Abstract
Objectives
To conduct a systematic review to address the following key questions: (1) what interventions have been successful in improving access for veterans with reduced health care access? (2) Have interventions that have improved health care access led to improvements in process and clinical outcomes?
Data Sources
OVID MEDLINE, CINAHL, PsychINFO.
Study Eligibility Criteria, Participants, and Interventions
English language articles published in peer-reviewed journals from 1990 to June 2010. All interventions designed to improve access to health care for US veterans that reported the impact of the intervention on perceived (e.g., satisfaction with access) or objective (e.g., travel time, wait time) access were included.
Appraisal and Synthesis Methods
Investigators abstracted data on study design, study quality, intervention, and impact of the intervention on access, process outcomes, and clinical outcomes.
Results
Nineteen articles (16 unique studies) met the inclusion criteria. While there were a small number of studies in support of any one intervention, all showed a positive impact on either perceived or objective measures of access. Implementation of Community Based Outpatient Clinics (n = 5 articles), use of Telemedicine (n = 5 articles), and Primary Care Mental Health Integration (n = 6 articles) improved access. All 16 unique studies reported process outcomes, most often satisfaction with care and utilization. Four studies reported clinical outcomes; three found no differences.
Limitations
Included studies were largely of poor to fair methodological quality.
Conclusions and Implications of Key Findings
Interventions can improve access to health care for veterans. Increased access was consistently linked to increased primary care utilization. There was a lack of data regarding the link between access and clinical outcomes; however, the limited data suggest that increased access may not improve clinical outcomes. Future research should focus on the quality and appropriateness of care and clinical outcomes.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-011-1849-8) contains supplementary material, which is available to authorized users.
KEY WORDS: health services accessibility, access, veterans, systematic review
Access to health care has been identified as a critical issue by the Department of Veterans Affairs (VA) and the larger medical community.1–4 Historically, VA has defined access as an individual's ability to obtain the health care they need within an appropriate time frame.4 Researchers within the VA have begun to develop an updated conceptualization of access that distinguishes access from downstream outcomes (e.g., utilization, quality of care, symptom levels, functioning).5 Nevertheless, it is important to examine the impact of improved access on these downstream outcomes. The VA has continued its commitment to improving access for veterans and has implemented several programs designed to improve access.6,7 As such, we sought to conduct a review of the literature that would examine the efficacy of interventions designed to improve access and the impact of such interventions on process and clinical outcomes.
The key questions addressed in this review were: (1) what interventions have been successful in improving access for veterans with reduced health care access? (2) Have interventions that have improved health care access led to improvements in downstream process and clinical outcomes? In order to answer the key questions, we examined studies of US veterans who had received any intervention designed to increase access to health care provided by the VA. All study design types were included; thus, there were no specifications for comparison groups. We examined the impact of the interventions on perceived (self-reported; e.g., satisfaction with access) and objective (observable; e.g., travel distance, wait times) access to health care, as well as process (e.g., utilization, satisfaction with care, receipt of evidence-based care) and clinical (e.g., quality of life, functioning, symptomology, mortality) outcomes.
METHODS
The key questions for this review were developed in consultation with the Planning Committee for the 2010 VA Health Services Research & Development State of the Art Conference on “Improving Access to VA Care,” the VA HSR&D Evidence Synthesis Program (ESP), and a Technical Expert Panel (TEP). The ESP review, which can be found at the VA HSR&D Evidence Synthesis Program website (www.hsrd.research.va.gov/publications/esp/), includes more articles for this key question (due to a broader definition of access outcomes) and an additional key question.
Study Selection and Abstraction
We searched MEDLINE (OVID), CINAHL, and PsycINFO for studies published from 1990 to June 2010. We limited the search to articles involving human subjects ages 18 and older published in English language. We used the following MEDLINE search terms: Health Services Accessibility, Access, Veterans, United States Department of Veteran Affairs, and Hospitals, Veterans (Appendix A, available online). Similar search terms were used in the CINAHL and PsycINFO searches. Additional references were identified by searching the reference lists and by suggestions from the TEP and other peer reviewers.
One of two investigators reviewed titles and abstracts to identify potentially eligible articles. A portion of abstracts were examined by both investigators to ensure uniformity in decisions. Inclusion criteria were as follows: (1) English language; (2) US veteran population; (3) published from 1990 to June 2010; (4) examined interventions to improve access to VA health care; (5) reported access outcomes of interest; (6) peer reviewed. In keeping with the updated conceptualization of access presented by Fortney, we defined access outcomes as both directly observable (geographical, temporal, digital, financial, and culture factors) and perceived measures of access (veteran’s self-reported satisfaction with access).5 This is a narrower definition of access outcome than we utilized in the ESP report, in which we included initiation of care (either first VA contact or initiation of specialty care) and referrals to specialty care. The downstream outcomes of interest were process outcomes (e.g., utilization, satisfaction with care, receipt of evidence-based care) and clinical (e.g., quality of life, functioning, symptomology, mortality) outcomes. Satisfaction was both an access and process outcome; satisfaction with access was categorized as an access outcome, while satisfaction with other aspects of care was a process outcome.
