Abstract
Aims:
To evaluate the diagnostic utility of virtual bronchoscopy, multiplanar reformatted images, and minimal-intensity projection in assessing airway stenoses.
Settings and Design:
It was a prospective study involving 150 patients with symptoms of major airway disease.
Materials and Methods:
Fifty-six patients were selected for analysis based on the detection of major airway lesions on fiber-optic bronchoscopy (FB) or routine axial images. Comparisons were made between axial images, virtual bronchoscopy (VB), minimal-intensity projection (minIP), and multiplanar reformatted (MPR) images using FB as the gold standard. Lesions were evaluated in terms of degree of airway narrowing, distance from carina, length of the narrowed segment and visualization of airway distal to the lesion.
Results:
MPR images had the highest degree of agreement with FB (Κ = 0.76) in the depiction of degree of narrowing. minIP had the least degree of agreement with FB (Κ = 0.51) in this regard. The distal visualization was best on MPR images (84.2%), followed by axial images (80.7%), whereas FB could visualize the lesions only in 45.4% of the cases. VB had the best agreement with FB in assessing the segment length (Κ = 0.62). Overall there were no statistically significant differences in the measurement of the distance from the carina in the axial, minIP, and MPR images. MPR images had the highest overall degree of confidence, namely, 70.17% (n = 40).
Conclusion:
Three-dimensional reconstruction techniques were found to improve lesion evaluation compared with axial images alone. The technique of MPR images was the most useful for lesion evaluation and provided additional information useful for surgical and airway interventions in tracheobronchial stenosis. minIP was useful in the overall depiction of airway anatomy.
Keywords: Airway, bronchoscopy, computed tomography, virtual
Introduction
Flexible bronchoscopy is an invasive procedure and has chances of complications.[1] Noninvasive techniques to depict airway lesions by multidetector computed tomography (MDCT) are important for interventional procedures and for determining treatment response and follow-up.[2,3] The aim of the study was to evaluate the performance of multiplanar reformatted (MPR), minimal-intensity projection (minIP), and virtual bronchoscopy (VB) images in terms of lesion detection, degree and length of narrowing, segment length assessment, distal airway depiction, and overall diagnostic confidence, using fiber-optic bronchoscopy (FB) as the gold standard.
Materials and Methods
Study design and sample size
Out of 150 patients presenting with major airway respiratory symptoms, 56 patients (31 males and 25 females; age range, 7–50 years) were selected on the basis of (1) the detection of a lesion in the major airways on routine axial 5-mm chest CT scans on a 40-row scanner (Somatom Sensation 40, Siemens, Erlangen, Germany) and (2) the performance of an FB.
For the CT scans, the kVp was 120 kV and the effective collimation was 40 × 0.6 mm. Images with thickness of 1 mm with 0.5 mm increment were reconstructed using a 30f smooth kernel. Virtual bronchoscopy images were generated using endoscopic shaded surface display (SSD) views. The lesion was viewed from the proximal and the distal perspective. Measurements were not possible in the endoscopic view. Multiplanar reformats were generated in orthogonal, nonorthogonal, and curved planes on a 3-D workstation and viewed using mediastinal and lung window settings. Thick-slab minIP images to include all the major airways (thickness range 25–55 cm) were reconstructed and viewed in various projections. Semi-quantitative grading was used to analyze the degree of narrowing, distal visualization, segment length, and overall confidence. Degree of narrowing was graded as grade-0: no narrowing, grade-1: <30% narrowing, grade-2: 30%-60% narrowing, grade-3: >60% but nonocclusive narrowing, grade-4: complete occlusion. Segment length of narrowing was graded as grade-0: no narrowing, grade-1: <1/3 of the involved airway segment, grade-2: 1/3 to 2/3 of the involved airway segment, grade-3: >2/3 of the involved airway segment. The length of narrowing on the thick-slab minIP images was assessed by measuring the maximal projectional length. Distal visualization was graded as grade-0: distal airway not visualized, grade-1: visualization of distal airway. The above-mentioned parameters of various reconstruction techniques were compared with those of FB using kappa statistics. Overall degree of confidence for evaluation of the lesion delineation was based on the detection of stenosis and depiction of lesion causing the stenosis as extrinsic, intramural, or intraluminal; and was graded as score-0: nondiagnostic, score-1: intermediate confidence, score-2: good confidence. Three radiologists independently analyzed the axial, MPR, and minIP images and were blinded to the findings of other image sets and the findings of bronchoscopy.
Causes of stenosis
Twenty-five patients had carcinoma lung, 3 had tracheal tumors, 12 had carcinoid tumor of the bronchus, 6 had tracheal stenosis, and 10 had posttuberculous bronchial stenosis.
