Abstract
Background
The filarial parasites Loa loa and Mansonnella perstans are endemic in the central and western African forest block. Loa loa is pathogenic and represents a major obstacle to the control of co-endemic filariae because its treatment can cause fatal complications such as encephalitis.
Methodology/Principal Findings
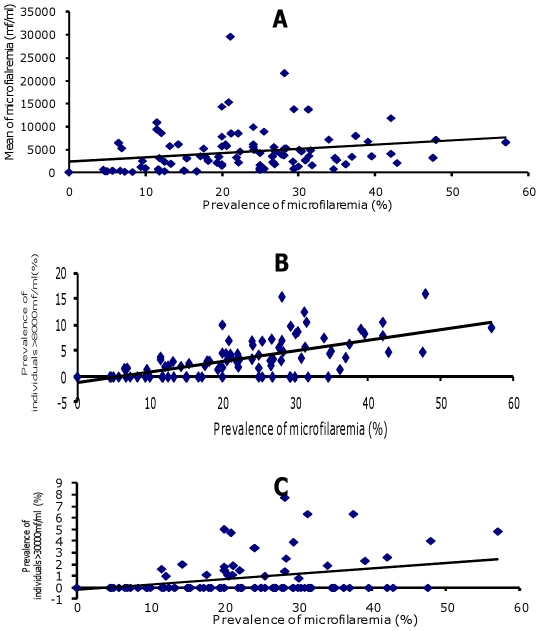
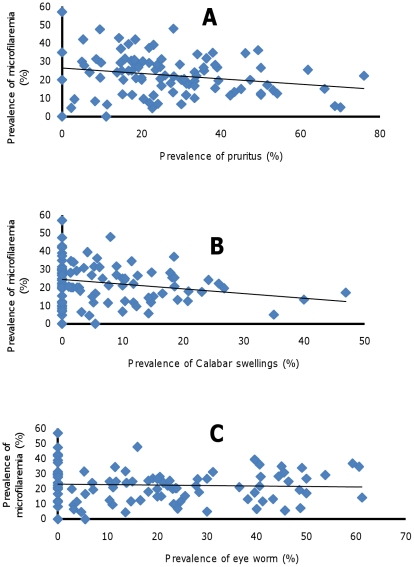
4392 individuals aged over 15 years were studied both by direct examination and a concentration technique. The overall prevalence rates were 22.4% for Loa loa microfilaremia, 10.2% for M. perstans microfilaremia, and 3.2% for mixed infection. The prevalence of both filariae was higher in the forest ecosystem than in savannah and lakeland (p<0.0001). The intensity of microfilariae (mf) was also higher in the forest ecosystem for both parasites. The prevalence and intensity of microfilaria were both influenced by age and gender. Correlations were found between the prevalence and intensity of Loa loa microfilariae (r = 0.215 p = 0.036), and between the prevalence of Loa loa and the prevalence of individuals with microfilaria >8000 mf/ml (r = 0.624; p<0.0001) and microfilariae >30 000 mf/ml (r = 0.319, p = 0.002). In contrast, the prevalence of pruritis and Calabar swellings correlated negatively with the prevalence of Loa loa microfilaria (r = −0.219, p = 0.032; r = −0.220; p = 0.031, respectively). Pruritis, Calabar swellings and eye worm were not associated with L. loa mf intensity (r = −0.144, p = 0.162; r–0.061, p = 0.558; and r = 0.051, p = 0.624, respectively), or with the prevalence or intensity of M. perstans microfilariae.
Conclusions/Significance
This map of the distribution of filariae in Gabon should prove helpful for control programs. Our findings confirm the spatial uniformity of the relationship between parasitological indices. Clinical manifestations point to a relationship between filariae and allergy.
Author Summary
Loa loa and Mansonella perstans are blood filarial parasites, endemic in the central and western African forest block, and transmitted by chrysops and culicoides flies, respectively. Loa loa is pathogenic and represents a major obstacle to the control of co-endemic filariae. Treatment of individuals with >8000 Loa loa microfilariae/ml can result in severe adverse reactions. M. perstans is prevalent in the tropics, with undefined clinical symptoms. We screened 4392 individuals for these infections in 212 Gabonese villages. The overall prevalence rates were 22.4% for Loa loa microfilariae, 10.2% for M. perstans, and 3.2% for mixed infection. These rates varied across the different ecosystems: forest, savannah, Lakeland, river (Ogouée), and equator. A correlation was found between the prevalence and intensity of microfilariae, while a negative relationship was found between clinical symptoms (pruritis, Calabar swelling) and the prevalence of Loa loa microfilaremia. This study confirms the spatial uniformity of the relationship between parasitological indices, and provides a map and baseline data for implementation of mass chemotherapy for these infections.
Introduction
Loa loa and Mansonella perstans are endemic filarial parasites in the central and western African rainforest. Loa loa infects 2 to 3 million people [1]. M. perstans is considered non pathogenic [2]–[3], although some clinical manifestations have been associated with M. perstans microfilaria [4], [5], [6] including ocular disorders [7], [8]. Interest in loiasis has grown during the last 30 years, for several reasons. First, in endemic areas loiasis is the second reason for medical visits, after malaria [1], [9]. Second, this infection mainly affects active young individuals, who contribute to agricultural productivity [10], and their health is often aggravated by co-infection by other parasites. Two-thirds of infected individuals are amicrofilaremic, despite subconjunctival migration of adults worms, suggesting immunological elimination of microfilariae [1], [11]. Severe adverse events can occur during treatment with diethylcarbamazine (DEC) and ivermectin in individuals with high-level microfilaremia, requiring close treatment monitoring and hindering mass administration of antifilarial drugs aimed at controlling other filariae in areas where Loa loa is co-endemic. This is not the case with M. perstans [12].
Many epidemiological studies of loiasis and Mansonellosis have been carried out throughout the western and central African forest block. These studies mainly focused on the distribution of loiasis and on the possible relationship between the prevalence and intensity of microfilaremia, in order to estimate the risk of adverse events during mass chemotherapy.
The prevalence of L. loa microfilaremia varies from country to country [13], as well as within a given country and even a given geographic area [14]. The highest prevalence is observed in forest areas and the lowest in savannah areas of both Gabon [15], [16] and Cameroon [17], [18], for example. Differences within a given geographic zone are directly linked to the bioecological specificity of a microzone [19]. These observations were recently used to create a predictive geographical model of loiasis endemicity based on satellite, vector habitat, prevalence, vegetation, temperature, relief, pluviometry and topography data [20]. However, when compared to field data, this model showed certain limitations [21].