Investigators abstracted data on study design, patient characteristics, intervention, and impact of the intervention on access, process outcomes, and clinical outcomes. Data were abstracted by an investigator directly onto summary tables created for this review.
Quality Assessment
All studies were assessed for methodological quality. Randomized control trials (RCTs) and cohort studies were assigned a methodological rating of good, fair, or poor using the United States Preventative Services Task Force (USPSTF) criteria.8 Observational studies were rated in the domains of participant selection (e.g., appropriate recruitment of subjects/choice of database, response rate, representativeness), outcomes assessment (e.g., valid and reliable measures, no differential or overall high loss to follow-up), and analysis (e.g., potential confounders equally distributed or adjusted for in analysis). If all three criteria were rated as adequate, the study received an overall methodological rating of fair. All other observational studies were rated as poor. Observational studies were not eligible for a methodological quality rating of good.
RESULTS
Literature Flow
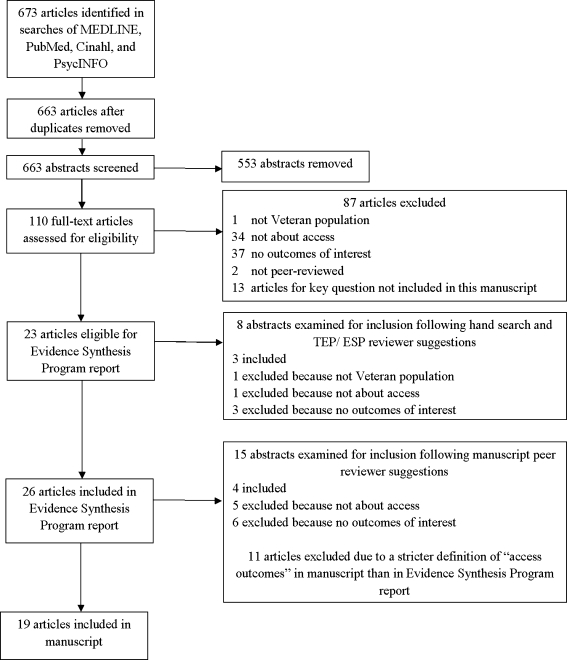
The MEDLINE search yielded 209 references, with 10 duplicates for a total of 199 unique references (Fig. 1). The CINAHL search yielded 212 additional references and the PsycINFO search yielded 252 additional references. A total of 34 articles were eligible for inclusion in the ESP report; however, 13 of those articles were for a key question not included in this manuscript. Thus, 21 articles were eligible for inclusion in the ESP report for the key question of interest. An additional seven articles were identified through hand searching reference lists and TEP member or reviewer suggestions; 28 articles (25 unique studies) were included in the ESP report for this key question. We followed a narrower definition of access outcome for the manuscript than for the ESP report, which resulted in the exclusion of 11 articles. Reviewers for this manuscript identified an additional four articles for inclusion. Thus, 19 articles (16 unique studies) were reviewed for this manuscript (Table A, available online). During abstraction, we found that the articles reported on three distinct types of interventions. The results are grouped by those interventions.
Fig. 1.
Literature flow diagram
Community-Based Outpatient Clinics (CBOCs)
In order to increase access to primary care for veterans living in rural or other underserved geographical areas, the VA opened satellite primary care clinics, known as CBOCs. We identified five articles (four studies) that examined the implementation of CBOCS.9–13 Three of the studies were rated as fair methodological quality,9–12 while 1 was rated as poor methodological quality.13
Impact on Access Four articles utilized either quasi-experimental or cohort designs to examine the impact of the opening of CBOCs on access factors (Table 1).9–12 The studies found that the opening of CBOCs resulted in a decrease in travel distance to the closest VA facility for those in CBOC catchment areas. However, CBOCs did not have a significant impact on a number of reported access outcomes (e.g., days between discharge and outpatient follow-up).9 One study examined veterans' satisfaction with access at CBOCs; veterans using CBOCs reported better access/timeliness.13 The same study found that veterans using CBOCS were more likely to report waits of less than 20 min than veterans getting care at VA Medical Centers (VAMCs).13
Table 1.
