Abstract
The aim of this study was to investigate the poorly understood relationship between the process of urbanization and noncommunicable diseases (NCDs) in Sri Lanka using a multicomponent, quantitative measure of urbanicity. NCD prevalence data were taken from the Sri Lankan Diabetes and Cardiovascular Study, comprising a representative sample of people from seven of the nine provinces in Sri Lanka (n = 4,485/5,000; response rate = 89.7%). We constructed a measure of the urban environment for seven areas using a 7-item scale based on data from study clusters to develop an “urbanicity” scale. The items were population size, population density, and access to markets, transportation, communications/media, economic factors, environment/sanitation, health, education, and housing quality. Linear and logistic regression models were constructed to examine the relationship between urbanicity and chronic disease risk factors. Among men, urbanicity was positively associated with physical inactivity (odds ratio [OR] = 3.22; 2.27–4.57), high body mass index (OR = 2.45; 95% CI, 1.88–3.20) and diabetes mellitus (OR = 2.44; 95% CI, 1.66–3.57). Among women, too, urbanicity was positively associated with physical inactivity (OR = 2.29; 95% CI, 1.64–3.21), high body mass index (OR = 2.92; 95% CI, 2.41–3.55), and diabetes mellitus (OR = 2.10; 95% CI, 1.58 – 2.80). There is a clear relationship between urbanicity and common modifiable risk factors for chronic disease in a representative sample of Sri Lankan adults.
Keywords: Urbanization, Noncommunicable disease, Sri Lanka
Introduction
Urbanization
In 2008, the world reached an invisible but important milestone where, for the first time in human history, more than 50% of the world populations were urban dwellers. It is expected that the global urban population will increase by 1.6 billion people (from 3.3 billion to 4.9 billion) by 2030, while during the same period the rural population will decrease by 28 million. The majority of this urban transition will take place in developing countries (particularly in Asia and Africa) while developed countries will experience slower growth. Within the next two decades the population of the developing world will comprise more than 80% of the world’s urban population.1
These recent and ongoing shifts in the urbanization of large populations are followed by changing patterns of disease. The United Nations (UN) recognizes that urbanization has implications for health including pollution and communicable disease and noncommunicable disease (NCD) including respiratory conditions, heart disease, cancers, and many more.2 Addressing the World Urban Forum in 2004, then-General Secretary of the United Nations Kofi Annan, said, “Rapid urban growth has become one of the major challenges facing the international community.”
In 2005, NCDs were responsible for more than 60% of deaths worldwide; and almost a third of these deaths were attributed to cardiovascular disease and diabetes mellitus.3 Currently, 80% of NCD deaths occur in 23 low and middle income countries.3,4 Without successful interventions it is estimated that heart disease, type 2 diabetes and stroke will cost developing economies US$84 billion between 2006 and 2015,7 and that half of the total burden of disease in these countries will be due to NCDs.5
Urbanization and Chronic Disease
Obesity, dietary changes (particularly increases in dietary fat intake), and physical inactivity are widely accepted lifestyle risk factors for NCDs which increase as environments become more urban.6–8 Multiple examples exist which identify associations between urban living and chronic disease risks such as diabetes mellitus, overweight and obesity, and hypertension across the developing world including Mexico,9 South Africa,10 Malaysia,11 Thailand,12 India,13 and Tanzania.14
Within Cameroon, Sobngwi et al.,15 examined the effect of time spent living in a developed (urban) environment area on a number of chronic disease risk factors. Their representative sample of adults in Cameroon showed that men who had spent more than 10 years in an urban environment, when compared with those who had never lived in an urban environment, were more than twice as likely to be overweight, have higher fasting glucose measurements, and increased blood pressure. A study of adults in the North Western province of South Africa16 found that blood pressure correlated positively with level of urbanization. A large risk factor surveillance study conducted in India found that the prevalence of diabetes was two and a half times higher in urban areas when compared to rural areas.17
Popkin and Gordan-Larsen18 describe “nutrition transition” as a recent and rapid change in the diet among populations of many developing countries, with increases in the consumption of foods sourced from animals, caloric sweeteners, and fat. Drewnoswski and Popkin19 show that the use of caloric sweeteners (including sugars and other sweeteners derived from cereals, fruits, milk, and so on) increases with the gross national product per capita of a country. Astrup and colleagues20 have identified the introduction of fast-food chains and a shift to Western dietary habits as markers of increasing obesity prevalence in what they term nutrition transition countries. These authors suggest that the increases in obesity are driven by higher energy density foods, larger portion size, and an increase in the consumption of sugar-rich soft drinks. In a cross-country analysis of over 100 countries, Ezzati et al.21 found that body mass index (BMI) and cholesterol increased rapidly with national income and level of urbanization.