A linear relationship between the prevalence and intensity of loiasis has been established. A high prevalence is indicative of intense L. loa infection and therefore a high risk of adverse events [22], [23]. The 20% threshold prevalence of microfilaremia at the community level corresponds to about 5% of high microfilaremia loads (>8000 mf/ml) and 2% of very high microfilaremia loads (>30000 mf/ml), the latter being the cut-off point above which there is a risk of severe adverse events during ivermectin treatment [24]. Owing to the difficulties of drawing regional maps based on microscopic analysis, a rapid method for evaluating the prevalence and intensity of Loa loa infection at the community level has been developed (RAPLOA: Rapid Assessment of Prevalence of Loa loa) [25]. RAPLOA is based on interviews assisted by photographs of adult worms in the eye, to detect subconjunctival migration of adult worms (which lasts 1 to 7 days), as reported by interviewees. A 40% prevalence of a history of eye worm corresponds to a 20% threshold prevalence of microfilaremia at the community level, 5% of high microfilaremia loads (>8000 mf/ml) and 2% of very high microfilaremia loads (>30000 mf/ml) [25]. Another clinical manifestation, Calabar swellings, was used to evaluate the risk of adverse events. This sign has shown to correlate with the prevalence of highly microfilaremic individuals [25].
The use of eye worm and Calabar edema to assess the risk of fatal side effects in patients with loiasis suggests a relationship between clinical symptoms and parasitological indices.
Most of these latter studies were performed in Cameroon, Nigeria, Republic of Congo and Democratic Republic of Congo [17]–[25], only a few concerning Gabon.
In Gabon, epidemiological surveys have identified five filarial species (L. loa, M. perstans, O. volvulus, M. streptocerca, and M. rodhaini), and yielded a preliminary map [12]–[16], [26]–[28]. L. loa is the predominant species and co-exists with M. perstans. The prevalence of microfilaremia varies across provinces and even within a given province, being higher in mountain forest than in savannah.
The aim of the present study was to obtain a fuller picture of the distribution of blood-borne filariae in Gabon, using both the wet blood film and concentration techniques, and to detect a linear relationship between the prevalence and intensity of loiasis and between clinical symptoms and parasitological indices. We therefore conducted a large survey, including all the country's ecological niches and recording the main clinical manifestations of Loa loa infection.
Materials and Methods
Area of study
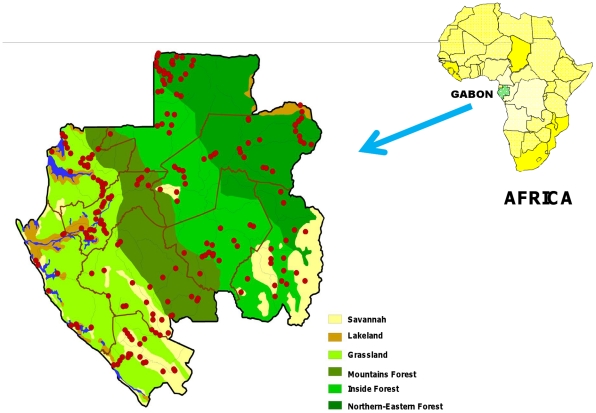
We surveyed rural Gabonese populations. The country is 800 km long and 20 to 300 km wide, consists of 80% rain forest, and is bordered to the west by the Atlantic Ocean. The forest zone extends from west to east, from the coastal basin with the grassland forest to the interior and north-eastern forest plates band, through a wide mountainous forest band from 60 to 100 km parallel to the coast. The south and southeast contain isolated areas of savannah and steppe. A coastal and continental marine ecosystem named lakeland is located around the mouth of River Ogooué (Figure 1) [29]. The population is about 1.5 million and there are 2048 villages located in 9 provinces. Rural populations are located along roads and rivers, and few villages have more than 300 inhabitants.
Figure 1. Map of Gabon with administrative regions and the locations of surveyed villages (red circles).
Strictly georeferenced and generated by MAPINFO. The ecosystems are represented in different colours.
Study population
This survey was conducted during nine-month field missions between June 2005 and September 2008. For this survey, a stratified random sampling method was used, based on the 9 provinces. Twenty to 30 villages per province were randomly selected. The required sample size was calculated on the basis of an estimated prevalence of 5 to 10% (using n = ε2 [p (1−p)]/e2; with ε = 1.96 (alpha risk = 5%), e (precision) = 2% and p = expected prevalence; with n varying from 188 to 864). Within each village, individuals over 16 years of age having lived for at least one year in their village and who accepted blood sampling where included in the study. A free medical examination was offered and basic medicines were provided to all participants and non participants, if appropriate. All the villages were georeferenced (Figure 1).
Questionnaire
The rationale of the study was explained and a one-page questionnaire was administered to all participants. We collected demographic data (age, sex and occupation), geographic data (name of the village, length of residence, department and province) and the medical history (eye worm, Calabar swellings, chronic arthralgia, pruritus, etc.) (Figure S1).
Ethical considerations
The study protocol was approved by the Ministry of Health. The Health Director, the governor of each province and the chiefs of each village received written information. Individual written consent was required before blood sampling. The results of the study were transmitted to the Ministry of Health.
Blood collection
Field laboratory facilities were set up in regional hospitals. Blood samples were collected, usually in the villages' healthcare centers, on a daily basis, into two 7-ml Vacutainer tubes containing EDTA (VWR International, France). The tubes were stored in the dark at +4°C before transportation to the field laboratory.
Parasitological analyses
Due to the variability of microfilarial load, the analysis started systematically by direct examination of a wet blood film, followed by a concentration technique. Two experienced technicians read the slides separately, and the results were controlled by a parasitologist. Briefly, microfilariae were counted directly in a 10-µl wet blood film between microscope slide and coverslip, using an optical microscope equipped with a 10× objective. Parasitemia was expressed in microfilariae per milliliter (mf/ml) of blood. A modified Knott's concentration technique [30] was applied routinely to each sample, as follows: 1 ml blood was diluted with 9 ml PBS in a conical tube and 200 µl of saponin (2% w/v) was added to lyze red cells. The tubes were centrifuged (10 min, 500 g) and the supernatants discarded. The entire pellet was then examined under the microscope (10× objective) and microfilariae were counted. Parasite species were identified by their size and motility, and by the absence or presence of a sheath.
Data analysis
Loa loa prevalence rates were estimated nationwide. As mentioned above, the 20% threshold prevalence of microfilaremia is the cut-off above which serious adverse events are likely to occur, and corresponds to 5% of high microfilaremia loads (>8000 mf/ml) and 2% of very high microfilaremia loads (>30000 mf/ml). Thus, prevalence rates were calculated in each province, village and ecosystem as prevalence rates for microfilaremia loads >8000/ml and >30000/ml. The intensity of infection was estimated as described elsewhere [25]. The difference between the results of the two laboratory tests was calculated. The Chi2 test and Fisher's exact test were used as appropriate. Minitab 16 software was used to calculate Spearman's correlation coefficient for the association between parasitological and clinical parameters, and the Mann Whitney U test was used to compare mf intensity among groups. Univariate crude conditional maximum likelihood estimates of odds ratios (OR) and exact 95% confidence intervals (CI) were determined for each potential risk factor, using STATA software version 9.0 (Stata Corporation, College Station, USA). Multivariate logistic regression models stratified by the ecosystem were constructed from risk factors with a significance of ≤0.10 in univariate analysis, using a backwards stepwise elimination procedure. P values below 0.05 were considered statistically significant.
