Abstract
Background
Asthma is a highly-prevalent chronic disease. Prevalence and mortality are particularly high in Puerto Ricans living in the US as compared with other populations.
Objective
To determine asthma mortality rates in Puerto Rico (1980 to 2007) and to assess the socio-demographic variables that may be associated with these rates.
Methods
Data was obtained from the Vital Statistics Office at the Puerto Rico Department of Health. Crude mortality rates and their 95% confidence intervals were used to evaluate differences between age groups and across years. Mortality risk ratios by socio-demographic variables were estimated using generalized lineal models with a Poisson link function to identify at-risk groups.
Results
. During the study period, there were 4,232 deaths recorded with asthma as the cause of death. From 1980 to 1998 annual asthma mortality rates fluctuated between 3.32 and 6.56 deaths per 100,000 (Mean 4.77), followed by a decline after implementation of the ICD-10 for reporting cause of death in 1999. Between 1999 and 2007 the mean asthma death rate declined to 3.01 (4.89 in 1999 to 2.02 in 2007). Overall, asthma mortality rates were between 1.77 and 4.0 times higher in Puerto Rico than in the US. Throughout the whole study period, mortality rates were higher in older age groups. In addition, the adjusted regression model for asthma deaths showed that persons divorced or widowed, and persons with only elementary education had significantly higher risk of asthma mortality than their counterparts.
Conclusion
. Asthma death rates were higher in Puerto Rico than in the US general population. Although asthma mortality in Puerto Rico declined, rates continued to be significantly higher than those recorded in the US. There was a progressive decline in asthma mortality rates after 1999 that may be explained by changes in reporting classification, increased use of corticosteroids, and improved asthma awareness. After controlling for possible confounding variables, age and elementary education were found to increase the risk of mortality due to asthma among Puerto Ricans.
Keywords: asthma, cause of death, epidemiology, mortality rate, vital statistics
Background
The analysis and dissemination of mortality data provide information about the risks of death in a population with a specific health condition (1). Asthma has been recognized as an important global health issue (2) and has become the most common chronic condition in many countries (3). During the 1970s and 1980s, increasing asthma death rates were reported in New Zealand, England and Wales, United States (US), and Russia (4–8). Although regional variability exists when describing mortality rates across countries efforts by health authorities to study asthma mortality data and dissemination of findings contributed to raising awareness internationally (9, 10). More recently, the use of inhaled corticosteroids (11), and the development of treatment guidelines such as the Global Initiative for Asthma guidelines in 1989, and the National Asthma Education and Prevention Program in 1991 aided physicians and public health practitioners to decrease and stabilize mortality rates in some regions (10, 12). Today, mortality due to asthma is less frequent (13) but deaths continue to be recorded.
Puerto Rico, an archipelago with about 4,004,000 inhabitants (14), has the highest lifetime asthma prevalence when compared to all US states and territories (15). Puerto Ricans living in the US have the highest mortality and morbidity rates when compared to Caucasians, African Americans, and other Hispanic groups such as Mexicans and Cubans (7, 16–19). Nevertheless, there are no published articles to evaluate the patterns of asthma mortality of the population living in Puerto Rico.
The objectives of this study were to examine the trends in mortality rates due to asthma from 1980 to 2007 in Puerto Rico and describe asthma deaths based on socio-demographic variables.
Methods
The asthma mortality data for Puerto Rico was obtained from the Vital Statistics Office at the Puerto Rico Department of Health (PRDOH). The data included information from the year 1980 to the year 2007. The Vital Statistics Office obtains mortality data from the Puerto Rico Demographic Registry, which collects information from death certificates on an ongoing basis.
The case definition (asthma death) for this study was all deaths in Puerto Rico listing asthma as the underlying cause. The death classification was conducted by means of the International Code of Diseases (ICD). Two different ICD’s were used within the study period: the 493.0–493.9 classifications for the ICD-9th revision from 1980 to 1998 and the J45-J46 classifications for the ICD-10th revision from 1999 to 2007. Demographic information includes the deceased gender, age, educational level, and marital status. The Census-PR Office provided general population estimates for Puerto Rico.
The Crude Mortality Rate (CMR) was calculated to obtain the estimated risk of death due to asthma in the general population. The CMR and its 95% Confidence Intervals (95% CI) were used to evaluate differences between age groups and across years. Age was aggregated in six groups 0–4, 5–14, 15–34, 35–64, 65 or older, according to those used by the CDC (20) and Homa (17). In addition, the 5–34 age group was analyzed for its importance in asthma-related epidemiological studies. In standard practice, asthma mortality rates have been confined to the 5 to 34 years of age because the correct assignment of asthma is firmly established in this group (11). The 95% CIs were calculated using the Poisson probability theory (21) for rare events, which usually follows a Poisson distribution (22).
Mortality risk ratios (RR) by socio-demographic variables (age, gender, education and civil status) were estimated using generalized linear models with a log-link function to identify at-risk groups (23, 24). Covariates were included in the models to calculate adjusted RRs useful to evaluate for the possibility of confounding. Results were included in a table containing population information, estimated risks, and measures of association. The Delta column represents the percent change between crude and adjusted RRs. A change of 10% was selected as cutoff point to indicate that, at least, one of the control variables produced a change in the magnitude of the association, a confounding effect. The model was performed with population estimates stratified by covariates obtained from the Census Public Use Microdata Sample (PUMS). PUMS data was restricted to year 2000 and obtained in a specific tabulated format. Asthma deaths were combined from 1999 to 2007 considering Census data availability, possible effects of changes in the ICD and changes in population age distribution. Moreover, Education and civil status were aggregated to match the Census data format.
