Abstract
Study Objectives:
To evaluate the effects of pediatric epilepsy on sleep in parents of epileptic children.
Methods:
Cohort design in which the sleep quality of parents of epileptic children (POEC) and parents of nonepileptic children (PONEC) in the month preceding recruitment were compared using the self-administered Pittsburgh Sleep Quality Index (PSQI).
Results:
Mothers of epileptic children had a 7-fold occurrence of sleep disturbances when compared to mothers of non-epileptic children (OR = 6.66 CI 95% 1.10-70.08). The sleep characteristics that showed statistically significant differences were: sleep duration, sleep continuity, and self-evaluation of sleep quality (p < 0.05 for all parameters). No significant difference in sleep quality was found between fathers of epileptic children and fathers of nonepileptic children.
Conclusions:
Sleep disturbances are more common in mothers of epileptic children. The sleep quality of mothers to epileptic children should be considered in their comprehensive management, and if necessary, the sleep disturbance should be addressed.
Citation:
Shaki D; Goldbart A; Daniel S; Fraser D; Shorer Z. Pediatric epilepsy and parental sleep quality. J Clin Sleep Med 2011;7(5):502-506.
Keywords: Pediatric epilepsy, sleep disturbance, PSQI, insomnia
Epilepsy is one of the most common chronic clinical problems in the pediatric population, and appears in approximately 0.5% children. As in other chronic pediatric diseases, epilepsy has an appreciable negative impact on the quality of life in the family in general, and the parents in particular.1,2 Furthermore, epilepsy has unique characteristics that contribute to a prolonged adaptive difficulty of the parent. This includes unpredictable stressful events, social stigma of the child and family, extended treatment regimen subject to frequent changes, and cognitive disturbances accompanying the disease and treatment. Previous research has shown that even in comparison with other chronic pediatric diseases, parents of children with epilepsy suffer from higher rates of stress, anxiety, and depression, which manifest in significant impairment in social, familial, and personal parental functioning.3,4
BRIEF SUMMARY
Current Knowledge/Study Rationale: Pediatric epilepsy leads to prolonged adaptive parental difficulties which in turn affect the quality of life in the child, eventually leading to a vicious cycle. Little data is available regarding the impact of pediatric epilepsy on parental sleep quality.
Study Impact: The study provides new data on the nature of sleep disturbances in parents of epileptic children. There is a need to consider the involvement of a sleep specialist in order to address a suspected sleep disturbance.
Despite the fact that there has been research investigating the effects on the lives of the parents in chronic pediatric disease in general and pediatric epilepsy in particular, there is insufficient data on the effects on the sleep quality of the parents, even though this impairment is liable to be accompanied by negative repercussions.
Insomnia, which may be a symptom, a sign, or a primary disturbance, is currently defined only as a symptom, in the presence of ≥ 1 of 4 characteristics: difficulty in falling asleep, involuntary early awakening, difficulty in remaining continually asleep, and unrefreshing sleep. As a syndrome, sleep difficulties must occur in association with a complaint of impaired daytime functioning (e.g., diminished vocational functioning) and in the presence of adequate opportunity to sleep.
For the purpose of this project we decided to use the ICSD-2 general criteria for insomnia that do not specify a frequency and duration for the insomnia symptoms.5 Studies of the pathophysiology of this disturbance have described physiological as well as psychological effects.6
Disturbances of sleep duration and associated daytime drowsiness have numerous clinical ramifications. Most commonly studied is the negative effect on essential cognitive functions, both lower and higher, such as attention, concentration, alertness, reaction time, risk taking, short-term memory, decision making, and judgment.7 The significance of these findings is in their impact on the quality of life of the individual, and in their heavy toll on society, expressed in economic standing from decreased productivity of those suffering from sleep disturbances, but mainly due to the increase in errors and accidents, including many fatal ones.8 In addition, sleep disturbances have direct strong negative effects on morbidity and mortality.9,10
Qualitative studies that show distinctive sleep patterns in families of pediatric epilepsy patients suggest increased occurrence of this impairment. These studies show that the appearance of a seizure, even febrile seizure, disrupts the family routine, expressing itself in the fact that in many families, parents begin to sleep in the child's room and/or check his/her condition numerous times during the night.11
Moreover, sleep of epileptic children is frequently disturbed, which may contribute to parental sleeping problems. Epileptic children often experience sleep fragmentation and excessive daytime sleepiness as a result of seizures, comorbid sleep disorders (sleep disordered breathing, obstructive sleep apnea, upper airway resistance syndrome, periodic leg movement of sleep), and antiepileptic drugs.12 As a result, the caregivers of these children are likely to experience concomitant sleep problems when trying to answer their children's needs during the night.