Results
Characteristics of the study population
In total, 4392 individuals from 15 to 85 years old were enrolled in 212 villages, representing 10.7% of all villages in the country. The distance between villages ranged from 5 to 30 km. The sex ratio (M/F) was 0.88 (47.4% men and 52.6% women). About 58% of individuals were more than 45 years old and 63.9% had spent more than 10 years in their village. Farmers represented 69.8% of the population and hunters 10.2%. Around 80% of individuals were surveyed in the forest area, 10% in the savannah and the lakeland. The reported proportions of eye worm, Calabar swellings and pruritis were 29.3%, 11.2% and 22.4% (Table 1).
Table 1. Sociodemographic and clinical characteristics of the study population.
| Characteristics | Total number | Percentage % | |
| Sex | Men | 2084 | 47.4 |
| Women | 2308 | 52.6 | |
| Age | [15–30[ | 645 | 14.7 |
| [30–45[ | 1146 | 26.1 | |
| [45–60[ | 1421 | 32.4 | |
| ≥60 | 1180 | 26.9 | |
| Length of residence | <10 years | 1514 | 36.1 |
| >10 years | 2682 | 63.9 | |
| Occupation | Farming | 3067 | 69.8 |
| Hunting | 448 | 10.2 | |
| Others | 680 | 15.5 | |
| Unknown | 197 | 4.5 | |
| Location | Forest | 3478 | 79.2 |
| Savannah | 460 | 10.5 | |
| Lakeland | 454 | 10.3 | |
| Clinical examination | Eye worm | 941 | 29.3 |
| Calabar swellings | 353 | 11 | |
| Pruritus | 1229 | 29.4 | |
Comparison of microfilariae counts with and without concentration
The wet blood smear identified 790 Loa loa and 116 M. Perstans microfilaremic subjects while the concentration technique detected 984 L. loa and 447 M. perstans microfilaremic subjects (difference of 19.7% for L. loa and 74% for M. perstans) (Table 2).
Table 2. Comparison of wet blood smear and the concentration technique for the detection of the filariae.
| Filarial species | Direct examination | Leukoconcentration | Difference n (%) |
| Loa loa | 790 | 984 | 194 (19.7) |
| Mansonella perstans | 116 | 447 | 331(74) |
| TOTAL | 906 | 1431 | 525 (36.6) |
Most of these individuals who were positive only after concentration had microfilaremia below 100/ml, for both species (Table 3).
Table 3. Evaluation of the concentration technique in individuals with different levels of microfilaremia.
| Filarial species | Microfilaremia <100/ml | Microfilaremia <200/ml | Difference n (%) |
| Loa loa n = 194 | 179 | 192 | 13 (6.7) |
| Mansonella perstans n = 447 | 435 | 444 | 9 (2) |
| TOTAL n = 641 | 614 | 636 | 22 (3.4) |
Geographic distribution of L. loa and M. perstans microfilaremia
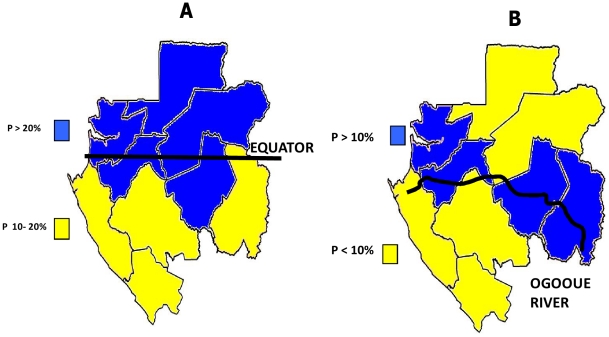
The overall prevalence rates of L. loa and M. perstans microfilaria were respectively 22.4% (95%CI: 21.2–23.7) (up to 57% in some villages), and 10.2% (95%CI: 9.3–11.1) (up to 67% in some villages), while 3.2% of subjects were coinfected (95%CI: 2.7–3.8) (Table 4, Table S1). The highest prevalence was found in the North Equator region (Figure 2A) for Loa loa (>10–20%) and along the Ogooué river for M. perstans (Figure 2B).
Table 4. Prevalence of Loa loa and Mansonella perstans microfilaremia in the nine administrative regions of Gabon.
| Provinces | Sampling period | Number of villages surveyed | Loa loa | Mansonella perstans | Co- infection | ||||||
| +/Total | % | CI 95% | +/Total | % | CI 95% | +/Total | % | CI 95% | |||
| ESTUAIRE | July 2005 | 30 | 105/314 | 33.4 | 28.3–39 | 72/314 | 22.9 | 18.5–28.1 | 29/314 | 9.2 | 6.4–13.1 |
| HAUT OGOOUE | April 2007 | 18 | 66/364 | 18.1 | 14.4–22.6 | 48/364 | 13.2 | 10–17.2 | 9/364 | 2.5 | 1.2–4.8 |
| MOYEN OGOOUE | January 2006 | 31 | 159/603 | 26.4 | 22.9–30.1 | 88/602 | 14.6 | 11.9–17.8 | 32/602 | 5.3 | 3.7–7.5 |
| NGOUNIE | June 2006 | 22 | 86/463 | 18.6 | 15.2–22.5 | 43/461 | 9.3 | 6.9–12.4 | 14/461 | 3 | 1.7–5.2 |
| NYANGA | January 2007 | 16 | 76/426 | 17.8 | 14.4–21.9 | 12/425 | 2.8 | 1.5–5 | 6/425 | 1.4 | 0.6–3.2 |
| OGOOUE IVINDO | June 2007 | 41 | 153/624 | 24.5 | 21.2–28.1 | 35/624 | 5.6 | 4–7.8 | 14/624 | 2.2 | 1.3–3.8 |
| OGOOUE LOLO | September 2007 | 18 | 118/423 | 27.9 | 23.7–32.5 | 81/423 | 19.1 | 15.6–23.3 | 23/423 | 5.4 | 3.6–8.2 |
| OGOOUE MARITIME | May 2008 | 10 | 25/206 | 12.1 | 8–17.4 | 3/206 | 1.4 | 0.3–4.2 | 1/206 | 0.5 | 0–2.7 |
| WOLEU NTEM | April 2006 | 34 | 196/969 | 20.2 | 17.8–22.9 | 65/969 | 6.7 | 5.3–8.5 | 13/969 | 1.3 | 0.7–2.3 |
| TOTAL | 220 | 984/4392 | 22.4 | 21.2–23.7 | 447/4388 | 10.2 | 9.3–11.1 | 141/4388 | 3.2 | 2.7–3.8 | |
Figure 2. Distribution of Loa loa (A) and Mansonella perstans (B) in Gabon according to the geographic region.
