Abstract
Non-invasive positive pressure ventilation or non-invasive ventilation (NIV) has emerged as a simpler and safer alternative to invasive mechanical ventilation in patients developing acute postoperative respiratory failure. The benefits of NIV as compared to intubation and mechanical ventilation include lower complications, shorter duration of hospital stay, reduced morbidity, lesser cost of treatment and even reduced mortality rates. However, its use may not be uniformly applicable in all patient groups. This article reviews the indications, contraindications and evidence supporting the use of NIV in individual patient groups in the postoperative period. The anaesthesiologist needs to recognise the subset of patients most likely to benefit from NIV therapy so as to apply it most effectively. It is equally important to promptly identify signs of failure of NIV therapy and be prepared to initiate alternate ways of respiratory support. The author searched PubMed and Ovid MEDLINE, without date restrictions. Search terms included Non-invasive ventilation, postoperative and respiratory failure. Foreign literature was included, though only articles with English translation were used.
Keywords: Non-invasive ventilation, postoperative, respiratory failure
INTRODUCTION
The postoperative period is fraught with complications related to the respiratory and cardiovascular systems, especially in the ‘at-risk’ patient population group. The severity of these complications depends upon the preoperative respiratory status as well as intraoperative factors, such as the type and site of surgery performed and the anaesthesia that the patient is exposed to.[1,2] With rapid advances in the medical care, better treatment options available and increasing longevity of our population, the anaesthesiologist may often be confronted with such medical challenges in the perioperative period. Hence, management begins with careful screening and selection of the at-risk patient, optimising his physiological status in the preoperative period, continuing to provide lung protective ventilation in the intraoperative period and extending optimal respiratory care into the postoperative period. The mainstay of treatment of postoperative respiratory failure so far has been reintubation and mechanical ventilation, which are associated with complications like pneumonia, infections, increased costs, morbidity and mortality. Thus, the anaesthesiologist is left with the dilemma of optimally managing postoperative respiratory failure while avoiding the attendant complications of reintubation. Non-invasive ventilation (NIV) has been used successfully in such instances. This article focuses on the benefits of NIV for the management and treatment of acute postoperative respiratory failure.
IDENTIFYING THE AT-RISK POPULATION
A study by Silva et al.[1] studied 521 patients over 5 years and reported that thoracic , cardiac and upper abdominal surgeries were associated with the highest risk of postoperative pulmonary complications. The predictors of postoperative respiratory failure in their study included the site of surgery, duration of anaesthesia (more than 3.5 hours) and the severity of ASA classification (grades III and IV). Other studies have also reported that, the at-risk population are those with underlying lung diseases, age >60 years, ASA functional status II or greater, obese patients, those with underlying congestive cardiac failure and obstructive sleep apnoea syndromes.[2] The risk of postoperative respiratory failure is especially greater if such patients are made to undergo long duration, high-risk surgical procedures like upper abdominal or thoracic surgeries. Gas exchange failure results from reduction of phrenic output, disruption of muscle output and pain.[2] General anaesthesia, by reducing the muscular tone, also adds to pump failure. Other insults like sepsis, shock, ischaemia and reperfusion injury and blood transfusions worsen lung injury leading to worsening of gas exchange.[2] Obese patients are at an increased risk of developing postoperative respiratory failure. Pulmonary atelectasis is reported to develop in 85 to 90% of obese patients during the first minutes of anaesthesia and can persist for even 24 hours after the end of the surgical procedure.[3] They are also particularly vulnerable to respiratory instability, episodic desaturations in supine position and the respiratory depressant effects of sedatives and opiates leading to postoperative hypoxaemia, hypercapnia and respiratory failure.[4,5]
ROLE OF NON-INVASIVE VENTILATION IN THE POSTOPERATIVE PERIOD
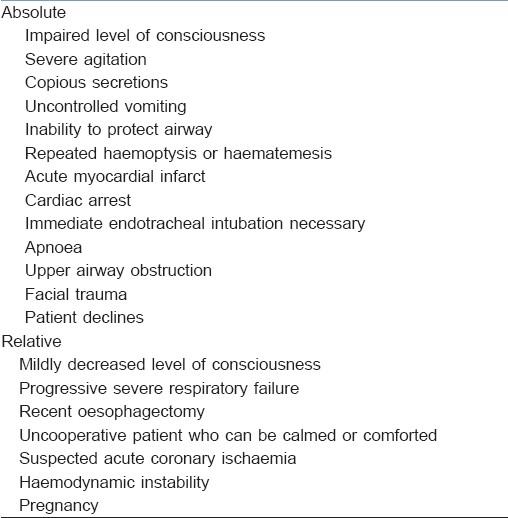
NIV has opened up new avenues in the management of respiratory failure in the postoperative patient. The data on the role of NIV for acute respiratory failure in the postoperative setting are selective, with clear evidence in certain patient groups who are undergoing specific surgical procedures. It is important to carefully rule out any of the contraindications to the application of NIV [Table 1][6] before starting its use. The benefits of NIV have been clearly established in the intensive care unit (ICU) especially in patients with hypercapnic respiratory failure secondary to chronic obstructive pulmonary disease (COPD) or to chest wall deformities, cardiogenic pulmonary oedema and as an aid to facilitate weaning from ventilatory support.[7] The evidence for the beneficial effects of NIV in postoperative patients mainly comes from studies in patients who have undergone major thoracoabdominal or cardiac surgeries. Here, NIV may be applied prophylactically, i.e., in the at-risk postoperative patient to prevent acute respiratory failure from developing, or therapeutically, i.e., to support the patient who has already developed postoperative respiratory failure. In addition, patients at risk of developing acute postoperative pulmonary oedema or postoperative airway obstruction also benefit from trials of NIV.
Table 1.
