Abstract
Climate change will likely exacerbate already existing urban social inequities and health risks, thereby exacerbating existing urban health inequities. Cities in low- and middle-income countries are particularly vulnerable. Urbanization is both a cause of and potential solution to global climate change. Most population growth in the foreseeable future will occur in urban areas primarily in developing countries. How this growth is managed has enormous implications for climate change given the increasing concentration and magnitude of economic production in urban localities, as well as the higher consumption practices of urbanites, especially the middle classes, compared to rural populations. There is still much to learn about the extent to which climate change affects urban health equity and what can be done effectively in different socio-political and socio-economic contexts to improve the health of urban dwelling humans and the environment. But it is clear that equity-oriented climate change adaptation means attention to the social conditions in which urban populations live—this is not just a climate change policy issue, it requires inter-sectoral action. Policies and programs in urban planning and design, workplace health and safety, and urban agriculture can help mitigate further climate change and adapt to existing climate change. If done well, these will also be good for urban health equity.
Keywords: Urban health, Health inequity, Climate change, Evidence
Introduction
Modern human society has seriously perturbed and depleted Earth’s systems that sustain life.1 Industrialized societies have become increasingly dependent on ever-increasing volumes of production and consumption. Added to population growth, this has led to increasing over-exploitation of finite natural resources and over-emission of greenhouse gases (GHGs).2,3 The combined concentration of GHGs in the atmosphere has already committed Earth’s mean surface temperature to a rise of at least 2°C by 2050, and a further total warming by 2100 to within the range of 1.8–4.0°C.4 As the temperature of the planet rises, there is, and will be, increased and more severe floods, droughts, storms, and heat waves.
Preliminary analyses suggest that associated adverse health outcomes will be greatest in low-income countries and among socially disadvantaged people living and working in urban areas, elderly people, children, and coastal populations, but the exact pathways from climate-related events to health inequities remain unclear.5–7
There has been increasing research and policy attention to the social determinants of urban health inequities,8–11 and there is a growing literature on the interface between global climate change and urbanization.12,13 There is, however, little documented specifically in relation to climate change and urban health inequities. In 2009/2010, the Global Research Network on Urban Health Equity (GRNUHE), financially supported by the Rockefeller Foundation, reviewed current knowledge about the social and environmental determinants of urban health inequities, documented effective action to improve urban health equity, and identified gaps in the evidence base, thereby setting direction for a global research agenda.14 As part of its work, GRNUHE asked how climate change combines with processes of urbanization and other social determinants of health to affect the risk of urban health inequities. This paper reports on that work. It outlines the plausible causal pathways from climate change to urban health inequities, lays out some key policy areas in which action can be taken to improve urban health inequities, and suggests a global research agenda which addresses the gaps in the evidence base concerning climate change and urban health inequities.
Plausible Causal Pathways from Climate Change to Urban Health Inequity
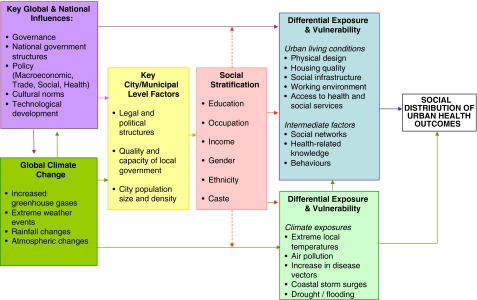
Climate change will likely exacerbate urban health inequities via direct and indirect pathways, some of which are discussed briefly below (Figure 1).
FIGURE 1.
Hypothesized pathways from global climate change through urban living conditions to urban health inequity. Source: adapted from Friel et al.5
Risks to Urban Health Equity from Extreme Weather Events and Sea Level Rise
Sea-level rise has profound implications for the 13% of the world’s urban population living in the low elevation coastal zone.15 Low-lying cities and towns near coasts will most probably face increased risks from more frequent and more intense hurricanes, cyclones, and storm surges causing flooding, direct injury, and damage to infrastructure, including roads, housing, water, and sanitation systems. Poorer urban households are usually at higher direct health risk due to less safe city locations and building sites, and the weaker resilience of infrastructure in poorer cities to withstand damage.16 Poorer urban households also often lack the economic resources to evacuate in the face of climate-related disasters or to rebuild damaged structures, and they typically lack the political influence to secure protective policies.
