ABSTRACT
National health reform is expected to increase how long individuals have to wait between requests for appointments and when their appointment is scheduled. The increase in demand for care due to more widespread insurance will result in longer waits if there is not also a concomitant increase in supply of healthcare services. Long waits for healthcare are hypothesized to compromise health because less frequent outpatient visits result in delays in diagnosis and treatment. Research testing this hypothesis is scarce due to a paucity of data on how long individuals wait for healthcare in the United States. The main exception is the Veterans Health Administration (VA) that has been routinely collecting data on how long veterans wait for outpatient care for over a decade. This narrative review summarizes the results of studies using VA wait time data to answer two main questions: 1) How much do longer wait times decrease healthcare utilization and 2) Do longer wait times cause poorer health outcomes? Longer VA wait times lead to small, yet statistically significant decreases in utilization and are related to poorer health in elderly and vulnerable veteran populations. Both long-term outcomes (e.g. mortality, preventable hospitalizations) and intermediate outcomes such as hemoglobin A1C levels are worse for veterans who seek care at facilities with longer waits compared to veterans who visit facilities with shorter waits. Further research is needed on the mechanisms connecting longer wait times and poorer outcomes including identifying patient sub-populations whose risks are most sensitive to delayed access to care. If wait times increase for the general patient population with the implementation of national reform as expected, U.S. healthcare policymakers and clinicians will need to consider policies and interventions that minimize potential harms for all patients.
KEY WORDS: wait times, health outcomes, chronic conditions, health care utilization, VA
INTRODUCTION
The Institute of Medicine identified ensuring timely access to health care as one of six essential ways to improve the quality of health care.1 In another article included in this supplemental issue, Fortney et al. emphasize that appointment wait times may be a potentially important determinant of temporal access to services.2 The number of days between a patient’s request for an appointment and the actual appointment (e.g. wait time) is likely to lengthen with the recent passage of health reform that expands the number of people with insurance coverage. If there is not a proportionate expansion of supply in healthcare services to respond to this increase in demand, waits will increase for the general patient population.3,4 The experience of wait times in Massachusetts highlights this phenomenon. Massachusetts passed a universal health insurance law in 2006 that served as a model for the national health reform law scheduled to take effect in 2014. In the aftermath of health reform in Massachusetts, waiting times for primary care grew to as much as 100 days.5
Long waits for healthcare decrease patient satisfaction. Survey data consistently indicates that patients facing longer waits have greater dissatisfaction with their care.6 Patients often do not feel competent to judge the technical quality of healthcare they receive so their satisfaction is based on aspects they can judge, such as timeliness of services.6–8
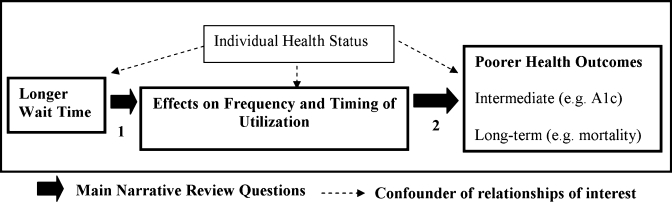
Beyond patient frustration, it is assumed that long delays for health care compromise health due to foregone or delayed utilization that defers appropriate diagnosis and treatment (see the graphical representation of this conceptual model in Fig. 1).1,8 For example, patients with diabetes who have toe ulcers will benefit from faster medical attention in order to prevent the more serious outcome of gangrene or lower-extremity amputations.9,10 Research testing the effect of wait times on health care utilization and health outcomes is sparse due to a paucity of data on wait times for health care in the United States.11 The main exception is the Veterans Health Administration (VA) in the U.S. Department of Veterans Affairs that provides free or low-cost health care to the nation’s veterans. Demand for VA care often exceeds supply, so balance is achieved through waiting times. Consequently, the few studies examining the effect of wait times on health care utilization and health outcomes have capitalized on VA data.12–15
Figure 1.
Conceptual model of the effect of wait times on health care utilization and health outcomes.
This narrative review summarizes the results of these studies to answer two main questions (see Fig. 1): 1) How much do longer wait times decrease health care utilization? and 2) Do longer wait times cause poorer health outcomes? In what follows, the next section provides background on VA wait time measures and highlights the need for a wait time measure that is independent of individual health status. The following section summarizes findings from studies examining the effect of wait times on health care utilization and health outcomes and the final section considers questions for future research and policy implications.