Beyond the repercussions of sleep disturbances of the parents of pediatric epilepsy patients on the parent himself, one must account for the implications for the child. It has been shown that treatment of chronic pediatric disease that included dealing with its repercussions on the rest of the family is highly correlated with best treatment results.13 Familial factors have been found to play an important role in the development and severity of psychopathology of the pediatric epilepsy patient.14 Since normal sleep serves as a sort of buffer, neutralizing daily stresses, and as pediatric epilepsy is connected with high parental stress, sleep disturbances are liable to cause uncontrollable stress and lowered accommodation abilities, possibly leading to lowered adaptation abilities of the child and failed treatment of the disease.
A previous uncontrolled study based on a group of 50 mothers of pediatric epilepsy patients without a comparison group, showed a negative effect on duration and continuity of sleep.15 The goal of our study was to test the effects of pediatric epilepsy on the quality of sleep of both mothers and fathers by controlling for potential confounders such as number of children and comparison to parents of nonepileptic children. Further goals of the study were to compare the effect of the exposure of the fathers with that of the mothers, and to identify which of the characteristics of sleep were most affected in order to achieve optimal coping methods.
METHODS
Participants
Parents of epileptic and nonepileptic children ≤ 18 years were enrolled in this study. Parents were excluded if they did not speak Hebrew or were unable to fill out the questionnaire in Hebrew. Epilepsy was defined according to currently accepted diagnostic criteria: ≥ 2 unprovoked seizures. A list of children who had been hospitalized in one of the Pediatric Departments of Soroka University Medical Center between June 1, 2009, and January 1, 2010, was obtained. Hebrew-speaking parents from a list of those 37 families with a child with documented diagnosis of epilepsy were approached by telephone. Two families could not be contacted and 4 refused to participate. In 8 families, both the fathers and the mothers were interested in participating in the study, while in the remaining 23 families, only one parent participated, giving a total of 39 enrolled parents in the investigation group (POEC).
The comparison group (PONEC) was sampled from the parents waiting in the pediatric emergency room of Soroka University Medical Center. The research team went to the waiting room twice a week for 8 weeks and distributed questionnaires to all Hebrew-speaking parents present at that time. None of the parents enrolled reported having an epileptic child. In 5 families, the parents refused to participate, while in 7 families, both the fathers and mothers were interested in participating in the study. In 28 cases, only one parent participated; thus a total of 42 parents were enrolled in the comparison group.
All parents were asked to fill out a demographic questionnaire, a medical history questionnaire, and the PSQI Sleep Quality Questionnaire, which tested the quality of sleep in the month preceding the completion of the questionnaire.
PSQI Questionnaire
The PSQI is a self-administered questionnaire commonly used in clinical research sleep studies. Using a cutoff value of 5, the questionnaire is validated to define subjective insomnia.16 The PSQI Questionnaire is more highly associated with psychological symptom ratings and sleep diary measures then the Epworth Sleepiness Scale (ESS), and has been shown to have a sensitivity of 89.6% and a specificity of 86.5%.17 The PSQI Questionnaire has 19 sections that subjectively evaluate the subject's sleep quality over the past month. The 19 sections contain 7 indices of clinical aspects of sleep quality: sleep disturbances—awakenings during sleep, involuntary earlier awakening, coughing, feelings of coldness or warmth, nightmares, and pain; sleep latency—amount of time between lying down in bed and falling asleep; sleep effectiveness—net sleep time between lying down in bed and awakening; sleep length—net sleep time; daily functioning—difficulty maintaining wakefulness and enthusiasm during the day; medications—use of medications to improve sleep quality; general evaluation—general self-evaluation of sleep quality. Each index can be evaluated on a scale of 0-3. The 7 indices were combined to achieve a total value ranging from 0 to 21. The questionnaire has been translated into 48 languages, including Hebrew. The Hebrew translation of the questionnaire has been validated.16
Demographic and Medical History Questionnaire
Demographic information was obtained from the study participants (sex, age, number and ages of children, years of schooling, number of daily work hours). The following 4 questions were directed only to POEC and were about the epileptic history (date of first and last seizure, total number of seizures, and number of seizures in the previous month).