Popkin and Gordan-Larsen18 show that in many developing regions, specifically Mexico, Egypt, and South Africa, obesity prevalence is outstripping rates in the developed world. There is further evidence that obesity rates in developing countries will soon match or overcome those in the developed world. The rate of increase among adults in Asia, North Africa, and Latin America are between two and five times of the rate of increase in Northern America.
Throughout the process of development and urbanization, national economies shift away from physically active economic activities such as farming, mining, and forestry toward more sedentary, often office-based occupations. Technological innovation leads to decreased activity in previously physically demanding jobs. Chinese data for 1989 to 1993 suggest that urban populations have moved from active to sedentary working patterns while employment for rural groups, particularly women, involves vigorous activity.22 Between 1989 and 1997, there was a 14% increase in household car ownership in China and children report spending around 1 hour per day watching television.
A Problem of Measurement
The development of policy responses to address the effect of urbanization as a risk for the development of NCD needs to understand how the urbanizing environment results in chronic disease. Research in this area has been limited by the basic measurement of urbanization used in the majority of research to date. The UN uses the following definitions:1
Urban—settlements or localities defined as “urban” by national statistical agencies
Urbanization—the process of transition from a rural to a more urban society
While simple, this UN definition does not provide any detail about what makes a particular region “urban.” Allender et al.’s23 systematic review identified nine health-related studies which quantified urbanization. Five used a single measure such as population density, while only four studies used more complicated measures to quantify urbanization. This review demonstrated the paucity of multi component measures of urbanization as a risk factor for NCDs and established the need for a measure of urbanization sensitive enough to track changes in urbanicity and subsequent emergence of chronic diseases or their risk factors.24
Mendez and Popkin25 created one of the few multicomponent measures which included ten components: population size, population density, access to markets, transportation, communications/media, economic factors, environment/sanitation, health, education, and housing quality. Dahly and Adair24 refined this tool into a multivariable scale and Allender et al.26 tested the feasibility of using this scale in Southern India.
It is important to develop this scale further and to assess whether it is feasible for use in other developing country settings. If it is applicable a secondary question is whether the scale can demonstrate the relationship between urbanization and chronic disease risk. The research questions informing this study were:
Is it possible to use a multicomponent measure of urbanicity as an exposure for chronic disease risk in Sri Lanka?
What associations exist between an urbanicity scale and chronic disease risk between areas of different urbanicity in Sri Lanka?
Methods
Noncommunicable Disease and Risk Factors Prevalence
The 2007–2008 Sri Lanka Diabetes and Cardiovascular Study (SLDCS) was a cross sectional study designed by the Oxford Centre for Diabetes, Endocrinology, and Metabolism and the University of Colombo Diabetes Research Unit to measure the prevalence of cardiovascular disease/risk factors in Sri Lanka.
This study was conducted in seven out of nine provinces in Sri Lanka, excluding the North and Eastern provinces, which were unsafe during the study period. Study methods have been reported elsewhere,27 but in brief the SLDCS thus provides a nationally representative sample of 4,485 noninstitutionalized adults over 18 years, excluding those who were pregnant, long term ill, or who declined to participate. The overall response rate for participation was 91%. Data were collected by trained medical graduates and nurses within each study community. An interviewer—administered questionnaire was used to collect sociodemographic factors, medical history, and details on smoking, alcohol and physical activity.
Measuring Urbanization
We assigned a maximum of 10 points to each item of the adapted urbanicity scale, with a resulting range from 0 (no urbanicity) to 70 (high urbanicity) points. The items were population size, population density, access to markets, transportation, communications/media, economic factors, environment/sanitation, health, education, and housing quality.
For each of the study villages, the village administrative officer was contacted and asked to provide the relevant information about their village. These data were collected through personal or telephone interview between April and June 2009 in Sinhala or English languages. Urbanization data were collected across the 100 villages to match the 2007–2008 SLDCS. Clusters were grouped into three categories according to tertiles of urbanization score: 1—low urbanicity, 2—medium urbanicity, and 3—high urbanicity.
