Abstract
We report a case of fibroid uterus with Wolff–Parkinson–White (WPW) syndrome in a 48-year-old female, posted for elective hysterectomy. Patient gave history of short recurrent episodes of palpitation and electrocardiograph confirmed the diagnosis of WPW syndrome. The anaesthetic management of these patients is challenging as they are known to develop life threatening tachyarrhythmia like paroxysmal supra-ventricular tachycardia (PSVT) and atrial fibrillation (AF). Epidural anaesthesia is preferred compared to general anaesthesia to avoid polypharmacy, noxious stimuli of laryngoscopy and intubation. To deal with perioperative complications like PSVT and AF, anti-arrhythmic drugs like adenosine, beta blockers and defibrillator should be kept ready. Perioperative monitoring is essential as patients can develop complications.
Keywords: Accessory pathway, adenosine, epidural anaesthesia, tachyarrhythmia, WPW syndrome
INTRODUCTION
Wolff–Parkinson–White (WPW) syndrome is caused by pre-excitation of ventricle due to an abnormal accessory pathway, bundle of Kent, between atria and ventricle bypassing atrio-ventricular node. The incidence is 0.9-3% of the general population.[1] Patients may present with symptoms ranging from mild chest discomfort, palpitation and hypotension to severe cardiopulmonary compromise in malignant variety of WPW syndrome. The diagnosis is done with history and electrocardiograph (ECG), which shows shortened PR interval, delta waves and widened QRS complex.[1,2] Anaesthetic management of such patient, if diagnosed preoperatively is not difficult, but sudden intraoperative appearance of short PR interval and delta wave can be troublesome as these patients are known to have life threatening tachyarrhythmias like paroxysmal supra-ventricular tachycardia (PSVT), atrial fibrillation (AF) etc.[3] Under anaesthesia, due to change in the physiology of conduction induced by anaesthetic drugs, complications may be precipitated, thus it is important to know about WPW syndrome and its management.[3,4] We are presenting this case of uterine fibroids with WPW syndrome, posted for elective abdominal hysterectomy.
CASE REPORT
A 48-year-old female patient presented with history of menorrhagia of 2-3 years duration to the gynaecological out-patient department. She also gave history of recurrent episodes of palpitations and uneasiness since the past twenty years. The palpitations lasted for 15-20 minutes and subsided on its own. She was not a known case of diabetes, hypertension or ischaemic heart disease. Her haemogram showed microcytic hypochromic anaemia with haemoglobin of 8.2 g%. Ultrasound sonography (USG) of the abdomen and pelvis revealed multiple uterine fibroids. ECG was suggestive of Type ‘A’ WPW syndrome with short PR interval, delta waves and widened QRS complex with right ventricular hypertrophy suggesting left posteroseptally positioned bundle of Kent [Figure 1]. Two-dimensional (2D) echocardiogram was normal. Pre-operatively anaemia was corrected with 2 units of blood transfusion with B positive compatible blood. Repeat Hb was 10.2 g%. Patient was posted for elective abdominal hysterectomy.
Figure 1.
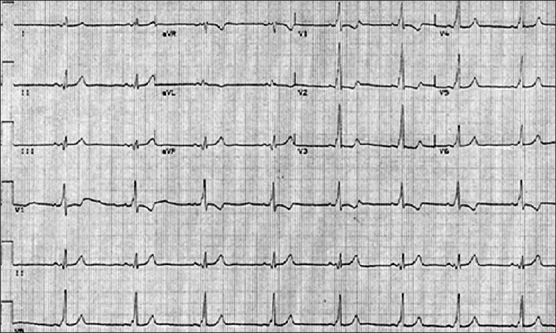
ECG depicting wide QRS complex due to “Delta waves” seen in Wolff–Parkinson–White syndrome
On pre-anaesthetic evaluation, patient was comfortable, pulse rate of 88/min, BP 110/80 mm of Hg, weight 52 kg and systemic examination was normal. Patient was accepted under ASA class 2. She was pre-medicated with oral Alprazolam 0.5 mg, Ondensetron 4 mg and Ranitidine 150 mg on previous night and early morning on the day of surgery.