DATA AND METHODS ISSUES
History of VA Wait Time Measures
Before 1999, there was only anecdotal evidence on how long veterans were waiting for outpatient care because the VA scheduling system was not set up to collect this information.16 In response to complaints from veterans’ organizations and acknowledgement from VA officials that waits were likely too long, Congress requested information on VA outpatient waiting times.16,17 Consequently, VA operations staff began systematically collecting that data. Individual-level wait times are averaged together for each appointment type (e.g. primary care) in a VA facility.18–21
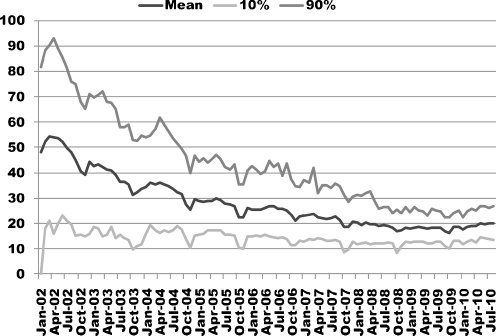
Since the VA began monitoring wait times, significant progress in decreasing waits has been made nationwide. For example, the average number of days new primary care patients had to wait has decreased from about 50 days in 2002 to 20 days in 2010 and the variation between VA facilities in how long individuals are waiting has substantially decreased (Fig. 2). Nonetheless, VA facilities continue to struggle with long waits from time to time. In 2010, 10% of VA facilities had waits of more than 25 days for new primary care patients.
Figure 2.
National wait times for new VA patients in primary care (2002–2010)* (*2002 was early in the collection of wait time data, which accounts for inconsistent reporting from some facilities on wait times in early 2002).
Effect of Individual Health Status
The main methodological concern in studies examining the causal effect of wait times on utilization and health outcomes is the need for a wait time measure that is not influenced by individual health status. It is tempting to examine the effect of wait times experienced by each individual on their own health outcomes. Medical triage makes this impossible. Providers identify those who have the most urgent needs when calling to request an appointment and schedule these patients with appointments first.18–22 Consequently, both observed (e.g. diagnosed comorbidities) and unobserved (e.g. natural rate of deterioration in health23) individual health status is likely to affect the services an individual uses, which in turn affect individual wait times as well as outcomes (see Fig. 1). Although statistical controls for observable differences in health status will reduce the severity of this problem, health status cannot be measured precisely enough to eliminate it. The simultaneous determination of unobserved individual health status, wait times and health outcomes confounds any attempt to study the effect of individual wait times on outcomes.12–15
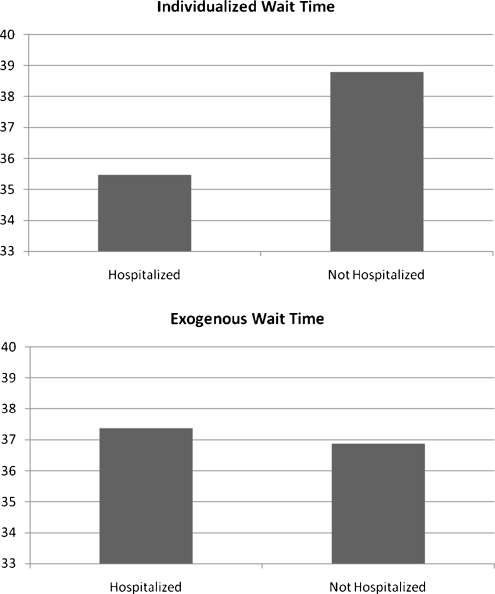
The top panel of Figure 3 abstracted from Prentice & Pizer13 illustrates this problem. It shows the mean wait time that was calculated for August 2001 based on the appointment types an individual actually used, tabulated by whether or not the individual experienced an ambulatory care sensitive condition (ACSC) hospitalization in August 2001. ACSC hospitalizations are hospitalizations that can be prevented with timely, high-quality outpatient care.24,25 Note this is still not the actual time individual patients waited for appointments. These facility level wait times were averaged together for all clinic appointments used by each individual.
Figure 3.
Individualized wait time versus exogenous^ wait time by ACSC Hospitalization Status in August 2001† (^exogenous = wait time not affected by individual health status). ±Individualized wait times reflect individual health status. Sicker patients are likely to be seen faster which creates an association between short wait times and poor health outcomes. Failure to adjust for this may lead researchers to conclude long waits are good for health. † Figure created from data reported in Prentice and Pizer (Table 1).13
The mean wait time for individuals with an ACSC hospitalization was three days shorter than the mean wait time for individuals without an ACSC hospitalization (Fig. 3). Using a wait time measure based on services individuals actually used seems to imply that waiting for health care reduced the probability of experiencing an ACSC hospitalization.