The study was approved by the Institutional Review Board of the Soroka University Medical Center and Ben-Gurion University of the Negev. All the parents signed the informed consent.
Statistical Analyses
We assessed the association between parenting an epileptic child to background variables using χ2 test for nominal variables and t-test for quantities variables.
The association between study group and sleep disturbance of the parents, adjusting for suspected confounders, was examined using a multivariate logistic regression. Clinically significant variables as well as variables with borderline statistical significance were available for this analysis.
The difference in various indices evaluating sleep quality between the 2 study groups was tested using the Mann-Whitney test; the correlation between the severity of the child's epilepsy and the severity of sleep disturbance of the parent was assessed using a Spearman correlation test.
We used the PSQI Hebrew validation data, which showed a mean of 3.54 units (SD 2.16) for the PSQI to compute the required sample size using the PS—Power and Sample Size Program. Assuming equal sizes of study groups, in order to identify an average difference of 1.5 units in the PSQI questionnaire, 34 subjects were required in each group in order to prove a significant difference with α = 0.05 and power = 0.8.
RESULTS
We initially compared the 2 groups by sex, age, number of children living at home, years of education, and number of hours of daily work. The number of educational years was considered an index of socioeconomic status.17 There were no statistically significant differences in background variables between the participants in the 2 groups (Table 1).
Table 1.
Comparison of background variables between POEC and PONEC
| Variable | POEC N = 39 | PONEC N = 42 | p value |
|---|---|---|---|
| Sex N men | 13 | 18 | 0.378 |
| N women | 26 | 24 | |
| Age (years) | 39.92 (± 7.29) | 36.43 (± 8.68) | 0.054 |
| Years of education | 13.92 (± 3.84) | 14.24 (± 2.75) | 0.671 |
| Daily working hours | 6.69 (± 4.56) | 7.23 (± 3.83) | 0.569 |
| Number of children living at home | 3.03 (± 2.15) | 2.69 (± 1.94) | 0.463 |
Means (SD) are presented unless otherwise specified.
Average sleep duration was 5.26 (± 1.55) h in parents of epileptic children and 6.04 (± 1.27) h in the comparison group.
We examined on POEC group the possible association between the severity of the epilepsy and severity of sleep disturbance using Spearman correlations, but no correlation was found between sleep disturbance in the parents with any of the characteristics of severity of epilepsy in the child as follows: number of seizures in the previous month (r = −0.058, p = 0.72), average number of epileptic seizures per month (r = −0.028, p = 0.865), duration of latency period since last seizure (r = −0.048, p = 0.771), current age of epileptic child (r = −0.042, p = 0.801), and duration of epilepsy since the first epileptic seizure (r = 0.036, p = 0.827).
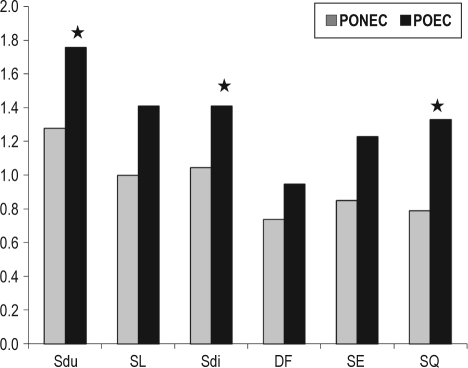
We tested the difference in various indices in the PSQI questionnaire between POEC and PONEC. Three indices were found to be significantly different between the 2 groups: sleep duration (p = 0.037), sleep disturbances (p = 0.01), and overall subjective feeling of sleep quality (p = 0.005; Figure 1).
Figure 1.
Mean score of PSQI indices by POEC and PONEC
Significant differences are noted with a star symbol. SDi, sleep disturbance; SL, sleep latency; SE, sleep efficiency; SDu, sleep duration; SQ, sleep quality; DF, daily functioning.
In order to examine the association between parental sleep disturbance and pediatric epilepsy adjusting for suspected confounders, we performed multivariable logistic regression analysis, presented in Table 2.
Table 2.