The experiences of severe storms and floods in Manila, as well as the 2010 earthquake in Haiti, have demonstrated the vulnerability of poor urban areas to major disasters. The flooding of New Orleans in 2005, and its effects on elderly rest home patients and poor people who could not evacuate because of lack of transport, gave a striking example of what might happen among socially disadvantaged urban communities, even in rich countries.17
Extreme Temperatures and Their Impact on Urban Health Inequities
Climate change, amplified by the heat island effect in inner city environments, is causing increased temperatures and urban health risks.18 The urban heat island effect is a result of higher average temperatures due to the lack of shade and vegetation as well as dark road and building surfaces.19 Heat wave mortality and morbidity increases have been reported in cities in the USA,20,21 Europe,22,23 and in developing countries.24–26 Heat-related health risk is socially graded—urban slum dwellers, lower socioeconomic, and minority ethnic groups are more likely to live and work in warmer neighborhoods and in buildings that are poorly ventilated and absorb heat.25 Many cities in low- and middle-income countries are built in marginal lowlands, which are particularly hot, humid, and often plagued by disease, thereby exposing people who live there to a variety of heat-related health risks.27
Densely populated urban neighborhoods with few trees have maximum temperatures during the day 1–3°C higher than cities with parks or open landscape areas.28 Poor neighborhoods with weak infrastructure, buildings, and unplanned settlement developments with little green spaces and use of black corrugated steel panels for roofs and walls are likely to be more exposed to high temperatures compared to more affluent neighborhoods and will have less capacity to adapt to the impact.25
Urbanization is both a result of the concentration of manufacturing and service enterprises in one place and a magnet for the emergence of new workplaces and workers in urban areas. Thus, the climate conditions in urban workplaces are a major concern as climate change makes many workplaces hotter during the hottest part of the year.26 Economic sectors frequently exposed to excessive heat in urban areas include construction workers, manufacturing workers with outdoor job activities or job activities in confined areas, and drivers. Many indoor factory and workshop jobs are not air-conditioned. The indoor exposure levels in the general environment of most of the tropics are already high and increasing.29
Climate Change Impacts on Infectious Diseases and the Risk to Urban Health Equity
Climate change will significantly influence, and mostly increase, the range of infectious diseases (food-borne, water-borne, and vector-borne).30,31 Poor urban living conditions, particularly those among the one billion people living in urban slums, are the breeding ground for climate-sensitive infectious diseases such as diarrhea, malaria, and dengue.31 When basic infrastructure is inadequate, existing conditions of poor sanitation and drainage and impure drinking water are further stressed under conditions of extreme weather events and flooding, leading to the transmission of infectious diseases, which puts poor urban households at higher than usual risk. Around half of the urban population of Africa and Asia lacks provision for water and sanitation to a standard that is healthy and convenient. A recent census in Dhaka, Bangladesh reveals that nearly 60% of slums lack basic drainage and are prone to flooding.32 In Latin America and the Caribbean, more than a quarter lack such provision.
Climate Change Pressures on Urban Food Security
Climate change is having uneven but generally negative impacts on agricultural production, largely through its effects on temperature and precipitation patterns. Drought-prone and long-term drying conditions in sub-tropical regions around the world, higher temperatures, and increasing frequency of flooding are already reducing agricultural yields.1 There is a significant risk that declining agricultural productivity growth, growing competition for land and water, and increasing food demands are creating a new era of increasing food prices.33,34 Low-income urban populations are among the most vulnerable to food price increases, as they generally depend on the market for their food supplies and have limited budgets.35,36 As prices rise, urban poor groups will be increasingly unable to afford a diet of the quality necessary to maintain their health.37 There may also be other health consequences if the price increases drive them deeper into poverty, as some recent research suggests,38 while riots and social instability can result from food shortages among low-income urban populations.