Data Analysis
Initial analysis produced descriptive statistics for the total sample and each urbanicity group. For continuous exposure data of normal distribution, a one-way analysis of variance (ANOVA) test was used to analyze the relationship between outcome variables from each of the urbanicity groups. A Kruskall–Wallis one-way ANOVA test was used for continuous exposure data not normally distributed. Normality was assessed by reviewing histograms and normal probability–probability plots of the data. A Mantel–Haenszel χ2 test and regression analyses were used to estimate the effect of urbanicity controlled for potential confounders and to assess for effect modification. Linear (in the case of continuous outcome variables) and logistic (in the case of binary outcome variables) regression methods were used to explore differences between the groups, with adjustment for confounding variables. Data assumptions related to linear regression methods were checked. All statistical analyses were performed using Statistical Package for the Social Sciences (Version 16) STATA, version 10.0 (StataCorp LP, College Station, TX, USA).
Ethical Approval
The ethics committee at the University of Colombo approved the SLDCS study.
Results
Urbanicity
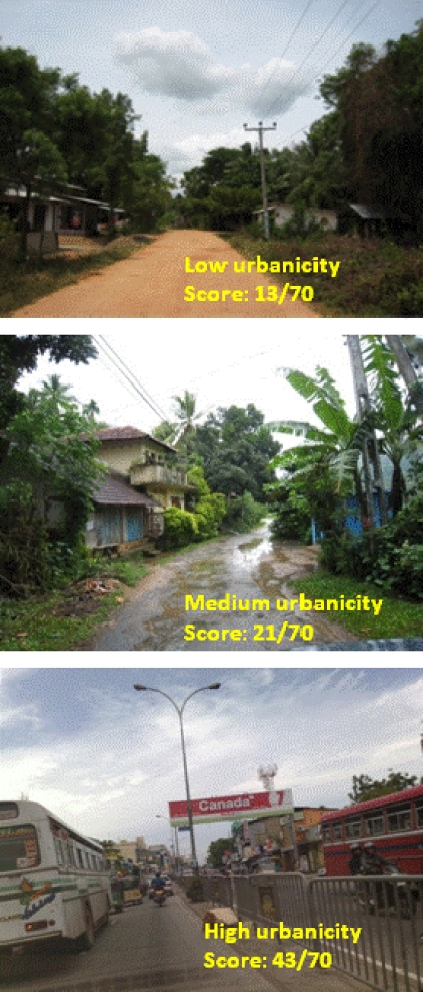
Figure 1 provides a visual representation of the spectrum of urbanicity measured in this study. Urbanicity ranged from 11 to 46 (mean = 22.08; SD = 8.5). The cut points for the tertiles of urbanicity were 16, 23, and, 26.
Fig. 1.
Photographs of the main road in areas representing three different levels of urbanicity, Sri Lanka
Participants in each stratum of urbanization had a similar proportion of men (low, 38%; medium, 41%; high, 39%) and the mean age of each stratum was also similar ranging from 45.3 to 46.1. The proportion achieving education above secondary school was higher in the most urban area (5%) compared to the least urban area (1%), and the proportion in the two highest income brackets (>37,500 Sri Lankan rupees) was higher in the most urban area (10%) than the least urban area (3%) (Table 1).
Table 1.