Contraindications to the use of non-invasive ventilation
Abdominal surgery
Abdominal surgery is most often followed by diaphragmatic dysfunction and a marked decrease in vital capacity, which often leads to atelectasis and hypoxaemia.[8] Surgeries which result in dysfunction of diaphragmatic movement tend to worsen respiratory impairment. Data suggest that 30 to 50% of patients undergoing abdominal surgeries develop hypoxaemia postoperatively, and 8 to 10% require endotracheal intubation postoperatively.[9] The beneficial effects of postoperative NIV have been demonstrated following laparoscopic surgeries for cholecystectomy, bariatric surgeries and thoracoabdominal surgeries for aneurysm repair.[10–12]
Prophylactic non-invasive ventilation
There have been several studies demonstrating the benefits of prophylactically applied NIV in patients undergoing abdominal surgeries. Stock et al.[13] reported that patients receiving continuous positive airway pressure (CPAP) and incentive spirometry after cholecystectomy by laparotomy had a significantly improved functional residual capacity (FRC) and lesser roentgenographic evidence of atelectasis than those treated with coughing and deep breathing exercises. Similarly, patients treated prophylactically with CPAP of 10 cm H2O for 12 to 24 hours a day after thoracoabdominal surgery (aneurysm of thoracoabdominal aorta) had significantly better oxygenation rates and shorter lengths of ICU and hospital stay.[12] In morbidly obese patients undergoing abdominal surgeries, studies have clearly demonstrated the benefits of prophylactic use of NIV in the postoperative period. Joris et al.[11] demonstrated that the application of bilevel positive airway pressure (BiPAP) set at 12 and 4 cm PEEP: Positive end-expiratory pressure H2O significantly improved the peak expiratory flow rate, the forced vital capacity and the oxygen saturation on the first postoperative day. In these patients, the beneficial effects of NIV was attributed to an improvement in lung inflation, prevention of alveolar collapse and reduced inspiratory threshold load.[11]
Therapeutic non-invasive ventilation
In a large randomised controlled study conducted across 15 ICUs in Italy, Squadarone et al.[9] studied 209 patients who underwent laparotomy longer than 90 minutes and developed postoperative hypoxaemia in the first hour after surgery. These patients were then randomised into 2 groups, one received CPAP (7.5 cmH2O) via helmet and the other received standard care, including oxygen. They concluded that use of CPAP significantly reduced the incidence of endotracheal intubation and other severe complications like pneumonia, sepsis, anastomotic leaks, infection and death. In fact, this study was terminated after the first interim analysis because of the significant benefits achieved in the CPAP group. Other smaller and observational studies have also reported benefits with the use of NIV, especially in avoiding intubation, reducing complications and length of ICU stay.[14,15] In patients undergoing liver resection surgeries, the postoperative use of NIV resulted in improved paO2/FiO2 and paCO2 levels, lower rates of re-intubation as well as lower respiratory-cause mortality and all-cause mortality.[16] Conti et al. matched 25 patients who received NIV therapy for acute respiratory failure following abdominal surgery with 25 matched controls who were treated with face mask and reported that the NIV group had better gas exchange, tolerance and lesser complications than the other group.[17]
There may be some concerns of increased anastomotic leakage in patients who receive NIV after gastrointestinal anastomoses, especially following upper gastrointestinal anastomosis, where use of NIV may be considered a relative contraindication [Table 1]. However, there have been several studies on the use of NIV in patients who had undergone procedures like oesophagectomies, digestive surgeries, gastrectomies and colostomies showing increased benefits and reduced morbidity with use of NIV postoperatively. Studies by Joris et al., Pessoa et al. and Kindgen-Milles et al. have not reported any problems with suture integrity.[11,12,18] Some studies have even reported that the incidence of anastomotic leak was lower in the NIV group.[9,19] Huerta et al. studied 159 patients treated with NIV following gastrojejunostomy as part of a Roux-en-Y gastric bypass procedure and reported that there was no correlation between NIV use and major anastomotic leakage postoperatively.[20] A word of caution though; while using NIV in patients following upper gastrointestinal anastomosis, gastric inflation pressures should be carefully monitored as the risk of anastomotic leakage seems to be more if very high insufflation pressures are applied (more than 25 cm H2O). Use of the Ryle's tube on drainage may be useful to detect excessive insufflation, should it occur.
Thoracic surgery
There is significant risk for postoperative lung dysfunction following lung resection surgeries as a result of several factors like inhibition of phrenic nerve, pain, reduced muscle tone due to general anaesthesia and loss of functioning lung parenchyma. These can lead to sputum retention, lobar atelectasis, pneumonia and respiratory failure.[21–23]
Prophylactic non-invasive ventilation
In a randomised study conducted by Perrin et al.,[24] the prophylactic use of NIV in patients with severe preoperative airflow obstruction (forced expiratory volume FEV1 <70%) undergoing lobectomy for carcinoma of the lung resulted in significant improvements in pulmonary function. In this study, patients who received NIV in the 7 days prior to surgery and 3 days after surgery had significantly higher paO2 and better forced vital capacity (FVC) and FEV1 on days 1, 2 and 3 after surgery. This group of patients also had a significantly lesser duration of hospital stay. Aguilo et al. studied 10 patients who received a trial of NIV following lung resection surgery and found that patients on NIV had improved oxygenation, which continued even one hour after withdrawing NIV support, with no associated increase in pleural air leaks.[25]
Therapeutic non-invasive ventilation
Lefebvre et al.[26] reported that of the patients at risk for severe complications following lung resection surgeries, 16.3% eventually developed acute respiratory failure, which were both hypoxaemic and hypercapnic types. The overall success rate of NIV in this group was 85.3%; however, the mortality associated with NIV failure was 46.1%. In the same study, presence of cardiac co-morbidities and lack of initial response to NIV were found to be independently associated with NIV failure. Auriant et al.[27] studied 48 patients who developed respiratory failure after lung resection. In this trial, 20.8% of patients assigned to the NIV group required intubation and invasive ventilation compared to 50% patients in the no-NIV group. Mortality rates too were significantly lower in the NIV group (13% vs 38%).