Puerto Rico’s age-adjusted asthma deaths rates were calculated to compare them to US rates using the US 2000 standard population. Asthma mortality adjusted rates for the US were obtained through the Center for Disease Control and Prevention (CDC), which collects data from the National Vital Statistics System and from the US Census Bureau (26, 27). The comparison of asthma mortality rates between Puerto Rico and the US was conducted because Puerto Rico is a US territory, and most of the guidelines to treat asthma used in the US are also applied in Puerto Rico.
The mortality data was managed with Microsoft Excel 2003 (28), and analyzed with the EpiTools (29) and MASS (30) libraries for the R statistical package Version 2.9.0 (31).
Results
During the time frame from 1980 through 2007, there were a total of 4,232 deaths recorded in the Vital Statistics data with asthma as the underlying cause of death in Puerto Rico. As shown in Table 1, the asthma CMR for the overall population during the ICD-9 implementation presents a fluctuating pattern. A decrease was observed from 1980 (4.35 deaths per 100,000 inhabitants) to 1988 (3.84 deaths per 100,000 inhabitants). Afterward, an increasing trend was observed in the asthma death rates ranging from 4.81 deaths per 100,000 inhabitants in 1989 to 6.56 deaths per 100,000 inhabitants in 1998. After ICD-10 implementation, the mortality rates show a decreasing trend from 4.89 deaths per 100,000 inhabitants in 1999 to 2.02 deaths per 100,000 inhabitants in 2007.
Table 1.
Asthma crude mortality rates (per 100,000 inhabitants) 95% C.I. by age in Puerto Rico from 1980 to 2007
| Years | 0–4† | 5–14† | 15–34 | 35–64 | 65 or more | 5–34 | Total | Total deaths |
|---|---|---|---|---|---|---|---|---|
| ICD-9
|
||||||||
| 1980 | 0.29 (0.007, 1.62) | 0.44 (0.093, 1.31) | 1.11 (0.58, 1.94) | 6.01 (4.50, 7.89) | 27.5 (21.5, 31.8) | 0.86 (0.48, 1.42) | 4.35 (3.62, 5.09) | 138 |
| 1981 | 2.09 (0.84, 4.30) | 0.60 (0.16, 1.53) | 1.02 (0.51, 1.82) | 4.41 (3.14, 6.03) | 29.0 (22.9, 36.3) | 0.86 (0.48, 1.41) | 4.24 (3.56, 5.02) | 137 |
| 1982 | 0.91 (0.19, 2.65) | 0.82 (0.38, 1.57) | 5.53 (4.11, 7.30) | 29.3 (23.2, 36.5) | 0.51 (0.23, 0.97) | 4.32 (3.64, 5.11) | 141 | |
| 1983 | 0.61 (0.07, 2.21) | 0.45 (0.093, 1.32) | 0.82 (0.38, 1.56) | 5.41 (4.02, 7.13) | 30.6 (24.5, 37.8) | 0.68 (0.35, 1.19) | 4.53 (3.83, 5.32) | 149 |
| 1984 | 0.92 (0.19, 2.71) | 0.30 (0.037, 1.09) | 1.27 (0.70, 2.13) | 4.65 (3.38, 6.25) | 30.4 (24.4, 37.5) | 0.91 (0.52, 1.47) | 4.52 (3.83, 5.30) | 150 |
| 1985 | 0.44 (0.14, 1.02) | 4.76 (3.59, 6.20) | 20.8 (16.4, 26.0) | 0.28 (0.09, 0.66) | 3.77 (3.16, 4.46) | 136 | ||
| 1986 | 0.63 (0.077, 2.29) | 0.98 (0.49, 1.77) | 4.24 (3.06, 5.73) | 19.4 (14.8, 25.1) | 0.62 (0.31, 1.11) | 3.37 (2.78, 4.05) | 114 | |
| 1987 | 0.31 (0.007, 1.74) | 0.30 (0.036, 1.08) | 1.38 (0.75, 2.31) | 5.12 (3.74, 6.82) | 13.2 (9.60, 17.7) | 0.95 (0.54, 1.54) | 3.32 (2.73, 4.02) | 107 |
| 1988 | 0.67 (0.81, 2.43) | 0.16 (0.004, 0.90) | 1.74 (1.07, 2.70) | 3.99 (2.97, 5.24) | 17.1 (13.4, 21.7) | 1.19 (0.73, 1.81) | 3.84 (3.24, 4.52) | 144 |