To overcome this problem, researchers have developed a proxy wait time measure that is not affected by prior individual health status. Refer to Prentice & Pizer 12,13 for a detailed example of how this measure is constructed. Using this wait time measure, the mean number of days waiting for an appointment is half a day longer for patients who experienced an ACSC hospitalization compared to patients who did not experience an ACSC hospitalization (Fig. 3).
REVIEW OF RESULTS
Studies Examining VA Wait Times and Utilization
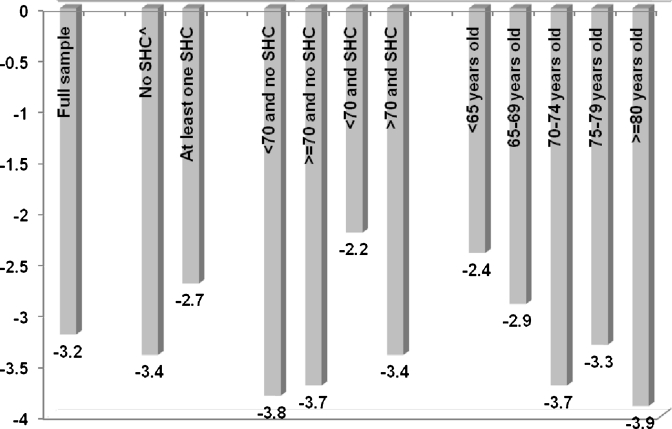
The first question addressed in this review is whether long waits for health care decrease health care utilization. Studies relying on VA data find small effects of wait times. In a VA-Medicare eligible sample of patients with diabetes that used only the VA for outpatient care in the baseline year, VA wait times slightly reduced primary care utilization. Prentice et al. found that an increase of 21 days in wait times for VA primary care induced a decline in primary care utilization of between 2% and 4% (see Fig. 4). The largest decreases in utilization were for patients without a selected health condition (e.g. conditions like heart failure that would increase the likelihood of experiencing poor outcomes) and individuals aged 70 or older.14
Figure 4.
Policy simulation predicting percent decrease in VA primary care utilization with a 21-day increase in wait times among a sample of patients with diabetes* (* Abstracted from Prentice JC, Fincke BG, Miller DR and Pizer, SD. “Waiting for primary care and health outcomes among elderly patients with diabetes” Health Services Research).14 ^ SHC = selected health condition and is defined as anyone diagnosed with retinopathy, neuropathy, nephropathy, cardiovascular, cerebrovascular, peripheral vascular or metabolic disease according to Young et al. 44 or anyone with congestive heart failure, cardiac arrhythmias, valvular disease, peripheral vascular disease, renal failure or obesity according to Elixhauser et al.45
Veterans who are eligible for both Medicare and the VA have the option to use Medicare services when faced with long waits in the VA, so it has been hypothesized that if dissatisfaction is great enough, veterans will substitute other public or private health care services for VA care. This does not appear to be the case. Prentice and colleagues found that there was no significant effect on Medicare utilization among the sample of patients with diabetes who relied exclusively on the VA for outpatient care in the baseline year.14 Likewise, a second study using a sample of veterans drawn from the Medicare Current Beneficiary Survey (MCBS) who largely relied on Medicare found that an annual increase in VA wait times of 10 days increased Medicare utilization by only 1.6 visits annually with no significant effect on VA utilization.26 The results from these two studies are consistent in that veterans who are mainly accessing one health care system for their care prefer to continue accessing the same system even if required to wait longer. Established clinical relationships probably prevent most veterans from making major changes in response to changes in waiting times in the short run.
Studies Examining VA Wait Times and Health Outcomes
Do long waits for health care cause poorer health outcomes? Studies that utilized VA wait time data to examine the effect of waiting for outpatient care in the VA on several different veteran populations are summarized in Table 1. There was a consistent relationship between waiting longer for VA care and poorer health outcomes, especially among older and more vulnerable populations.
Table 1.