Cardiac surgery
Respiratory failure after cardiac surgery is associated with morbidity, mortality and decreased quality of life. The incidence of respiratory failure varies from 5 to 20% in the literature.[28–29] In a study on 5,798 patients undergoing cardiac surgery over a 6-year period, Filsoufi et al.[30] reported that combined valve and coronary artery bypass graft was associated with the highest incidence of respiratory failure, followed by aortic procedures. The overall reported incidence of respiratory failure in the first group was 9.1% and mortality rate was 15.5%. Patients with lower preoperative ejection fraction, those undergoing combined cardiac surgical procedures and those with severe SAPS II scores were reportedly at the greatest risk of developing postoperative respiratory failure.[31]
Prophylactic non-invasive ventilation
In a study on the prophylactic use of nasal CPAP following cardiac surgeries, Zarbock et al. randomised 500 patients to receive either intermittent nasal CPAP at 10 cm H2O every 4 hours or prophylactic nasal CPAP at 10 cm H2O for at least 6 hours. They concluded that use of CPAP significantly improved arterial oxygenation, reduced pulmonary complications and ICU readmission rates.[32] Kilger et al.[31] noted that 35% of the cardiac surgical patients studied over four years developed post extubation respiratory failure and intermittent NIV benefited 33% of these patients. Matte et al.[33] reported that when preventive NIV was used in 96 patients in the first 2 days after cardiac surgery, there was improved oxygenation and lower reduction of lung volumes. However, the incidence of atelectasis was similar (12–15%) to the non-NIV group.
Therapeutic non-invasive ventilation
There have been only a few studies reporting the use of NIV for treatment of respiratory failure following cardiac surgeries. Olper et al.[34] studied 85 patients who received NIV for treatment of respiratory failure following cardiac surgery and reported that NIV was a safe and feasible solution for postoperative acute respiratory failure, even when applied after discharge from the ICU. Pasquina et al. reported that when CPAP was applied in patients who developed postoperative atelectasis (based on roentgenographic evidence) following cardiac surgeries, there was considerable improvement of atelectasis, as determined by radiological scores.[35]
Acute postoperative pulmonary oedema
Causes of acute pulmonary oedema in the postoperative period include non-cardiogenic causes like fluid maldistribution, neurogenic causes, anaphylaxis, acute lung injury and negative pressure pulmonary oedema following upper airway obstruction or residual neuromuscular blockade. The cardiogenic causes include acute left ventricular failure. There are many reports of successful use of NIV in patients developing acute pulmonary oedema from cardiogenic or non-cardiogenic causes.[36] A meta-analysis of 15 trials by Masip et al. reported that NIV significantly reduced the need for intubation and mortality in patients with acute cardiogenic pulmonary oedema.[37] A Cochrane review in 2008 on the use of negative pressure pulmonary ventilation (NPPV) in cardiogenic pulmonary oedema collected data on 1,071 patients in 21 studies and reported that CPAP is an effective and safe intervention for the treatment of adult patients with acute cardiogenic pulmonary oedema. The use of NIV reduced need for endotracheal intubation and hospital mortality without increasing the risks of further ischaemic events.[38]
Potential postoperative airway obstruction
Obstructive sleep apnoea is one of the commonest causes of upper airway obstruction in the postoperative period and occur typically in the obese or patients with pre-existing neurological disorders. A review of the inciting causes, clinical findings, onset and duration, electrocardiographic findings, laboratory findings and chest radiographic findings will aid in the differential diagnoses of these conditions. Besides treatment of the primary problem and use of drugs like diuretics and inhaled β-agonists, supplemental aids for respiratory support include oxygen, use of NIV or invasive mechanical ventilation (in severe cases). Rennotte et al. reported a series of 16 adult patients undergoing various operative procedures who had documented evidence of obstructive sleep apnoea syndrome. The first two patients developed serious complications postoperatively. Following this, the remaining patients were instituted on nasal CPAP prior to and following surgery on a continuous basis for 24 to 48 hours and none of these patients suffered any complications. They also had a comparable postoperative length of stay as other non-obstructive sleep apnoea patients.[39] In a study by Friedman et al., application of NIV in children following adenoidectomy or tonsillectomy improved respiratory symptoms in all children who were at an increased risk of postoperative airway obstruction.[40] Also, in patients undergoing laryngotracheal surgeries, the use of NIV benefits patients by providing ventilatory support and airway stenting till tracheal oedema and pulmonary dysfunction resolves, at the same time avoiding the risk of further tracheal mucosal injury from tracheal intubation.[41]
Missed opportunities?