In the administrative regions, Estuaire province had the highest prevalence of L. loa (33.4%), M. perstans (22.9%) and co-infection (9.5%), while Ogooue maritime province had the lowest prevalence rates (respectively 12.1%, 1.4% and 0.5%) (Table 4).
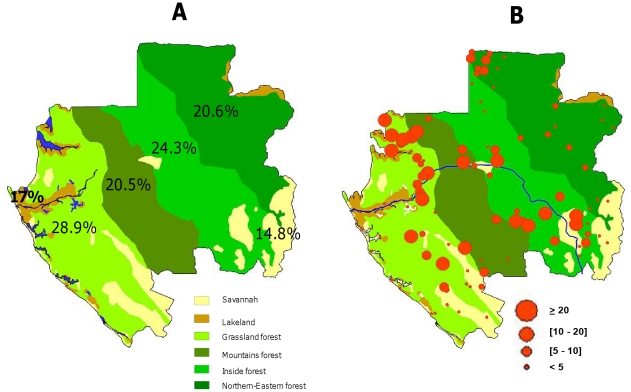
In the ecological regions, the L. loa prevalence rate (Table 5, Figure 3A) was significantly higher (p<0.0001) in the forest (24.1%) than in the lakeland (17%) and savannah (14.8%). No difference (p = 0.4) was observed between lakeland and savannah. Moreover, within the forest ecosystem, the prevalence was significantly higher in grassland (28.9%) than in the mountain (20.5%), interior (24.3%) and north eastern (20.6%) forest regions (p<0.0002). In the same way, the M. perstans prevalence rate (Table 5) was significantly higher (p<0.0001) in the forest region (11.3%) than in lakeland (4.2%) and savannah (7.4%), and no difference (p = 0.053) was observed between lakeland and savannah. Within the forest ecosystem, the prevalence in the north-eastern forest (5.2%) was significantly lower (p<0.0001) than in the grassland (14.6%), mountain (14.9%) and interior forest (11.9%) (Table 5). Finally, most villages with high L. loa prevalence rates were located in the forest area (Table S1, Figure 3B).
Table 5. Prevalence of Loa loa and Mansonella perstans microfilaremia in the main ecosystems of Gabon.
| Number of villages surveyed | Loa loa | Mansonella perstans | |||||
| Ecosystems | Positive/tested | % (95% CI) | p value | Positive/tested | % (95% CI) | p value | |
| Lakeland | 24 | 77/454 | 17 (13.7–20.8) | <0.0001 | 19/454 | 4.2 (2.6–6.6) | <0.0001 |
| Savannah | 22 | 68/460 | 14.8 (11.7–18.4) | 34/460 | 7.4 (5.2–10.3) | ||
| Forest | 174 | 839/3478 | 24.1 (22.7–25.6) | 394/3474 | 11.3 (10.3–12.5) | ||
| Grassland forest | 62 | 258/894 | 28.9 (25.9–32) | <0.0002 | 130/892 | 14.6 (12.4–17.1) | <0.0001 |
| Mountains forest | 22 | 87/425 | 20.5 (16.8–24.7) | 63/423 | 14.9 (11.7–18.7) | ||
| Inside forest | 50 | 322/1326 | 24.3 (22–26.7) | 158/1326 | 11.9 (10.2–13.8) | ||
| North eastern forest | 40 | 172/833 | 20.6 (18–23.6) | 43/833 | 5.2 (3.8–6.9) | ||
| All population | 220 | 984/4392 | 22.4 (21.2–23.7) | 447/4392 | 10.2 (9.3–11.1) | ||
Figure 3. Distribution of L. loa in Gabon in the different ecosystems (A) (Prevalence rates of Loa loa are shown within the corresponding ecosystem), and villages (B).
Analysis of risk factors
In univariate analysis, males had a significantly higher risk of Loa loa infection than females (OR: 2.38, 95%CI: 2.05–2.75, p<00001), and the prevalence of Loa loa parasitemia increased linearly with age (p<0.00001) (Table 6). The prevalence of Loa loa microfilaremia was higher in hunters than in farmers and other occupational groups (p<0.04), and higher in individuals with eye worm (p<0.001) and those without Calabar swellings (p<0.014) (Table 6). Only gender was a risk factor for M. perstans microfilaremia, males having a significantly higher prevalence than females (OR: 1.89, 95%CI: 1.54–2.31, p<0.0001) (Table 7). In multivariate analysis, only age and sex remained significantly associated with Loa loa parasitemia, throughout the country and within the forest ecosystem (Table 8 and 9).
Table 6. Univariate analysis of sociodemographic and clinical risk factors for Loa loa microfilaremia in Gabon.
| Variable | Number (%) | 95% CI | OR[95%CI] | p-value | ||
| Sex | Men | 629 (30.2) | 28.2–32.2 | 2.38 [2.05; 2.75] | <0.0001 | |
| Women | 355 (15.4) | 13.9–16.9 | 1 | |||
| Age | [15–30[ | 94 (14.6) | 11.8–17.3 | 1 | <0.0001 | |
| [30–45[ | 234 (20.4) | 18.1–22.7 | 1.50 [1.16; 1.95] | |||
| [45–60[ | 348 (24.5) | 22.2–26.7 | 1.90 [1.48; 2.44] | |||
| ≥60 | 308 (26.1) | 23.6–28.6 | 2.07 [1.60 ; 2.67] | |||
| Occupation | Farming | 657 (21.4) | 20–22.9 | 0.77 [0.61 ; 0.97] | 0.04 | |
| Hunting | 117 (26.1) | 22.2–30.5 | 1 | |||
| Others | 165 (24.3) | 21.1–27.7 | 0.91 [0.69 ; 1.19] | |||
| Clinical examination | Eye worm | Yes | 232 (24.7) | 22–27.6 | 1.34 [1.12 ; 1.61] | 0.001 |
| No | 445 (19.6) | 18–21.3 | 1 | |||
| Calabarswellings | Yes | 56 (15.9) | 12–19.7 | 0.69 [0.51 ; 0.93] | 0.014 | |
| No | 613 (21.5) | 20–23 | 1 | |||
| Pruritus | Yes | 259 (21.1) | 18.8–23.4 | 0.89 [0.76; 1.05] | 0.155 | |
| No | 682 (23.1) | 21.6–24.6 | 1 | |||
Table 7. Univariate analysis of sociodemographic and clinical risk factors for Mansonella perstans microfilaremia in Gabon.