Climate Change and Rural–Urban Migration
Migration is expected to be a response to anthropogenic climate change, though some of those worst affected will not be able to afford to migrate far.39,40 Most of the migratory shifts are likely to be within countries or between neighboring countries. Where agricultural livelihoods are threatened by changing temperatures and precipitation patterns, there will be pressure to migrate to urban areas. The failure to accept and plan for the growth of low-income urban populations can make it difficult for poor urban groups to secure the benefits of urban living, including adequate homes with piped water and sanitation facilities. This is already an important source of urban health inequities.41 Where rural–urban migration due to climate change coincides with or encourages exclusionary policies, urban health inequities are likely to be amplified.
Action to Reduce Urban Health Inequities through Attention to Climate Change
Policy and programs that aim to address the common determinants of urban health and climate change have the potential to both reduce levels of health inequities and help avoid further climate change, and manage the existing climate change. Some of the key areas for action are outlined below.
Urban Design and the Built Environment
Effective urban management can help cities both mitigate further climate change and adapt to the impacts of existing climate change. The design of a city to be easily walkable, safe, and with adequate provision of cycle lanes and public transport corridors and hubs, in all parts of the city, will, if done well, help improve health equity42 and reduce GHG emissions through reduced use of fossil fuel transport.
Ensuring parks, green spaces, and roadside trees as part of the basic urban infrastructure will help regulate city temperature, thus helping to cope with extreme heat as a result of climate change and also act as carbon sinks. The planning and allocation of these “green” adaptation measures must be done in such a way that low-income groups have the same access to them as higher-income groups; otherwise, there will be inequities in the associated health benefits. An example of equity-focused city adaptation to heat-related health risks are the “heat emergency” policies in place in a number of North American and European cities. These emphasize monitoring low-income, elderly, and other populations who do not have air conditioning or are otherwise at risk, declaring heat emergencies as appropriate, and getting them to places where there is air conditioning (such as government and community buildings, recreational centers, churches, malls).
Planning and land-use controls are useful tools with which to prevent developers from building in zones at risk of flooding and landslides (e.g., restrictions on building within 50-year floodplains in South Africa). Guidelines and regulations, such as a decision issued in 2006 by the Thua Thien Hue provincial authorities in Vietnam to encourage cyclone-resistant building practices, can increase resilience to climatic events.43 Such regulations, however, should not penalize lower-income groups who may not have sufficient resources to follow such building practices nor be able to afford the premiums that may be attached to houses built to these specifications.
Urban households with poor sanitation and housing conditions are at increased risk of climate-related infectious diseases. Virtually all urban centers in high-income nations have high adaptive capacity; a large proportion of their populations have universal provision for safe, sufficient piped-water supplies, provision for sewers and drains that protect them from environmental hazards or health care, and emergency services to help them cope when illness occurs. Very little of this is the case in most urban centers in low- and middle-income countries. One example of a successful approach to improving sanitation is the Orangi Pilot Project in Pakistan. Residents built simple sewers, with technical and administrative support, while the government took responsibility for installing trunk lines to transport sewage for treatment. This project has had an enormous impact on the sanitary conditions in the low-income settlements, improving population health and reducing health inequities, and is now national policy in Pakistan.44 This will improve the resilience of Pakistani urban dwellers to climate-change-related infectious disease risks.