Despite the many reported benefits of NIV in the perioperative period, the utilisation rates for NIV vary enormously among different acute care hospitals, even within the same region. NIV is often underutilised in many hospitals. Sweet et al.[42] in their 6-year review of patients who had acute respiratory failure, noted that of all the patients who met the criteria for a trial of NIV, only 34% received it and the remaining 66% were intubated instead. The perceived reasons for lower utilisation rates include lack of physician knowledge, insufficient respiratory therapist training and inadequate equipment. Maheshwari et al.[43] suggest that educational programmes directed at individual institutions may be useful to enhance and optimise utilisation rates. In a telephonic survey on the practice of NIV in the postoperative period among 60 French ICUs, it was reported that 69% of the respondents used NIV as the first choice for the treatment of acute postoperative respiratory failure and 54% for the treatment of acute postoperative atelectasis.[44] In a study by Carlucci et al.[45] on the incidence of use and effectiveness of NIV in clinical practice, when 42 ICUs were surveyed over a 3-week period, it was found that NIV was attempted as the first-line therapy for acute respiratory failure in only 16% patients. In a questionnaire survey on the practice patterns of NIV use in India, Chawla et al.[46] reported that NIV was used almost exclusively in the ICU setting and COPD was the most common reason for initiating NIV in clinical practice. While it is not clear how many postoperative patients were reported by the respondents, NIV was not commonly used for post extubation respiratory failure. There were wide variations in the site of its use, patterns of use, protocols followed and even monitoring of patients on NIV and nearly 30% of Indian clinicians reportedly do not perform baseline blood gas measurements before initiating NIV.[46]
MODES OF NON-INVASIVE VENTILATION
For providing NIV, most clinicians prefer using a standard, portable non-invasive machine. These machines mostly deliver pressures during expiration (end expiratory positive airway pressure [EPAP]) and/or at inspiration (inspiratory positive airway pressure [IPAP]). When EPAP is applied alone, it is referred to as CPAP mode and when both EPAP and IPAP are applied together, it is referred to as NPPV mode. Some machines have additional timed modes that can be used to ensure delivery of pressure support (PS) at prefixed time intervals. Ventilators used to ventilate intubated patients may also be used to deliver NIV and some of the newer invasive ventilators have facilities to provide NIV as well. Though most Indian physicians prefer using portable pressure ventilators for applying NIV, more recent users of NIV reportedly use conventional ventilators more often than their older colleagues.[46] If the older machines are used to provide NIV, they may constantly give ‘air-leak’ alarms as they are not designed to compensate for flow changes. This leak compensation mechanism, designed specifically on ventilators meant to provide NIV, basically consists of microprocessors in the ventilatory circuit which detect differences between inspiratory and expiratory tidal volumes over the initial breaths and then increase the peak inspiratory flow (without increasing inspiratory time), accordingly. If a conventional ventilator is used to provide NIV, the ASB (assisted spontaneous breathing) or the CPAP modes are commonly used. Here, the set CPAP and PS levels correspond to the EPAP and IPAP of the portable machine, respectively. It may be worthwhile remembering that the amount of PS set on the conventional ventilator delivers an additional PS above the set CPAP level, whereas the IPAP of the portable NIV machine is the pressure support inclusive of the EPAP that is set. Thus, pressure settings of 14 and 8 cm H2O on a portable machine, corresponds to 6 and 8 cm H2O when a conventional ventilator is used to deliver the same. If one wishes to deliver additional back up breaths to the patient, the synchronised intermittent mandatory ventilation (SIMV)-pressure control mode may be used. Here, the ventilation (or tidal volume) achieved in the patient is determined by the inspiratory pressure and PEEP set for the mandatory breaths, and the PS and CPAP set for the spontaneous breaths. Thus, in order to deliver NIV, the minimum features required on a conventional ventilator are modalities to deliver ASB, i.e., CPAP with provision of an additional PS during inspiration.
INTERFACES
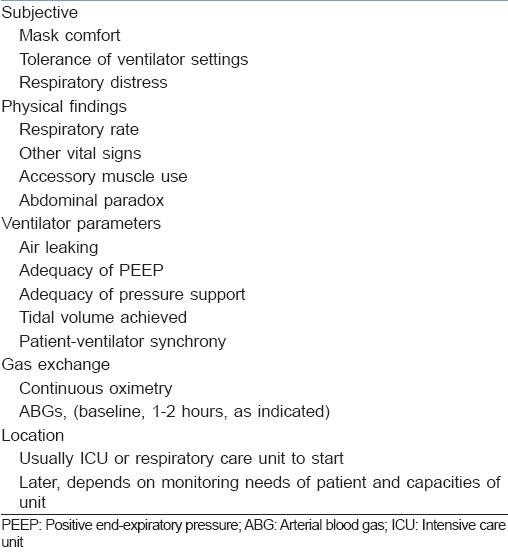
There are many interfaces available in the market today. While there is no evidence favouring the use of any one over the other,[47] oronasal masks are more commonly used than others, especially in Indian hospitals.[46] The other interfaces available are nasal masks, nasal pillows, full face masks and helmets. Holanda et al.[47] observed that while the full face mask avoided pain over the bridge of the nose and prevented air leaks around the eyes and mouth, they caused more oronasal dryness and claustrophobia. Kwok et al.[48] noted that in the dyspnoeic patient, nasal masks are less well tolerated than are oronasal masks. The most important factor to be taken into consideration while choosing the right mask is a good fit, patient comfort and mask tolerance. Thus, one may need to use several mask types and fits before choosing one most suited to an individual patient. It is advisable to gently allow the patient to get used to the mask by allowing him to hold the mask over his face and breathe into the mask against the positive pressure, till he feels comfortable. Then, it may be gently strapped onto his face. The monitoring parameters for adult patients on NIV for respiratory failure are as given in Table 2.[49]
Table 2.
Monitoring of patients on NIV in the postoperative period
GETTING STARTED
Trials of NIV in the postoperative period should always be provided in appropriately monitored locations. It is important to talk to the patient, explain the procedure and reassure the patient before initiating NIV. The patient must be propped up at least 30 degrees and have received adequate analgesia. It is advisable to begin with low PS as it usually takes a few minutes for the patient to accommodate to the pressure applied and synchronise his breathing with that of the machine. Once the patient starts to feel comfortable and breathing begins to improve, it is easier to gradually increase the PS and apply the straps onto the patient. The end points of the PSs applied must be always individualised till there is improvement in symptoms, reduced respiratory rates and good synchrony. An arterial blood gas should be obtained by 1 to 2 hours to verify clinical improvements. Normally, an inspiratory trigger of 1 to 2 l/min or –1 to –2 cm of H2O is applied, with moderate to maximal slope. EPAP levels of 4 cm and IPAP of 8 cm of H2O (4 cm above EPAP) are normally used at initiation. These may be gradually increased by increments of 1 to 2 cm till a maximum EPAP of 10 and IPAP of 25 cm of H2O. If higher pressures are required, it may be necessary to change the interface, adjust mask fit or even consider the need for possible intubation and invasive ventilation. The expiratory trigger is generally fixed at 0.8 to 1 seconds or between 40 to 60% of the peak flow rate.