| 1989 | 1.35 (0.35, 3.36) | 0.15 (0.004, 0.84) | 1.23 (0.67, 2.07) | 5.64 (4.30, 7.25) | 26.7 (21.5, 32.9) | 2.28 (1.28, 3.77) | 4.81 (4.11, 5.60) | 168 |
| 1990 | 0.66 (0.08, 2.39) | 0.46 (0.094, 1.33) | 0.88 (0.42, 1.61) | 5.41 (4.12, 6.99) | 30.1 (24.5, 36.5) | 0.72 (0.39, 123). | 5.02 (4.31, 5.81) | 177 |
| 1991 | 1.33 (0.36, 3.40) | 0.15 (0.0038, 0.85) | 0.96 (0.48, 1.72) | 4.95 (3.73, 6.44) | 26.9 (21.7, 32.9) | 0.67 (0.35, 1.17) | 4.64 (3.98, 5.41) | 165 |
| 1992 | 1.66 (0.54, 3.89) | 0.16 (0.0039, 0.86) | 1.40 (0.80, 2.28) | 4.50 (3.35, 5.92) | 28.0 (22.8, 34.0) | 0.95 (0.55, 1.52) | 4.82 (4.15, 5.62) | 173 |
| 1993 | 2.34 (0.93, 4.81) | 0.33 (0.038, 1.12) | 1.22 (0.67, 2.06) | 6.14 (4.80, 7.75) | 35.8 (30.0, 42.5) | 0.90 (0.51, 1.45) | 6.25 (5.46, 7.12) | 225 |
| 1994 | 0.67 (0.08, 2.41) | 0.47 (0.097, 1.32) | 1.51 (0.54, 1.83) | 5.43 (4.18, 6.93) | 29.7 (24.4, 35.8) | 0.84 (0.47, 1.39) | 5.29 (4.57, 6.10) | 192 |
| 1995 | 1.68 (0.54, 3.91) | 0.47 (0.98, 1.38) | 0.61 (0.24, 1.26) | 7.23 (5.80, 8.92) | 30.9 (25.6, 37.0) | 0.56 (0.27, 1.03) | 6.02 (5.24, 6.87) | 220 |
| 1996 | 1.01 (0.21, 2.94) | 0.63 (0.17, 1.63) | 1.13 (0.60, 1.94) | 6.27 (4.95, 7.84) | 27.4 (22.5, 33.1) | 0.96 (0.56, 1.53) | 5.53 (4.80, 6.35) | 204 |
| 1997 | 0.34 (0.09, 1.87) | 0.64 (0.18, 1.64) | 0.78 (0.36, 1.49) | 5.51 (4.28, 6.97) | 29.1 (24.0, 34.8) | 0.73 (0.39, 1.26) | 5.35 (4.63, 6.15) | 199 |
| 1998 | 0.34 (0.009, 1.88) | 0.32 (0.039, 1.68) | 0.61 (0.25, 1.26) | 6.10 (4.81, 7.61) | 38.7 (32.9, 45.2) | 0.51 (0.23, 0.96) | 6.56 (5.77, 7.43) | 246 |
|
|
||||||||
| ICD-10
|
||||||||
| 1999 | 0.67 (0.81, 2.44) | 0.16 (0.004, 0.91) | 1.05 (0.54, 1.82) | 5.05 (3.91, 6.42) | 24.8 (20.3, 30.2) | 0.73 (0.39, 1.26) | 4.89 (4.21, 5.64) | 185 |
| 2000 | 0.49 (0.10,1.43) | 1.30 (0.72,2.14) | 5.05 (3.91, 6.42) | 20.2 (16.1, 24.9) | 1.02 (0.61, 1.61) | 4.17 (3.54, 4.86) | 159 | |
| 2001 | 0.34 (0.009, 1.92) | 0.16 (0.004, 0.91) | 0.70 (0.30, 1.37) | 4.13 (3.11, 4.37) | 19.2 (15.3, 23.8) | 0.51 (0.23, 0.97) | 3.59 (3.02, 4.25) | 138 |
| 2002 | 0.35 (0.009, 1.96) | 0.32 (0.04,1.19) | 0.17 (0.021, 0.62) | 2.55 (1.77, 5.38) | 14.7 (11.4, 18.7) | 0.22 (0.06, 0.58) | 2.75 (2.24, 3.32) | 106 |
| 2003 | 0.43 (0.14, 1.01) | 2.30 (1.57, 3.24) | 11.0 (8.21, 14.5) | 0.29 (0.09, 0.67) | 2.26 (1.82, 2.79) | 88 | ||
| 2004 | 0.33 (0.040, 1.20) | 0.26 (0.054, 0.77) | 1.63 (1.03, 2.44) | 13.9 (10.7, 0.67) | 0.28 (0.09, 0.67) | 2.41 (1.95, 2.95) | 94 | |
| 2005 | 0.38 (0.01, 2.16) | 0.17 (0.004, 0.94) | 0.61 (0.24, 1.26) | 2.87 (2.06, 3.90) | 12.9 (9.88, 16.46) | 0.46 (0.20, 0.91) | 2.89 (2.38, 3.47) | 113 |
| 2006 | 0.17 (0.004, 0.94) | 0.26 (0.054, 0.77) | 2.76 (1.98, 3.77) | 7.54 (5.33, 10.4) | 0.23 (0.06, 0.59) | 2.09 (1.66, 2.59) | 82 | |
| 2007 | 0.81 (0.99, 2.94) | 0.34 (0.042, 1.25) | 0.62 (0.24, 1.27) | 1.84 (1.21, 2.68) | 8.03 (5.38, 23.8) | 0.52 (0.24, 1.00) | 2.02 (1.61, 2.52) | 80 |
Age categories with years without recorded deaths due to asthma.