Summary of Abstracted Results from Studies Examining the Effect of Wait Times on Health Outcomes
| Study | Population | Outcomes | Significant Results |
|---|---|---|---|
| Prentice & Pizer 12 | Veterans visiting geriatric clinics | Mortality (long-term) | Veterans who visited facilities with an outpatient wait time of 31 days or more were 21% more likely to die compared with veterans who visited a facility with a wait time of less than 31 days (P < =0.05) |
| Prentice & Pizer 13σ | Veterans visiting geriatric clinics | ACSC hospitalization (long-term) | Veterans who visited facilities with outpatient waits of greater than 29 days had a significantly higher probability of experiencing an ACSC hospitalization compared to veterans who visit facilities with waits of less than 22.5 days. Significant at P < 0.05 for all waits > =29 days except for 31.5-34.4 days which is significant at P < =0.10 |
| Prentice, Fincke, Miller & Pizer 14 | Veterans diagnosed with diabetes | Mortality AMI Stroke ACSC hospitalization (long-term) | Mortality A 10-day increase in facility-level primary care wait time led to a 2% (P < =0.10) increase in the odds of mortality for veterans aged > =70 and with a selected health condition (SHC)^ and a 4% (P < =0.05) increase for veterans aged > =80 |
| AMI A 10-day increase in facility-level primary care wait time led to a 3% increase in the odds of experiencing an AMI for veterans with a SHC and a 5% increase for veterans aged 75–79 years old (P < =0.10 for both groups) | |||
| Stroke A 10-day increase in facility-level primary care wait time led to a 6% increase in the odds of experiencing a stroke for veterans aged > =70 and with a SHC and a 9% increase for veterans aged 70–74 years old (P < =0.05 for both groups) | |||
| ACSC hospitalization A 10-day increase in facility = level primary care wait time led to a 3% increase (P < =0.05) for veterans aged 80 or older | |||
| Prentice, Fincke, Miller & Pizer 15 | Veterans diagnosed with diabetes | A1C (intermediate) | Veterans who visited VA facilities with wait times of longer than 32.5 days had small significant (P < =0.05) increases in A1C levels of 0.14 percentage point for the whole sample, 0.07 percentage points for patients with baseline A1C levels less than 7%, 0.11 percentage points for patients with baseline A1C levels between 7% and 8%, and 0.18 percentage points for patients with baseline A1C levels greater than 8% |
σ With kind permission from Springer Science + Business Media: Health Services and Outcomes Research Methodology "Waiting Times and Hospitalizations for Ambulatory Care Sensitive Conditions," 8, 2008, p. 12, Prentice & Pizer, Table 4
^ SHC = selected health condition and is defined as anyone diagnosed with retinopathy, neuropathy, nephropathy, cardiovascular, cerebrovascular, peripheral vascular or metabolic disease according to Young et al.44 or anyone with congestive heart failure, cardiac arrhythmias, valvular disease, peripheral vascular disease, renal failure or obesity according to Elixhauser et al. 45
Prentice & Pizer initially selected a sample of veterans who had geriatric clinic appointments in the VA during the baseline period and predicted mortality and ACSC hospitalizations.12,13 Geriatric clinics were selected because these outpatient clinics are specifically focused on preventing and managing complications and conditions due to aging. As a result, these patients were older and more frail than the general population, making them particularly sensitive to variation in wait times.12,13 The wait time used in these studies was an average of waits until the next available appointment in 46 different outpatient appointment types that the VA relies on for performance measures. These appointment types were high volume, represented over 90% of patient-provider interactions (versus other services such as labs or telephone consultations), and covered all major medical sub-specialties.27 There was a significant and positive relationship between longer waits for VA care and an increased risk of both mortality and experiencing an ACSC hospitalization. The relationship was a step function with significant increases in risk occurring around 31 days for mortality and 29 days for ACSC hospitalization (Table 1).12,13
These two studies on geriatric clinic patients provided initial evidence that waiting for outpatient care is related to health, but this was a heterogeneous group of patients with a variety of health conditions and the influence of wait times on outcomes for patients with specific conditions was unknown. To overcome this limitation, Prentice et al. (in press, 2011) identified a sample of veterans diagnosed with diabetes and examined the effect of wait times on long-term and intermediate outcomes.14,15 A sample of patients with diabetes was chosen because it is well established that complications from diabetes can be prevented or managed with timely outpatient care.9,24,28 These studies used the wait until the next available appointment in primary care because VA primary care doctors manage the majority of diabetes care.29