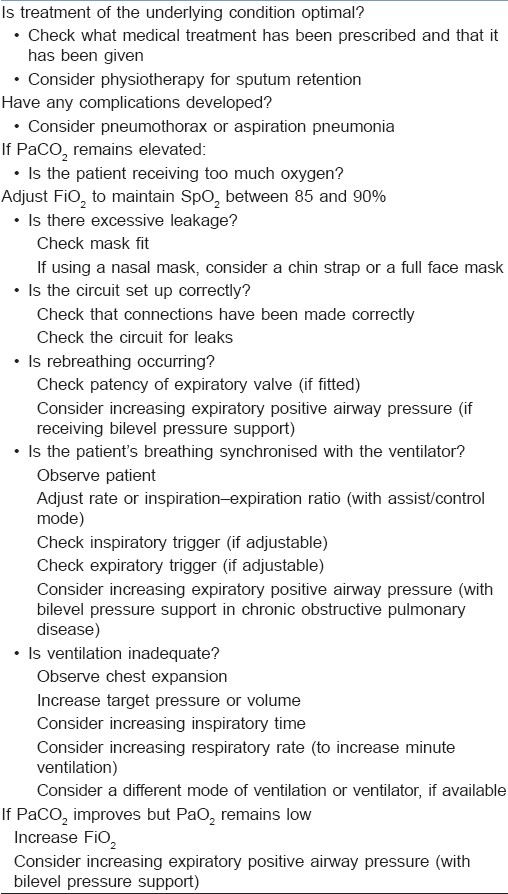
NON-INVASIVE VENTILATION FAILURE
While there is a clear role for the use of NIV in the postoperative period, it is important to carefully monitor these patients and recognise those who are not responding adequately. One may need to consider other factors like leaks in circuit, poor mask fit, inadequate trigger levels, etc., which may be readjusted for better results. Table 3 gives the recommendations of the British Thoracic Society Standards of Care Committee for trouble shooting in cases of non-improvement of patients on NIV.[50] However, if respiratory distress persists despite these measures, one may need to abandon the trial of NIV and consider intubation and mechanical ventilation instead. Two Indian studies which analysed outcome predictors for NIV failure used for post extubation respiratory failure found that the arterial oxygen pressure /fractional inspired oxygen (Pao2/Fio2) ratio and baseline parameter such as heart rate and respiratory rates at the time of initiation of NIV were indicative of the likelihood of success or failure after NIV use.[51,52] Wallet et al.[53] reported that the factors associated with NIV failure used in the treatment of postoperative acute respiratory insufficiency were a decrease in the paO2/FiO2 ratio after 1 hour of NIV use, development of nosocomial pneumonia and an increased simplified acute physiology score (SAPS) II score. Other studies from the ICU have reported that increased severity of the underlying illness, high acute physiology and chronic health evaluation (APACHE) II scores, presence of multiple organ dysfunctions, acute lung injury (ALI) or acute respiratory distress syndrome (ARDS), community-acquired pneumonia and shock have predicted failure of NIV therapy when used for the management of acute respiratory failure.[54]
Table 3.
Recommendations of the British Thoracic Society Standards of Care Committee for treatment failure in non-invasive ventilation
It is as important to recognise when to call off NIV therapy as it is to identify when to use it. A delay in intubation in these patients results in worse outcomes and higher mortality. In patients failing extubation after requiring mechanical ventilation longer than 48 hours, there have been conflicting reports of their benefits. In fact, Keenan et al.[55] showed no difference in rates of reintubation and mortality when NIV was compared with standard therapy. Esteban et al.[56] reported that NIV did not reduce rates of reintubation and in fact delayed the time to reintubation in patients developing respiratory failure, resulting in increased mortality.
CONCLUSION
In conclusion, the NIV has exciting new applications in the postoperative field today. This is no truer than in the ‘at-risk’ patient undergoing major thoracoabdominal surgery. In the past decade, the NIV has proven to be an effective alternative to invasive ventilation in the setting of moderate and severe acute postoperative respiratory failure. The use of NIV has not only reduced intubation rates with the attendant complications associated with mechanical ventilation, but has also reduced morbidity, length of hospital stay and mortality in these patients. This translates to huge benefits in costs of treatment too, especially in a country like ours where resources are limited and costs of therapy play a major role in deciding treatment options. NIV can be useful in peripheral setups and at primary level hospitals in our country if adequate paramedical staff and nurses are trained in the use, applications and monitoring. As with any other new therapeutic modality, to optimally apply NIV, a learning curve is necessary, and centres documenting their experience report better outcomes over time despite treating increasingly sicker patients.[57] Such centres are believed to achieve better outcomes as a result of a superior approach to patient selection, as well as to NIV application, titration and weaning. If the contraindications to the use of NIV are carefully ruled out and if used judiciously, under closed monitoring in selected patients, the NIV can be a very useful tool in the ever-increasing armamentarium of the anaesthesiologist.