Urban Workplace
A number of actions may be taken to adapt to climate-related heat exposure in workplaces and at the same time mitigate further climate change. These include improving the design of the workplace using engineering techniques to improve ventilated indoor working areas, redesigning workplaces using special materials for walls and roofs in order to isolate the outdoor climate effect and reduce the use of air conditioning, promoting the use of clean technologies for heat reduction, and providing shaded areas for outdoor workplaces. Other activities are recommended such as increasing workers’ tolerance to heat by incorporating them gradually in heated activities; modifying working schedules to favor doing certain heat-producing tasks during the cooler times of the day; shortening shiftwork for specific physically demanding activities; and ensuring adequate recesses during the daily working hours, fluid and electrolytes replenishment for workers, and the use of personal protective clothing. However, many of the workers who are likely to be exposed to extreme temperatures are in the informal economy, often with little occupational health and safety supports or social protection generally. Key to reducing climate-related urban health inequities among these groups is to extend coverage of social protection and occupational health legislation, policy, and services to all workers.27
Climate Proofing the Urban Food Supply Systems
Adaptive responses to climate change by domestic urban food systems are vital. Urban food policies can both help to ensure the local provision of nutritious foods in climate-stressed conditions and help to create a local food supply that is environmentally sustainable.45,46 If done well, the implementation of urban agriculture—the cultivation, process, and distribution of food within the city—could prove an important response to the anticipated urban food pressure and potentially reduce urban poverty, reduce social inequity generally, help get people back to work, increase civic involvement, and improve sustainability. However, in both rich and poor countries, it is often the case that well-placed socially advantaged people benefit most from urban farming, whereas the poor, landless, and women benefit least, thereby potentially widening social and health inequities.47,48
Box 1: Urban Agriculture in Ghana
| In 1972, Ghana’s food movement “Feed Yourself Operation” encouraged city dwellers in Accra to farm in enclosed gardens around their homes and on the edges of cities. Without costing the city, the benefits of urban agriculture extended beyond greening and management of public spaces: it reduced refuse dumping and illegal-drug-related activities. In addition, there have been calls to recycle the mounting daily municipal organic waste for urban agriculture and discourage the use of artificial fertilizers by the uninformed cultivators. For Ghanaian families, urban agriculture is a significant income-diversification strategy by supplying months of staple food for the family. However, despite the socio-economic and environmental benefits, the Ghanaian policy makers and municipal government have yet to reevaluate their current urban land use planning regulations to address issues of land tenure and security to support urban agriculture.48 This oversight is typical of most cities in developing countries and speaks to the need for urban agriculture to be at the heart of all urban planning and urban health efforts. |
Urban agriculture is increasingly common in cities of high-income countries and holds promise for reducing social and health inequities and helping cites adapt to climate change. Detroit, a city of spiraling social and economic decline, has transformed many vacant land plots into community allotments. According to projected figures, urban agriculture in Detroit in the future could generate US $200 million in sales and approximately 5,000 jobs, with a US $1 investment returning approximately US $6 in fruit and vegetables.49 In Skid Row, Los Angeles, home to one of the largest homeless populations in the USA, the Urban Farming Food Chain Project installed a series of 30-ft long walls, each containing 4,000 plants to supply tomatoes, spinach, peppers, lettuce, and leeks and herbs. The program has also drawn together diverse disadvantaged members of the community of all ages and ethnicities as well as provided them an opportunity to learn new skills (http://www.urbanfarming.org/). A project of the German Association of International Gardens aims to improve racial integration in addition to producing healthy fruits and vegetables for participants.
Climate change mitigation is, indirectly, also important for urban food security. Agricultural yields are increasingly affected by climate change. Urban food security therefore is dependent on climate security and requires immediate implementation of climate change mitigation policies.
Gaps in the Evidence Base: An Action-Oriented Research Agenda
As the evidence presented above will attest, currently, we can hypothesize and describe how some aspects of climate change will affect urban health inequities and identify key areas in which policy and programs, if done well, will protect urban communities from climate change and reduce urban health inequities. However, there is still much to learn, especially with respect to tailoring these concepts and applying them in the cities of low- and middle-income countries.
Work is in its infancy, internationally, to attempt to quantify climate change’s contribution to human health patterns. In countries at all stages of economic development, there is a paucity of quantifiable evidence about the relationship between climate change and urban health inequities. There are gaps in the global evidence base in terms of understanding how different aspects of climate change contribute to urban health inequities. Research is needed that focuses on providing a better understanding of the plausible causal relationships and mechanisms by which different climate change components (temperature extremes, extreme weather, drought and flooding impacts on food, and infectious disease threats) affect health and its social distribution among urban dwellers.
Action-oriented research is needed that can help to develop and evaluate policy and actions to reduce the urban health impacts of different climate change events in different socio-political and socio-economic contexts. We need a better understanding of what can be done to mitigate and adapt to climate change such that urban health equity is improved. GRNUHE’s work identified the need to embed considerations of health equity in climate change mitigation and adaptation policies. Systematic assessment is needed that explores the urban health equity impact of climate change mitigation and adaptation strategies, both qualitative and quantitative, and that draws on health equity impact assessment research internationally. Conversely, research is needed that evaluates the effectiveness of urban policies and programs to incorporate climate change mitigation and adaptation in ways that also improve urban health and health equity.