Prentice et al. 14 examined the effect of wait times on long-term health outcomes including mortality, acute myocardial infraction (AMI), stroke and ACSC hospitalization. Waiting for outpatient care did not significantly increase the risk of poor health outcomes for the entire sample. Subsequent analyses stratified the sample by the presence of a selected health condition (e.g. conditions like heart failure that would increase the likelihood of experiencing one of the long-term health outcomes) and age. Consistent with the findings on geriatric clinic patients, veterans aged 70 or older with a selected health condition were at a significantly increased risk of experiencing poor health outcomes when their VA facility has longer versus shorter waits. The relationship between longer wait times and AMI bordered on significant for veterans with a selected health condition regardless of age. Veterans aged 70 or older with a selected health condition had a 2% increase in the odds of dying and a 6% increase (P = 0.05) in the odds of experiencing a stroke when their VA facility has longer versus shorter waits (Table 1).14
Longer wait times significantly increased the risk of experiencing poor health outcomes for veterans aged 70 or older regardless of whether they suffered from a selected health condition (Table 1). Veterans aged 70 to 74 visiting facilities with longer waits had a 9% increase in the odds of experiencing a stroke (P < 0.05), veterans aged 75 to 79 visiting facilities with longer waits had a 8% increase in the odds of experiencing an AMI (P < 0.10) and veterans aged 80 or more visiting facilities with longer waits had a 4% and 3% increase in the odds of dying and experiencing an ACSC hospitalization (P < 0.05 for both).14
In a subsequent study intermediate outcomes were also poorer, especially for veterans with the poorest baseline glycemic control (Table 1). Glycated hemoglobin (A1C) levels were predicted to increase 0.073 percentage points for veterans with baseline levels less than 7, 0.114 percentage points for veterans with baseline levels between 7 and 8 and 0.177 percentage points for veterans whose baseline levels were greater than 8 when the VA facility had waits of more than 32.5 days versus 32.5 days or less.15
DISCUSSION
This narrative review examined research conducted in the VA to answer two questions. First, how much do longer wait times decrease health care utilization? There are small, yet statistically significant decreases in utilization as a result of longer VA wait times (Fig. 4).14 Second, do longer wait times cause poorer health outcomes? Delayed access to healthcare is related to poorer health, especially among elderly and vulnerable veteran populations. Both long-term outcomes such as mortality and intermediate outcomes such as HbA1c levels are worse for veterans who visit facilities with longer waits compared to veterans who visit facilities with shorter waits (Table 1).12–15
The small effects of wait times on health care utilization suggest that the mechanism connecting delayed access to care and poor health works more through the timing of appointments than the volume of appointments.14 Research outside of the VA supports this hypothesis. Solberg et al. found that open access scheduling (e.g. next day scheduling (OA)) had no effect on overall utilization but significantly decreased urgent care visits for depression, diabetes and coronary heart disease.30
The main goal of the reviewed studies in the VA (Table 1) that examined the effect of wait times on health outcomes was to indentify the causal relationship between waiting for healthcare and health outcomes. Methodological techniques such as the use of exogenous wait times measures or facility-fixed effects were employed to help identify causality.12–15 Despite the use of these techniques, the principal limitation of these studies is that alternative explanations for the findings, including reverse causation and omitted variables, cannot be ruled out. An example of reverse causation is an unobserved local flu epidemic at a VA facility that may increase wait times and cause poorer health outcomes that are not attributable to longer wait times. An example of omitted variable bias is a change in facility management that could simultaneously improve quality, reduce waiting times and improve outcomes through better resource allocation. The key to these explanations is that they feature unobservable local changes that are correlated with both local waiting time variations and local outcome changes. Either of these situations could in principle have caused the observed relationships between waiting for healthcare and health outcomes. In the absence of truly random variation in wait times, this limitation is unavoidable.14
A key area for future research is to investigate the connections between longer waits for health care, patient satisfaction, health care utilization and health outcomes. A limitation of many of the studies that find effects of waiting times on patient satisfaction is their focus on populations waiting in emergency departments or waiting for elective surgery (see Fogarty & Cronin 2007)6 where there is typically not an established clinical relationship. Prentice et al. (in press) and Pizer & Prentice (in press) find that veterans who are largely accessing one network for health care prefer to wait out short-term fluctuations in waits instead of switching networks to get care faster.14,26 More research is needed to determine the health consequences of a patient’s preference to wait longer to obtain care from their usual source of care (and potentially forego care altogether) versus receiving care faster from unfamiliar providers.