| Variable | Number (%) | 95% CI | OR[95%CI] | p-value | ||
| Sex | Men | 275 (13.2) | 11.7–14.7 | 1.89 [1.54; 2.31] | <0.0001 | |
| Women | 172 (7.5) | 6.4–8.5 | 1 | |||
| Age | [15–30] | 55 (8.5) | 6.4–10.7 | 1 | 0.197 | |
| [30–45] | 118 (10.3) | 8.5–12.1 | 1.23 [0.88; 1.72] | |||
| [45–60] | 138 (9.7) | 8.2–11.3 | 1.15 [0.83; 1.60] | |||
| ≥60 | 136 (11.5) | 9.7–13.4 | 1.40 [1.01 ; 1.95] | |||
| Occupation | Farming | 296 (9.7) | 8.6–10.7 | 0.75 [0.55 ; 1.01] | 0.168 | |
| Hunting | 56 (12.5) | 9.4–15.6 | 1 | |||
| Others | 71 (10.4) | 8.1–12.7 | 0.82 [0.56 ; 1.18] | |||
| Clinical examination | Eye worm | Yes | 86 (9.15) | 7.3–11 | 1.23 [0.94 ; 1.61] | 0.138 |
| No | 172 (7.6) | 6.5–8.7 | 1 | |||
| Calabarswellings | Yes | 28 (7.93) | 5.1–10.8 | 0.99 [0.66 ; 1.5] | 0.998 | |
| No | 226 (7.94) | 6.9–8.9 | 1 | |||
| Pruritus | Yes | 110 (8.95) | 7.4–10.5 | 0.82 [0.65; 1.03] | 0.092 | |
| No | 315 (10.7) | 9.6–11.8 | 1 | |||
Table 8. Multivariate analysis of sociodemographic and clinical risk factors for Loa loa microfilaremia in Gabon.
| Variable | OR | [95%CI] | p-value | |
| Sex | Men/Women | 2.07 | 1.70–2.52 | <0.0001 |
| Age | [15–30[ | 1 | ||
| [30–45[ | 1.19 | 0.86–1.65 | 0.287 | |
| [45–60[ | 1.75 | 1.28–2.38 | <0.0001 | |
| ≥60 | 1.76 | 1.28–2.41 | <0.0001 | |
| Occupation | Farming | 0.94 | 0.73–1.21 | 0.614 |
| Hunting | 1 | |||
| Others | 0.83 | 0.60–1.14 | 0.244 | |
| Clinical examination | Eye worm | 1.42 | 1.17–1.73 | <0.0001 |
| Calabar swellings | 0.68 | 0.49–0.95 | 0.022 | |
| Pruritus | 0.98 | 0.81–1.20 | 0.876 | |
Table 9. Multivariate analysis of sociodemographic and clinical risk factors for Loa loa microfilaremia in forest ecosystem.
| Variable | OR | [95%CI] | p-value | |
| Sex | Men/Women | 2.07 | 1.68–2.55 | <0.0001 |
| Age | [15–30[ | 1 | ||
| [30–45[ | 1.21 | 0.85 –1.72 | 0.282 | |
| [45–60[ | 1.79 | 1.29–2.50 | <0.0001 | |
| ≥60 | 1.80 | 1.28–2.51 | <0.0001 | |
| Occupation | Farming | 0.92 | 0.70–1.21 | 0.564 |
| Hunting | 1 | |||
| Others | 0.82 | 0.57–1.15 | 0.250 | |
| Clinical examination | Eye worm | 1.42 | 1.16–1.74 | 0.001 |
| Calabar swellings | 0.61 | 0.43–0.87 | 0.006 | |
| Pruritus | 1.00 | 0.81–1.24 | 0.996 | |
For clinical symptoms, only eye worm and Calabar swellings remained significantly associated with Loa loa parasitemia, both throughout the country and within the forest ecosystem (Table 8 and 9).
Intensity of microfilaremia
Microfilaremia in Loa loa-positive individuals ranged from 1 to 500 000 mf/ml (arithmetic mean: 5441 mf/ml; median: 900 mf/ml), while M. perstans microfilaremia ranged from 1 to 12 000 mf/ml (mean: 189 mf/ml; median: 18 mf/ml) overall. Mean L. loa microfilaremia was significantly higher in the forest ecosystem than in the savannah (median values: 3469 vs 1357; p = 0.048)) and similar to that in the lakeland (3469 vs 3140; p = 0.18). There was no difference between lakeland and savannah (3140 vs 1357; p = 0.8) (Table 10).
Table 10. Intensity of Loa loa and Mansonella perstans (arithmetic mean microfilaremia) stratified by ecosystem.
| Ecosystem | Intensity of Loa loa microfilaremia | Intensity of M. perstans microfilaremia | ||
| Arithmetic mean mf/ml | Min- Max | Arithmetic mean mf/ml | Min- Max | |
| Savannah | 2660 | 1–17600 | 34.2 | 1–400 |
| Lakeland | 4626 | 1–75600 | 64 | 1–300 |
| Forest | 5742 | 0–500000 | 207.7 | 1–12000 |
| Grassland | 5859 | 1–119500 | 108.7 | 1–2000 |
| Mountains | 7777 | 0–92200 | 314.8 | 1–10900 |
| Inside | 6020 | 1–500000 | 313.6 | 1–12000 |
| Northern Eastern | 4006 | 1–83600 | 19.9 | 1–200 |
Likewise, mean M. perstans microfilaremia was significantly higher in the forest ecosystem than in the savannah (44 vs 4; p = 0.010) and lakeland (44 vs 0; p = 0.014) (Table 10).
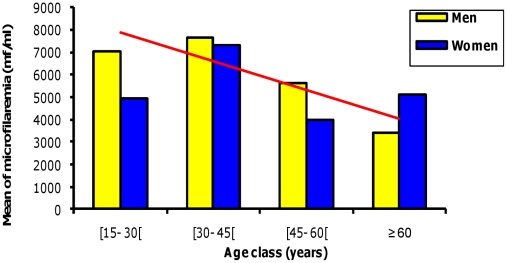
The intensity of Loa loa microfilaremia did not vary with age countrywide (r = 0.249, p = 0.634), while it correlated with age in males (r = 0.915 p = 0.011) but not in females (r = 0.684 p = 0.134) (Figure 4). At the district level, the intensity of Loa loa microfilaremia did not vary significantly with age and sex.
Figure 4. Intensity of Loa loa microfilaremia in Gabon according to age and gender.
Relationship between the prevalence and intensity of Loa loa microfilaremia
The intensity of Loa loa microfilaremia (Figure 5A) correlated with the prevalence of microfilaremia nationwide (r = 0.215 p = 0.036) but not at the regional level (r = 0.163, p = 0.675). The intensity of microfilaremia also correlated with the prevalence of microfilaremia >8000 mf/ml (Figure 5B) and >30 000mf/ml (Figure 5C) (respectively r = 0.624, p = 0.0001 and r = 0.319, p = 0.002).
Figure 5. Correlation between the prevalence and intensity of Loa loa microfilaremia.
A. Total studied population. B. In individuals with >8000 Loa microfilariae/ml. C. In individuals with >30 000 Loa microfilariae/ml.
Furthermore, in the subpopulation of individuals with microfilaremia >8000 mf/ml, this relationship was observed in lakeland (r = 0.839, p = 0.001), savannah (r = 0.625, p = 0.027) and forest (r = 0.575, p = 0.0001), while in individuals with microfilaremia >30 000 mf/ml this relationship was only observed in the forest (r = 0.328, p = 0.005).