In conclusion, there is evidence to suggest that climate change does, and will increasingly, exacerbate underlying social inequities that contribute to urban health inequities. But there is still much to be learned about the extent to which climate change affects urban health equity and what can be done in different socio-political and socio-economic contexts to improve the health of urban dwelling humans and their living and working environment. It is clear, however, that policies and programs in urban planning and design, workplace health and safety, and urban agriculture can help mitigate further climate change and adapt to existing climate change. If done well, these will also be good for urban health equity. This highlights the importance of taking direct action on urban health inequities by addressing the social determinants of urban health inequities, key aspects of which are addressed in the other papers in this series.42,50–51
Acknowledgements
This work was made possible through funding provided by the Rockefeller Foundation and undertaken as a contribution to the Global Research Network on Urban Health Equity. The views presented herein are those of the author(s) and do not necessarily reflect the decision, policy, or views of our institutions.
References
- 1.United Nations Development Programme. Human Development Report: Fighting Climate Change: Human Solidarity in a Divided World. New York, NY: United Nations Development Programme; 2007.
- 2.Satterthwaite D. The Implications of Population Growth and Urbanization for Climate Change: UNFPA and IIED. In: Guzmán JM, Martine G, McGranahan G, Schensul D, Tacoli C, editors. Population Dynamics and Climate Change. New York: UNFPA; 2009. [Google Scholar]
- 3.Climate change 2007: the Physical Science Basis—Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. New York: Cambridge University Press; 2007. [Google Scholar]
- 4.Parry M, Arnell N, Berry P, et al. Assessing the Costs of Adaptation to Climate Change: a Review of the UNFCCC and Other Recent Estimates. London, UK: International Institute for Environment and Development and Grantham Institute for Climate Change; 2009.
- 5.Friel S, Marmot M, McMichael A, Kjellstrom T, Vågerö D. Global health equity and climate stabilisation - need for a common agenda. Lancet. 2008;372(9650):1677–1683. doi: 10.1016/S0140-6736(08)61692-X. [DOI] [PubMed] [Google Scholar]
- 6.Patz J, Gibbs H, Foley J, Rogers J, Smith K. Climate change and global health: quantifying a growing ethical crisis. EcoHealth. 2007;4:397–405. doi: 10.1007/s10393-007-0141-1. [DOI] [Google Scholar]
- 7.Kjellstrom T, Holmer I, Lemke B. Workplace heat stress, health and productivity - an increasing challenge for low and middle-income countries during climate change. Global Health Action. 2009;2:46–51. doi: 10.3402/gha.v2i0.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vlahov D, Freudenberg N, Proietti F, et al. Urban as a determinant of health. J Urban Health. 2007;84(1):i16–i26. doi: 10.1007/s11524-007-9169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knowledge Network on Urban Settings. Our Cities, our Health, our Future: Acting on Social Determinants for Health Equity in Urban Settings. Final Report of the Urban Settings Knowledge Network of the Commission on Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2007.
- 10.Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2008.
- 11.Frumkin H, Frank L, Jackson R. Urban sprawl and public health: designing, planning, and building for healthy communities. Washington DC: Island Press; 2004. [Google Scholar]
- 12.Revi A. Climate change risk: an adaptation and mitigation agenda for Indian cities. Environ Urban. 2008;20(1):207–229. doi: 10.1177/0956247808089157. [DOI] [Google Scholar]
- 13.Satterthwaite D, Huq S, Pelling M, Reid H. Adapting to Climate Change in Urban Areas—The Possibilities and Constraints in Low- and Middle-Income Nations. London: International Institute for Environment and Development; 2007. [Google Scholar]
- 14.Global Research Network on Urban Health Equity (GRNUHE). Improving urban health equity through action on the social and environmental determinants of health: final report of The Rockefeller Foundation Global Research Network on Urban Health Equity. London, UK: University College London and the Rockefeller Foundation; 2010.