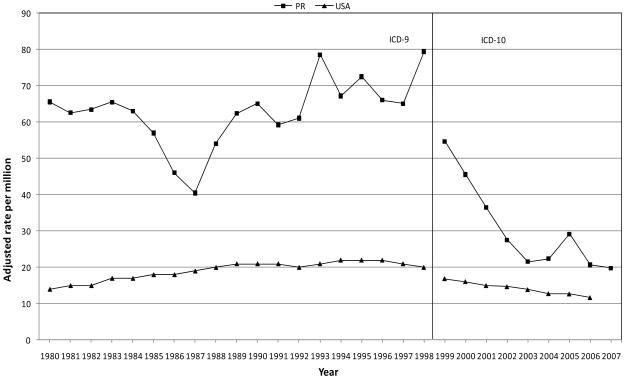
As shown in Figure 1, the age adjusted mortality rates for Puerto Rico were consistently higher than in US. In 1987 and 1998 the risk of death due to asthma was 2.13 and 4 times higher in PR than in the US. During the ICD-10 implementation, in 1999 and 2006 the risk of death due to asthma was 3.22 and 1.77 times higher in Puerto Rico than in the US.
Figure 1.
Age adjusted asthma mortality rate per 1,000,000 person/year, Puerto Rico & USA, 1980–2007.
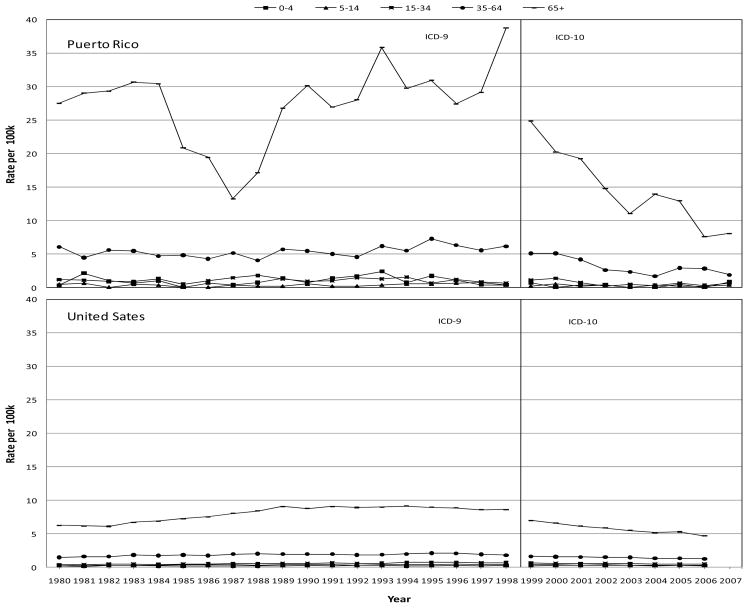
Age-specific mortality rates in Puerto Rico (Table 1) showed that the 65+ age group had significantly higher death rates due to asthma than their counterparts, while the 35–64 age group showed significantly higher rates when compared to the 0–4, 5–14 and 15–34 age groups. In 2000, the 65+ age group presented four (4) times higher risk of dying from asthma than the 35–64 age group and 15.38 higher risk than the 15–34 age group. Figure 2 shows that rates among those 65 or older fluctuated over time but remained consistently higher while in other age group rates were more stable over time. The age-specific mortality rates in the 0–4, 5–14 and 15–34 age groups were similar between Puerto Rico and US. In contrast, rates in the 35–64 age group were higher in Puerto Rico than in the US prior to the ICD-10 implementation. For those in the 65+ group, death rates were higher in Puerto Rico than in the US throughout the study period. In 1998, the 65+ age group had four (4) times higher risk of dying from asthma in Puerto Rico than in US. In 2006, the 65+ age group had 1.62 times higher risk of dying from asthma in Puerto Rico than in the US.
Figure 2.
Asthma crude mortality rate per 100,000 person/year by age group, Puerto Rico & USA form 1980 to 2007.
Regarding the 5–34 age group, Table 1 shows that asthma mortality rates increased from 0.28 per 100,000 in 1985 to 2.28 per 100,000 in 1989 followed by a decrease of 0.51 per 100,000 in 1998. Then, after the implementation of the ICD-10, the 5–34 age group asthma mortality rates ranged between 1.02 per 100,000 in 2000 and 0.23 per 100,000 in 2006.
Regression analysis was conducted to evaluate the relative risk by demographic variables adjusted for possible confounders (Table 2). A statistically significant association was not found in the adjusted model between gender and asthma mortality. The adjusted risk of death due to asthma by age revealed that the 35–64 and the 65+ age groups were significantly higher (5.21 and 17.02 per 100,000 inhabitants, respectively) than the 15–34 age group. Even though no major changes in magnitude or in direction of the associations were observed, the adjusted model revealed a confounding effect.
Table 2.
Risk on mortality due to asthma and results of multivariate regression analysis from 1999 to 2007.
| Model | N | Rate per 100k | Crude RR†† (95% CL) | Adjusted RR†† (95% CL) | Delta* |
|---|---|---|---|---|---|
| Death ~ sex | |||||
| Male† | 1,370,676 | 30.71 | 1.00 | 1.00 | |
| Female | 1,534,332 | 37.80 | 1.23 (1.10, 1.23) | 1.02 (0.90, 1.16) | −19.92% |
| Death ~ age | |||||
| 15–34 † | 1,146,011 | 6.72 | 1.00 | 1.00 | |
| 35–64 | 1,335,203 | 27.63 | 4.11 (3.87, 4.36) | 5.21 (4.95, 5.48) | 21.11% |
| 65+ | 423,794 | 130.96 | 19.49 (19.24, 19.80) | 17.02 (16.74, 17.29) | −14.53% |
| Death ~ Civil Stat | |||||
| Single† | 811,600 | 25.63 | 1.00 | 1.00 | |
| Married | 1,615,845 | 25.00 | 0.97 (0.81. 1.14) | 0.38 (0.20, 0.56) | −155.25% |
| Div/Widow | 477,563 | 81.45 | 3.17 (3.00, 3.35) | 0.67 (0.48, 0.86) | −373.21% |
| Death ~ education | |||||
| No School† | 115,929 | 67.28 | 1.00 | 1.00 | |
| Elementary | 325,825 | 126.44 | 1.88 (1.64, 2.12) | 2.15 (1.91, 2.40) | 12.72% |
| Middle/H. School | 1,407,342 | 26.57 | 0.39 (0.15, 0.64) | 0.99 (0.74, 1.24) | 60.23% |
| University | 1,055,912 | 12.97 | 0.19 (−0.09, 0.47) | 0.55 (0.27, 0.84) | 65.23% |
Reference Group
RR: Risk Ratio
Delta: ((adjusted RR-crude RR)/adjusted RR)* 100; if Delta is ± 10% then the covariates included in the model are considered confounding variables. All variables included in the table were used for adjustment.