Relationship between clinical symptoms and parasitological indices
The prevalence of pruritis correlated negatively with the prevalence of Loa loa microfilaremia (r = −0.219; p = 0.032) (Figure 6A) but not with the intensity of Loa loa microfilaria (r = −0.144; p = 0.162) or with very intense microfilaremia (>30 000: r = −0.117; p = 0.255). Similarly, microfilaria >8000 mf/ml correlated negatively with the prevalence of prurits (r = −0.22; p = 0.027). Pruritis was associated with Calabar swellings (r = 0.578; p<0.001) and eye worm (r = 0.425; p<0.001). The prevalence of Calabar swellings (Figure 6B) correlated negatively with the prevalence of L. loa microfilaria (r = −0. 220; p = 0.031) but did not correlate with the intensity of microfilaria (r = −0. 061; p = 0.558), microfilaria >8000 (r = −0.185; p = 0.071) or microfilaria >30 000 (r = 0.093; p = 0.370); in contrast, it correlated positively with the prevalence of pruritis (r = 0.578; p<0.001) and eye worm (r = 0.335; p<0.001). The prevalence of eye worm (Figure 6C) did not correlate with the prevalence of microfilaremia (r = −0.05; p = 0.624) or with microfilaremia intensity (r = −0.137, p = 0.182), microfilaria >8000 (r = −0.139; p = 0.178) or microfilaria >30 000 (r = −0.106; p = 0.302), while it correlated positively with pruritis (r = 0.425; p<0.001) and Calabar swellings (r = 0.335; p<0.001). Interestingly, there was no relationship between these three symptoms and the prevalence of M. perstans microfilaria (r = −0.146; p = 0.155 for pruritis; r = −0.090. p = 0.385 for Calabar swellings; and r = −0.164; p = 0.110 for eye worm) or the intensity of M. perstans microfilaria (pruritis: r = 0.004; p = 0.971; Calabar swelling: r = −0.169; p = 0.100; eye worm: r = 0.182; p = 0.075).
Figure 6. Correlation between the prevalence of Loa loa microfilaremia and clinical symptoms.
A. Pruritus B. Calabar swellings. C. Eye worm.
Discussion
We conducted a large-scale survey of two blood-borne filarial parasites, using direct examination and a concentration technique, in rural populations of 212 villages in Gabon, in order to map their distribution throughout the country, to characterize the modalities of population exposure and to explore the relationship between prevalence and intensity, and between clinical symptoms and parasitological indices.
The overall prevalence rates were 22.4% for Loa loa microfilariae, 10.2% for M. perstans, and 3.2% for mixed infection. These rates varied across the different ecosystems, the Ogooue River, and the equator. A correlation was found between the prevalence and the intensity of microfilariae, and between clinical symptoms (eye worm, Calabar swelling) and the prevalence of Loa loa microfilaremia.
As direct microscopic detection of microfilaria in wet blood films is not very sensitive, we combined two techniques for this survey, namely direct examination of 10 µl of blood (wet film) and prior concentration of 1 ml of blood. If we had used direct examination only, 19.7% Loa loa mf carriers and 74% of M. perstans carriers would have been missed. Most of these subjects had fewer than 100 mf/ml. Such underestimation may have implications for estimates of the risk of transmission and even for control programmes. Better sensitivity after sample concentration has been reported [14], [30], although this method is more tedious for large-scale surveys. Previous surveys used direct examination with larger volumes (30–50 µl [22], 50 µl [10] or 75 µl [19]).
The prevalence of Loa loa microfilaremia was 22.4% overall (up to 57% in some villages) while that of M. perstans was 10% (up to 67% in some villages). Gabon is thus a highly endemic country and a zone at high risk of fatal treatment complications. These prevalence rates are similar to those reported in southern Cameroon (up to 38% in the district of Elig-Mfomo) [13] and Equatorial Guinea (27%). This contrasts with Central African Republic (CAR) and Chad, where prevalence is lower (11% and 8.4% respectively). In DRC-Congo, Republic of Congo and Nigeria the prevalence rates range from 1.2% to 97% [13]. It should be noted that these prevalence rates are for specific regions of these countries, whereas our survey covered the whole of Gabon. The prevalence of Loa loa remains high in Gabon [15], [28].
Loa loa was highly prevalent in the north Equator (>20%), compared to the south (10–20%). Most areas crossed by the Ogooue River from the south-east (its source) to the north-west (towards the Atlantic Ocean) had an M. perstans prevalence of more than 10%, while other areas had a prevalence below 10%.
Among the three major ecosystems, forest had a higher prevalence of both parasites than savannah and lakeland. Differences were also seen among the different types of forest, as previously observed in Cameroon [19]. Geographic factors have been implicated in the prevalence of diseases like arteriosclerosis [31]. Sunlight might have a protective effect on some diseases [32], as ultraviolet B radiation stimulates the synthesis of vitamin D, which plays a role in immunity [33]. Geographic factors may influence filarial distribution by affecting the host immune system or the vector. The environment created by Ogooue River may affect the distribution and transmission of M. perstans. Although no soil studies around Ogooue River are available, studies in other areas have shown that low-pH soil, low organic soil content, salty soil, and wet soil promote Culicoides fly breeding [34], [35] while temperature may affect vector competence [36].
The prevalence of Loa loa microfilaremia was influenced by age in both sexes. In some parts of the country the prevalence continued to increase up to 70 years of age, while in others the prevalence appeared to plateau after 60 years. Males tended to be more microfilaremic than females, possibly because men are more exposed to chrysops bites due to their outdoor occupations (hunting, etc.), which become more intense with age, hence the correlation between age and microfilaremia. Genetic factors may also have a role [37]. Furthermore, the negative correlation of the intensity of microfilaremia with age in males may due to concomitant immunity against new incoming infection [38] or natural death of existing microfilariae [39].
In some areas of Cameroon where the general prevalence of microfilaremia exceeds 20%, approximately 5% of individuals have 8000 mf/ml and 2% have more than 30 000 mf/ml [24]. Similarly, in an area with a prevalence of 30%, 9% of carriers had >30 000 mf/ml, while in an area with a prevalence of 40%, approximately 16% of carriers had >8000 mf/ml and 5–6% had >30 000 mf/ml. Therefore, areas with a prevalence of more than 20% are considered to be at a high risk of treatment complications. Such studies have only been conducted in Cameroon [24], [25]. In this study, we observed a positive relationship between the prevalence and intensity of microfilaria. This suggests that the relationship between these two parasitological indices is spatially stable.