LITERATURE SEARCH
The author searched PubMed and Ovid MEDLINE, without date restrictions. Search terms included Non-invasive ventilation, postoperative and respiratory failure. Foreign literature was included, though only articles with English translation were used.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Silva DR, Gazzana MB, Knorst MM. Merit of preoperative clinical findings and functional pulmonary evaluation as predictors of postoperative pulmonary complications. Rev Assoc Med Bras. 2010;56:551–7. doi: 10.1590/s0104-42302010000500016. [DOI] [PubMed] [Google Scholar]
- 2.Jaber S, Chanques G, Jung B. Postoperative noninvasive ventilation. Anesthesiology. 2010;112:453–61. doi: 10.1097/ALN.0b013e3181c5e5f2. [DOI] [PubMed] [Google Scholar]
- 3.Eichenberger A, Proietti S, Wicky S, Frascarolo P, Suter M, Spahn DR, et al. Morbid obesity and postoperative pulmonary atelectasis: An underestimated problem. Anesth Analg. 2002;95:1788–92. doi: 10.1097/00000539-200212000-00060. [DOI] [PubMed] [Google Scholar]
- 4.Taylor RR, Kelley TM, Elliott CG, Jensen RL, Jones SB. Hypoxemia after gastric bypass surgery for morbid obesity. Arch Surg. 1985;120:1298–302. doi: 10.1001/archsurg.1985.01390350078016. [DOI] [PubMed] [Google Scholar]
- 5.El-Solh A, Sikka P, Bozkanat E, Jaafar W, Davies J. Morbid obesity in the medical ICU. Chest. 2001;120:1989–97. doi: 10.1378/chest.120.6.1989. [DOI] [PubMed] [Google Scholar]
- 6.Peñuelas O, Frutos-Vivar F, Esteban A. Noninvasive positive-pressure ventilation in acute respiratory failure. CMAJ. 2007;177:1211–8. doi: 10.1503/cmaj.060147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.British Thoracic Society Standards of Care Committee. Noninvasive ventilation in acute respiratory failure. Thorax. 2002;57:192–211. doi: 10.1136/thorax.57.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dureuil B, Cantineau JP, Desmonts JM. Effects of upper or lower abdominal surgery on diaphragmatic function. Br J Anaesth. 1987;59:1230–35. doi: 10.1093/bja/59.10.1230. [DOI] [PubMed] [Google Scholar]
- 9.Squadrone V, Coha M, Cerutti E, Schellino M, Biolino P, Occella P, et al. Continuous positive airway pressure for treatment of postoperative hypoxia: A randomized controlled trial. JAMA. 2005;293:589–95. doi: 10.1001/jama.293.5.589. [DOI] [PubMed] [Google Scholar]
- 10.Stock M, Downs J, Gauer P, Alster J, Imrey P. Prevention of postoperative pulmonary complications with CPAP, incentive spirometry and conservative therapy. Chest. 2009;35:663–70. doi: 10.1378/chest.87.2.151. [DOI] [PubMed] [Google Scholar]
- 11.Joris J, Sottiaux T, Chiche J, Desaive C, Lamy M. Effect of bi-level positive airway pressure (BiPAP) on the postoperative pulmonary restrictive syndrome in obese patients undergoing gastroplasty. Chest. 1997;111:665–70. doi: 10.1378/chest.111.3.665. [DOI] [PubMed] [Google Scholar]
- 12.Kindgen-Milles D, Muller E, Buhl R, Bohner H, Ritter D, Sandmann W, et al. Nasal continuous positive airway pressure reduces pulmonary morbidity and length of hospital stay following thoracoabdominal aortic surgery. Chest. 2005;128:821–8. doi: 10.1378/chest.128.2.821. [DOI] [PubMed] [Google Scholar]
- 13.Stock M, Downs J, Gauer P, Alster J, Imrey P. Prevention of postoperative pulmonary complications with CPAP, incentive spirometry, and conservative therapy. Chest. 1985;87:151–7. doi: 10.1378/chest.87.2.151. [DOI] [PubMed] [Google Scholar]
- 14.Varon J, Walsh G, Fromm RJ. Feasibility of non-invasive mechanical ventilation in the treatment of acute respiratory failure in postoperative cancer patients. J Crit Care. 1998;13:55–7. doi: 10.1016/s0883-9441(98)80002-6. [DOI] [PubMed] [Google Scholar]
- 15.Jaber S, Delay J, Sebbane M, Chanques G, Jacquet E, Souche B, et al. Outcomes of patients with acute respiratory failure after abdominal surgery treated with non-invasive post-operative pressure ventilation. Chest. 2005;128:2688–95. doi: 10.1378/chest.128.4.2688. [DOI] [PubMed] [Google Scholar]
- 16.Narita M, Tanizawa K, Chin K, Ikai I, Handa T, Oga T, et al. Noninvasive Ventilation Improves the Outcome of Pulmonary Complications after Liver Resection. Intern Med. 2010;49:1501–7. doi: 10.2169/internalmedicine.49.3375. [DOI] [PubMed] [Google Scholar]
- 17.Conti G, Cavaliere F, Costa R, Craba A, Catarci S, Festa V, et al. Noninvasive positive pressure ventilation with different interfaces in patients with respiratory failure after abdominal surgery: A matched-control study. Respir Care. 2007;52:1463–71. [PubMed] [Google Scholar]
- 18.Pessoa KC, Araujo GF, Pinheiro AN, Ramos MR, Maia SC. Non-invasive ventilation in the immediate postoperative of gastrojejunal derivation with Roux-en-Y gastric bypass. Rev Bras Fisioter. 2010;14:290–5. [PubMed] [Google Scholar]
