the previous year were significantly more likely to receive the H1N1 vaccine, z = -6.71, p < .001. Students who had a chronic medical condition (diabetes, asthma, cardiac disease) were at high risk for influenza, and were also more likely to receive the H1N1 vaccine, z = -2.24, p = .025. Students who lived on-campus were no different from students who lived off-campus in their plans to receive an H1N1 vaccine, z = -.699, p = .484, despite the fact that students living on-campus are at higher risk.
Table 1.
Characteristics of study participants
| Characteristics | n | n (%) intending to be vaccinated | p |
|---|---|---|---|
| Gender | |||
| Male | 245 | 42 (17.1) | .417 |
| Female | 268 | 39 (14.6) | |
| Total | 513 | ||
| Class | |||
| Freshman | 313 | 50 (16.0) | .883 |
| Sophomore | 109 | 14 (12.8) | |
| Junior | 48 | 6 (12.5) | |
| Senior | 36 | 8 (22.2) | |
| Continuing education | 4 | 2 (50.0) | |
| Total | 510 | ||
| Doctor recommendation | |||
| Recommended | 199 | 55 (27.6) | < .001 |
| Not recommended | 264 | 21 (8.0) | |
| Couldn't remember | 51 | 5 (9.8) | |
| Total | 514 | ||
| Previous seasonal vaccine | |||
| Yes last year | 111 | 40 (36.0) | <.001 |
| Not last year | 368 | 39 (10.6) | |
| Couldn't remember | 35 | 2 (5.7) | |
| High risk status | |||
| Yes | 84 | 19 (22.6) | .025 |
| No | 430 | 62 (14.4) | |
| Total | 514 | ||
| Living arrangements | |||
| On-campus | 112 | 21 (18.8) | .484 |
| Off-campus | 400 | 59 (14.6) | |
| Total | 512 |
*Mann-Whitney U test
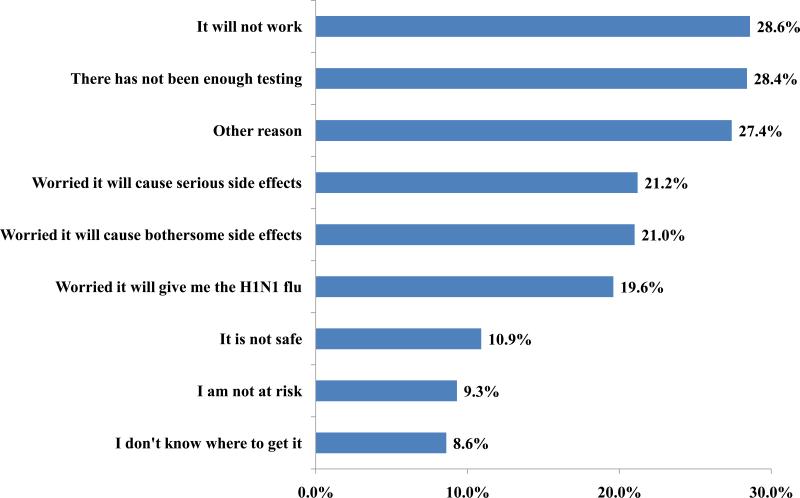
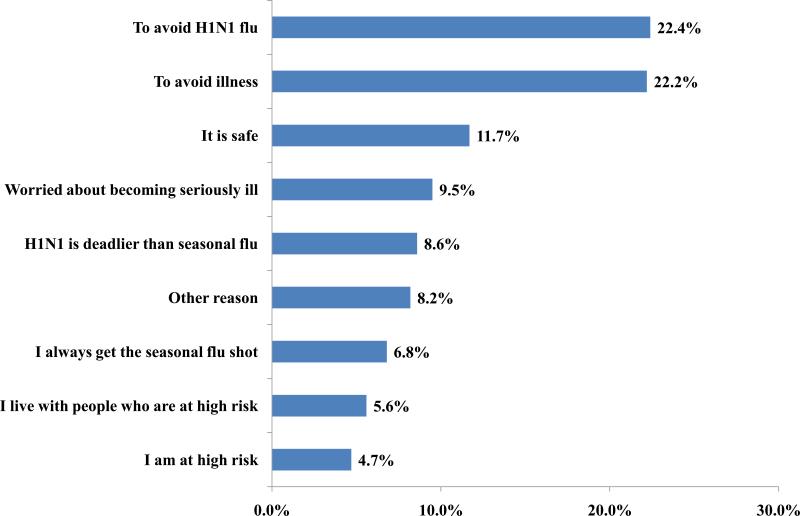
Figure 1 illustrates the top reasons for refusing H1N1 vaccination. Many participants thought that the vaccine would not work (29%), that there had not been enough testing (29%), that the vaccine would give them the H1N1 flu (20%), and/or they were worried about bothersome and serious side effects (21%). Figure 2 illustrates the top reasons stated for H1N1 vaccination for those receptive individuals. These individuals stated that they sought vaccination to avoid the H1N1 flu (22.4%), to avoid illness (22.2%), and/or they thought it was safe (11.7%).