Clinical symptoms have also been used to predict the risk of side effects during mass chemotherapy. As previously described, eye worm and Calabar swelling have been found to correlate strongly with prevalence [25]. Photographs of ocular passage of the eye worm were used in previous studies [25]. Whether the lack of photographs in the present study influenced the accuracy of the patients' answers is not known. Yet, in our opinion, the use of photographs would yield a higher prevalence of amicrofilaremic subjects. Another striking observation is the negative correlation of pruritis and Calabar swelling with the prevalence of Loa loa but not M. perstans. Pruritis is a clinical sign of an allergic reaction. The negative relationship suggests that Loa loa filaria may induce desensitization. In Gabon, skin test reactivity against common allergens is low [40], while treatment of helminth infections increases skin test reactivity to mite antigens [41]. Similar observations have been made with M. perstans in Ugandan women [42]. A previous study in Gabon showed a high level of polyclonal IgE and Loa loa-specific IgG4 in permanent residents [27].
Further investigations are needed to elucidate the relation between filaremia and allergy in Gabon.
In conclusion, we provide a map of Loa loa and M. perstans microfilaremia in Gabon, and describe important relationships between parasitological indices and clinical manifestations. A clear and spatially uniform relationship was found between the prevalence and intensity of parasitemia. These data should be of use for planning mass chemotherapy.
Supporting Information
Prevalence and mean of Loa loa and Mansonella perstans microfilaremia in surveyed villages.
(DOC)
Questionnaire.
(PDF)
STROBE checklist.
(DOC)
Acknowledgments
We thank populations all over Gabon who accepted to participate in this study, and express our gratitude to the staff of hospitals around the country, who provided logistic support for our team during the field work.
Footnotes
The authors have declared that no competing interests exist.
Centre International de Recherches Médicales de Franceville (CIRMF) is supported by the Government of Gabon, Total Gabon, and Ministère des Affaires Etrangères de la France. This work was supported by Fonds de Solidarité Prioritaire n° 2002005700 (Ministère des Affaires Etrangères de la France) and Global Viral Forecasting Initiative, San Francisco, United States of America. The funders had no role in study design,data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Fain A. Epidémiologie de la loase. Ann Soc Belge Méd Trop. 1981;61:277–285. [PubMed] [Google Scholar]
- 2.Asio Santa Maria, Simonsen Paul, Onapa Ambrose. Mansonella perstans filariasis in Uganda: patterns of microfilaremia and clinical manifestations in two endemic communities. Trans Roy Soc Trop Med Hyg. 2009;103:266–273. doi: 10.1016/j.trstmh.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Asio Santa Maria, Simonsen EPaul, Onapa WAmbrose. A randomised, double-blind field trial of ivermectin alone and in combination with albendazole for the treatment of Mansonella perstans infections in Uganda. Trans Roy Soc Trop Med Hyg. 2009;103:274–279. doi: 10.1016/j.trstmh.2008.10.038. [DOI] [PubMed] [Google Scholar]
- 4.Anosike JC, Dozie IN, Onwuliri CO, Nwoke BE, Onwuliri VA. Prevalence of Mansonella perstans infections among the nomadic fulanis of northern Nigeria. Ann Agric Environ Med. 2005;12:35–38. [PubMed] [Google Scholar]
- 5.Fux CA, Chappuis B, Holtzer B, Aebi C, Bordman G, et al. Mansonella perstans causing symptomatic hypereosinophilia in a missionary family. Travel Med Infect Dis. 2006;4:275–280. doi: 10.1016/j.tmaid.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 6.Bregani ER, Tantardini F, Rovellini A. Mansonella perstans filariasis. Parassitologia. 2007;49:23–26. [PubMed] [Google Scholar]
- 7.Baird Kevin J, Ronald C, Neafie Daniel, Connor H. Nodule in the Conjunctiva, Bung-Eye, and Bulge-Eye in Africa Caused by Mansonella perstans. Am J Trop Med Hyg. 1988;38:553–557. doi: 10.4269/ajtmh.1988.38.553. [DOI] [PubMed] [Google Scholar]
- 8.Bregani ER, Ceraldi T, Rovellini A, Ghiringhelli C. Case report: intraocular localization of Mansonella perstans in a patient from south Chad. Trans R Soc Trop Med Hyg. 2002;96:654. doi: 10.1016/s0035-9203(02)90343-3. [DOI] [PubMed] [Google Scholar]
- 9.Boulestiex G, Carme B. Encéphalite au cours du traitement de la filariose à L. loa par la diethylcarbamazine. A propos de 6 observations. Bull Soc Pathol Exot. 1986;79:649–654. [Google Scholar]
- 10.Agbolade OM, Akinboye DO, Ogunkolo OF. Loa loa and Mansonella perstans: Neglected human infections that need control in Nigeria. Afr J Biotechnol. 2005;4:1554–1558. [Google Scholar]
- 11.Pinder M. Loa loa a neglected filarial. Parasitol Today. 1988;4:279–284. doi: 10.1016/0169-4758(88)90019-1. [DOI] [PubMed] [Google Scholar]
- 12.Keiser PB, Coulibaly YI, Keita F, Traoré D, Diallo DA, et al. Clinical characteristics of post-treatment reactions to ivermectin/albendazole for Wuchereria bancrofti in a region co-endemic for Mansonella perstans. Am J Trop Med Hyg. 2003;69:331–335. [PubMed] [Google Scholar]
- 13.Boussinesq M, Gardon J. Prevalences of Loa loa microfilaraemia throughout the area endemic for the infection. Ann Trop Med Parasitol. 1997;91:573–589. doi: 10.1080/00034989760671. [DOI] [PubMed] [Google Scholar]
- 14.Boussinesq M. Loiasis. Ann Trop Med Parasitol. 2006;100:715–731. doi: 10.1179/136485906X112194. [DOI] [PubMed] [Google Scholar]
- 15.Richard-Lenoble D, Kombila M, Carme B, Gilles JC, Delattre PY. Prevalence des filaires humaines sanguicoles au Gabon. Bull Soc Pathol Exot. 1980;73:192–199. [PubMed] [Google Scholar]
- 16.Languillat G, Garin Y, Tursz A, Beauvais B, Larivière M. Enquête sur l'étiologie de l'hypo fécondité au Gabon oriental. Rev Epidémiol Santé Publique. 1978;26:273–282. [PubMed] [Google Scholar]
- 17.Kamgno J, Boussinesq M. Hyperendémicité de la loase dans la plaine de Tikar, région de savane arbustive du Cameroun. Bull Soc Pathol Exot. 2001;94:342–346. [PubMed] [Google Scholar]