Studies Examining the Efficacy of Interventions Designed to Increase Access for Veterans
| Author, date | Study design | Intervention/comparator | Main outcomes | Study quality |
|---|---|---|---|---|
| Community-based outpatient clinics (CBOCS) | ||||
| Borowsky et al. 200212 | Cross-sectional survey | Utilization of CBOCS/VAMC users | Better self-reported access/timeliness | Fair |
| Fortney et al. 20029 | Retrospective cohort analysis | Utilization of CBOCS/VAMC users | Veterans in CBOC catchment areas had a decrease in travel distance to closest facility. CBOC patients more likely to be new VA users, have more primary care encounters, and fewer specialty care encounters | Fair |
| Fortney et al. 2005a10; 2005b11 | Quasi- experimental | Implementation of CBOCs/a matched group of veterans residing outside the catchment area of any new CBOCs | Decrease in travel distance to the closest VA facility, more primary care visits, ancillary visits, and extended care physical health visits | Fair |
| Morgester et al. 200213 | Case series | Utilization of CBOCS/utilization of VAMC or non-VA care | All three groups reported few problems finding clinic and found the hours of operation convenient. | Poor |
| Primary care mental health integration | ||||
| Blue-Howells et al. 200818; McGuire et al. 200919 | Quasi- experimental | Implementation of integrated mental health, primary care, and homeless social services clinic/ pre-implementation | Shorter wait time for initial primary care visit. Improved preventative care, more primary care visits, lower emergency care service use. No significant differences in clinical outcomes | Poor |
| Druss et al. 200116 | RCT | Integrated primary care services into mental health clinic/usual care | Better self-reported access, more primary care visits, fewer ER visits, improved preventative care, higher satisfaction with care, higher (better) scores on the SF-36 physical component summary | Fair |
| Saxon et al. 200617 | RCT | Implemented an onsite (within the substance use clinic) primary care clinic/usual care | Shorter wait for initial primary care visit; greater odds of attending rescheduled initial visit; more likely to attend at least 1 primary care visit. More likely to remain engaged in substance use treatment at 60 days. No significant differences in clinical outcomes | Good |
| Shiner et al. 200914 | Cohort study | Varying models of Primary Care Mental Health (PCMH)/no PCMH integration | Models in which PCMH integration occurred onsite had increase of veterans seen within 30 days and percentage receiving optimal care | Poor |
| Watts et al. 200715 | Cohort study | PCMH Integration/no PCMH integration | More veterans received mental health services in primary care, were seen in mental health; shorter wait time for initial mental health appointment | Fair |
| Telemedicine | ||||
| Agha et al. 200920 | RCT | Consultations were conducted via videoconferencing from remote sites/in-person consultation | Veterans in the telemedicine condition were significantly more satisfied with convenience of their care. Perceived physician communication was not inferior in telemedicine as compared to in-person consultations | Fair |
| Wakefield et al. 200423 | Cross-sectional survey | Implemented interactive video conferencing to provide specialty consultation/no comparison | 92% of veterans reported that using telemedicine made it easier to see the specialist. 81% reported satisfaction with the telemedicine consultation process | Poor |
| Whited et al. 200222; 200421 | RCT | Implemented teledermatology program in which provider saw a still digital image of the lesion, a standardized history, and the standard consultation/usual care (in-person consultation). | Veterans in the teledermatology condition initiated treatment in a significantly shorter amount of time; 18.5% in the teledermatology condition did not require an in-person dermatology clinic visit. Veterans were satisfied with care in both methods of consultation | Fair |
| Wilkins et al. 200724 | Pilot case series | Implemented telemedicine to seek consultations from a remote wound care team/no comparison | Veterans reported that telemedicine was more convenient than travelling to wound care team. Almost all (92.8%) participants were satisfied with telemedicine care | Poor |
| Other | ||||
| Rodriguez et al. 200727 | Qualitative study following implementation | Implemented a mobile care program, which had health care staff and resources to conduct basic medical care within the van | Accessibility of care was mentioned 26 times in 18 interviews (2nd most common topic behind quality of care). Quality of care was mentioned 28 times in 18 interviews | Poor |
| Weinberger et al. 199625 | RCT | Implemented intensive primary care program designed to increase access to primary care/usual care | Median time from hospital discharge to primary care shorter. More likely to have one or more general medical clinic visit; higher monthly hospital readmission rate; more days of hospital readmission | Good |
| Wray et al. 199926 | Cohort study | Implemented mobile primary care clinics for veterans located more than 100 miles from a VAMC | 56% of veterans using the mobile clinic were new VA users. Veterans experienced a decrease in travel distance: 80% of the mobile clinic users lived at least 100 miles from the VAMC, 94% lived within 50 miles of the mobile clinic. Utilization of veterans within 30 miles of the mobile clinic increased by 40% while the mobile clinics were operational | Poor |
Impact on Downstream Outcomes CBOCs attracted more new VA users than the parent VAMCs and led to higher rates of primary care utilization in counties with a CBOC.9–11 Findings regarding the utilization of specialty care were mixed, although in counties with CBOCs that offered specialty mental health services, more veterans accessed mental health services.9–11 The impact on some process outcomes was small and may not be clinically significant. For example, Fortney et al. reported that those in the CBOC catchment area only had 0.5 more primary care visits in the 18 months post-implementation than pre-implementation.10 Veterans using CBOCs reported fewer problems in a variety of areas (e.g., preferences, care coordination, education), greater satisfaction with care, and were more likely to have an overall reported rating of good or excellent visits than veterans getting care at VAMCs.12,13 No clinical outcomes were reported.
