Abstract
The purpose of this study was to test the effect of computer-generated, tailored feedback on the quality of chronic disease management for type 2 diabetes when provided to a patient prior to a scheduled physician visit. A stand-alone computer application was developed to provide tailored feedback aimed at empowering patients to engage more actively in their diabetes management. Adults with type 2 diabetes (n = 203) were randomly assigned to groups receiving either efficacy (positive) messages (n = 68), risk (negative) messages (n = 67), or to a delayed treatment control group (n = 68). The intervention was delivered prior to a patient's visit with his or her physician so that patients would have the opportunity to discuss the messages at the clinical appointment.
Although there were no significant differences in the percentage of participants who received intensified care or routine tests between the control and intervention groups, we learned that more directive messaging may be needed to help patients effectively manage their diabetes.
Patients may benefit from directive feedback, providing them with specific questions to ask their physician that can lead to improved care, rather than receiving general and educational informational messages. (Population Health Management 2009;12:197–204)
Introduction
Diabetes is one of the most prevalent chronic diseases in the United States. This chronic disease affects approximately 20.8 million people in the United States, with 6.2 million of these individuals remaining undiagnosed.1 Of diagnosed cases, 90%–95% are type 2 diabetes.2
Though guidelines for caring for patients with diabetes are available from a variety of organizations, such as the American Diabetes Association (ADA), and medical experts,3–5 wide differences in blood sugar control and quality of care remain.6,7 In the Third National Health and Nutrition Interview Examination Survey, fewer than half of Americans with known diabetes met blood sugar goals (glycosylated hemoglobin [A1c] <7%) and fewer than 30% reported having an A1c test at least once each year.6 Another study found that fewer than 20% of 2865 adults with diabetes who received care at community health centers met similar blood sugar goals.7 Given the 35% increase in the risk of micro-vascular complications for each percentage increase in A1c, improvement in diabetes care is not only desirable, but also increasingly necessary.3,8
Research has shown that getting patients actively involved in the management of their chronic illness is essential to improving care.9,10 In one intervention that had a significant positive effect on improving glucose control, patients with diabetes met with an assistant who reviewed their medical record and, using a diabetes care algorithm, encouraged the patients to use the information to negotiate medical decisions with their doctors.9 This finding supports the fact that patients who are encouraged to ask their physician for treatments are more likely to receive them.11
Further research conducted on improving quality of care for chronic conditions through patient involvement utilizes the Chronic Care Model, which employs 6 basic elements for improving chronic illness (eg, self-management support, decision support, clinical information systems).12 Use of the model is intended to foster productive interactions between patients who proactively participate in their care and providers who can draw on the expertise of guideline-based reminders and decision support.10,13 Preliminary results suggest that organizational interventions based on this model lead to improvements in chronic diseases.12 The intervention in this study is based on active participation of both patients and providers, using tailored messaging.
Tailoring health messages to individual patients has been identified as a key way of making information more relevant to its intended audience and, as a result, more effective.14 Studies demonstrating positive results have tested tailored messages to determine their effects on behavior changes ranging from quitting smoking and eating fruit to increasing physical activity and receiving preventive medical services.15–19 In addition, research has shown that the type of message an individual receives with regard to health-related behaviors can impact the effectiveness of the message. A recent study showed that positive and neutral messages were more successful in facilitating self-reported hearing protection behaviors among coal miners than negative messages.20
Past research has examined the use of computer-generated decision support reports for both physicians and patients to help increase recommended services utilization for individuals with diabetes.21–24 However, no study to date has examined the effects of computer-generated decision support messages, given to a patient prior to a scheduled clinical appointment, on the improvement of chronic disease management.