Results of multiple logistic regression examining the association between parental sleep disturbance and pediatric epilepsy adjusting for suspected risk factors or confounders
| Variable | OR | p value | 95% CI |
|---|---|---|---|
| Pediatric epilepsy | 4.06 | 0.01 | 1.49 – 11.07 |
| Fathers = 0 | 1.50 | 0.5 | 0.47 – 4.79 |
| Mothers = 1 | |||
| Number of children | 1.11 | 0.46 | 0.84 – 1.47 |
| Age of youngest child at home (years) | 0.94 | 0.25 | 0.84 – 1.05 |
| Parental years of education | 0.88 | 0.12 | 0.76 – 1.03 |
| Daily work hours | 0.95 | 0.51 | 0.82 – 1.10 |
Significant differences are noted with a star symbol. SDi, sleep disturbance; SL, sleep latency; SE, sleep efficiency; SDu, sleep duration; SQ, sleep quality; DF, daily functioning.
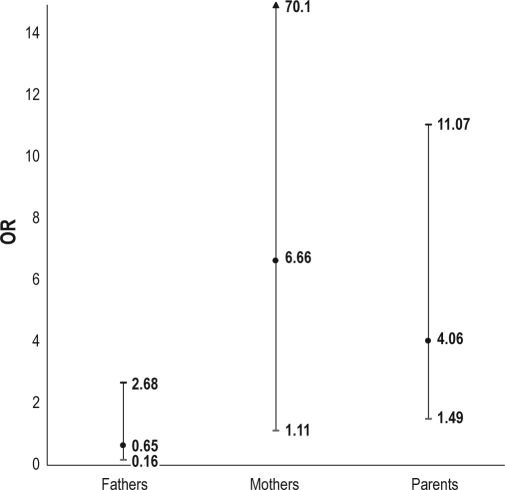
After controlling for background variables we found that the risk for sleep disturbance is raised 4-fold in the presence of pediatric epilepsy (OR = 4.05 CI 95% 1.48-11.06). We did not find any excess risk for sleep disturbance in mothers compared to fathers (OR = 1.50 CI 95% 0.46-4.79).
When testing the model including an interaction variable between sex of the parent and pediatric epilepsy (data not presented), the risk of mothers to epileptic children for sleep disturbance comparing to mothers of nonepileptic children was 7-fold (OR = 6.66, CI 95% 1.108-70.088) higher. However, the risk of fathers to epileptic children was not significantly different from that of fathers of nonepileptic children (OR = 0.65, CI 95% 0.16-2.68; Figure 2).
Figure 2.
Significant difference in odds ratio for self-reported sleep disturbance between POEC and PONEC using logistic regression
DISCUSSION
Our study demonstrated a strong association between sleep disturbance of sleep quality in mothers of children with epilepsy, regardless of the severity of the epilepsy and time since last episode. This study also demonstrated severe sleep disturbances, including short sleep duration and poor sleep quality in mothers of children with epilepsy, regardless of the severity of epilepsy and time since last episode.
The present findings are in line with similar studies showing associations between other pediatric diseases, such as asthma and cystic fibrosis, with parental sleep disturbance.18,19 It is reasonable to assume that the pathogenesis of the disturbance is similar to that of other chronic pediatric diseases.
It should be noted that the two sleep characteristics, sleep duration and continuity, which we found to be correlated with exposure are the two chief characteristics associated with severe clinical consequences. Thus, their identification is likely to contribute to the diagnostic and treatment efforts regarding parental well-being and functioning.
Contrary to current perception, we did not find correlations between the various indices of severity of epilepsy and the presence of sleep disturbance in the parents. These findings strengthen the understanding that pediatric epilepsy has an intractable and sustained influence on the parent, which should be expressed in suitable arrangement for prevention or treatment of parental sleep disturbance.
We show that the influence of the child's epilepsy on the sleep of mothers is much stronger than that on the sleep of fathers. Studies have shown that the mother bears the chief burden in the area of health in general, and in the care of the chronically ill child in particular.20 Therefore, impingement on the sleep quality of the mother has severe implications, especially on the effectiveness of care for the epileptic pediatric patient.