Primary Care Mental Health Integration
Five articles (four unique studies) examined the impact of primary care mental health (PCMH) integration on veterans' access to health care services.14–19 One study was rated as good,17 two as fair,15,16 and two as of low methodological quality.14,18,19
Impact on Access Watts et al. examined a primary care clinic before and after PCMH integration at a VAMC and associated CBOCs.15 After PCMH integration wait times for appointments in the mental health clinic decreased substantially. None of these differences were significant at the CBOCs.15 Shiner et al. reported on the effect of implementing four different models of PCMH integration at one VAMC and four CBOCs.14 The clinics in which integration included onsite mental health care with advance or open access experienced increases in the number of veterans receiving mental health care within both 4 and 30 days.14Druss et al. conducted a RCT to examine the efficacy of integrating primary care into a mental health clinic.16 Veterans randomized to the PCMH integrated clinic reported significantly better satisfaction with access. Saxon et al. conducted a similar study in which veterans receiving care in a substance use clinic were randomized to receive primary care from a clinic located within the substance use clinic or through a medical clinic (treatment as usual).17 The integrated clinic fared better on measures of access, including length of wait for initial primary care visit.17 Finally, one study reported on the effort to integrate primary care, mental health, and social services for homeless veterans.18,19 The intervention resulted in shorter wait times for an initial primary care appointment; the integration group had on average less than a day lapse, while the usual care group waited approximately 2 months for their initial visit.18,19
Impact on Downstream Outcomes In regard to process outcomes, Watts et al. found that more veterans at the VAMC received "optimal depression treatment" following integration.15 Similarly, Shiner et al. found that more veterans at the VAMC received care for depression, fewer veterans received no depression treatment, more veterans received care in mental health clinics, and more veterans received optimal care.14 When implementing primary care into mental health clinics, Druss et al. found that veterans in the PCMH condition had more primary care visits, fewer ER visits, received more preventative services, and reported greater satisfaction with care across a number of domains.16 Saxon et al. reported that those assigned to the PCMH integrated condition were more likely to attend return primary care visits and had more primary care visits during the study period, were less likely to seek non-VA care, and were more likely to remain engaged in substance use treatment at 60 days (although not at 6 or 12 months).17 When primary care, mental health, and homeless services were integrated, the PCMH group received more preventative services, had a higher number of primary care visits, and had lower levels of ER use.19,20 There were no differences on rates of admission, inpatient days, or the number of veterans receiving primary care.19,20Three of the studies examined clinical outcomes. Druss et al. reported that veterans assigned to PCMH integration had better physical component SF-36 scores at 1-year post randomization; however, there was no difference on the mental component score.16 The other two studies that report clinical outcomes found no differences between intervention and control clinics.17–19
Telemedicine
Impact on Access Five articles (four studies) examined the use of telemedicine.20–24 Two studies were of fair quality20–22 and two were of poor quality.23,24 All four telemedicine studies examined the utility of telemedicine in receiving consultations from specialty providers. Agha et al. conducted a RCT in which veterans in need of consultation were randomly assigned to receive consultation in person at the hub VAMC or via telemedicine from a remote site.20 Veterans who received their consultation via telemedicine reported that their care was significantly more convenient than those who attended in-person appointments. Similarly, Wakefield et al. examined the use of telehealth to receive a variety of consultations from specialists at a VAMC for veterans in a long-term care facility, while Wilkins et al. evaluated the feasibility of using telehealth to receive consultations from a multidisciplinary wound care team for veterans at a VAMC without such a team.23,24 Both Wakefield and Wilkins found that the veterans reported that telemedicine was easier and more convenient than traveling to meet with a specialist.23,24Whited et al. conducted a RCT in which in-person consultations were compared to teledermatology for veterans being referred for dermatology consultation.21,22 In the teledermatology condition, providers electronically viewed a still digital image of the lesion, a standardized history, and the standard consultation. Dermatologists could then decide to see the veteran in person, or send a diagnosis and treatment plan back to the referring provider without seeing the veteran. Veterans assigned to teledermatology initiated treatment significantly more quickly (73.8 vs 114.3 days).22
Impact on Downstream Outcomes All four studies examined process outcomes. Agha et al. found that veterans’ perceptions of physician communication (patient-centeredness, clinical competence, interpersonal skills) were not inferior to physician communication during in-person consultations, suggesting that veterans’ found interactions conducted via telemedicine as satisfying as in-person interactions.20 Whited et al. found that 18.5% of veterans in the teledermatology condition did not require a follow-up in-person consultation.22 Whited et al., Wilkens et al., and Wakefield et al. all found that a large majority of veterans were satisfied with telemedicine care; in support of its use, Whited et al. did not find a difference in satisfaction with care between telemedicine and in-person consultation.21–24 No clinical outcomes were assessed.