Therefore, we conducted a study to assess the effectiveness of computer-tailored diabetes care messages to empower patients to ask their physicians about improvements that could be made to their diabetes self-management. The research seeks to determine how the type of message received by patients—risk-oriented (negative) or efficacy-oriented (positive)—impacts the effectiveness of the message. In addition, we wanted to determine if patients who received the tailored messages inquired about these messages at their clinical appointment. The hypothesis was that efficacy-oriented messages would lead to greater improvement in diabetes management than risk-oriented messages. We were also interested in determining if the interventions would lead to greater physician compliance with diabetes care guidelines, and would empower patients to discuss diabetes management with their physicians.
Methods
Study design
Using a randomized controlled trial, 203 adults with type 2 diabetes were assigned to 1 of 2 intervention groups or to a delayed treatment control group. The intervention, delivered prior to a patient's visit with their primary care physician (PCP), included an assessment of adherence to standards of care for diabetes management. One group then received efficacy-oriented (positive) tailored messages (n = 68), and the other received risk-oriented (negative) messages (n = 67) about their diabetes care. An exit interview was conducted with both groups within 72 h of the patient's physician visit. The delayed treatment group (n = 68) received the efficacy-oriented messages after their exit interview. Approval for the study was obtained from the Institutional Review Board, Office of Research Administration at The Miriam Hospital in Providence, Rhode Island.
Subjects
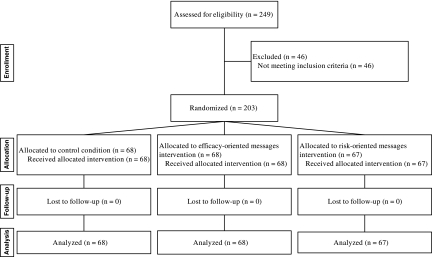
The study population (≥age 21 years) was receiving routine outpatient care for type 2 diabetes between September 2003 and July 2004 (Fig. 1). Participants were recruited through an advertisement on www.google.com. Interested individuals (n = 249) contacted the study's research assistant and were screened for eligibility based on the following criteria: (1) upcoming visit scheduled within 6 weeks with physicians who cared for their diabetes, (2) self-reported type 2 diabetes mellitus that was not related to pregnancy, (3) self-reported use of a glucometer 1 or more times in the past month, (4) a visit to a PCP for diabetes care at least once in the past 12 months, and (5) access to the Internet at home or at work. Forty-six patients were excluded for the following reasons: (1) not diagnosed with diabetes; (2) had type 1 diabetes; (3) lived outside the United States; or (4) the study closed before their scheduled PCP visit. All of the remaining 203 patients completed the post-visit questionnaire with no attrition.
FIG. 1.
Participant flow.
Intervention
The intervention consisted of 3 main components. First, a telephone survey was administered to assess the degree to which certain ADA guidelines were being met for compliance to care.3 These guidelines included the following: (1) blood pressure (BP) < 130/80; (2) low-density lipoprotein (LDL) cholesterol < 100 mg/dL (5.5 mmol/L); (3) A1c < 7.0%; (4) blood test for A1c within the past 6 months; (5) tests for LDL, A1c, and urine protein within the last year; (6) foot exam, eye exam, and flu shot within the last year; and (7) a diabetes self-management course and appointment with a dietitian or nutritionist within the past year.3
Second, tailored, computer-generated reminders aimed at empowering patients to engage in their diabetes management more actively were mailed to both intervention groups. These reminders suggested appropriate tests and treatments for which the patient was due, as well as guideline-based changes to treatment.5,25,26 The type of messages participants received differed between the 2 intervention groups. The efficacy-oriented (positive) message group received a message discussing the health benefits of diabetes management. For example, patients with LDL ≥100 mg/dL received messages such as: “It's important for people like yourself with diabetes to keep blood pressure well controlled, to protect the heart and the kidneys . . .” Conversely, patients in the risk-oriented (negative) message group received a message discussing the risks of poor diabetes management. For example, patients with BP ≥130/80 received the following message: “High blood pressure can be deadly for people with diabetes. It can severely damage the heart, it can cause your kidneys to malfunction, and it can also lead to blindness . . .” Table 1 presents additional examples.