Figure 1.
Reasons for refusing the H1N1 vaccine for those unwilling to be vaccinated
Figure 2.
Reasons for accepting the H1N1 vaccine for those willing to be vaccinated
Discussion
This research examined college students’ perceptions of H1N1 influenza risk and likelihood to receive a vaccination. The results showed that even though these students were exposed to an extensive public health campaign for pandemic H1N1 influenza, they were unlikely to get vaccinated to protect themselves. Many of our participants were unconcerned about the H1N1. Alarmingly, many students reported that they would still attend class even if they were sick with the flu. Misconceptions about vaccine usefulness and safety were common. Top reasons for refusing the H1N1 vaccine included questioning vaccine safety and concerns about side effects. Moreover, our participants were inaccurate in assessing their risk level, since the H1N1 strain is more likely to sicken a younger person. Additionally, there were no differences in H1N1 vaccination acceptance between students living on- and off-campus, even though on-campus students are at higher risk.
This research reveals that college students lack knowledge of vaccination safety, effectiveness, and necessity. Psychologists who study attitudes and persuasion may play an important role in addressing this serious public health concern, as behavioral and psychological factors are of great importance in marketing vaccinations [4]. Greater understanding is needed of the factors that motivate people to receive vaccinations, especially since they are effective in reducing disease occurrence.
Highlights.
Only 15.8% of participants were planning on receiving an H1N1 vaccination
32.5% between ages 18-24 felt they weren't at risk for H1N1 because they were young
Many students reported they would still attend class if they had influenza
Students questioned H1N1 vaccine safety, effectiveness, and potential side effects
Vaccination predictor: doctor recommendation, previous vaccination, being high-risk
Acknowledgements
This research was supported by NIH grants R15AA019795 and P20RR016481 awarded to Cecile A. Marczinski.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention [Internet] [2011 Jul 13];CDC guidance for responses to influenza for institutions of higher education during the 2009-2010 academic year. 2009 Available from: http://www.cdc.gov/h1n1flu/institutions/guidance.
- 2.Uddin M, Cherkowski GC, Liu G, Zhang J, Monto AS, Aiello AE. Demographic and socioeconomic determinants of influenza vaccination disparities among university students. J Epidemiol Community Health. 2010;64:808–13. doi: 10.1136/jech.2009.090852. [DOI] [PubMed] [Google Scholar]
- 3.Iuliano AD, Reed C, Guh A, Desai M, Dee DL, Kutty P, Gould H, Sotir M, Grant G, Lynch M, Mitchell T, Getchell J, Shu B, Villanueva J, Lindstrom S, Massoudi MS, Siebold J, Silverman PR, Armstrong G, Swerdlow DL. Notes from the field: Outbreak of 2009 pandemic influenza A (H1N1) virus at a large public university in Delaware, April-May 2009. Clin Infect Dis. 2009;49:1811–20. doi: 10.1086/649555. [DOI] [PubMed] [Google Scholar]
- 4.Kar-Purkayastha I, Ingram C, Roche M. The importance of school and social activities in the transmission of influenza A(H1N1)v: England, April-June 2009. Euro Surveill. 2009;14(33):1–4. doi: 10.2807/ese.14.33.19311-en. [DOI] [PubMed] [Google Scholar]
- 5.Van D, McLaws M, Crimmins J, MacIntyre CR, Seale H. University life and pandemic influenza: Attitudes and intended behaviour of staff and students towards pandemic (H1N1) 2009. BMC Public Health. 2010;130(10):1–9. doi: 10.1186/1471-2458-10-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization [Internet] [2011 July 13];Clinical management of human infection with new influenza A(H1N1) virus: Initial guidance. 2009 Available from: http://www.who.int/csr/resources/publications/swineflu/clinical_managementH1N1_21_May_2009.pdf.