With regards to civil status and asthma deaths, the adjusted regression model showed a significantly higher risk of asthma mortality in the Single group. The direction and magnitude of the association was highly affected by the inclusion of the confounder variables. After adjustment, the married group was modified by −155% and the divorce/widow group by −373%.
The adjusted association between asthma deaths and education showed that people in the Elementary group had 115% higher risk than those in the No School group. Adjusted asthma mortality rates in the Middle/High School group were not statistically different from the No school group. The University group was significantly lower (54%) compared to the No School group. A confounding effect was evident for the Middle/High School and University groups.
Discussion
Asthma mortality is mainly attributed to long periods of unwieldy management patterns of the condition. The poor management could be caused by a series of preventable factors such as: lack of knowledge or misapplication of the asthma guidelines by health care providers, lack of a written action plan, patient’s unawareness of the condition severity, and lack of access to specialists or medications (12, 13).
In Puerto Rico, asthma mortality rates for the period 1980–2007 showed a non-monotonic trend. The overall mortality rate had a significant decrease from 1984 to 1988 but increased until 1998. Later, in 2000 a significant decrease in the asthma mortality rate was assessed. After 2000, the rate consistently decreased until 2005. The lowest rate in the whole period was during 2007.
After adjusting mortality rate by age, we found that Puerto Ricans consistently had higher mortality rates than people in the US for the whole observed period (1980–2007). Studies conducted in the US reported that Puerto Ricans have higher asthma mortality and morbidity than other racial or ethnic groups in the United States (17, 35–37). In addition, the observed asthma mortality rate in Puerto Ricans living in the archipelago was similar to the death rate of Puerto Ricans living in the United States, from 1990 to 1995 (17). These observations support the idea that genetic factors could have an effect on Puerto Ricans’ asthma mortality rates. A study by Choudhry and colleagues (38) demonstrated that Puerto Ricans with asthma have an ethnic-specific genetic predisposition to more severe asthma when compared to Mexicans, the group with the lowest asthma prevalence in the US. Furthermore, Puerto Ricans living in the archipelago have intricate interactions between the heterogeneous ancestry mix (Native American, European, and African), socioecomic status and complex environmental triggers (39). In addition, other factors such as disease perception, limitation in access to health care services, and lack of adherence to treatment could influence the asthma mortality rates of Puerto Ricans.
The overall asthma mortality rate stratified by age showed that trends associated to the 0–4 and 15–34 age groups did not change significantly during the study period. A stable pattern was recorded in the 35–64 age group but rates were higher in Puerto Rico than in the US. The population over the age of 64 suffered the bulk of the mortality reported in both countries. However, the magnitude of the burden was much greater in Puerto Rico.
The analysis of mortality rates in the 5 to 34 years old is important in asthma epidemiologic studies due to the high accuracy in establishing diagnosis in this group. The inclusion of this age group in our analysis gave us the opportunity to compare asthma mortality rates in Puerto Rico with other countries. Based on our data, Puerto Rico not only has a higher asthma mortality rate than those reported in the US, but also higher than those reported in Austria, Finland, France, Germany, Italy and Spain among others (11).
Reasons for differences in an epidemiological trend may be multifactorial and difficult to elucidate. Several factors to explore are changes in: disease recognition, and concept; diagnosis and detection techniques; procedures to classify the cause of death; classification codes of the cause of death; precision to classify the age at death; population estimates; population age distribution; changes in the fatality rate; and incidence of the disease attributed to genetics or to environmental factors (32).
The asthma mortality rate dropped 59% between 1998 and 1999 in Puerto Rico after the ICD changed from the 9th to the 10th revision. Although the impact of the ICD change has not been documented in Puerto Rico, a study conducted at the CDC demonstrated that the ICD-10 implementation reduced US’s asthma mortality rate by 11% between 1998 and 1999 (33). The rationale for ICD periodic revisions has reflected advances in medical science and in diagnostic terminology (33). We assume that differences between classifications might affect our trends due to the following reasons: the ICD-10 is far more detailed than the ICD-9 (about 8,000 categories compared with 4,000 categories); the cause-of-death titles have been changed, and conditions have been regrouped; and some coding rules have been changed (33). Another factor that could influence mortality rates is the inaccurate reporting of asthma as the underlying cause of death due to the existing coding rules (34). Even though the accuracy of the death certificates has not been studied in Puerto Rico, events such as administrative and political changes may have influenced the Vital Statistics Office at the PRDOH and consequently the mortality trends. Nonetheless, if the aforementioned reasons hold true, we could expect to observe variation in all age groups and not only on older age groups.