- 19.Michelet P, D’Journo XB, Seinaye F, Forel JM, Papazian L, Thomas P. Non-invasive ventilation for treatment of post-operative respiratory failure after esophagectomy. Br J Surg. 2009;96:54–60. doi: 10.1002/bjs.6307. [DOI] [PubMed] [Google Scholar]
- 20.Huerta S, DeShields S, Shpiner R, Li Z, Liu C, Sawicki M, et al. Safety and efficacy of postoperative continuous positive airway pressure to prevent pulmonary complications after Roux-en-Y gastric bypass. J Gastrointest Surg. 2002;6:354–8. doi: 10.1016/s1091-255x(01)00048-8. [DOI] [PubMed] [Google Scholar]
- 21.Ali J, Weisel RD, Layug AB, Kripke BJ, Hechtman HB. Consequences of postoperative alterations in respiratory mechanics. Am J Surg. 1974;128:376–82. doi: 10.1016/0002-9610(74)90176-7. [DOI] [PubMed] [Google Scholar]
- 22.Nunn JF. Respiratory aspects of anaesthesia. In: Nunn JF, editor. Applied respiratory physiology. 3rd ed. Cambridge: Butterworth; 1987. pp. 350–78. [Google Scholar]
- 23.Brown LK. Surgical considerations: Effects of surgery on lung function. In: Brown LK, editor. Pulmonary function tests in clinical and occupational lung disease. Orlando, FL: Grune and Stratton; 1986. pp. 341–51. [Google Scholar]
- 24.Perrin C, Jullien V, Venissac N, Berthier F, Padovani B, Guillot F, et al. Prophylactic use of non-invasive ventilation in patients undergoing lung resectional surgery. Respir Med. 2007;101:1572–8. doi: 10.1016/j.rmed.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 25.Aguilo R, Togores B, Pons S, Mateu R, Barbé F, Agusti A. Noninvasive ventilatory support after lung resectional surgery. Chest. 1997;112:117–21. doi: 10.1378/chest.112.1.117. [DOI] [PubMed] [Google Scholar]
- 26.Lefebvre A, Lorut C, Alifano M, Dermine H, Roche N, Gauzit R, et al. Noninvasive ventilation for acute respiratory failure after lung resection: An observational study. Intensive Care Med. 2009;35:663–70. doi: 10.1007/s00134-008-1317-z. [DOI] [PubMed] [Google Scholar]
- 27.Auriant I, Jallot A, Herve P, Cerrina J, Ladurie LF, Fournier LJ, et al. Noninvasive ventilation reduces mortality in acute respiratory failure following lung resection. Am J Respir Crit Care Med. 2001;164:1231–5. doi: 10.1164/ajrccm.164.7.2101089. [DOI] [PubMed] [Google Scholar]
- 28.Canver CC, Chanda J. Intraoperative and postoperative risk factors for respiratory failure after coronary bypass. Ann Thorac Surg. 2003;75:853–57. doi: 10.1016/s0003-4975(02)04493-4. [DOI] [PubMed] [Google Scholar]
- 29.Hein OV, Birnbaum J, Wernecke KD, Konertz W, Jain U, Spies C. Three-year survival after four major post-cardiac operative complications. Crit Care Med. 2006;34:2729–37. doi: 10.1097/01.CCM.0000242519.71319.AD. [DOI] [PubMed] [Google Scholar]
- 30.Filsoufi F, Rahmanian PB, Castillo JG, Chikwe J, Adams DH. Predictors of early and late outcomes of respiratory failure in contemporary cardiac surgery. Chest. 2008;133:713–21. doi: 10.1378/chest.07-1028. [DOI] [PubMed] [Google Scholar]
- 31.Kilger E, Mohnle P, Nassau K, Beiras-Fernandez A, Lamm P, Frey L, et al. Noninvasive mechanical ventilation in patients with acute respiratory failure after cardiac surgery. Heart Surg Forum. 2010;13:91–5. doi: 10.1532/HSF98.20091116. [DOI] [PubMed] [Google Scholar]
- 32.Zarbock A, Mueller E, Netzer S, Gabriel A, Feindt P, Kindgen- Milles D. Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications: A prospective, randomized, controlled trial in 500 patients. Chest. 2009;135:1252–9. doi: 10.1378/chest.08-1602. [DOI] [PubMed] [Google Scholar]
- 33.Matte P, Jacquet M, Vandyck M, Goenen M. Effects of conventional physiotherapy, continuous positive airway pressure and non-invasive ventilatory support with bilevel positive airway pressure after coronary artery bypass grafting. Acta Anaesthesiol Scand. 2000;44:75–81. doi: 10.1034/j.1399-6576.2000.440114.x. [DOI] [PubMed] [Google Scholar]
- 34.Olper L, Cabrini L, Landoni G, Rossodivita A, Nobile L, Monti G, et al. Non-invasive ventilation after cardiac surgery outside the intensive care unit. Minerva Anestesiol. 2010;76:1–6. [PubMed] [Google Scholar]
- 35.Pasquina P, Merlani P, Granier JM, Ricou B. Continuous positive airway pressure versus noninvasive pressure support ventilation to treat atelectasis after cardiac surgery. Anesth Analg. 2004;99:1001–8. doi: 10.1213/01.ANE.0000130621.11024.97. [DOI] [PubMed] [Google Scholar]
- 36.McConkey PP. Postobstructive pulmonary oedema--a case series and review. Anaesth Intensive Care. 2000;28:72–6. doi: 10.1177/0310057X0002800114. [DOI] [PubMed] [Google Scholar]
- 37.Masip J, Roque M, Sánchez B, Fernández R, Subirana M, Expósito JA. Noninvasive Ventilation in Acute Cardiogenic Pulmonary Edema Systematic Review and Meta-analysis. JAMA. 2005;294:3124–30. doi: 10.1001/jama.294.24.3124. [DOI] [PubMed] [Google Scholar]
- 38.Vital FM, Saconato H, Ladeira MT, Sen A, Hawkes CA, Soares B, et al. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary edema. Cochrane Database Syst Rev. 2008;3:CD005351. doi: 10.1002/14651858.CD005351.pub2. [DOI] [PubMed] [Google Scholar]