- 18.Wanji S, Tendongfor N, Esum M, Ndindeng S, Enyong P. Epidemiology of concomitant infections due to Loa loa, Mansonella perstans, and Onchocerca volvulus in rain forest of Cameroon. Med Microbiol Immunol. 2003;192:15–21. doi: 10.1007/s00430-002-0154-x. [DOI] [PubMed] [Google Scholar]
- 19.Wanji S, Tendongfor N, Esum M, Atanga SN, Enyong P. Heterogeneity in the prevalence and intensity of loiasis in five constrasting bioecological zones in Cameroon. Trans R Soc Trop Med Hyg. 2003;97:182–187. doi: 10.1016/s0035-9203(03)90114-3. [DOI] [PubMed] [Google Scholar]
- 20.Thomson MC, Obsomer V, Kamgno J, Gardon J, Wanji S, et al. Mapping the distribution of Loa loa in Cameroon in support of the African Programme for Onchocerciasis Control. Filaria J. 2004;3:7. doi: 10.1186/1475-2883-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diggle PJ, Thomson MC, Christensen OF, Rowlingson B, Gardon J, et al. Spatial modelling and prediction of Loa loa risk: decision making under uncertainty. Ann Trop Med Parasitol. 2007;101:499–509. doi: 10.1179/136485913X13789813917463. [DOI] [PubMed] [Google Scholar]
- 22.Chippaux JP, Boussinesq M, Gardon J, Gardon-Wendel N, Ernould JC. Severe adverse reaction risks during mass treatment with ivermectin in loiasis-endemic areas. Parasitol Today. 1996;12:448–450. doi: 10.1016/0169-4758(96)40006-0. [DOI] [PubMed] [Google Scholar]
- 23.Gordon J, Gardon-wendel, Demanga-Ngangue, Kamgno J, Chippaux JP, et al. Serious reaction after mass treatment of onchocerciasis with ivermectin in an area for Loa loa infection. Lancet. 1997;350:18. doi: 10.1016/S0140-6736(96)11094-1. [DOI] [PubMed] [Google Scholar]
- 24.Boussinesq M, Gardon J, Kamgno J, Pion SD, Gardon- Wendel N, et al. Relationships between the prevalence and intensity of Loa loa infection in the Central province of Cameroon. Ann Trop Med Parasitol. 2001;95:495–507. doi: 10.1080/00034980120073184. [DOI] [PubMed] [Google Scholar]
- 25.Takougang I, Meremikwu M, Wanji S, Yenshu EV, Aripko B, et al. Rapid assessment method for prevalence and intensity of Loa loa infection. Bull World Health Organ. 2002;11:852–858. [PMC free article] [PubMed] [Google Scholar]
- 26.Duong TH, Kombila M, Ferrer A, Bureau P, Gaxotte P, et al. Reduced Loa loa microfilaria count ten to twelve months after a single dose of ivermectin. Trans Roy Soc Trop Med Hyg. 1997;91:592–593. doi: 10.1016/s0035-9203(97)90040-7. [DOI] [PubMed] [Google Scholar]
- 27.Akue JP, Hommel M, Devaney E. Markers of Loa loa infection in permanent residents of a loiasis endemic area of Gabon. Trans Roy Soc Trop Med Hyg. 1996;90:115–118. doi: 10.1016/s0035-9203(96)90105-4. [DOI] [PubMed] [Google Scholar]
- 28.Richard Lenoble D, Kombila M, Burner L, Maganga ML. Filarioses au Gabon: traitement par le Mebendazole des filarioses à M. perstans et à Loa loa. Bull Soc Path Exot. 1985;78:485–491. [PubMed] [Google Scholar]
- 29.Collectif. Grands ensembles végétaux du Gabon. Atlas du Gabon. Editions du Jaguar, 2004, Paris, France.
- 30.Goldsmid JM. Studies on the laboratory diagnosis of human filariasis: preliminary communication. J Clin Path. 1970;23:632–635. doi: 10.1136/jcp.23.7.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Voors AW, Johnson WD. Altitude and arteriosclerosis heart disease mortality in white residents of 99 of the 100 largest cities in the United States. J Chronic Dis. 1979;32:157–162. doi: 10.1016/0021-9681(79)90044-4. [DOI] [PubMed] [Google Scholar]
- 32.Bodiwala D, Luscombe CJ, Liu S, Saxby M, French M, et al. Prostate cancer risk and exposure to ultraviolet radiation: further support for protective effect of sunlight. Cancer Lett. 2003;192:145–149. doi: 10.1016/s0304-3835(02)00710-3. [DOI] [PubMed] [Google Scholar]
- 33.Cannell JJ, Vieth R, Umhau JC, Holick MF, Grant WB, et al. Epidemic influenza and vitamin D. Epidemiol Infect. 2006;134:1129–40. doi: 10.1017/S0950268806007175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lubega R, Khamala CP. Larval habitats of common culicoides Latreille (Diptera, Ceratopogonidae) in Kenya. Bull Entomol Res. 1976;66:421–425. [Google Scholar]
- 35.Narladkar BW, Deshpande PD, Shivpuje PR. Bionomics and life cycle studies on culicoides sp. (Diptera: Ceratopogonidae). J Vet Parasitol. 2006;20:7–12. [Google Scholar]
- 36.Mullens BA, Gerry AC, Lysyk TJ, Schmidtmann ET. Environmental effects on vector competence and virogenesis of bluetongue virus in culicoides: interpreting laboratory data in a field context. Vet Ital. 2004;40:160–166. [PubMed] [Google Scholar]
- 37.Garcia A, Abel L, Cot M, Richard P, Ranque S, et al. Genetic epidemiology of host predisposition microfilaremia in human loiasis. Trop Med Int Health. 1999;4:565–574. doi: 10.1046/j.1365-3156.1999.00442.x. [DOI] [PubMed] [Google Scholar]
- 38.Day KP, Gregory WF, Maizels RM. Age-specific acquisition of immunity to infective larvae in a bancroftian filariasis endemic area of Papua-New Guinea. Parasite Immunol. 1991;13:277–290. doi: 10.1111/j.1365-3024.1991.tb00282.x. [DOI] [PubMed] [Google Scholar]
- 39.Pinder M, Leclere A, Evereare S. Antibody-dependent cell-mediated immune reactions to Loa loa microfilariae in amicrofilaraemic subjects. Parasite Immunol. 1992;14:541–556. doi: 10.1111/j.1365-3024.1992.tb00027.x. [DOI] [PubMed] [Google Scholar]
- 40.Van den Biggelaar Anita HJ, Lopuhaa C, van Ree R, van der Zee JS, Jans J, et al. The prevalence of Parasite Infection and House Dust Mite Sensitization in Gabonese, Schoolchildren. Int Arch Allergy Immunol. 2001;126:231–236. doi: 10.1159/000049519. [DOI] [PubMed] [Google Scholar]
- 41.Van den Biggelaar AH, Rodrigues LC, van Ree R, van der Zee JS, Hoeksma-Kruize YC, et al. Long-term treatment of intestinal helminth increases mite skin-test reactivity in Gabonese schoolchildren. J Infect Dis. 2004;189:892–900. doi: 10.1086/381767. [DOI] [PubMed] [Google Scholar]
- 42.Mpairwe H, Muhangi L, Ndibazza J, Tumuslime J, Muwanga M, et al. Skin prick test reactivity to common allergen among women in Entebbe, Uganda. Trans Roy Soc Trop Med Hyg. 2008;102:367–373. doi: 10.1016/j.trstmh.2008.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Prevalence and mean of Loa loa and Mansonella perstans microfilaremia in surveyed villages.
(DOC)
Questionnaire.
(PDF)
STROBE checklist.
(DOC)