Other Access Interventions
Three studies examined the effect of a distinct intervention on access: one RCT of good methodological quality25 and two studies (one qualitative, one cohort study) of poor quality.26,27
Weinberger et al. conducted a RCT in which hospitalized veterans with chronic health conditions, who did not have ongoing primary care, were assigned to either treatment as usual or an intensive primary care program.25 The intensive case management program had a number of goals, including increasing access to primary care following hospitalization. The intervention included both inpatient (doctor and nurse visits, discharge planning, plan for primary care appointment) and outpatient (reminder and check in calls) components. For those in the intensive care condition, the median time from hospital discharge to primary care was shorter and self-reported satisfaction with access was higher.25 The two groups differed on process outcomes, with intervention veterans being more satisfied with care, more likely to visit a general medicine clinic, and less likely to visit specialty care.25 Those in the intervention condition were more likely to be readmitted to the hospital, readmitted sooner, and have more days of rehospitalization.25 There were no differences on clinical outcomes.
Rodriguez et al. conducted a qualitative study to examine elderly African American veterans' reaction to a mobile geriatric care unit (MGU).27 The MGU was a vehicle with a patient education room and examination room equipped to perform standard preventative care. The qualitative analyses revealed that veterans commented on the accessibility of care 26 times in 18 interviews.27 The access-related comments were positive and related to geographic proximity, hours of operation, and wait time.27 In regard to process outcomes, veterans mentioned quality of care 28 times.27 Comments focused on the helpfulness and friendliness of staff and the accommodations.27 No clinical outcomes were assessed.
Finally, Wray et al. examined the impact of six mobile primary care clinics for veterans who lived over 100 miles from the nearest VAMC.26 The vast majority of veterans experienced a decrease in travel distance; 94% of veterans lived with 50 miles of a mobile clinic, while 80% lived at least 100 miles from the closest VAMC.26 In regard to process outcomes, the mobile clinics drew new users (56% of veterans were new users), and for those within 30 miles of the mobile clinics, utilization increased by 40%.26 No clinical outcomes were assessed.
DISCUSSION
The results suggest that access to health care can be improved through structural/organizational interventions. All of the articles reported an association between the intervention and at least one measure of access (either perceived or objective). The evidence was strongest for the implementation of PCMH, which consistently resulted in shorter wait times for both primary care and mental health appointments.14,15,17–19 A finding of particular interest in the PCMH literature was that integration at varying levels (e.g., colocation versus walk in access 1 day per week) resulted in improved access, suggesting that a range of models may yield positive effects.14 The opening of CBOCs and the use telemedicine each had four studies showing that they resulted in improved access for veterans. As would be expected, the opening of CBOCs led to decreased travel time/distance for veterans in CBOC catchment areas.9–11 Researchers examining the use of telemedicine were primarily interested in veterans’ perceived access; they consistently found that veterans reported that specialists were easier to access using telemedicine than traditional in-person meetings.
It is important to note that for many access interventions, it would be impossible for the target access outcome not be impacted. For example, building a VA clinic in a rural area will always decrease the travel distance to the nearest VA clinic for those in that rural community. We required that studies report on the impact of the intervention on either perceived or objective access because we thought that while an access intervention may have a positive impact on the target access outcome, it could negatively impact other aspects of access. For example, while using telemedicine may have a positive impact on geographic access barriers, it could create digital (e.g., connectivity or usability) or cultural (e.g., perceived lack of understanding) barriers. However, few studies included in the review reported on more than the target access outcome. We suggest that future studies include measures on a variety of perceived and objective measures of access. This will provide a more thorough understanding of access barriers and will help researchers identify new barriers that may arise as access interventions are implemented.