The effect of delayed access to care on intermediate health outcomes and chronic disease management also needs further research. Studies outside of the VA have also found an effect of delayed access to care on HbA1c levels. For example, Subramanian et al.31 compared private sector primary care clinics that had implemented OA to control clinics using patients diagnosed with diabetes. There was a statistically significant, yet modest effect of visiting an OA clinic on HbA1c levels that was similar to the effect found in the Prentice et al. study.15,31 The effect of more timely access to care in these two studies is roughly a quarter to a third of the effect seen for the most successful multi-faceted quality improvement programs aimed at glycemic control. These quality improvement programs implement a wide range of interventions, such as patient registries, clinician education or case management but do not usually focus on improving timely access to care,32–34 making the significant effect of timely access to healthcare on HbA1c notable. Future research should examine the effect of longer wait times on intermediate outcomes beyond HbA1c, such as lipid control or blood pressure. As well, research should focus on the effect of longer wait times on chronic disease management. A "white coat effect" has been found on medication adherence where patients are more likely to adhere to medications right before and after doctor’s appointments.35,36 Consequently, timely access to care may mediate intermediate health outcomes by helping to promote consistent medication adherence. On the other hand, Subramanian et al. found that HbA1c testing occurred less frequently in OA clinics versus control clinics resulting in fears that OA scheduling increased focus on acute care management and crowded out long-term chronic disease management.31
More work also needs to be done to identify patient populations most adversely affected by delays in access to health care. Prentice et al. (in press) used a sample of patients diagnosed with diabetes, and found the largest decreases in utilization were for patients without a selected health condition and individuals aged 70 or older. The former group was not at an increased risk of experiencing poor health outcomes measured by the study, but the latter group was.14 Similarly, Solberg et al. found patients with coronary heart disease had a significantly lower number of hospital admissions and shorter lengths of stay after OA implementation compared to before OA implementation but there were no significant differences in hospitalizations for patients with depression and diabetes.30
Policymakers debate the most effective scheduling policies to best serve the needs of all patients. Opponents of triaging argue the process may be wasteful of healthcare resources. Triaging decreases health care supply because it requires providers to take the time to determine the seriousness of the condition and manage future appointments instead of providing care. As well, triaging increases demand because patients with urgent needs see a clinician who is not their regular provider and the patient must see their regular physician for follow-up, converting one appointment into two.22 As noted in this review some patient populations can wait without measured adverse effects. Supporters of triage argue determining the patient populations at highest risk of experiencing poor health outcomes and subsequently prioritizing access for these patients outweighs the costs of triaging less vulnerable patients.37
Consequently, VA managers may want to consider prioritizing patients based on vulnerability to wait time-related outcomes to further reduce wait times. Similar policies have been implemented in healthcare systems outside the United States with the hope of achieving more rational management of demand, but have met with mixed success.38–40 The implementation of prioritization policies is difficult due to their controversial nature with many patients objecting to the idea that their care may be rationed. Healthcare systems that have been successful in implementing prioritization policies established committees with decision making power to set prioritization criteria and relied heavily on experts to make these decisions.39 The strong central management focus in the VA (e.g. holding senior managers accountable for performance measures)41 makes it likely that prioritization policies could be successfully implemented.
If wait times increase with the implementation of national health care reform as expected, some of the policies used to decrease wait times in the VA can be considered outside of the VA. The policy with the greatest impact may be the systematic collection of wait time data. Collecting the data allowed the VA to evaluate the success of specific policies aimed at decreasing wait times. Overall, VA interventions to reduce wait times have been focused on maximizing the efficiency of currently available resources and have had significant success (Fig. 2). These interventions have included nationwide implementation of OA scheduling in six target clinics (e.g. primary care, cardiology), instituting and maintaining a primary care gatekeeper model with a cap on how many patients are assigned to each primary care physician to help ensure that patients can access primary care physicians when desired, performance monitors that track which clinics and facilities are meeting targets for access, directives on which patients should receive priority access (e.g. veterans with service-connected disability) when clinics have long waits for appointments, and denied enrollment to new veterans in the lowest priority groups.18–21,42,43 Similar to the VA, healthcare systems outside of the United States struggling with long waits have historically focused on increasing capacity through increased funding or system redesigns that increase productivity.40 The likelihood of longer wait times with health reform in combination with poorer health outcomes for some patient populations due to long waits means U.S. policymakers will need to consider the same strategies to manage wait times and ensure appropriate access for all patient populations.
Funding Sources and Acknowledgements
Funding for this research was provided by Grant No: IAD-06-112 and IIR 04–233 from the Health Services Research and Development Service, Department of Veterans Affairs and Grant No: 62967 from the Health Care Financing and Organization Initiative under the Robert Wood Johnson Foundation. Neither author has any conflicts of interest to report. The authors are indebted to Matthew Neuman and John Gardner for programming support. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs. This research was approved by the VA Boston Health Care System institutional review board.
Conflict of interest None disclosed.