While our study does not prove causality (which would require different methodology), its findings can not be ignored. This is because even known risk factors, such as depression, general anxiety disorders, back and joint pain, and diabetes (which were once considered causal factors for insomnia, and in their presence the latter was classified as secondary), are no longer considered as such, and insomnia in their presence is now considered a comorbid condition.6 This is because there is a theoretical and clinical difficulty in determining causality between insomnia and various background conditions. It is important to note that it has also been proposed that insomnia can be a predictor of depression.21
PONEC group was sampled in a situation which makes our findings even stronger, as we did not sample parents of healthy children but recruited parents from the pediatric emergency room. Sitting up with a sick child after numerous hours to days of an acute disease is liable to temporarily impinge on the sleep quality of the parent, and, as a result, influence the self-evaluation of sleep quality in the previous month. Therefore, the findings in this study which were obtained under these conditions support the conclusion that the relative risk of developing sleep disturbance in parents of epileptic children as compared to healthy children is even greater than that detected.
One of the limitations of the present study is that measures of children sleeping problems or parents depression/anxiety were not performed. Although, it can be assumed that the child's sleep quality might be afflicted by disease severity, we could not find any differences between parents to children with several severity indicators, such as the number of epileptic attacks or the longevity of the condition. We decided not to conduct an objective psychiatric evaluation of the parents. We felt that such an evaluation would decrease the response rate. We believe that this type of evaluation may be appropriate in future studies. There is a potential selection bias in parents who chose to report. Indeed, in only a small minority both parents agreed to participate. It is therefore possible that parents with more sleep disturbances tended to agree.
A topic that arose during the study and which is worthy of research is the degree of underdiagnosis of generalized anxiety disorder among parents, especially mothers of pediatric epilepsy patients. Generalized anxiety disorder is a disorder whose basis is uncontrollable worry expressed in a number of symptoms, among them insomnia. Interviews with the parents left an impression of severe uncontrollable worry, particularly regarding nighttime.
Numerous studies showing the efficacy of continuous positive air pressure for obstructive sleep apnea patients served for some sleep and sleep disturbance researchers as a model that demonstrates the reversal of impingement of health and quality of life through appropriate treatment for sleep disturbance. Despite the fact that this understanding has been at the heart of a disagreement among sleep specialists in recent years, the generally accepted opinion among researchers is that appropriate treatment for sleep disturbance resulting in improved sleep quality can serve as a means of improving general health and quality of life and decreasing morbidity and mortality.22 This popular view stands as the basis for our recommendations.
For a number of years it has been recommended that family physicians routinely ask all patients about their sleep quality as part of their periodic general health check-up, a recommendation that is self-evident in light of the importance of the subject. At any rate, when speaking of risk groups such as mothers of pediatric epileptic patients, it should be, in our opinion, mandatory to address the question of sleep quality seriously and often.
Raising awareness of and detailed instruction in proper sleep hygiene is an important first step in addressing parental sleep disturbance. This instruction should be given, in our opinion, immediately after the diagnosis of pediatric epilepsy. Improper sleep hygiene is considered a common and reversible cause of insomnia. Neutralization of habits contributing to development and exacerbation of sleep disturbances, at the mere expense of instruction, seems a self-evident step when considering a risk group for sleep disturbance. In cases where the attending physician is not experienced in this type of instruction, a specialist should be consulted.
A number of studies have shown the efficacy of various informational programs aimed at families of epilepsy patients such as SEE (the Seizures and Epilepsy Education Program) and CEP (Children's Epilepsy Program) in upgrading knowledge and understanding regarding epilepsy, reducing anxiety, and improving quality of life. These studies did not examine the effect on sleep quality. It is likely that, in light of the clinical impression that anxiety has a central role in parental sleep disturbance, these programs would have a positive effect on sleep quality; it would be suitable for future studies of the efficacy of these programs to consider their effect on sleep quality.
Our study shows that of all participants, only one in each group used sleep medication. In other words, despite the fact that the POEC group had a much higher rate of sleep disturbance than the PONEC group, the use of medications in the two groups was equal, and in both was minimal.
In conclusion, we demonstrated an association between pediatric epilepsy and maternal insomnia. We recommend that pediatricians routinely question mothers of pediatric epilepsy patients regarding their quality of sleep, and if there is any suspicion of the existence of sleep disturbance, to consider referral to a sleep specialist for the clarification of diagnosis and possible necessary treatment.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Dr. Goldbart is supported by the Israel Science Foundation legacy program grant 1817/07.