All of the 16 unique studies reported process outcomes. The most frequently reported process outcomes were satisfaction with care and utilization. The implementation of CBOCs led to increases in the initiation of care and primary care visits.9–11 PCMH integration also led to an increase in primary care visits and increases in preventative care.16–19 Across the interventions, findings regarding the use of specialty care and hospitalization were mixed.9–11,16,18,19,25 Across interventions, increases in access were associated with satisfaction with care.12,16 The telemedicine studies consistently found that veterans are as satisfied with their care and communication with providers when appointments are delivered via telemedicine as when they are delivered in person.20–22 These findings are important given the accumulating data showing that in-person and telemedicine interventions yield equivalent outcomes for high-priority conditions, such as posttraumatic stress disorder.28
Finally, only 4 of the 16 unique studies reported clinical outcomes.16–19,25 Three found no difference between intervention and control conditions. The RCT by Druss and colleagues was the only study to show that improvements in access led to improvements in clinical outcomes, specifically greater improvements in physical component scores on the SF-36.16 Veterans had a nearly five point increase on their physical component score in the year following integration, while those in the usual care condition had a 0.3 point decrease over the same time period.16 Research on clinical outcomes must be a priority in the future. Such work will be challenging because there are a number of variables that might impact both access and outcomes (e.g., comorbidities). Rigorous, highly controlled research, such as that conducted by Druss et al., will be needed to clarify whether increased access results in improved health for veterans.
In addition to measuring clinical outcomes, we recommend that future research examine process outcomes beyond service utilization. The data regarding utilization are difficult to interpret as it is unclear whether increased utilization led to improved patient outcomes. In one study that did link access and outcomes, increased access to primary care resulted in increased rates and length of hospitalization.25 While the increase in hospitalization was not necessarily a negative outcome, the study highlights the complicated association between utilization and patient health. Thus, we recommend a decreased focus on utilization as an outcome and suggest that if utilization is included as an outcome, it is either specific to the type of care received (e.g., receipt of evidence-based care) or linked to clinical outcomes.
There were important limitations to this study. First, the studies included in this review were primarily of poor to fair methodological quality. Further, we identified a number of well-designed studies that examined access interventions, but they were not included in our review because they did not include data regarding either actual or perceived access outcomes.29–40 Therefore, there are studies that report on the impact of access interventions on downstream outcomes that are not included in this review. As discussed above, we suggest that future research examining access interventions collect and compare a broad range of perceived and actual access outcomes across groups. In conclusion, interventions can improve access to health care for veterans. Increased access was consistently linked to increased primary care utilization and satisfaction with care; however, there was a lack of data regarding the link between access and clinical outcomes. Future research should focus on the quality and appropriateness of care and clinical outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOC 62 kb)
Acknowledgements
This report is based on research conducted by the Evidence-based Synthesis Program (ESP) Center located at the Minneapolis VA Health Care System, Minneapolis, MN, funded by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development. The findings and conclusions in this document are those of the author(s) who are responsible for its contents; the findings and conclusions do not necessarily represent the views of the Department of Veterans Affairs or the United States government. Therefore, no statement in this article should be construed as an official position of the Department of Veterans Affairs. This material is the result of work supported with resources and the use of facilities at the Minneapolis VA Medical Center, Minneapolis, MN. Dr. Kehle is supported by a VA Health Services Research & Development Career Development Award.
Conflict of Interest None disclosed.
References
- 1.Agency for Healthcare Research and Quality. 2007 National Healthcare Disparities Report. Rockville, MD: US Department of Health and Human Services, Agency for Healthcare Research and Quality, AHRQ Pub. No. 08–0041, February 2008.
- 2.Demakis JG. “Rural Health-Improving Access to Improve Outcomes.” Management Brief, Health Services Research & Development Service, No. 13:1–3, Jan 2000.
- 3.Millman M, editor. Access to healthcare in America. Washington, DC: National Academy Press; 1993. [Google Scholar]
- 4.Miller LJ. “Improving Access to Care in the VA Health System: A progress report.” FORUM, VA Health Services Research & Development Service, June 2001.
- 5.Fortney J. “A Re-conceptualization of Access for 21stCentury Healthcare.” Oral presentation given to the VA Health Services Research & Development Service Timely Topics of Interest Cyber Seminar Series, August 2010.
- 6.Mayo-Smith MF. “Access Issues Within VA Offer Challenges Research Opportunities.” FORUM, VA Health Services Research & Development Service, July 2008.
- 7.Weeks WB. “Access to Care: A VA Research Agenda.” FORUM, VA Health Services Research & Development Service. July 2008.