References
- 1.Crossing the quality chasm: a new health system for the 21st century. Washington D.C: Institute of Medicine; 2001. [PubMed] [Google Scholar]
- 2.Fortney JC, Burgess JF, Bosworth HB, Booth BM, Kaboli PJ. A re-conceptualization of access for 21st century healthcare, J Gen Intern Med. In press. doi:10.1007/s11606-011-1806-6 [DOI] [PMC free article] [PubMed]
- 3.Buchmueller TC, Grumbach K, Kronick R, Kahn JG. The rffect of health insurance on medical care utilization and implications for insurance expansion: a review of the literature. Med Care Res Rev. 2005;62(1):3–30. doi: 10.1177/1077558704271718. [DOI] [PubMed] [Google Scholar]
- 4.Congressional Budget Office. Key issues in analyzing major health insurance proposals. Washington D.C.; 2008. http://www.cbo.gov/ftpdocs/99xx/doc9924/toc.shtml [Accessed on October 13, 2010].
- 5.Kowalczyk L.Across Mass., waits to see the doctor grows. The Boston Globe. September 22, 2008.
- 6.Fogarty C, Cronin P. Waiting for healthcare: a concept analysiss. J Adv Nurs. 2007;61(4):463–471. doi: 10.1111/j.1365-2648.2007.04507.x. [DOI] [PubMed] [Google Scholar]
- 7.Eilers GM. Improving patient satisfaction and waiting time. J Am Coll Heal. 2004;53(1):41–45. doi: 10.3200/JACH.53.1.41-48. [DOI] [PubMed] [Google Scholar]
- 8.Kenagy JW, Berwick DM, Shore MF. Service quality in health care. J Am Med Assoc. 1999;281(7):661–665. doi: 10.1001/jama.281.7.661. [DOI] [PubMed] [Google Scholar]
- 9.American Diabetes Association Standards of medical care in diabetes. Diabetes Care. 2005;28(1):S4–S36. doi: 10.2337/diacare.28.suppl_1.S4. [DOI] [PubMed] [Google Scholar]
- 10.Mayfield JA, Reiber GE, Sanders LJ, Jannisse D, Pogach LM. Preventive foot care in people with diabetes. Diabetes Care. 1998;21(12):2161–2177. doi: 10.2337/diacare.21.12.2161. [DOI] [PubMed] [Google Scholar]
- 11.The doctor will see you in 3 months. Bloomberg Businessweek, 2007.
- 12.Prentice JC, Pizer SD. Delayed access to health care and mortality. Heal Serv Res. 2007;42(2):644–662. doi: 10.1111/j.1475-6773.2006.00626.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prentice JC, Pizer SD. Waiting times and hospitalizations for ambulatory care sensitive conditions. Health Serv Outcomes ResMethodology. 2008;8:1–18. doi: 10.1007/s10742-007-0024-5. [DOI] [Google Scholar]
- 14.Prentice JC, Fincke BG, Miller DR, Pizer SD. Waiting for primary care and health outcomes among elderly patients with diabetes. Health Serv Res. In Press. [DOI] [PMC free article] [PubMed]
- 15.Prentice JC, Fincke BG, Miller DR, Pizer SD. Outpatient waiting times and diabetes care quality improvement. Am J Managed Care. 2011;17(2):e43–e54. [PubMed] [Google Scholar]
- 16.United States General Accounting Office. VA needs better data on extent and causes of waiting times; 2000. GAO/HEHS-00-90.
- 17.United States General Accounting Office. More national action needed to reduce waiting times, but some clinics have made progress. 2001:22 GAO-01-953.
- 18.Department of Veterans Affairs. Priority for outpatient medical services and inpatient hospital care: 2002. VHA Directive 2002–059.
- 19.Department of Veterans Affairs. Process for managing patients when patient demand exceeds current clinical capacity: VHA Directive 2003.2003-068.
- 20.Department of Veterans Affairs. Process for ensuring timely access to outpatient clinical care: 2006. VHA Directive 2006–028.
- 21.Department of Veterans Affairs. VHA outpatient scheduling processes and procedures 2010. 2010. VHA Directive 2010–027.
- 22.Murray M, Berwick DM. Advanced access: reducing waiting and delays in primary care. J Am Med Assoc. 2003;289:1035–1040. doi: 10.1001/jama.289.8.1035. [DOI] [PubMed] [Google Scholar]
- 23.Yang Z, Gilleskie DB, Nortaon EC.Prescription drugs, medical care and health outcomes: a model of elderly health dynamics: University of North Carolina; 2006.
- 24.AHRQ wuality indicators-Guide to prevention wuality indicators: hospital sdmission for ambulatory care sensitive conditions. Rockville, MD: Agency for Healthcare Research and Quality; 2001. 02-R0203.