Descriptive information on study participants
| Low | Medium | High | Total | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |
| Gender | ||||||||
| Male | 606 | 38.1% | 640 | 41.0% | 526 | 39.4% | 1,772 | 39.5% |
| Female | 984 | 61.9% | 921 | 59.0% | 808 | 60.6% | 2,713 | 60.5% |
| Total | 1,590 | 35.5% | 1561 | 34.8% | 1,334 | 29.7% | 4,485 | 100.0% |
| Age | ||||||||
| Mean | 45.5 | 47.5 | 45.3 | 46.1 | ||||
| SD | 15.1 | 15.3 | 14.8 | 15.1 | ||||
| Range | 18–90 | 18–89 | 18–85 | 18–90 | ||||
| Education | ||||||||
| Primary school | 527 | 33.2% | 317 | 20.3% | 229 | 17.2% | 1,073 | 23.9% |
| Secondary school | 1,039 | 65.5% | 1200 | 76.9% | 1,040 | 78.0% | 3,279 | 73.2% |
| Above school | 21 | 1.3% | 44 | 2.8% | 65 | 4.9% | 130 | 2.9% |
| Income (Sri Lanka rupees) | ||||||||
| <3500.00 | 1,081 | 69.5% | 845 | 55.2% | 527 | 40.1% | 2,453 | 55.8% |
| <10000.00 | 279 | 17.9% | 381 | 24.9% | 391 | 29.8% | 1,051 | 23.9% |
| <17000.00 | 152 | 9.8% | 230 | 15.0% | 259 | 19.7% | 641 | 14.6% |
| <37500.00 | 39 | 2.5% | 61 | 4.0% | 107 | 8.1% | 207 | 4.7% |
| <75000.00 | 4 | 0.3% | 13 | .8% | 30 | 2.3% | 47 | 1.1% |
Among Sri Lankan men, smoking prevalence was highest in the low urban category (42%) compared to 35% and 40% in medium and high urban categories, respectively. Insufficient physical activity was reported from more than one-fifth (23%) of the most urban participants compared with 8% and 13% of middle and low urban respondents, respectively. The prevalence of overweight (BMI > 23 kg/m2) was highest in the high urban areas (38%) compared to low (20%) and middle (28%) urban areas (Table 2). Almost 16% of urban men were diagnosed with diabetes mellitus compared with 7.4% and 10.8% of men in low and middle urbanicity areas, respectively. Prevalence of hypertension was highest in the middle urban (71%) group than the low (63%) and high (67%) urban groups.
Table 2.
Prevalence of selected NCD risk factors by level of urbanicity, Sri Lanka
| Risk factor | Urbanicity group | Male Total (1,772) | Prev. % | (95% CI) | Female Total (1,772) | Prev. % | (95% CI) |
|---|---|---|---|---|---|---|---|
| Daily smoking | Low | 606 | 41.7 | 37.8–45.7 | 984 | 0.1 | 0.1–0.3 |
| Medium | 640 | 34.7 | 31.0–38.4 | 921 | 0.1 | 0.1–0.3 | |
| High | 526 | 39.7 | 35.5–43.9 | 808 | 0.0 | – | |
| Low physical activity | Low | 606 | 8.4 | 6.2–10.6 | 984 | 6.0 | 4.5–7.5 |
| Medium | 640 | 13.6 | 10.9–16.3 | 921 | 8.1 | 6.4–10.0 | |
| High | 526 | 22.8 | 19.2–26.4 | 808 | 12.7 | 10.4–15.0 | |
| High BMI | Low | 606 | 19.6 | 16.5–22.8 | 984 | 30.7 | 27.8–33.6 |
| Medium | 640 | 27.7 | 24.1–31.1 | 921 | 35.7 | 32.7–38.8 | |
| High | 526 | 37.5 | 33.3–41.6 | 808 | 56.4 | 53.0–59.9 | |
| Diabetes mellitus | Low | 606 | 7.4 | 5.3–9.5 | 984 | 8.8 | 7.0–10.6 |
| Medium | 640 | 10.8 | 8.3–13.2 | 921 | 12.1 | 10.0–14.2 | |
| High | 526 | 16.3 | 13.2–19.5 | 808 | 16.7 | 14.4–19.5 | |
| High blood pressure | Low | 606 | 63.2 | 59.3–67.0 | 984 | 56.3 | 53.2–59.4 |
| Medium | 640 | 70.8 | 67.2–74.3 | 921 | 60.3 | 57.0–63.4 | |
| High | 526 | 67.1 | 63.0–71.1 | 808 | 57.9 | 54.5–61.3 |
Daily smoking: smoking any form of tobacco (cigarettes, bidi, or cigars) either every day or on some days, at the time of the study or within the preceding 6 months
Low physical activity: Those not in mild, moderate, or health-enhancing physically active groups
High BMI: BMI (height cm/weight kg2) >23 kg m2
Diabetes mellitus: fasting plasma glucose (FPG) was ≥7.0 mmol/l or 2 h post-OGTT plasma glucose was ≥11.1 mmol/l
High blood pressure: Any value above 120 systolic/80 diastolic
CI confidence interval, NCD noncommunicable disease
Among Sri Lankan women, the prevalence of current smoking was less than 1% across all three levels of urbanicity groups. Almost 13% of urban women were physically inactive, compared with 8% and 6% of women in middle and low urbanicity areas, respectively. The prevalence of overweight was lowest among the low urban respondents (31%) compared to mid (36%) and high (57%) urban respondents (Table 2). Diabetes mellitus prevalence was highest in the high urban areas (16.7%) compared to low (8.8%) and middle (12.1%) urban areas. Prevalence of hypertension was 56% among the low urban respondents and 60% and 58% in mid and high urban respondents.