Asthma mortality around the world significantly decreased, particularly in those countries adopting modern approaches to treat asthma (9). Wijesinghe (11) stated that the most likely reason for the marked reduction in asthma mortality since the late 1980’s was the spread and progressive increase in inhaled corticosteroids (ICS) use. In Puerto Rico, since 2000, strong community efforts to educate public health professionals and patients about the appropriate methods to diagnose, treat and control asthma have been conducted through diverse government, private and non-profit organizations. Many of those institutions carried out asthma initiatives based on the National Institute of Health and the Global Initiative for Asthma guidelines, which promote adequate diagnosis methods, use of ICS, use of a written asthma action plan and control of environmental triggers. It is possible that these efforts contributed significantly to the observed decreases in asthma mortality rates.
The mortality information was controlled by gender, age group, education and civil status to identify groups that may be at higher risk than others. We found that Puerto Rican females did not have a different risk of death as a cause of asthma compare to males. Asthma mortality has been observed to be higher in Puerto Rican females living in the US (17, 40). Other studies did not detect differences in asthma mortality by gender (18, 41) and still others have found higher death risk in males (32, 42, 43).
Regarding asthma mortality by age group, we observed an increase in asthma mortality rate in older age groups. Risk estimation confirms this observation even after adjusting for possible confounders. Mortality rates for the 65 and older age group fluctuated over the years of study while other age-group rates were more stable. Similarly, the New York Department of Health reported that people 65 years and older had six times higher risk of asthma mortality compared to any other age group (44). Also, it has been observed that the risk of asthma mortality increased with age in all ethnicities and races in the US (17, 40). Studies in other countries, such as, Singapore, Uruguay, Spain and France observed the same pattern (42, 45–47). Various factors may contribute to the possible explanations of this observation. First, older people naturally have higher probability of dying than the younger population. It is not unusual that the group 65+ years may have co-morbid conditions such as obesity, cardiovascular or other respiratory diseases that put them at higher risk of mortality from asthma. It is known that at younger and older ages the diagnosis of asthma is prone to be misclassified with respiratory conditions such as bronchiolitis in younger patients or with Chronic Obstructive Pulmonary Disease (COPD) in older patients (48–50). Thus, misdiagnosis can be another contributing factor to the disproportionate risk in this age group. Also, the older population might not have appropriate access to medications in order to properly manage the condition and to reduce the probability of having a fatal asthma exacerbation or an airway remodeling (49).
In terms of educational level, higher asthma mortality risk was observed in individuals who had completed only elementary school education at the moment of death, even after controling for possible confounders. This is a puzzling finding that might be explained by the lack of adjustment for other covariates, for instance, household income, occupational exposure, smoking habits, and co-morbidities.
The analysis of civil status after adjustment showed a change in magnitude and direction of the association, where single individuals had higher mortality rates than the comparison groups. Education, income, civil status and other variables have been used as surrogates of socioeconomic status (SES). We agree with Wright (51) that this is an issue that is not fully understood, and it is likely that multiple factors play contributing roles.
In conclusion, our results suggest that asthma mortality has not been stable from 1980 to 2007. Furthermore, asthma mortality rates were consistently higher in Puerto Rico than in the US. A reduction in the difference was noticeable after 2000; however, in 2007, Puerto Rico still had double the asthma mortality rate of the US. Age group and education level influenced most of the associations observed in this death record analysis. Our findings demonstrated the importance of further investigations focused on documenting external factors that affect asthma in Puerto Rico.
Acknowledgments
We thank the Office of Vital Statistics of the Puerto Rico Department of Health for providing the data. This research was supported in part by the Center for Disease Control and Prevention (1U59EH000521-01), the Ford Foundation, the National Institutes of Health Fogarty International Center (5D43TW000640) and the National Institute of Environmental Health Sciences (1D43ES018745). Thanks to Ivonne Amill for her proof reading and review contributions.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.Center for Disease Control and Prevention. Mortality data from the National Vital Statistics System. MMWR. 1989;38:119–123. [Google Scholar]