Results
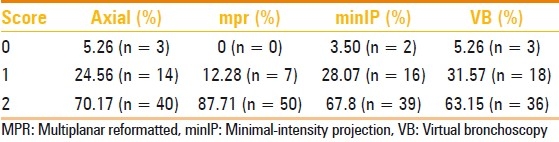
MPR images had the highest degree of agreement with FB in the estimation of degree of narrowing [Κ = 0.76]. MinIP had the least degree of correlation with FB [Κ = 0.51] [Tables 1 and 2] [Figure 1]. There was poor agreement of all these techniques with FB due to the fallacy of FB as a gold standard as it could visualize the distal airway in only 26 (45.45%) cases [Table 2]. The distal visualization was best on MPR images (84.21%) [Figure 2], and therefore the stenotic segment length evaluation was also the most reliable on MPR images [Figures 3 and 4]. VB and minIP were less effective in detecting distal airways. VB had a fallacious good agreement with FB in assessing the segment length (Κ = 0.62) [Table 2] as VB and FB both had poor distal visualizations. There was no statistically significant difference in the measurement of the distance from the carina on the axial, minIP, and MPR images. There were 12 lesions in our study group, wherein the difference in distance measured on the axial and MPR images and on the minIP images, was more than 5 mm. These included 6 lesions in the left upper lobe, 2 in the lingular lobe, and 4 lesions in the right upper lobe bronchi [Figure 5]. MPR images had the highest degree of confidence (87.71%), whereas VB had the least (63.15%) [Table 3].
Table 1.
Percentage of underestimation and overestimation of degree of narrowing using various reconstruction techniques
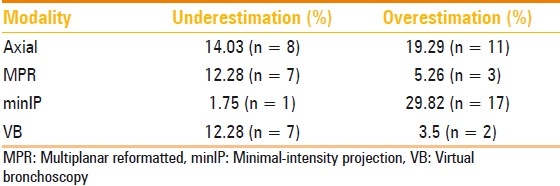
Table 2.
Comparison of agreement with FB (Kappa) of various reconstruction techniques
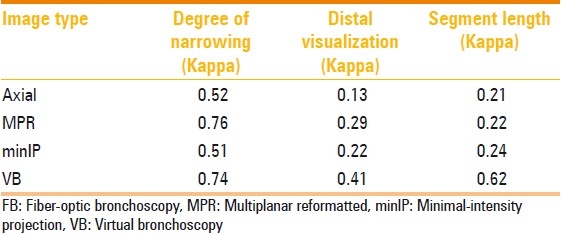
Figure 1 (A, B).
Tracheomalacia. Sagittal MPR (A) and minIP (B) images show a wavy contour of the trachea in this case of tracheomalacia with narrowing (arrow) in its upper portion. The minIP image overestimates the degree of narrowing and the segment length
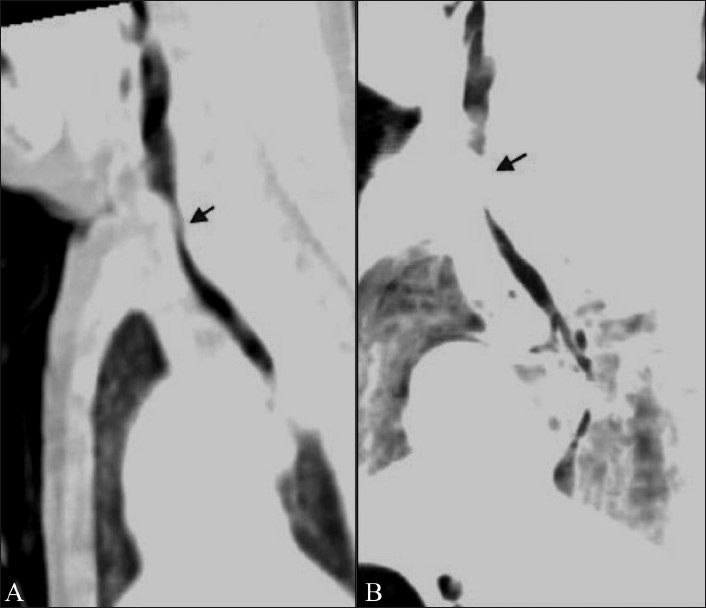
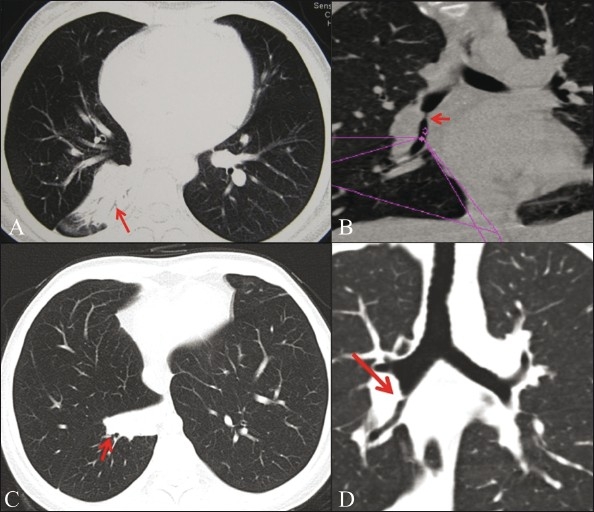
Figure 2 (A-D).