Using the lowest urbanicity group as a referent Table 3 shows that urban dwelling men were three times more likely to be physically inactive (odds ratio [OR] = 3.22; 95% confidence interval [CI], 2.27–4.57), more than twice as likely to have increased BMI (2.45; 1.88–3.20) and more than twice as likely to have diabetes mellitus (2.44; 1.66–3.57). Adjustment of these results for age and income show that these relationships remain significant; physically inactive (OR = 2.79; 95% CI, 1.92–4.04), increased BMI (1.80; 1.41–2.48), diabetes mellitus (2.05; 1.35–3.11).
Table 3.
Crude and adjusted odds ratios for NCD risk factor, by urbanicity group, Sri Lanka
| Risk factor | Urbanicity group | OR | (95% CI) | P value | Adjusted OR | (95% CI) | P value | ||
|---|---|---|---|---|---|---|---|---|---|
| Low | High | Low | High | ||||||
| Men | |||||||||
| Daily smoking | Low | 1.00 | 0.000 | 1.00 | 0.000 | ||||
| Medium | 0.74 | 0.59 | 0.93 | 0.78 | 0.62 | 0.99 | |||
| High | 0.92 | 0.72 | 1.17 | 1.05 | 0.82 | 1.35 | |||
| Low physical activity | Low | 1.00 | 0.000 | 1.00 | 0.000 | ||||
| Medium | 1.71 | 1.19 | 2.47 | 1.59 | 1.09 | 2.32 | |||
| High | 3.22 | 2.27 | 4.57 | 2.79 | 1.92 | 4.04 | |||
| High BMI | Low | 0.000 | 1.00 | 0.000 | |||||
| Medium | 1.56 | 1.20 | 2.04 | 1.42 | 1.08 | 1.86 | |||
| High | 2.45 | 1.88 | 3.20 | 1.80 | 1.41 | 2.48 | |||
| Diabetes mellitus | Low | 1.00 | 0.000 | 1.00 | 0.000 | ||||
| Medium | 1.51 | 1.02 | 2.23 | 1.30 | 0.86 | 1.98 | |||
| High | 2.44 | 1.66 | 3.57 | 2.05 | 1.35 | 3.11 | |||
| High blood pressure | Low | 1.00 | 0.000 | 1.00 | 0.000 | ||||
| Medium | 1.41 | 1.11 | 1.79 | 1.30 | 1.02 | 1.66 | |||
| High | 1.19 | 0.93 | 1.52 | 1.05 | 0.80 | 1.36 | |||
| Women | |||||||||
| Daily smoking | Low | 1.00 | 0.000 | 1.00 | 0.000 | ||||
| Medium | 1.39 | 0.98 | 1.98 | 1.25 | 0.85 | 1.84 | |||
| High | 2.29 | 1.64 | 3.21 | 2.26 | 1.56 | 3.25 | |||
| Low physical activity | Low | 1.00 | 0.000 | 1.00 | 0.000 | ||||
| Medium | 1.25 | 1.04 | 1.52 | 1.12 | 0.92 | 1.37 | |||
| High | 2.92 | 2.41 | 3.55 | 2.47 | 2.02 | 3.01 | |||
| Diabetes mellitus | Low | 1.00 | 0.000 | 1.00 | 0.000 | ||||
| Medium | 1.43 | 1.06 | 1.92 | 1.27 | .93 | 1.74 | |||
| High | 2.10 | 1.58 | 2.80 | 2.14 | 1.58 | 2.91 | |||
| High blood pressure | Low | 1.00 | 0.000 | 0.000 | |||||
| Medium | 1.18 | 0.99 | 1.41 | 1.06 | 0.88 | 1.29 | |||
| High | 1.07 | 0.88 | 1.29 | 0.99 | 0.81 | 1.22 | |||
Urbanicity is categorized into tertiles
Daily smoking: smoking any form of tobacco (cigarettes, bidi, or cigars) either every day or on some days, at the time of the study or within the preceding 6 months. Too few smokers among women to calculate results
Low physical activity: those not in mild, moderate, or health-enhancing physically active groups
High BMI: BMI (height cm/weight kg2) >23 kg m−2
Diabetes mellitus: fasting plasma glucose (FPG) was ≥7.0 mmol/l or 2 h post-OGTT plasma glucose was ≥11.1 mmol/l
High blood pressure: any value above 120 systolic/80 diastolic
Adjusted model for age and income
CI confidence interval, NCD noncommunicable disease
Using the lowest urbanicity group as a referent, Table 3 shows that urban dwelling women were more than twice as likely to be physically inactive (OR = 2.29; 95% CI, 1.64–3.21), almost three times as likely to have increased BMI (2.92; 2.41–3.55) and more than twice as likely to have diabetes mellitus (2.10; 1.58–2.80) than their rural counterparts. Adjustment of these results for age and income show that these relationships remain significant: physically inactive (OR = 2.26; 95% CI, 1.56–3.25), increased BMI (2.47; 2.02–3.01), diabetes mellitus (2.14; 1.58–2.91).