REFERENCES
- 1.Lawoko S, Soares JJF. Quality of life among parents of children with congenital heart disease, parents of children with other disease and parents of healthy children. Qual Life Res. 2003;12:655–66. doi: 10.1023/a:1025114331419. [DOI] [PubMed] [Google Scholar]
- 2.Ellis N, Upton D, Thompson P. Epilepsy and the family: a review of current literature. Seizure. 2000;9:22–30. doi: 10.1053/seiz.1999.0353. [DOI] [PubMed] [Google Scholar]
- 3.Chiou HH, Hsieh LP. Parenting stress in parents of children with epilepsy and asthma. J Child Neurol. 2008;23:301–6. doi: 10.1177/0883073807308712. [DOI] [PubMed] [Google Scholar]
- 4.Thomas SV, Bindu VB. Psychosocial and economic problems of parents of children with epilepsy. Seizure. 1999;8:66–9. doi: 10.1053/seiz.1998.0241. [DOI] [PubMed] [Google Scholar]
- 5.American Academy of Sleep Medicine. International classification of sleep disorders: diagnostic and coding manual. 2nd edition. Westchester, Il: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 6.National Institutes of Health. State of the science conference statement on manifestations and management of chronic insomnia in adults. Sleep. 2005;28:1049–57. doi: 10.1093/sleep/28.9.1049. [DOI] [PubMed] [Google Scholar]
- 7.Balkinv TJ, Rupp T, Picchioni D, Wesenten NJ. Sleep loss and sleepiness, current issues. Chest. 2008;134:653–60. doi: 10.1378/chest.08-1064. [DOI] [PubMed] [Google Scholar]
- 8.Lockley SW, Cronin JW, Evans EE, Cade BE, Lee CJ, Landrigan CP. Effect of reducing interns' weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351:1829–37. doi: 10.1056/NEJMoa041404. [DOI] [PubMed] [Google Scholar]
- 9.Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S. Meta- analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea - hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365:1046–53. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 11.Wirrel E, Turner T. Parental anxiety and family disruption following first febrile seizure in childhood. Paediatr Child Health. 2001;6:139–43. doi: 10.1093/pch/6.3.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kothare SV, Kaleyias J. Sleep and epilepsy in children and adolescents. Sleep Med. 2010;11:674–85. doi: 10.1016/j.sleep.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 13.Cohen MS. Families coping with childhood chronic illness: a research review. Fam Syst Health. 1999;17:149–64. [Google Scholar]
- 14.Rodenburg HR, Stams GJJM, Meijer AM, Aldenkamp AP, Deković M. Psychopathology in children with epilepsy: a meta-analysis. Pediatr Psychol. 2005;30:453–68. doi: 10.1093/jpepsy/jsi071. [DOI] [PubMed] [Google Scholar]
- 15.Cottrell L, Khan A. Impact of childhood epilepsy on maternal sleep and socioemotional functioning. Clin Pediatr. 2005;44:613–6. doi: 10.1177/000992280504400709. [DOI] [PubMed] [Google Scholar]
- 16.Shochat T, Tzischinsky O, Oksenberg A, Peled R. Validation of the Pittsburgh Sleep Quality Index Hebrew Translation (PSQI-H) in a sleep clinic sample. IMAJ. 2007;9:853–6. [PubMed] [Google Scholar]
- 17.Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719–29. doi: 10.1056/NEJMoa1010679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yilmaz O, Sogust A, Gulle S, Can D, Ertan P, Yuksel H. Sleep quality and depression-anxiety in mothers of children with two chronic respiratory disease: asthma and cystic fibrosis. J Cyst Fibros. 2008;7:495–500. doi: 10.1016/j.jcf.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 19.Yuksel H, Sogut A, Yilmaz O, Demet M, Ergin D, Kirmaz C. Evaluation of sleep quality and anxiety-depression parameters asthmatic children and their mothers. Respir Med. 2007;101:2550–4. doi: 10.1016/j.rmed.2007.07.025. [DOI] [PubMed] [Google Scholar]
- 20.Knafl K, Zoeller L. Childhood chronic illness: a comparison of mothers' and fathers' experiences. Fam Nurs. 2000;6:287–302. [Google Scholar]
- 21.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011 Feb 5; doi: 10.1016/j.jad.2011.01.011. DOI: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Buysse DJ, Grunstein R, Horne J, Lavie P. Can an improvement in sleep positively impact on health? Sleep Med Rev. 2010;14:405–10. doi: 10.1016/j.smrv.2010.02.001. [DOI] [PubMed] [Google Scholar]