Table 1.
Tailored Messages
| Uncontrolled parameter | Risk-oriented message | Efficacy-oriented message |
|---|---|---|
| Blood pressure | High blood pressure can be deadly for people with diabetes. It can severely damage the heart, it can cause your kidneys to malfunction, and it can also lead to blindness | Controlling blood pressure can be particularly helpful for people with diabetes. By keeping your blood pressure controlled, you can protect your eyes, heart, and kidneys. You can take simple and effective steps to keep your blood pressure under control. |
| Cholesterol | High blood cholesterol can be deadly for people with diabetes. It greatly increases the chances of a heart attack or stroke. High cholesterol is a high-risk factor for people with diabetes. | Controlling blood cholesterol can be particularly helpful for people with diabetes. By keeping cholesterol controlled, you can greatly lower your chances of a heart attack or a stroke. You can take simple and effective steps to control your blood cholesterol level. |
| Blood sugar | High blood sugar causes much of the damage from diabetes. It damages the heart, eyes, and kidneys, leading to heart attacks, blindness, and kidney failure. High blood sugar is a high-risk factor for people with diabetes. | Controlling blood sugar is essential for people with diabetes. Good blood sugar control can greatly help to protect your eyes, heart, and kidneys. You can take simple and effective steps to control your blood sugar level. |
Lastly, pocket-sized charts were provided to participants on which to enter key clinical data and track it over time before a primary care visit. The information collected on the charts included BP, A1c, LDL, urine protein, and fasting plasma glucose levels. These pocket-sized cards have been shown to be accurate at assisting patients to collect key clinical data during visits with health care providers.17
Procedures
Eligible individuals were mailed consent forms. Those who completed and returned the consent form were considered to be enrolled participants. Participants then completed a telephone-based pre-visit questionnaire, based on the ADA guidelines, approximately 10 days before their planned visit date with their PCP. Using an automated computer algorithm, participants were then randomly allocated to 1 of 3 groups: control, risk-oriented message group, or efficacy-oriented message group. Each of the 2 intervention groups were mailed computerized reports 1 week prior to their scheduled primary care visit. These tailored messages were generated based on the patient's answers to the pre-visit questionnaire. These reports contained the patient's recent test results (ie, blood pressure, cholesterol, A1c) along with his/her currently prescribed medications. Further, the computerized report included a personalized assessment plan that contained several efficacy or risk-oriented messages relating to blood pressure, cholesterol, blood sugar, and urine protein, as well as offered educational information on diabetes and diet. Patients assigned to the control group received reports containing the efficacy message shortly after the visit with their PCP. For example, the control group would receive a message such as, “Having a yearly flu shot each fall or early winter is essential for people with diabetes. You can take simple and effective steps to protect yourself from getting a severe case of the flu.” No face-to-face visits were scheduled with research staff for this study.
Within 72 hours of the patient's visit with their PCP, a research assistant administered a telephone follow-up survey. The research assistant did not know which group the patients had been randomly assigned to at the time of survey administration. The follow-up survey asked patients about counseling and other care that may have happened during their visit, including physical activity counseling, medication dose changes, and cholesterol testing (see Table 3).
Table 3.