- 15.McGranahan G, Balk D, Anderson B. The rising tide: assessing the risks of climate change and human settlements in low elevation coastal zones. Environ Urban. 2007;19(1):17–37. doi: 10.1177/0956247807076960. [DOI] [Google Scholar]
- 16.Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change. UCL Institute for Global Health and Lancet Commission. Lancet. 2009;373:1693–1733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 17.Sharkey P. Survival and death in New Orleans: an empirical look at the human impact of Katrina. J Black Studies. 2007;37:482–501. doi: 10.1177/0021934706296188. [DOI] [Google Scholar]
- 18.Huq S, Kovats S, Reid H, Satterthwaite D. Reducing risk to cities from disasters and climate change. Environment and Urbanisation. 2007;19:3–15. doi: 10.1177/0956247807078058. [DOI] [Google Scholar]
- 19.Watkins R, Palmer J, Kolokotroni M. Increased temperature and intensification of the urban heat island: implications for the human comfort and urban design. Built Environment. 2007;33:85–96. doi: 10.2148/benv.33.1.85. [DOI] [Google Scholar]
- 20.Intergovernmental Panel on Climate Change. Climate Change 2007: Impacts, Adaptation and Vulnerability—Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. New York, NY: Cambridge University Press; 2007.
- 21.Luber G, McGeehin M. Climate Change and Extreme Heat Events. Am J Prev Med. 2008;35(5):429–435. doi: 10.1016/j.amepre.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 22.Robine J, Cheung S, Roy S, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. C. R. Biologies. 2008;331:171–178. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Hoffman B, Hertel S, Boes T. Increased cause-specific mortality associated with 2003 heat wave in Essen, Germany. J Toxicol Environ Health. 2008;71:759–765. doi: 10.1080/15287390801985539. [DOI] [PubMed] [Google Scholar]
- 24.Hajat S, Armstrong BG, Gouveia N, Wilkinson P. Mortality displacement of heat-related deaths: a comparison of Delhi, Sao Paulo, and London. Epidemiology. 2005;16(5):613–620. doi: 10.1097/01.ede.0000164559.41092.2a. [DOI] [PubMed] [Google Scholar]
- 25.Kovats S, Akhtar R. Climate, climate change and human health in Asian cities. Environ Urban. 2008;20(1):165–175. doi: 10.1177/0956247808089154. [DOI] [Google Scholar]
- 26.Kjellstrom T. Climate change, direct heat exposure, health and well-being in low and middle income countries. Global Health Action. 2009;2:1–3. doi: 10.3402/gha.v2i0.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kjellstrom T. Climate change exposures, chronic diseases and mental health in urban populations—a threat to health security, particularly for the poor and disadvantaged. Kobe, Japan: World Health Organization Kobe Centre; 2009. Technical report.
- 28.Reducing urban heat islands: compendium of strategies—trees and vegetation. Washington DC: United States Environmental Protection Agency; 2007. [Google Scholar]
- 29.Hyatt O, Lemke B, Kjellstrom T. Regional maps of occupational heat exposure: past, present and potential future. Global Health Action. 2010;3. doi:10.3402/gha.v3403i3400.5715. [DOI] [PMC free article] [PubMed]
- 30.Patz J, Olson S, Uejio C, Gibbs H. Disease emergence from global climate and land use change. Med Clin N Am. 2008; 92: 1473–1491. [DOI] [PubMed]
- 31.Campbell-Lendrum D, Corvalan C. Climate Change and developing-country cities: implications for environmental health and equity. J Urban Health. 2007;84(1):109–117. doi: 10.1007/s11524-007-9170-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bartlett S, Dodman D, Hardoy J, Satterthwaite D, Tacoli C. Social Aspects of Climate Change in Urban Areas in Low- and Middle Income Nations. http://www.dbsa.org/Vulindlela/Presentations/Session1_Dodman_old.pdf. 2009.
- 33.McCalla AF. World food prices: causes and consequences. Can J Agricultural Econ/Revue canadienne d'agroeconomie. 2009; 57(1): 23–34.
- 34.Nelson GC, Rosegrant MW, Koo J, et al. Climate Change: Impact on Agriculture and Costs of Adaptation. Washington DC: International Food Policy Research Institute; 2009.