- 2.Redd SC. Asthma in the United States: Burden and current theories. Environ Health Perspect. 2002;110:557–560. doi: 10.1289/ehp.02110s4557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bousquet J, Bousquet PJ, Godard P, Daures J-P. The public health implications of asthma. World Health Organization Bulletin of the World Health Organization. 2005;83:548–554. [PMC free article] [PubMed] [Google Scholar]
- 4.Beasley R, Smith K, Pearce N, Crane J, Burguess C, Culling C. Trends in asthma mortality in New Zealand, 1908–1986. Med J Aust. 1990;153:366–367. doi: 10.5694/j.1326-5377.1990.tb125385.x. [DOI] [PubMed] [Google Scholar]
- 5.Campell MJ, Cogman GR, Holgate ST, Johnston SL. Age specific trends in asthma mortality in England and Wales, 1983–95: results of an observational study. BJM. 1997;314:1439–1441. doi: 10.1136/bmj.314.7092.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodrigo GJ, Rodrigo C, Nannini LJ. Asma casi fatal: ¿entidad clínica o manejo adecuado? Arch Bronconemol. 2004;40:24–33. doi: 10.1016/s1579-2129(06)60188-2. [DOI] [PubMed] [Google Scholar]
- 7.Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynnc C, Redd SC. Surveillace of asthma – United States, 1980–1999. MMWR. 2002;51:SS-1. [PubMed] [Google Scholar]
- 8.Oganov RG, Maslennikova GY. Asthma mortality in Russia between 1980 and 1989. Eur Respir J. 1999;13:287–289. doi: 10.1034/j.1399-3003.1999.13b11.x. [DOI] [PubMed] [Google Scholar]
- 9.Beasley R, Pearce N, Crane J. The rising trends in asthma. Wiley; Chiester: 1997. Internationals trends in asthma mortality; pp. 140–156. [DOI] [PubMed] [Google Scholar]
- 10.Braman S. The global burden of asthma. Chest. 2006;130:4–12. doi: 10.1378/chest.130.1_suppl.4S. [DOI] [PubMed] [Google Scholar]
- 11.Wijesinghe M, Weatherall M, Perrin K, Crane J, Beasley R. International trends in asthma mortality rates in the 5- to 34-year age group. Chest. 2009;135:1045–1049. doi: 10.1378/chest.08-2082. [DOI] [PubMed] [Google Scholar]
- 12.Wilson DH, Tucker G, Frith P, Appleton S, Ruffin RE, Adams RJ. Trends in hospital admissions and mortality from asthma and chronic obstructive pulmonary disease in Australia, 1993–2003. Med J Australia. 2007;186:408–411. doi: 10.5694/j.1326-5377.2007.tb00974.x. [DOI] [PubMed] [Google Scholar]
- 13.Blaiss MS. Asthma: Prevalence and Economic Implications. P&T Digest. 2005;14:610–15. [Google Scholar]
- 14.Oficina del Censo, Junta de Planificación de Puerto Rico. [accessed October 6, 2009];Population estimates. Available at: http://www.censo.gobierno.pr/Last.
- 15.Pérez-Perdomo R, Pérez-Cardona C, Disdier O, Cintrón Y. Prevalence and correlates of asthma in the Puerto Rican population: Behavioral Risk Factor Surveillance System, 2000. J Asthma. 2003;40:465–474. doi: 10.1081/jas-120018713. [DOI] [PubMed] [Google Scholar]
- 16.Hunninghake GM, Weiss ST, Celedón JC. Asthma in Hispanics. Am J Respir Crit Med. 2006;173:143–163. doi: 10.1164/rccm.200508-1232SO. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Homa D, Mannino D, Lara M. asthma mortality in US Hispanics of Mexican, Puerto Rican, and Cuban heritage, 1990–1995. Am J Repir Crit Care Med. 2000;161:504–509. doi: 10.1164/ajrccm.161.2.9906025. [DOI] [PubMed] [Google Scholar]
- 18.Grant EN, Lyttle CS, Weiss KB. The relation of sociodemografic factors and racial/ethnic differences in US asthma mortality. Am J Public Health. 2000;90:1923–1925. doi: 10.2105/ajph.90.12.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Claudio L, Stingone JA, Godbold J. Prevalence of Childhood Asthma in Urban Communities: The Impact of Ethnicity and Income. Ann Epidemiol. 2006;16:332–340. doi: 10.1016/j.annepidem.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 20.Moorman JE, Ruud RA, Johnson CA, King M, Minor P, Baily C, scalia MR, Akimbami MD Center for disease Control and Prevention. National surveillance for asthma-United States, 1980–2004. Mortality and Morbidity weekly Report. 2007;56:1–54. [PubMed] [Google Scholar]
- 21.Morgenstern H. Ecologic Studies. In: Rothman KJ, Greenland S, editors. Modern Epidemiology. Philadelphia: Lippincott-Raven; 1998. pp. 459–80. [Google Scholar]
- 22.Rosner B. Fundamentals of Biostatistics. 5. California: Duxbury Press; 2000. pp. 98–102. [Google Scholar]
- 23.Kleinbaum DJ, Kupper LL, Muller KE, Nizam A. Applied Regression Analysis and Other Multivariate Methods. 3. California: Duxbury Press; 1998. [Google Scholar]
- 24.Hosmer DW, Lemeshow S. Applied Logistic Regression. Canada: John Wiley &Sons Inc; 2000. [Google Scholar]
- 25.Oficina del Censo, Junta de Planificación de Puerto Rico. Public Use Microdata Sample. Available by request to the Puerto Rico Planning Board at June 2009. [Google Scholar]
- 26.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1979–1998. [July 28, 2010];CDC WONDER On-line Database, compiled from Compressed Mortality File CMF 1968–1988, Series 20, No. 2A, 2000 and CMF 1989–1998, Series 20, No. 2E. 2003 Accessed at http://wonder.cdc.gov/cmf-icd9.html on.
- 27.Centers for Disease Control and Prevention, National Center for Health Statistics. Compressed Mortality File 1999–2006. [July 28, 2010];CDC WONDER On-line Database, compiled from Compressed Mortality File 1999–2006 Series 20 No. 2L. 2009 Accessed at http://wonder.cdc.gov/cmf-icd10.html on.