Intensification of Care and Routine Testing Across Groups
| Control condition, n = 68 (%) | Efficacy-oriented message condition n = 68 (%) | Risk-oriented message condition n = 67 (%) | P value | |
|---|---|---|---|---|
| Intensification of Care | ||||
| Did your doctor recommend that you START taking a new medication for your diabetes? | 8.8 | 11.8 | 13.4 | 0.69 |
| Did your doctor recommend that you CHANGE the dose of at least 1 medicine that you were already taking for your diabetes? | 22.0 | 31.6 | 25.4 | 0.50 |
| Did your doctor recommend that you START taking a new medication for your blood pressure? | 8.2 | 4.4 | 8.5 | 0.68 |
| Did your doctor recommend that you CHANGE the dose of at least 1 medicine that you were already taking for your blood pressure? | 8.3 | 11.4 | 17.1 | 0.44 |
| Did your doctor recommend that you START taking a new medication for your blood cholesterol? | 7.3 | 2.6 | 14.0 | 0.17 |
| Did your doctor recommend that you CHANGE the dose of at least 1 medicine that you were already taking for your cholesterol? | 5.3 | 6.9 | 5.3 | 0.95 |
| Routine Testing | ||||
| Did your doctor recommend that you have a blood test for HEMOGLOBIN “A ONE C”? A blood test called hemoglobin “A one C” measures the average level of blood sugar over the previous 3 months, and is a test you cannot do at home. | 63.2 | 72.1 | 59.7 | 0.30 |
| Did you have your blood pressure checked? | 98.5 | 95.6 | 97.0 | 0.60 |
| Did your doctor recommend that you have your blood tested for cholesterol? | 63.2 | 55.9 | 58.2 | 0.67 |
| Did someone weigh you? | 92.7 | 97.1 | 91.0 | 0.33 |
| Did your doctor recommend that you have an eye exam in which your pupils will be dilated? (This test is usually done by an ophthalmologist or an optometrist and makes your eyes temporarily sensitive to bright light.) | 50.0 | 51.5 | 38.8 | 0.27 |
| Did your doctor recommend that your urine be checked for protein? People with diabetes often have a test of their urine looking for “protein” or “microalbumin” to measure how well the kidneys function. | 42.7 | 55.9 | 47.8 | 0.30 |
| Did you receive a pneumonia vaccination? | 1.5 | 5.9 | 3.0 | 0.36 |
| Did your doctor recommend that you take a course or class on how to manage your diabetes yourself? | 17.7 | 26.5 | 26.9 | 0.36 |
Patient-reported information was the only source of data, as providers were not interviewed and research staff did not have access to patient charts. Patients were compensated with a $50 gift card following completion of the follow-up survey.
Measures
The main outcome measures of the study were patient-reported medication dose increases and the addition of medication(s) to control blood pressure, blood glucose, and LDL cholesterol. The need for intensified blood glucose therapy was defined as an A1c level ≥7% and/or the mean of 3 recent fasting blood glucose levels ≥126 mg/dL. The need for intensified hypertensive therapy was defined as BP ≥130/80. The need for intensified LDL therapy was defined as LDL ≥100 mg/dL.3 In addition, patient satisfaction with the physician visit was measured using a validated 9-item measure.27 These measures were collected during the telephone follow-up survey after the physician visit.
Statistical analysis
Intent-to-treat analysis looked for changes in diabetes care, comparing the control group to each intervention group. Outcomes of interest were intensification of care to lower blood glucose, BP, and LDL, based on information from the follow-up survey. To further explore changes in care, the analysis also compared the combined intervention groups vs. the control group, then compared the 2 intervention groups to each other. A number of subgroup analyses were performed. These determined whether participants in need of intensified care, a subgroup of the overall sample, actually received care, according to the exit surveys. For example, participants not meeting LDL goals at baseline were included as the denominator in the cholesterol care subgroup analysis. Numerators were calculated based on the number of eligible participants who received improved care. Finally, differences in patient visit satisfaction among the intervention groups and the control group were examined for significance.
Results
Participants in the control and intervention groups were statistically similar with regard to all characteristics examined, except sex and history of high blood pressure (Table 2).The mean (SD) age of participants was 51.8 (11.0) years. The majority of participants were white, insured, were planning to attend a routine care visit (rather than an urgent visit), and had been with their physician for 3 or more years. Of the 135 participants who received the feedback document prior to the visit (the intervention groups), 116 reported reading all or most of the document.
Table 2.