Discussion
Principal Findings
This study demonstrated that it was possible to collect urbanicity data and that this scale can help illuminate the relationship between urbanicity and NCD risk factors. A clear relationship was observed between risk factors for chronic disease and level of urbanicity. The relationships were observed in more distal risk factors such as BMI and physical inactivity rather than proximal risk factors such as blood pressure and cholesterol. Reasons for this may include the time lag for the effect of urbanization in Sri Lanka so that urbanization has affected the proximal risk factors but that we are yet to see significant changes in the harder medical outcomes such as hypertension.
Strengths and Weaknesses of the Study
There have been few studies of chronic disease prevalence in Sri Lanka, even fewer at the national level, and none which have used a representative sample to examine the relationship between urbanicity and noncommunicable disease risk factors. Previous work28 provided surveillance data for 2003, but from only one province of Sri Lanka. This study is the first to use an objective measure of urbanicity alongside a nationally representative sample rather than the existing government classification. While this makes it difficult to make direct comparisons with existing studies, it also overcomes the previous problem whereby urbanization was defined by administrative boundaries without taking into account those elements of the environment that would be likely to infer an increase in NCD risk.
The SLDCS study is based on interviewer collected anthropometry, biochemistry, and self report data. The self-reported behavioral data are susceptible to social desirability bias and the collection of biometric and anthropometric data provides more objective measures of NCD risk. We observed similar directions in the association between urbanicity and self-reported risk behaviors and urbanicity and anthropometric measures. More detailed risk factor information should be collected in future studies. Dietary information in this study was limited and future work should collect information on fat, oil, sugar, and processed food consumption.
A second strength of this study is that it develops a previously used tool and provides more evidence that the data collected does reflect some elements of the urban environment that pertain to increased chronic disease risk. In contrast to studies that rely on a population based dichotomy defining urban versus rural, this study builds on hypothesized relationships and helps develop a picture of those elements of the rapidly urbanizing environment that are important for NCD risk.
Strengths and Weaknesses in Relation to other Studies, Discussing Particularly any Differences in Results
There are few risk factor surveillance studies conducted in Sri Lanka and even fewer which examine urban and rural differences. The WHO world health survey reported daily cigarette smoking prevalence as 24.6% for males and 1.7% for females in Sri Lanka. They used the existing administrative urban/rural definition and reported smoking prevalence around 13% for both sexes in urban and rural areas.28 The large variance in smoking rates between the least urban (41%) and middle urban (35%) shown in our study demonstrates the importance of considering an objective measure of urbanization. Perera et al.29 reported daily smoking prevalence as 21% for males and 0.6% for females.
There are similarities between obesity prevalence figures presented in previous studies and this paper. A WHO Steps survey (sample from Western Province) reported mean BMI (kg m−2) of 22 for males and 23 for females while this study reported 21 for males and 22.1 for females. Another study conducted in Colombo district showed a difference in BMI between urban (males: 23.3; 22.8–23.8; women: 24.2; 23.7–24.7) and rural (men: 22.3; 21.9–22.7; women: 23.2; 22.7–23.7).30
Meaning of the Study: Possible Mechanisms and Implications for Clinicians or Policymakers
The studies of urbanicity presented above show the type of evidence that is important for health systems, practitioners, and policy makers considering the social, economic and urban environment when developing policy options to prevent obesity and chronic disease.