- 25.Wang G, Zhang Z, Ayala C, Wall HK, Fang J. Cost of heart failure-related hospitalizations in patients aged 18 to 64 years. Am J Managed Care. 2010;16(10):769–776. [PubMed] [Google Scholar]
- 26.Pizer SD, Prentice JC. Time Is money: delayed access to outpatient care and health insurance choices of elderly veterans in the United States. J Health Econ. In press. [DOI] [PubMed]
- 27.Baar B.New patient monitor: data definitions: Veteran Health Administration Support Services Center; 2005.
- 28.Ross SA. Controlling diabetes: the need for intensive therapy and barriers in clinical management. Diabetes Res Clin Practice. 2004;65S:S29–S34. doi: 10.1016/j.diabres.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 29.Helmer DA, Sambamoorthi U, Rajan M, Tseng C-L, Pogach LM. Glycemic control in elderly veterans with diabetes: individualized, not age-based. Diabetes Care. 2008;31:728–731. doi: 10.2337/dc07-1431. [DOI] [PubMed] [Google Scholar]
- 30.Solberg LI, Maciosek MV, Sperl-Hillen JM, et al. Does improved access to care affect utilization and costs for patients with chronic conditions? Am J Managed Care. 2004;10(10):717–722. [PubMed] [Google Scholar]
- 31.Subramanian U, Ackermann RT, Brizendine EJ, et al. Effect of advanced access scheduling on processes and intermediate outcomes of diabetes care and utilization. J Gen Internal Med. 2009;24(3):327–333. doi: 10.1007/s11606-008-0888-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knight K, Badamgarav E, Henning JM, et al. A systematic review of diabetes disease management programs. Am J Managed Care. 2005;11:242–250. [PubMed] [Google Scholar]
- 33.Norris SL, JNichols PJ, Caspersen CJ, 4S et al. The effectiveness of disease and case management for people with diabetes. Am J Prev Med. 2002;22:15–38. doi: 10.1016/S0749-3797(02)00423-3. [DOI] [PubMed] [Google Scholar]
- 34.Shojania KG, Ranji SR, McDonald KM, et al. Effects of quality improvement strategies for Type 2 Diabetes on glycemic control: a meta-regression analysis. J Am Med Assoc. 2006;296:427–440. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]
- 35.Cramer JA, Scheyer RD, Mattson RH. Compliance declines between clinic visits. Archives of Internal Med. 1990;150:1509–1510. doi: 10.1001/archinte.150.7.1509. [DOI] [PubMed] [Google Scholar]
- 36.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–3035. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- 37.Gravelle H, Siciliani L. Third degrees waiting time discrimination: optimal allocation of a public sector healthcare treatment under rationing by waiting. Heal Econ. 2009;18:977–986. doi: 10.1002/hec.1423. [DOI] [PubMed] [Google Scholar]
- 38.Alter DA, Newman AM, Cohen EA, Sykora K, Tu JV. The evaluation of a formalized queue management system for coronary angiography waiting lists. Can J Cardiol. 2005;21(13):1203–1209. [PubMed] [Google Scholar]
- 39.Sabik LM, Lie RK. Priority setting in health care: lessons from the experiences of eight countries. Int J Equity Health. 2008;7(4):1–13. doi: 10.1186/1475-9276-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Willcox S, Seddon M, Dunn S, Edwards RT, Pearse J, Tu JV. Measuring and reducing waiting times: A cross-national comparison of strategies. Heal Aff. 2007;26(4):1078–1087. doi: 10.1377/hlthaff.26.4.1078. [DOI] [PubMed] [Google Scholar]
- 41.Congressional Budget Office CB. Quality initiatives undertaken by the Veterans Health Administration; 2009. http://www.cbo.gov/ftpdocs/104xx/doc10453/08-13-VHA.pdf [Accessed on October 21, 2010]
- 42.Lukas CV, Meterko M, Mohr D, Seibert MN.The implementation and effectiveness of advanced clinicaccess. HSR&D Management Decision and Research Center. Boston: Office of Research and Development, Department of Veteran Affairs; 2004:80.
- 43.Congressional Budget Office. The potential cost of meeting demand for veterans’ health care. 2005. http://www.cbo.gov/ftpdocs/61xx/doc6171/03-23-Veterans.pdf [Accessed on September 28, 2010].
- 44.Young BA, Lin E, Korff MV, Simon G, Ciechanowski P, Ludman EJ, Everson-Stewart S, Kinder L, Oliver M, Boyko EJ, Katon WJ. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Managed Care. 2008;14(1):15–24. [PMC free article] [PubMed] [Google Scholar]
- 45.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]