Characteristics of Study Participants
| Control condition n = 68 | Efficacy-oriented message condition n = 68 | Risk-oriented message condition n = 67 | P value | |
|---|---|---|---|---|
| Mean age | 52.7 | 51.0 | 52.0 | 0.65 |
| Sex, female (%) | 54.4 | 69.1 | 77.6 | 0.01 |
| Race, white (%) | 86.8 | 77.9 | 83.6 | 0.39 |
| Ethnicity, Hispanic (%) | 4.4 | 7.4 | 6.0 | 0.77 |
| Insured (%) | 94.1 | 95.6 | 88.1 | 0.21 |
| Education level, college graduate (%) | 51.5 | 42.7 | 44.8 | 0.56 |
| Household income >$50,000 (%) | 33.8 | 36.8 | 35.8 | 0.94 |
| Mean number of diabetes provider visits in past year | 6.4 | 7.1 | 7.6 | 0.74 |
| History of high blood pressure (%) | 75.0 | 66.2 | 55.2 | 0.05 |
| History of high blood cholesterol (%) | 58.8 | 64.7 | 59.7 | 0.75 |
| History of heart disease (%) | 19.1 | 20.6 | 25.4 | 0.65 |
| Diabetes complication history (%) | 50.0 | 42.7 | 49.3 | 0.64 |
| Blood sugar level controlled (%) | 56.1 | 47.4 | 53.9 | 0.73 |
| Blood pressure controlled (%) | 32.8 | 25.0 | 34.3 | 0.45 |
| LDL cholesterol controlled (%) | 42.1 | 25.0 | 35.7 | 0.52 |
| General health, fair or poor (%) | 26.5 | 39.7 | 34.3 | 0.26 |
| Last time went online for health information, in the last week (%) | 57.4 | 60.3 | 67.2 | 0.49 |
| Visit reason: | ||||
| –Routine examination (%) | 50.0 | 57.4 | 53.7 | 0.65 |
| –A brand new problem (%) | 7.4 | 1.5 | 4.5 | |
| –Follow-up (%) | 39.7 | 35.3 | 38.8 | |
| –Other (%) | 2.9 | 5.9 | 3.0 | |
| Length of physician-patient relationship | 0.80 | |||
| –less than 6 months (%) | 23.5 | 22.1 | 17.9 | |
| –between 6 months and 1 year (%) | 11.8 | 5.9 | 9.0 | |
| –between 1 year and 3 years (%) | 27.9 | 29.4 | 25.4 | |
| –3 years or longer (%) | 36.8 | 42.7 | 47.8 | |
LDL, low-density lipoprotein.
Table 3 presents the percentage of participants in each condition who received intensified care or routine tests at their PCP visit. There were no significant differences in the percentage of participants who received intensified care or routine tests between the control, efficacy-oriented message, and risk-oriented message groups.
For example, there was no significant difference in the number of patients in each group who reported that their physician changed any dose of their diabetes medication (22.0, 31.6, and 25.4, respectively, P = 0.50). The same pattern held true for routine testing. For example, there were no significant differences in the number of patients in each group who reported that their physician recommended that they have their blood tested for cholesterol (63.2, 55.9, and 58.2, respectively, P = 0.67). Subsequent analyses that compared the control condition to the grouped intervention conditions (risk-oriented message and efficacy-oriented message), as well as those that compared the risk-oriented message condition to the efficacy-oriented message condition, likewise showed no significant differences in intensification of care during provider visits.
The exploratory subgroup analyses examined whether care was intensified for patients not meeting diabetes care goals at baseline. Again, no significant differences between the control, efficacy-oriented message, and risk-oriented message groups were revealed (data not presented). Last, analyses of measurements of patient satisfaction with the physician visit also showed no significant differences (data not presented).