There are some examples of specific policy approaches that might be considered. Chow et al.31 shows solid evidence from developed countries that tobacco price policy can reduce tobacco consumption. Interestingly, when considering the hours of labor spent to purchase cigarettes, the relative cost has increased in the developed world, while cigarettes have become cheaper in much of the developing world.32
Unanswered Questions and Future Research
There are clearly established relationships between living in an “urban” area and increases in chronic disease risk and prevalence. There is little known about how different aspects of the urban context affect different risk factors for chronic disease. Most of our understanding comes from studies set in developed countries, yet the coming burden of urbanization is likely to be most closely felt in the developing world. A far clearer understanding of the ways in which different elements of the urban environment lead to specific disease risks is needed before we can suggest, implement, and test policy change to alleviate the overwhelming predicted burden of disease as countries develop.
Conclusion
This study demonstrated that it was possible to quantify urbanization in a continuous multicomponent scale. There is a clear relationship between the level of urbanization in Sri Lanka and noncommunicable disease risk factors.
Immediate policy level action is needed to manage health issues arising from future planned urbanization and to overcome the likely detriments associated with past unplanned urbanization in Sri Lanka.
References
- 1.State of world population: Unleashing the potential of urban growth. New York, NY: The United Nations Free Peoples Association; 2007.
- 2.Patel RB, Burke TF. Urbanization – an emerging humanitarian disaster. N Engl J Med. 2009;361(8):741–3. doi: 10.1056/NEJMp0810878. [DOI] [PubMed] [Google Scholar]
- 3.Strong KL, Mathers CD, Leeder S, Beaglehole R. Preventing chronic diseases: how many lives can we save? Lancet. 2005;366:1578–82. doi: 10.1016/S0140-6736(05)67341-2. [DOI] [PubMed] [Google Scholar]
- 4.Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. The burden and costs of chronic diseases in low-income and middle-income countries. Lancet. 2007;370:1929–38. doi: 10.1016/S0140-6736(07)61696-1. [DOI] [PubMed] [Google Scholar]
- 5.Mathers1 CD, Loncar D. Updated projections of global mortality and burden of disease, 2002–2030. World Health Organization. 2008. http://www.who.int/healthinfo/global_burden_disease/en/index.html. Accessed May 3, 2009. [DOI] [PMC free article] [PubMed]
- 6.Cockram CS. Diabetes mellitus: perspective from the Asia-Pacific region. Diab Res Clin Pract. 2000;2:S3–7. doi: 10.1016/S0168-8227(00)00202-3. [DOI] [PubMed] [Google Scholar]
- 7.Azeredo Passos VM, Barreto SM, Diniz LM, Lima-Costa MF. Type 2 diabetes: prevalence and associated factors in a Brazilian community—the Bambuí health and aging study. Sao Paulo Med J. 2005;123(2):66–71. doi: 10.1590/S1516-31802005000200007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu FB, Wang B, Chen C, et al. Body mass index and cardiovascular risk factors in a rural Chinese population. Am J Epidemiol. 2000;151:88–97. doi: 10.1093/oxfordjournals.aje.a010127. [DOI] [PubMed] [Google Scholar]
- 9.Rivera JA, Barquera S, González-Cossío T, Olaiz G, Sepúlveda J. Nutrition transition in Mexico and in other Latin American countries. Nutr Rev. 2004;62(7 Pt 2):S149–57. doi: 10.1111/j.1753-4887.2004.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 10.Vorster HH. The emergence of cardiovascular disease during urbanisation of Africans. Public Health Nutr. 2002;5(1A):239–43. doi: 10.1079/PHN2001299. [DOI] [PubMed] [Google Scholar]
- 11.Noor MI. The nutrition and health transition in Malaysia. Public Health Nutr. 2002;5(1A):191–5. doi: 10.1079/PHN2001293. [DOI] [PubMed] [Google Scholar]
- 12.Kosulwat V. The nutrition and health transition in Thailand. Public Health Nutr. 2002;5(1A):183–9. doi: 10.1079/PHN2001292. [DOI] [PubMed] [Google Scholar]
- 13.Shetty PS. Nutrition transition in India. Public Health Nutr. 2002;5(1A):175–82. doi: 10.1079/PHN2001291. [DOI] [PubMed] [Google Scholar]