Fluid-filled bronchi. Axial mediastinal window image (A) shows occlusion (arrow) of the left main bronchus (LMB) and collapse of the left lung (arrowhead). Left anterior oblique MPR mediastinal window image (B) shows the occlusion of the LMB (arrow) and fluid filled bronchi in the collapsed left lung (arrowhead), but the lung window MPR image (C) shows a collapsed left lung with a tiny speck on air in the LMB (arrow). Left anterior coronal oblique minIP image (D) shows the cut off of the LMB only without distal airway visualization
Figure 3.
Post-tuberculous bronchial narrowing. Axial image (A) shows collapse (arrow) of the right lower lobe (RLL). MPR image (B) shows a short segment narrowing (arrow) in the bronchus intermedius. Post-balloon dilatation axial image (C) shows improvement in the RLL aeration (arrow) with residual collapse of the medial basal segment (arrow). Coronal MPR image (D) shows improvement in the caliber of the previously narrowed bronchus intermedius (arrow)
Figure 4 (A, B).
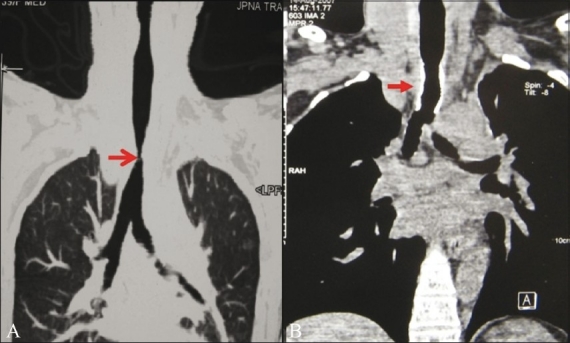
Post-intubation stenosis: Curved coronal lung window MPR image (A) shows segmental narrowing of the trachea (arrow). Post-metallic stenting soft tissue coronal MPR image (B) shows improvement in tracheal caliber (arrow)
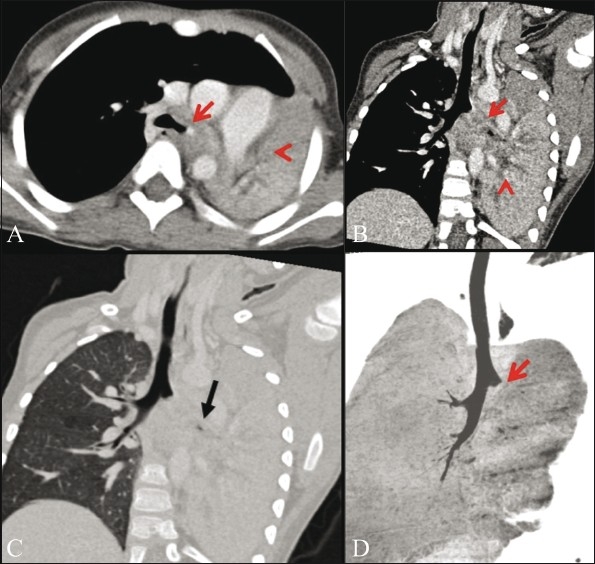
Figure 5 (A, B).
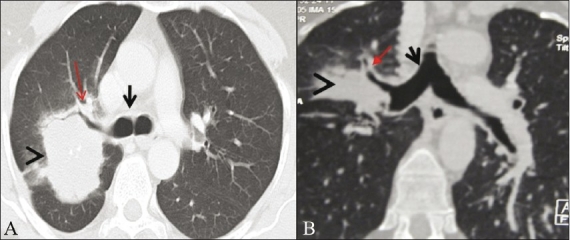
Bronchogenic carcinoma. Axial (A) and coronal MPR (B) lung window images show the presence of a mass in the posterior segment of the right upper lobe (arrowhead), which encases the right upper lobe (RUL) bronchus (arrow). The distance of the mass from the carina (short arrow) the on the axial image (1.5 cm) was less than on the MPR image (3.3 cm)
Table 3.