Discussion
The aim of this study was to examine whether the use of computer-tailored diabetes care reminders, which were aimed at empowering patients, influenced the care that they received and also improved their self-management of type 2 diabetes. Research has shown not only that computerized prompts for both physicians and patients have been successful in increasing the performance of certain preventive care procedures, but also that patients who are more proactive in requesting treatments are more likely to receive them.11,15,16 It was hypothesized that the interventions would lead to greater physician compliance with diabetes care guidelines and would empower patients to discuss diabetes management with their physicians. The main observation of the study, however, was that the computerized interventions did not result in increased counseling compared to the control group.
In addition, it was hypothesized that the efficacy-oriented messages would lead to greater improvement in chronic disease self-management than the risk-oriented messages. Research has shown that positive (“gain-framed”) messages appear to have a greater impact than negative messages.20 Analyses of the study data indicated that participants who received the efficacy-oriented messages were no more likely to receive diabetes-related intensification of care and routine care than those who received risk-oriented messages. Similarly, limiting the analysis to those with uncontrolled type 2 diabetes did not show that participants received improved processes of care. Satisfaction with care also was unaffected by participant condition.
Few studies have examined the use of computer-tailored messages to overcome clinical inertia in chronic disease management.28 The results, however, were still unexpected, given the consistently positive findings of similar interventions aimed at increasing preventive services utilization.29 There are a few possible explanations for these findings. First, the tailored message was provided only once, rather than repeatedly, as previous work has shown to be effective.30,31 Second, the intervention may not have been directive enough. The tailored messages used in this study were general and not specific in nature. Previous research on tailored messages has shown that patients need and desire more “directive” information.32,33 Perhaps the take-away message to ask their doctor for a needed test or increased dose of medication was lost within the additional educational content. Instead of the message, “Controlling blood pressure can be particularly helpful for people with diabetes. By keeping your blood pressure controlled, you can protect your eyes, heart, and kidneys. You can take simple and effective steps to keep your blood pressure under control,” we could have stated, “We see that your blood pressure is elevated. You should try to engage in cardiovascular activity for 20 minutes at least 3 times a week and also follow a healthy diet. These lifestyle changes will help to protect your eyes, heart, and kidneys.” In another study that used a similar Web-based intervention to overcome clinical inertia among patients with migraine, the intervention suggested specific questions to ask.28 It is possible, therefore, that without specific suggestions, patients are less able to translate what they learn into action during the doctor–patient interaction.
Third, the population examined in this study was different from previous populations examined. While the intervention has been shown to be successful in increasing preventive care procedures and changing adverse health behaviors in other studies, it may not have been successful in this study as a result of the change in population. Perhaps tailored messages are not effective quality improvement tools for individuals with chronic diseases such as diabetes. Further research is warranted to determine if this statement is accurate.
There are a few limitations to this study. The sample size of overall participants was small, and when participants were broken into and examined as subgroups, the sample sizes decreased further. As none of the analyses of outcome measures achieved statistical significance, it is possible that sample size may be at fault. For example, when examining the results of the 2 main outcome questions from the exit survey—about starting or modifying the dose of a diabetes medication—the control condition was the lowest of all 3 groups, yet for neither was the difference significant. It is possible that a larger sample size would have led to significant differences, but it is unlikely that these differences would have been clinically meaningful.
An additional limitation of the study findings was the use of self-reported data. Participant self-report as the sole method of data collection can be questionable due to its subjective nature. In measuring this type of clinical activity, authors have reported mixed results on the validity of self-report shortly after a doctor visit.34,35 Based on the findings of previous research, it is possible that this method of data collection underestimated the effectiveness of the intervention, as patients have a tendency to underreport services compared to direct observation.34 A recent study observed that, in most cases, doctors do tell patients about new medications they are starting. For example, when starting cardiovascular medications, providers mentioned that they were starting a cardiovascular medication 98% of the time, and mentioned the specific name of the medication 74% of the time.36 What is not known is how often doctors tell patients about dose adjustments, but the available evidence suggests that patients would underreport these changes, due either to doctors not telling them or to not remembering.