- 7.Nichol K, D'Heilly S, Ehlinger E. Influenza vaccination among college and university students. Arch Pediatr Adolesc Med. 2008;162(12):1113–8. doi: 10.1001/archpedi.162.12.1113. [DOI] [PubMed] [Google Scholar]
- 8.Merrill RM, Kelley TA, Cox E, Layman AB, Layton BJ, Lindsay R. Factors and barriers influencing influenza vaccination among students at Brigham Young University. Med Sci Monit. 2010;16(2):PH29–34. [PubMed] [Google Scholar]
- 9.Gallaher W. Towards a sane and rational approach to management of influenza H1N1 2009. Virol J. 2009;6(51) doi: 10.1186/1743-422X-6-51. doi:10.1186/1743-422X-6-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaygisiz U, Gaygisiz E, Ozkan R, Lajunen T. Why were Turks unwilling to accept the A/H1N1 influenza-pandemic vaccination? People's beliefs and perceptions about the swine flu outbreak and vaccine in the later stage of the epidemic. Vaccine. 2010;29(2):329–33. doi: 10.1016/j.vaccine.2010.10.030. [DOI] [PubMed] [Google Scholar]
- 11.Velan B, Kaplan G, Ziv A, Boyko V, Lerner-Geva L. Major motives in non-acceptance of A/H1N1 flu vaccination: the weight of rational assessment. Vaccine. 2011;29:1173–1179. doi: 10.1016/j.vaccine.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Barrière J, Vanjak D, Kriegel I, Otto J, Peyrade F, Estève M, Chamorey E. Why were Turks unwilling to accept the A/H1N1 influenza-pandemic vaccination? People's beliefs and perceptions about the swine flu outbreak and vaccine in the later stage of the epidemic. Vaccine. 2010;28:7030–4. [Google Scholar]
- 13.Bults M, Beaujean DJMA, Richardus JH, van Steenbergen JE, Voeten HACM. Pandemic influenza A (H1N1) vaccination in the Netherlands: Parental reasoning underlying child vaccination choices. Vaccine. 2011 doi: 10.1016/j.vaccine.2011.06.075. doi:10.1016/j.vaccine.2011.06.75. [DOI] [PubMed] [Google Scholar]
- 14.Alkuwari MG, Aziz NA, Nazzal ZA, Al-Nuaimi SA. Pandemic influenza A/H1N1 vaccination uptake among health care workers in Qatar: motivators and barriers. Vaccine. 2011;29:2206–11. doi: 10.1016/j.vaccine.2010.08.093. [DOI] [PubMed] [Google Scholar]
- 15.Seale H, Kaur R, Wang Q, Yang P, Zhang Y, Wang X, Li X, Zhang H, Zhang Z, MacIntyre CR. Acceptance of a vaccine against pandemic influenza A (H1N1) virus amongst healthcare workers in Beijing, China. Vaccine. 2011;29:1605–10. doi: 10.1016/j.vaccine.2010.12.077. [DOI] [PubMed] [Google Scholar]
- 16.Esteves-Jaramillo A, Omer SB, Gonzalez-Diaz E, Salmon DA, Hixson B, Navarro F, Kawa-Karasik S, Frew P, Morfin-Otero R, Rodriguez-Noriega E, Ramirez Y, Rosas A, Acosta E, Varela-Badillo V, Del Rio C. Acceptance of a vaccine again novel influenza A(H1N1) virus among health care workers in two major cities in Mexico. Arch Med Res. 2009;40(8):705–11. doi: 10.1016/j.arcmed.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seale H, Heywood AE, McLaws M, Ward KF, Lowbridge CP, Van D, MacIntyre CR. Why do I need it? I am not at risk! Public perceptions towards the pandemic (H1N1) 2009 vaccine. BMC Infect Dis. 2010;10:99. doi: 10.1186/1471-2334-10-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferrante G, Baldissera S, Moghadam PF, Carrozzi G, Trinito MO, Salmaso S. Surveillance of perceptions, knowledge, attitudes and behaviors of the Italian adult population (18-69 year) during the 2009-2010 A/H1N1 influenza pandemic. Eur J Epidemiol. 2011;26(3):211–9. doi: 10.1007/s10654-011-9576-3. [DOI] [PubMed] [Google Scholar]
- 19.Sunil TS, Zottarelli LK. Student utilization of a university 2009 H1N1 vaccination clinic. Vaccine. 2011;29:4687–9. doi: 10.1016/j.vaccine.2011.04.110. [DOI] [PubMed] [Google Scholar]
- 20.Grant VJ, Le Saux NL, Plint AC, Correll R, Gaboury I, Ellis E, Tam TWS. Factors influencing childhood influenza immunization. Can Med Assoc J. 2003;168(1):39–41. [PMC free article] [PubMed] [Google Scholar]