- 14.Maletnlema TN. A Tanzanian perspective on the nutrition transition and its implications for health. Public Health Nutr. 2002;5(1A):163–8. doi: 10.1079/PHN2001289. [DOI] [PubMed] [Google Scholar]
- 15.Sobngwi E, Mbanya JC, Unwin NC, et al. Exposure over the life course to an urban environment and its relation with obesity, diabetes, and hypertension in rural and urban Cameroon. Int J Epidemiol. 2004;33:769–76. doi: 10.1093/ije/dyh044. [DOI] [PubMed] [Google Scholar]
- 16.Rooyen JM, Kruger HS, Huisman HW. An epidemiological study of hypertension and its determinants in a population in transition: the THUSA study. J Hum Hypertens. 2000;14(12):779–87. doi: 10.1038/sj.jhh.1001098. [DOI] [PubMed] [Google Scholar]
- 17.Mohan V, Mathur P, Deepa R, et al. Urban rural differences in prevalence of self-reported diabetes in India—The WHO–ICMR Indian NCD risk factor surveillance. Diab Res Clin Pract. 2008;10:1016–8. doi: 10.1016/j.diabres.2007.11.018. [DOI] [PubMed] [Google Scholar]
- 18.Popkin B, Gordan-Larsen P. The nutrition transition: worldwide obesity dynamics and their determinants. Int J Obes Related Metab Disord. 2004;28(Suppl 3):2–9. doi: 10.1038/sj.ijo.0802804. [DOI] [PubMed] [Google Scholar]
- 19.Drewnoswski A, Popkin BM. The nutrition transition: new trends in the global diet. Nutr Rev. 1997;55:31–43. doi: 10.1111/j.1753-4887.1997.tb01593.x. [DOI] [PubMed] [Google Scholar]
- 20.Astrup A, Dyerberg J, Selleck M, Stender S. Nutrition transition and its relationship to the development of obesity and related chronic diseases. Obes Rev. 2008;9(Suppl 1):48–52. doi: 10.1111/j.1467-789X.2007.00438.x. [DOI] [PubMed] [Google Scholar]
- 21.Ezzati M, Vander Hoorn S, Lawes C, et al. Rethinking the diseases of affluence paradigm: global patterns of nutritional risks in relation to economic development. PLoS Medicine 2005; 2(5):e133. [DOI] [PMC free article] [PubMed]
- 22.Popkin BM. Urbanization, lifestyle changes and the nutrition transition. World Dev. 1999;27:1905–16. doi: 10.1016/S0305-750X(99)00094-7. [DOI] [Google Scholar]
- 23.Allender S, Foster C, Hutchinson L, Arambepola C. Quantification of urbanization in relation to chronic diseases in developing countries: a systematic review. J Urban Health. 2008;85:938–51. doi: 10.1007/s11524-008-9325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dahly DL, Adair LS. Quantifying the urban environment: a scale measure of urbanicity outperforms the urban–rural dichotomy. Soc Sci Med. 2007;64(7):1407–19. doi: 10.1016/j.socscimed.2006.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mendez MA, Popkin BM. Globalization, urbanization and nutritional change in the developing world. Electron J Agric Dev Econ. 2004;1:220–41. [Google Scholar]
- 26.Allender S, Lacey B, Webster P, et al. Level of urbanization and noncommunicable disease risk factors in Tamil Nadu, India. Bull World Health Organ. 2010;88(4):297–304. doi: 10.2471/BLT.09.065847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katulanda P, Constantine GR, Mahesh JG, et al. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka — Sri Lanka Diabetes, Cardiovascular study (SLDCS) Diabet Med. 2008;25:1062–9. doi: 10.1111/j.1464-5491.2008.02523.x. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. World Health Survey 2003, Sri Lanka. http://apps.who.int/infobase/mddetails.aspx?surveycode=101735a1. Accessed March 31, 2010.
- 29.Perera B, Fonseka P, Ekanayake R, Lelwala E. Smoking in adults in Sri Lanka: prevalence and attitudes. Asia Pac J Publ Health. 2005;17:40–5. doi: 10.1177/101053950501700110. [DOI] [PubMed] [Google Scholar]
- 30.Arambepola C, Allender S, Ekanayake R, Fernando D. Urban living and obesity: is it independent of its population and lifestyle characteristics? Trop Med Int Health. 2008;13(4):448–57. doi: 10.1111/j.1365-3156.2008.02021.x. [DOI] [PubMed] [Google Scholar]
- 31.Chow C, Lock K, Teo K, Subramanian SV, McKee M, Yusuf S. Environmental and social influences acting on cardiovascular risk factors and disease at a population level: a review. Int J Epidemiol. 2009;38(6):1580–94. doi: 10.1093/ije/dyn258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guindon GE, Tobin S, Yach D. Trends and affordability of cigarette prices: ample room for tax increases and related health gains. Tob Control. 2002;11:35–43. doi: 10.1136/tc.11.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]