The finding that the tailored messages did not impact the care reported is surprising, based on previous research. However, there are several factors, as aforementioned, that may be responsible for the seemingly ineffectiveness of the intervention. Perhaps most important may be the content of the message.
Implications/Recommendations
One implication or recommendation is that tailored messages should provide a specific directive action for participants to follow (ie, explicit instruction to ask their physician questions about tests, medications, or treatment goals). Rather than “educating” patients with diabetes about the risks of high blood pressure or benefits of controlling their blood pressure, patients should receive a message “directing” them to ask their physician what they can do to lower their blood pressure. It is possible that the removal of extraneous information and the arming of patients with merely the appropriate questions to ask their physicians will lead to patient engagement in their care and an increase in guideline-based care. Given the success of these direct-to-consumer interventions11 and the sharp rise in consumer-directed health plans,37 effective patient-directed interventions to improve the quality of care are an area of great need.
Disclosures
This study was funded by a grant from the National Institutes of Health. Drs. Crawford, Rimal, and Sciamanna and Ms. Adams, Ms. Lee, and Ms. Janneck have no conflicts of interest or financial ties to disclose.
References
- 1.American Diabetes Association. Diabetes statistics. http://diabetes.org/diabetes-statistics.jsp http://diabetes.org/diabetes-statistics.jsp
- 2.Centers for Disease Control and Prevention. National Diabetes Fact Sheet: General Information and National Estimates on Diabetes in America, 2005. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2005. [Google Scholar]
- 3.American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2002;25:213–229. doi: 10.2337/diacare.25.1.213. [DOI] [PubMed] [Google Scholar]
- 4.Fleming B. Greenfield S. Engelgau M. Pogach L. Clauser S. Parrott M. The Diabetes Quality Improvement Project: Moving science into health policy to gain an edge on the diabetes epidemic. Diabetes Care. 2001;24:1815–1820. doi: 10.2337/diacare.24.10.1815. [DOI] [PubMed] [Google Scholar]
- 5.DeFronzo R. Pharmacologic therapy for type 2 diabetes mellitus. Ann Intern Med. 1999;131(4):281–303. doi: 10.7326/0003-4819-131-4-199908170-00008. [DOI] [PubMed] [Google Scholar]
- 6.Saaddine J. Engelgau M. Beckles G. Gregg E. Thompson T. Narayan K. A diabetes report card for the United States: Quality of care in the 1990s. Ann Intern Med. 2002;136:565–574. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 7.Chin M. Auerbach S. Cook S. Harrison JF. Koppert J. Jin L. Thiel F. Karrison TG. Narrand AG. Schaefer CT. Takashima HT. Egbert N. Chiu SC. McNabb WL. Quality of diabetes care in community health centers. Am J Public Health. 2000;90:431–434. doi: 10.2105/ajph.90.3.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nasr C. Hoogwerf B. Faiman C. Reddy S. United Kingdom Prospective Diabetes Study (UKPDS). Effects of glucose and blood pressure control on complications of type 2 diabetes mellitus. Cleve Clin J Med. 1999;66:247–253. doi: 10.3949/ccjm.66.4.247. [DOI] [PubMed] [Google Scholar]
- 9.Greenfield S. Kaplan S. Ware JJ. Yano E. Frank H. Patients' participation in medical care: Effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–457. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 10.Wagner E. Grothaus L. Sandhu N. Galvin MS. McGregor M. Artz K. Coleman EA. Chronic care clinics for diabetes in primary care: A system-wide randomized trial. Diabetes Care. 2001;24:695–700. doi: 10.2337/diacare.24.4.695. [DOI] [PubMed] [Google Scholar]