- 8.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, Atkins D. Current methods of the US Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3S):21–35. doi: 10.1016/S0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 9.Fortney JC, Borowsky SJ, et al. VA community-based outpatient clinics: access and utilization performance measures. Med Care. 2002;40:561–9. doi: 10.1097/00005650-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Fortney JC, Maciejewski ML, et al. Does improving geographic access to VA primary care services impact patients' patterns of utilization and costs? Inquiry. 2005;42:29–42. doi: 10.5034/inquiryjrnl_42.1.29. [DOI] [PubMed] [Google Scholar]
- 11.Fortney JC, Steffick DE, et al. Are primary care services a substitute or complement for specialty and inpatient services? Health Serv Res. 2005;40:1422–42. doi: 10.1111/j.1475-6773.2005.00424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borowsky SJ, Nelson DB, et al. VA community-based outpatient clinics: performance measures based on patient perceptions of care. Med Care. 2002;40:578–86. doi: 10.1097/00005650-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Morgester WA, Biggs CJ. Community-based VHA clinics: effect on patient satisfaction and resource utilization. J Healthc Qual. 2002;24:34–8. doi: 10.1111/j.1945-1474.2002.tb01014.x. [DOI] [PubMed] [Google Scholar]
- 14.Shiner B, Watts BV, et al. Access to what? An evaluation of the key ingredients to effective advanced mental health access at a VA medical center and its affiliated community-based outreach clinics. Mil Med. 2009;174:1024–32. doi: 10.7205/milmed-d-03-6608. [DOI] [PubMed] [Google Scholar]
- 15.Watts BV, Shiner B, et al. Outcomes of a quality improvement project integrating mental health into primary care. Qual Saf Healthcare. 2007;16:378–81. doi: 10.1136/qshc.2007.022418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Druss BG, Rohrbaugh RM, et al. Integrated medical care for patients with serious psychiatric illness. Arch Gen Psychiat. 2001;58:861–8. doi: 10.1001/archpsyc.58.9.861. [DOI] [PubMed] [Google Scholar]
- 17.Saxon AJ, Malte CA, et al. Randomized trial of onsite versus referral primary medical care for veterans in addictions treatment. Med Care. 2006;44:334–42. doi: 10.1097/01.mlr.0000204052.95507.5c. [DOI] [PubMed] [Google Scholar]
- 18.Blue-Howells J, McGuire J, et al. Co-location of healthcare services for homeless veterans: a case study of innovation in program implementation. Soc Work Healthcare. 2008;47:219–231. doi: 10.1080/00981380801985341. [DOI] [PubMed] [Google Scholar]
- 19.McGuire J, Gelberg L, et al. Access to primary care for homeless veterans with serious mental illness or substance abuse: a follow-up evaluation of co-located primary care and homeless social services. Admin Policy Ment Health. 2009;36:255–64. doi: 10.1007/s10488-009-0210-6. [DOI] [PubMed] [Google Scholar]
- 20.Agha Z, Schapira RM, Laud PW, McNutt G, Roter DL. Patient satisfaction with physician-patient communication during telemedicine. Telemed J E Health. 2009;15:830–9. doi: 10.1089/tmj.2009.0030. [DOI] [PubMed] [Google Scholar]
- 21.Whited JD, Hall RP, Foy ME, Marbrey LE, Grambow SC, Dudley TK, Datta SK, Simel DL, Oddone EZ. Patient and clinician satisfaction with a store-and-forward teledermatology consult system. Telemed J E Health. 2004;10:422–31. doi: 10.1089/tmj.2004.10.422. [DOI] [PubMed] [Google Scholar]
- 22.Whited JD, Hall RP, Foy ME, Marbrey LE, Grambow SC, Dudley TK, Datta S, Simel DL, Oddone EZ. Teledermatology’s impact on time to intervention among referrals to a dermatology consult service. Telemed J E Health. 2002;8(3):313–21. doi: 10.1089/15305620260353207. [DOI] [PubMed] [Google Scholar]
- 23.Wakefield BJ, Buresh KA, et al. Interactive video specialty consultations in long-term care. J Am Geriatr Soc. 2004;52:789–93. doi: 10.1111/j.1532-5415.2004.52220.x. [DOI] [PubMed] [Google Scholar]
- 24.Wilkins E, et al. Feasibility of virtual wound care. Adv Skin Wound Care. 2007;20:275–8. doi: 10.1097/01.ASW.0000269315.30639.82. [DOI] [PubMed] [Google Scholar]