Anaesthesia technique
The patient was counseled and consent obtained. Nil per oral was confirmed. The case was planned to be performed under graded epidural anaesthesia.
Eutectic mixture of local anaesthetic was applied, intravenous access secured with 18-G canula and preloading was done with Ringer lactate 500 ml at the rate of 8 ml/min. The anti-arrhythmic drugs like inj. Adenosine, inj. Esmolol, inj. Lignocaine 2% and defibrillator were kept ready. Perioperative monitoring included Pulse oximeter (SpO2), ECG (lead II) and noninvasive blood pressure (NIBP). ECG was showing short PR interval, delta wave and widened QRS complex with the heart rate of 100/min and BP of 110/80 mm of Hg. Epidural space was located in L3-L4 intervertebral space, by loss of resistance to air. An 18-G epidural catheter was passed and fixed at 8 cms mark. After negative aspiration for blood and cerebrospinal fluid (CSF), test dose of 3 cc of inj. Lignocaine, was given. Adrenaline was avoided with test dose as it may precipitate tachycardia. The graded epidural anaesthesia was given with 7 cc of inj. Lignocaine 2% and 7 cc of inj. Bupivacaine 0.5%, administered in divided doses, over a period of 20 minutes, to achieve sensory blockade up to T6. Oxygen supplemented through Hudson's mask at 3 L/min and sedation given with intravenous Midazolam 2 mg. Intraoperatively, all vitals were maintained, and top up dose of inj. Bupivacaine 0.5% 5 cc was administered, as surgery lasted for two and a half hours. Postoperatively, patient was monitored for 24 hrs in cardiac care unit. Postoperative analgesia was achieved with epidural inj. Fentanyl 50 microgram 6 hourly, for next 48 hours and inj. Tramadol 100 mg IV s.o.s. (given twice in 48 hrs). Post-operative period remained uneventful.
DISCUSSION
Individuals with WPW syndrome have an accessory pathway, which allows electrical conduction between atria and ventricle, at site other than AV node that does not share the rate slowing property of AV node. This may lead to reentrant tachyarrhythmia and sudden cardiac arrest.[2]
The goal during perioperative management of anaesthesia is to avoid any factor that increases sympathetic activity such as pain, anxiety, stress response of intubation, lighter plane of anaesthesia and hypovolemia.[4,5] The anti-arrhythmic drugs like Digoxin and Verapamil that could enhance anterograde conductions of cardiac impulses through an accessory pathway should be avoided.[4,5]
Regional anaesthesia is preferred technique over general anaesthesia to avoid polypharmacy, noxious stimuli of laryngoscopy and intubation.[4,5,6] Sympathetic blockade in spinal anaesthesia can lead to sudden hypotension and bradycardia. The vasopressors used for treating these complications could be initiators of tachycardia and arrhythmias.[7] The reduced atrial filling after spinal anaesthesia has also been implicated in increasing arrhythmogenecity of the heart. Therefore, preloading not only helps to prevent decreased atrial filling, but also reduces sympathomimetic requirement, which may trigger PSVT.[8] Graded epidural anaesthesia with segmental blockade provides added advantage of haemodynamic stability and post-operative analgesia.[7] As our patient was symptomatic with history of palpitation, we preferred graded epidural anaesthesia. For post-operative analgesia, epidural analgesics are preferred over IV non steroidal anti-inflammatory analgesics. We gave inj. Fentanyl 50 microgram epidurally, as it provides adequate haemodynamic stability. However, low concentrations of Bupivacaine epidural infusion can also be used.