Overall diagnostic confidences of various reconstruction techniques
Discussion
The grading of the degree of stenosis by MPR was as accurate as VB in our study probably because we used various orthogonal and nonorthogonal planes, unlike a previous study by Hoppe et al.[4] that compared only coronal and sagittal MPR individually with VB and found VB to be more accurate than MPR. The relatively poor agreement of axial images and FB was noted in bronchi parallel to the imaging plane. minIP had the highest tendency to overestimate the degree and length of stenosis, contrary to what has been reported in previous studies, which may possibly be attributed to differences in the slab thickness used in various studies.[5,6] The distance from the carina measured on the axial images correlated well with those measured on the MPR and minIP images in the bronchus intermedius and the right and left lower lobe bronchi but not in the right and left upper lobe and lingular lobe bronchi. Although VB is considered superior to FB for distal airway visualization,[7] MPR and axial images performed better than VB. Our observations that MPR images are the best for measuring the degree of narrowing, the depiction of airways distal to long segment narrowing as well as depiction of fluid-filled airways distal to obstruction, are similar to earlier studies [Figure 2].[8,9] The overall degree of confidence in characterizing airway lesions was the best with MPR images as they showed subtle distortions due to external causes with more clarity. Similar observations have been made by Boiselle et al.[10]
Conclusion
MPR images are accurate in the detection of lesions, the depiction of degree of narrowing, distal visualization, in the evaluation of the segment of narrowing and in the measurement of the distance of the lesion from the carina in selected locations. VB has no distinct role in the evaluation of airway lesions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Pereira W, Jr, Kovnat DM, Snider GL. A prospective cooperative study of complications following bronchoscopy. Chest. 1978;73:813–6. doi: 10.1378/chest.73.6.813. [DOI] [PubMed] [Google Scholar]
- 2.Dialani V, Ernst A, Sun M, Lee KS, Kopman DF, Litmanovich D, et al. MDCT detection of airway stent complications: Comparison with bronchoscopy. Am J Roentgenol. 2008;191:1576–80. doi: 10.2214/AJR.07.4031. [DOI] [PubMed] [Google Scholar]
- 3.McAdams HP, Palmer SM, Erasmus JJ, Patz EF, Connolly JE, Goodmann PC, et al. Bronchial anastomotic complications in lung transplant recipients: Virtual bronchoscopy for noninvasive assessment. Radiology. 1998;209:689–95. doi: 10.1148/radiology.209.3.9844660. [DOI] [PubMed] [Google Scholar]
- 4.Hoppe H, Walder B, Sonnenschein M, Vock P, Dinkel HP. Multidetector CT virtual bronchoscopy to grade tracheobronchial stenosis. Am J Roentgenol. 2002;178:1195–200. doi: 10.2214/ajr.178.5.1781195. [DOI] [PubMed] [Google Scholar]
- 5.Bernhardt LR, Welet T, Doehring W, Kropf S, Bernhardt TM. Diagnostic potential of virtual bronchoscopy advantages in comparison with axial CT rows, MPR and MinIP. Eur Radiol. 2000;10:981–8. doi: 10.1007/s003300051049. [DOI] [PubMed] [Google Scholar]
- 6.Bernhardt UR, Welte T, Budinger M, Bernhardt TM. Comparison of 3-D virtual bronchoscopy in patients with carcinoma esophagus invading the trachea. Br J Radiol. 1998;71:1271–8. doi: 10.1259/bjr.71.852.10319000. [DOI] [PubMed] [Google Scholar]
- 7.Fleiter T, Merkle EM, Aschoff AJ, Lang G, Stein M, Gorlich J, et al. Comparison of real time virtual and fiberoptic bronchoscopy in patients with bronchial carcinoma: Opportunities and limitations. Am J Roentgenol. 1997;169:1591–5. doi: 10.2214/ajr.169.6.9393172. [DOI] [PubMed] [Google Scholar]
- 8.Heyer CM, Kagel T, Lemburg SP, Nikolas V, Reiger CL. Evaluation of tracheobronchial anomalies in children using low-dose multidetector CT: Report of a 13-year-old boy with a tracheal bronchus and recurrent pulmonary infections. Pediatr Pulmonol. 2004;38:168–73. doi: 10.1002/ppul.20077. [DOI] [PubMed] [Google Scholar]
- 9.LoCicero J, 3rd, Costello P, Campos CT, Francalancia N, Dushay KM, Silvestri RC, et al. Spiral CT with multiplanar and three-dimensional reconstructions accurately predicts tracheobronchial pathology. Ann Thorac Surg. 1996;62:811–7. doi: 10.1016/s0003-4975(96)00532-7. [DOI] [PubMed] [Google Scholar]
- 10.Boiselle PM, Reynolds KF, Ernst A. Multiplanar and three-dimensional imaging of the central airways with multidetector CT. Am J Roentgenol. 2002;179:301–8. doi: 10.2214/ajr.179.2.1790301. [DOI] [PubMed] [Google Scholar]