- 25.Weinberger M, Oddone EZ, et al. Does increased access to primary care reduce hospital readmissions? Veterans Affairs Cooperative Study Group on Primary Care and Hospital Readmission. New Engl J Med. 1986;334:1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 26.Wray NP, Weiss TW, Menke TJ, Gregor PJ, Ashton CM, Christian CE, Hollingsworth JC. Evaluation of the VA mobile clinics demonstration project. J Healthc Manag. 1999;44:133–47. [PubMed] [Google Scholar]
- 27.Rodriguez KL, Appelt CJ, et al. African American veterans’ experiences with mobile geriatric care. J Healthcare Poor Underserved. 2007;18:44–53. doi: 10.1353/hpu.2007.0016. [DOI] [PubMed] [Google Scholar]
- 28.Frueh BC, Monnier J, Yim E, Grubaugh AL, Hamner MB, Knapp RG. A randomized trial of telepsychiatry for post-traumatic stress disorder. J Telemed Telecare. 2007;13:142–7. doi: 10.1258/135763307780677604. [DOI] [PubMed] [Google Scholar]
- 29.Bauer MS, McBride L, et al. Impact of an easy-access VA clinic-based program for patients with bipolar disorder. Psychiatr Serv. 1997;48:491–6. doi: 10.1176/ps.48.4.491. [DOI] [PubMed] [Google Scholar]
- 30.Bauer MS, McBride L, et al. Collaborative care for bipolar disorder: part II. Impact on clinical outcome, function, and costs. Psychiatr Serv. 2006;57:937–45. doi: 10.1176/appi.ps.57.7.937. [DOI] [PubMed] [Google Scholar]
- 31.Boutelle KN, Dubbert P, et al. A pilot study evaluating a minimal contact telephone and mail weight management intervention for primary care patients. Eat Weight Disord. 2005;10:e1–5. doi: 10.1007/BF03354659. [DOI] [PubMed] [Google Scholar]
- 32.Chumbler NR, Chuang HC, Wu SS, Wang X, Kobb R, Haggstrom D, Jia H. Mortality risk for diabetes patients in a care coordination, home-telehealth programme. J Telemed Telecare. 2009;15:98–101. doi: 10.1258/jtt.2008.080803. [DOI] [PubMed] [Google Scholar]
- 33.Wakefield BJ, Ward MM, Holman JE, Ray A, Scherubel M, Burns TL, Kienzle MG, Rosenthal GE. Evaluation of home telehealth following hospitalization for heart failure: a randomized trial. Telemed J E Health. 2008;14:753–61. doi: 10.1089/tmj.2007.0131. [DOI] [PubMed] [Google Scholar]
- 34.Ruskin PE, Silver-Aylaian M, Kling MA, Reed SA, Bradham DD, Hebel JR, Barrett D, Knowles F, 3rd, Hauser P. Treatment outcomes in depression: comparison of remote treatment through telepsychiatry to in-person treatment. Am J Psychiat. 2004;161:1471–6. doi: 10.1176/appi.ajp.161.8.1471. [DOI] [PubMed] [Google Scholar]
- 35.Dobscha SK, Corson K, Perrin NA, Hanson GC, Leibowitz RQ, Doak MN, Dickinson KC, Sullivan MD, Gerrity MS. Collaborative care for chronic pain in primary care: a cluster randomized trial. JAMA. 2009;301:1242–52. doi: 10.1001/jama.2009.377. [DOI] [PubMed] [Google Scholar]
- 36.Dobscha SK, Corson K, Hickam DH, Perrin NA, Kraemer DF, Gerrity MS. Depression decision support in primary care: a cluster randomized trial. Ann Intern Med. 2006;145:477–87. doi: 10.7326/0003-4819-145-7-200610030-00005. [DOI] [PubMed] [Google Scholar]
- 37.Hedrick SC, Chaney EF, Felker B, Liu CF, Hasenberg N, Heagerty P, Buchanan J, Bagala R, Greenberg D, Paden G, Fihn SD, Katon WJ. Effectiveness of collaborative care depression treatment in Veterans' Affairs primary care. Gen Intern Med. 2003;18:9–16. doi: 10.1046/j.1525-1497.2003.11109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oslin DW, Sayers S, Ross J, Kane V, Ten Have T, Conigliaro J, Cornelius J. Disease management for depression and at-risk drinking via telephone in an older population of veterans. Psychosom Med. 2003;65:931–7. doi: 10.1097/01.PSY.0000097335.35776.FB. [DOI] [PubMed] [Google Scholar]
- 39.Felker BL, Barnes RF, Greenberg DM, Chaney EF, Shores MM, Gillespie-Gateley L, Buike MK, Morton CE. Preliminary outcomes from an integrated mental health primary care team. Psychiatr Serv. 2004;55:442–4. doi: 10.1176/appi.ps.55.4.442. [DOI] [PubMed] [Google Scholar]
- 40.Ross JT, TenHave T, Eakin AC, Difilippo S, Oslin DW. A randomized controlled trial of a close monitoring program for minor depression and distress. J Gen Intern Med. 2008 Sep;23:1379–85. Epub 2008 May 23. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
(DOC 62 kb)