For general anaesthesia, Thiopentone is safe but Propofol is preferred, as it has no effect on the refractory period of accessory pathway. Atropine, Glycopyrrolate and Ketamine precipitate tachycardia, therefore should be avoided. Isoflurane and Sevoflurane have no effect on AV node conduction and provide the optimal haemodynamic status. Fentanyl provides adequate haemodynamic stability. Vecuronium and Rocuronium are cardio stable muscle relaxants preferred over Pancuronium and Atracurium.[4–6] Neostigmine slows AV conduction, may facilitate transmission via the accessory pathway and may cause AF with rapid ventricular rate. Newer relaxants like Cis-atracurium, Mivacurium can be safe as reversal with Neostigmine and Glycopyrrolate not required.[6]
PSVT, a common complication, can be treated with vagal maneuvers or adenosine 6-12mg IV or beta blockers (Esmolol 50-300 μg/kg/min IV). Patients developing AF with haemodynamic stability should be treated pharmacologically, whereas haemodynamically unstable patients should be treated by cardio version with 150-200 Joules. (Biphasic defibrillator). Digitalis and verapamil are contraindicated.[5–7,9]
To summarize, patient with WPW syndrome may develop perioperative tachyarrhythmias and hypotension leading to cardiac arrest. Epidural anaesthesia is preferred because of haemodynamic stability and provides post-operative analgesia. Anti-arrhythmic drugs and defibrillator must be kept ready. Perioperatively, even asymptomatic patient can develop arrhythmias, therefore meticulous monitoring is essential.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Rosner MH, Brady WJ, Jr, Kefer MP, Martin ML. Electrocardiography in patient with the WPW syndrome: Diagnostic and initial therapeutic issues. Am J Emerg Med. 1999;17:705–14. doi: 10.1016/s0735-6757(99)90167-5. [DOI] [PubMed] [Google Scholar]
- 2.Mark DG, Brady WJ, Pines JM. Pre-excitation syndrome, diagnostic consideration in the ED. Am J Emerg Med. 2009;27:878–88. doi: 10.1016/j.ajem.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 3.Kadoya T, Seto A, Aoyama K, Takenaka I. Development of rapid atrial fibrillation with wide QRS complex after neostigmine in patients with intermittent WPW syndrome. Br J Anaesth. 1999;85:815–8. doi: 10.1093/bja/83.5.815. [DOI] [PubMed] [Google Scholar]
- 4.Rahul S, Patel RD, Dewoolka Anesthetic management of WPW syndrome: TM. [Last cited on 2011 Jan 3]. available from: http://www.ispub.com/journal/the_internet_journal_of_anesthesiology/archive/volume_11_number_2_1.html. ISSN: 1092-406X, 2007 .
- 5.Hines RL, Marschall KE. Abnormalities of Cardiac Conduction and Cardiac Rhythm. In: Stoelting RK, Dierdorf SF, editors. Anesthesia and co-existing disease. 5th ed. Philadelphia: Churchill-Livingstone; 2008. pp. 72–3. [Google Scholar]
- 6.Chhabra A, Trikha A, Sharma N. Unmasking of benign Wolff -Parkinson-White pattern under general anesthesia. Indian J Anesth. 2003;47:208–11. [Google Scholar]
- 7.Nazir SA, Shoukat AG, Ayaz KF, Qazi MS, Nissa WUI. Anesthetic management of Wolff–Parkinsons–White syndrome for caesarean section:TM. [Last cited on 2011 Jan 3]. available from http://www.ispub.com/journal/the_internet_journal_of_anesthesiology/archive/volume_16_number_2_1.html. ISSN: 1092-406X, 2008 .
- 8.Nakaigawa Y, Akazawa S, Shimizu R, Ishii R, Yamato R. Comparison of the effects of halothane, isoflurane and sevoflurane on atrioventricular conduction times in pentobarbital anesthetized dogs. Anesth Analg. 1995;81:249–53. doi: 10.1097/00000539-199508000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Khatib SK, Tadwalkar GV. WPW syndrome: A challenge for anaesthetist. J Anaesth Clin Pharmacol. 2010;26:417–8. [Google Scholar]