- 39.Rennotte MT, Baele P, Aubert G, Rodenstein DO. Nasal continuous positive airway pressure in the perioperative management of patients with obstructive sleep apnea submitted to surgery. Chest. 1995;107:367–74. doi: 10.1378/chest.107.2.367. [DOI] [PubMed] [Google Scholar]
- 40.Friedman O, Chidekel A, Lawless ST, Cook SP. Postoperative bilevel positive airway pressure ventilation after tonsillectomy and adenoidectomy in children- a preliminary report. Int J Pediatr Otorhinolaryngol. 1999;51:177–80. doi: 10.1016/s0165-5876(99)00260-8. [DOI] [PubMed] [Google Scholar]
- 41.Hertzog JH, Siegel LB, Hauser GJ, Dalton HJ. Noninvasive positive-pressure ventilation facilitates tracheal extubation after laryngotracheal reconstruction in children. Chest. 1999;116:260–3. doi: 10.1378/chest.116.1.260. [DOI] [PubMed] [Google Scholar]
- 42.Sweet DD, Naismith A, Keenan SP, Sinuff T, Dodek PM. Missed opportunities for noninvasive positive pressure ventilation: A utilization review. J Crit Care. 2008;23:111–7. doi: 10.1016/j.jcrc.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 43.Maheshwari V, Paioli D, Rothaar R, Hill NS. Utilization of non-invasive ventilation in acute care hospitals: A regional survey. Chest. 2006;129:1226–33. doi: 10.1378/chest.129.5.1226. [DOI] [PubMed] [Google Scholar]
- 44.Chanques G, Jaber S, Delay JM, Perrigault PF, Lefrant JY, Eledjam JJ. Phoning study about postoperative practice and application of non-invasive ventilation. Ann Fr Anesth Reanim. 2003;22:879–85. doi: 10.1016/j.annfar.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 45.Carlucci A, Richard JC, Wysocki M, Lepage E, Brochard L. Noninvasive versus conventional mechanical ventilation.An epidemiologic survey. Am J Respir Crit Care Med. 2001;163:874–80. doi: 10.1164/ajrccm.163.4.2006027. [DOI] [PubMed] [Google Scholar]
- 46.Chawla R, Sidhu US, Kumar V, Nagarkar S, Brochard L. Noninvasive ventilation: A survey of practice patterns of its use in India. Indian J Crit Care Med. 2008;12:163–9. doi: 10.4103/0972-5229.45076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Holanda MA, Reis RC, Winkeler GF, Fortaleza SC, Lima JW, Pereira ED. Influence of total face, facial and nasal masks on short-term adverse effects during noninvasive ventilation. J Bras Pneumol. 2009;35:164–73. doi: 10.1590/s1806-37132009000200010. [DOI] [PubMed] [Google Scholar]
- 48.Kwok H, McComack J, Cece R, Houtchens J, Hill NS. Controlled trial of oronasal versus nasal mask ventilation in the treatment of acute respiratory failure. Crit Care Med. 2003;31:468–73. doi: 10.1097/01.CCM.0000045563.64187.20. [DOI] [PubMed] [Google Scholar]
- 49.Hill NS, Brennen J, Garpestad E, Nava S. Non-invasive ventilation in acute respiratory failure. Crit Care Med. 2007;35:2402–7. doi: 10.1097/01.CCM.0000284587.36541.7F. [DOI] [PubMed] [Google Scholar]
- 50.British thoracic society standards of care committee: Noninvasive ventilation in acute respiratory failure. Thorax. 2002;57:192–211. doi: 10.1136/thorax.57.3.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Agarwal R, Handa A, Aggarwal AN, Gupta D, Behera D. Outcomes of noninvasive ventilation in acute hypoxemic respiratory failure in a respiratory intensive care unit in north India. Respir Care. 2009;54:1679–87. [PubMed] [Google Scholar]
- 52.Singh VK, Khanna P, Rao BK, Sharma SC, Gupta R. Outcome predictors for non-invasive positive pressure ventilation in acute respiratory failure. J Assoc Physicians India. 2006;54:361–5. [PubMed] [Google Scholar]
- 53.Wallet F, Schoeffler M, Reynaud M, Duperret S, Workineh S, Viale JP. Factors associated with noninvasive ventilation failure in postoperative acute respiratory insufficiency: An observational study. Eur J Anaesthesiol. 2010;27:270–4. doi: 10.1097/EJA.0b013e32832dbd49. [DOI] [PubMed] [Google Scholar]
- 54.Antonelli M, Conti G, Moro ML, Esquinas A, Gonzalez-Diaz G, Confalonieri M, et al. Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: A multi-center study. Intensive Care Med. 2001;27:1718–28. doi: 10.1007/s00134-001-1114-4. [DOI] [PubMed] [Google Scholar]
- 55.Keenan SP, Powers C, McCormack DG, Block G. Noninvasive positive-pressure ventilation for postextubation respiratory distress: A randomized control trial. JAMA. 2002;287:3238–44. doi: 10.1001/jama.287.24.3238. [DOI] [PubMed] [Google Scholar]
- 56.Esteban A, Frutos-Vivar F, Ferguson ND, Arabi Y, Apezteguía C, González M, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med. 2004;350:2452–60. doi: 10.1056/NEJMoa032736. [DOI] [PubMed] [Google Scholar]
- 57.Carlucci A, Delmastro M, Rubini F, Fracchia C, Nava S. Changes in the practice of non-invasive ventilation in treating COPD patients over 8 years. Intensive Care Med. 2003;29:419–25. doi: 10.1007/s00134-002-1574-1. [DOI] [PubMed] [Google Scholar]