- 28.Microsoft Inc. Microsoft Excel 2007. [Google Scholar]
- 29.Aragon T. [Accessed August 2008];Package Epitools. 2007 Available at: http://www.r-project.org/
- 30.Venables WN, Ripley BD. [Accessed June 2009];MASS package V7.2–48. 2009 Available at: http://www.r-project.org/
- 31.R Foundation. R Version 2.9.0. Vienna, Austria. Vienna, Austria: 2009. [Google Scholar]
- 32.Ito Y, Tamakoshi A, Wakai J, Takagi K, Yamaki K, Ohno Y. Trends in asthma mortality in Japan. J Asthma. 2002;39:633–639. doi: 10.1081/jas-120014928. [DOI] [PubMed] [Google Scholar]
- 33.Anderson R, Miñino AM, Hoyert DL, Rosemberg HM. Comparability of cause of death between ICD-9 and ICD-10: preliminary estimates. National Vital Statistics Reports. 2001;49:1–32. [PubMed] [Google Scholar]
- 34.Brunner WM, Ross SK, Johnson JE. Review of the asthma mortality rate for Minnesota residents aged 55 years or older, 2004–2005: when deaths certificate deserves a second look. Prev Chronic Dis. 2009:6. Available at http://www.cdc.gov/ [PMC free article] [PubMed]
- 35.Carter-Pokras OD, Green PJ. Reported asthma among Puerto Rican, Mexican-American, Cubans, 1982 through 1984. Am J Public Health. 1993;83:580–582. doi: 10.2105/ajph.83.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rose D, Mannino DM, Leadered BP. Asthma prevalence among US adults, 1998–2000: Role of Puerto Rican ethnicity and behavioral and geographical factors. Am J Public Health. 2006;96:880–888. doi: 10.2105/AJPH.2004.050039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lugogo NL, MacIntyre NR. Life-threatening asthma: pathophysiology and management. Respiratory Care. 2008;53:726–735. [PubMed] [Google Scholar]
- 38.Choudhry S, Ung N, Avila PC, Ziv E, Nazario S, Casal J, Torres A, Gorman JD, Salari K, Rodriguez-Santana JR, Toscano M, Sylvia JS, Alioto M, Castro RA, Salazar M, Gomez I, Fagan JK, Salas J, Clark S, Lilly C, Matallana H, Selman M, Chapela R, Sheppard D, Weiss ST, Ford JG, Boushey HA, Drazen JM, Rodriguez-Cintron W, Silverman EK, Burchard EG. Pharmacogenetic differences in response to albuterol between Puerto Ricans and Mexicans with asthma. Am J Respir Crit Care Med. 171(6):563–70. doi: 10.1164/rccm.200409-1286OC. [DOI] [PubMed] [Google Scholar]
- 39.Choudhry S, Burchard EG, Borrell LN, Tang H, Gomez I, Naqvi M, Nazario S, Torres A, Casal J, Martinez-Cruzado JC, Ziv E, Avila PC, Rodriguez-Cintron W, Risch NJ. Ancestry-environment interactions and asthma risk among Puerto Ricans. Am J Respir Crit Care Med. 174(10):1088–93. doi: 10.1164/rccm.200605-596OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCoy L, Redelings M, Sorvillo F, Simon P. A multiple cause of death analysis of asthma mortality in the United states, 1990–2000. J Asthma. 2005;42:757–763. doi: 10.1080/02770900500308189. [DOI] [PubMed] [Google Scholar]
- 41.Ringbaek T, Seersholm N, Viskum K. Standardise mortality rates in females and males with COPD and asthma. Eur Respir J. 2005;25:891–895. doi: 10.1183/09031936.05.00099204. [DOI] [PubMed] [Google Scholar]
- 42.Ng TP, Tan WC. Temporal trends and ethnic variations in asthma mortality in Singapore, 1976–1995. Thorax. 1999;54:990–994. doi: 10.1136/thx.54.11.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Connelly CK, Alcock SM, Prescott RJ. Mortality in asthma tics over 15 yrs: a dynamic cohort study from 1983–1998. Eur Respir J. 2002;19:593–598. doi: 10.1183/09031936.02.00203002. [DOI] [PubMed] [Google Scholar]
- 44.New York State Department of Health, Public Health Information Group Center for Community Health. New York State Asthma Surveillance Summary Report. 2007 October; Available at http://www.health.ny.gov/statistics/ny_asthma/
- 45.Baluga JC, Sueta A, Ceni M. asthma mortality in Uruguay, 1984–1988. Ann Allergy Asthma Immunol. 2001;87:124–128. doi: 10.1016/S1081-1206(10)62205-3. [DOI] [PubMed] [Google Scholar]
- 46.López-Campo JL, Cayuela A, Rodríguez-Domínguez S, Vigil E. Temporal trnds in asthma mortality over 30 years. J Asthma. 2008;45:611–614. doi: 10.1080/02770900802127006. [DOI] [PubMed] [Google Scholar]
- 47.Fuhrman C, Jougla E, Uhry Z, Delmas MC. Deaths with asthma in France, 2000–2005: a multiple-cause analysis. J Athma. 2009;46:402–406. doi: 10.1080/02770900902795553. [DOI] [PubMed] [Google Scholar]
- 48.Akinbami LJ. Advance data from vital and health statistics. Hyattsville, MD: National Center for Health Statistics; 2006. The State of childhood asthma, United States, 1980–2005; p. 381. [PubMed] [Google Scholar]
- 49.Barua P, O’Mahony Overcoming Gaps in the Management of Asthma in older Patients: New Insights. Drugs Aging. 2005;22:1029–59. doi: 10.2165/00002512-200522120-00004. [DOI] [PubMed] [Google Scholar]
- 50.Enright P. The Diagnosis and Management of Asthma is much tougher in Older Patients. Curr Opin Allergy Clin Immunol. 2002;2:175–81. doi: 10.1097/00130832-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 51.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiology research on asthma disparities. Chest. 2005;132:757–769. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]