- 35.Cohen MJ, Garrett JL. The food price crisis and urban food (in)security. Environ Urban. 2010;22(2):467–482. [Google Scholar]
- 36.Ruel MT, Garrett JL, Hawkes C, Cohen MJ. The food, fuel, and financial crises affect the urban and rural poor disproportionately: a review of the evidence. J Nutr. 2010;140(1):170S–176S. doi: 10.3945/jn.109.110791. [DOI] [PubMed] [Google Scholar]
- 37.Brinkman H, Pee S, Sanogo I, Subran L, Bloem M. High food prices and the global financial crisis have reduced access to nutritious food and worsened nutritional status and health. J Nutr. 2009;140:153S–161S. doi: 10.3945/jn.109.110767. [DOI] [PubMed] [Google Scholar]
- 38.Hertel TW, Burke MB, Lobell DB. The poverty implications of climate-induced crop yield changes by 2030. Glob Environ Chang. 2010;20(4):577–585. doi: 10.1016/j.gloenvcha.2010.07.001. [DOI] [Google Scholar]
- 39.Kniveton D, Schmidt-Verkerk K, Smith C, Black R. Climate change and migration: improving methodologies to estimate flows. Brighton: International Organization for Migration, University of Sussex; 2008. [Google Scholar]
- 40.Tacoli C. Crisis or adaptation? Migration and climate change in a context of high mobility. Environ Urban. 2009;21(2):513–525. doi: 10.1177/0956247809342182. [DOI] [Google Scholar]
- 41.McGranahan G, Jacobi P, Songsore J, Surjadi C, Kjellén M. The Citizens at Risk: From Urban Sanitation to Sustainable Cities. London, UK: Earthscan; 2001.
- 42.Smit W, Hancock T, Kumaresan J, Santos-Burgoa C, Meneses R, Friel S. Toward a research and action agenda on urban planning/design and health equity in cities in low and middle-income countries. J Urban Health. 2011; 88(5). doi:10.1007/s11524-011-9605-2. [DOI] [PMC free article] [PubMed]
- 43.UN-HABITAT. Cities & Climate Change: An Introduction. Nairobi, Kenya: UN-HABITAT; 2010.
- 44.Pervaiz A, Perween R, Hasan A. Lessons from Karachi: the Role of Demonstration, Documentation, Mapping and Relationship Building in Advocacy for Improved Urban Sanitation and Water Services. London, England: International Institute for Environment and Development; 2008. Human Settlements Working Paper 6, Water Series.
- 45.Dixon J, Omwega A, Friel S, et al. The health equity dimensions of urban food systems. J Urban Health. 2007;84(1S):118–129. doi: 10.1007/s11524-007-9176-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Friel S. Climate change, food insecurity and chronic diseases: sustainable and healthy policy opportunities for Australia. N S W Public Health Bull. 2010;21:129–133. doi: 10.1071/NB10019. [DOI] [PubMed] [Google Scholar]
- 47.Sawio C. Who are the farmers of Dar-es-Salaam? In: Egziabher A, Lee-Smith D, Maxwell D, Memon P, Mougeot L, Sawio C, eds. Cities Feeding People: An Examination of Urban Agriculture in East Africa. Ottawa, Canada: International Development Research Centre; 1994.
- 48.Obosu-Mensah K. Changes to official attitudes to urban agriculture in Accra. Afr Stud Q. 2002; 6(3): 19–32.
- 49.Mogk J. Urban Agriculture: good food, good money, good idea! Paris, France: Organisation for Economic Co-operation and Development; 2010.
- 50.Barten F, Ackerman M, Becker D, Friel S, et al. Rights, knowledge, and governance for improved health equity in urban settings. J Urban Health. 2011; 88(5). doi:10.1007/s11524-011-9608-z. [DOI] [PMC free article] [PubMed]
- 51.Salgado de Snyder V, Friel S, Fotso JC. Social conditions and urban health inequities: realities, challenges and opportunities to transform the urban landscape through research and action. J Urban Health. 2011; 88(5). doi:10.1007/s11524-011-9609-y. [DOI] [PMC free article] [PubMed]