- 11.Kravitz RL. Epstein RM. Feldman MD, et al. Influence of patients' requests for direct-to-consumer advertised antidepressants: A randomized controlled trial. JAMA. 2005;293:1995–2002. doi: 10.1001/jama.293.16.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Glasgow R. Funnell M. Bonomi A. Davis C. Beckham V. Wagner E. Self-management aspects of the improving chronic illness care breakthrough series: Implementation with diabetes and heart failure teams. Ann Behav Med. 2002;24:80–87. doi: 10.1207/S15324796ABM2402_04. [DOI] [PubMed] [Google Scholar]
- 13.Wagner E. Chronic disease management: What will it take to improve care for chronic illness? Eff Clin Pract. 1998;1:2–4. [PubMed] [Google Scholar]
- 14.Kreuter MW. Wray RJ. Tailored and targeted health communication: Strategies for enhancing information relevance. Am J Health Behav. 2003;27:S227–S232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- 15.Campbell MK. DeVellis BM. Strecher VJ. Ammerman AS. DeVellis RF. Sandler RS. Improving dietary behavior: The effectiveness of tailored messages in primary care settings. Am J Public Health. 1994;84:783–787. doi: 10.2105/ajph.84.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prochaska JO. DiClemente CC. Velicer WF. Rossi JS. Standardized, individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychol. 1993;12:399–405. doi: 10.1037//0278-6133.12.5.399. [DOI] [PubMed] [Google Scholar]
- 17.Sciamanna CN. Gifford DR. Smith RJ. Design and acceptability of patient-oriented computerized diabetes care reminders for use at the point of care. Med Inform Internet Med. 2004;29:157–168. doi: 10.1080/14639230412331280413. [DOI] [PubMed] [Google Scholar]
- 18.Sciamanna CN. Goldstein MG. Marcus BH. Lawrence K. Pinto BM. Accuracy of recall of exercise counseling among primary care patients. Prev Med. 2004;39:1063–1067. doi: 10.1016/j.ypmed.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Sciamanna CN. Marcus BH. Goldstein MG. Lawrence K. Swartz S. Bock B. Graham AL. Ahern DK. Feasibility of incorporating computer-tailored health behaviour communications in primary care settings. Inform Prim Care. 2004;12:40–48. doi: 10.14236/jhi.v12i1.107. [DOI] [PubMed] [Google Scholar]
- 20.Stephenson MT. Witte K. Vaught C. Quick BL. Booth–Butterfield S. Patel D. Zuckerman C. Using persuasive messages to encourage voluntary hearing protection among coal miners. J Safety Res. 2005;36:9–17. doi: 10.1016/j.jsr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Glasgow R. Davis C. Funnell M. Beck A. Implementing practical interventions to support chronic illness self-management. Jt Comm J Qual Saf. 2003;29:563–574. doi: 10.1016/s1549-3741(03)29067-5. [DOI] [PubMed] [Google Scholar]
- 22.Glasgow R. Nutting P. King D. Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care. 2005;28:33–39. doi: 10.2337/diacare.28.1.33. [DOI] [PubMed] [Google Scholar]
- 23.Glasgow R. Toobert D. Brief, computer-assisted diabetes dietary self-management counseling: effects on behavior, physiologic outcomes, and quality of life. Med Care. 2000;38:1062–1073. doi: 10.1097/00005650-200011000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Glasgow R. Toobert D. Hampson S. Noell J. A brief office-based intervention to facilitate diabetes dietary self-management. Health Educ Res. 1995;10:467–478. doi: 10.1093/her/10.4.467. [DOI] [PubMed] [Google Scholar]
- 25.National Committee for Quality Assurance. Health Plan Employer Data and Information Set (HEDIS 3.0) Washington DC: National Committee for Quality Assurance; 1998. [Google Scholar]
- 26.American Diabetes Association. Standards of care for patients with diabetes mellitus. Diabetes Care. 2000;23:1514–1522. [Google Scholar]
- 27.Rubin HR. Gandek B. Rogers WH. Kosinski M. McHorney CA. Ware JE., Jr Patients' ratings of outpatient visits in different practice settings. Results from the Medical Outcomes Study. JAMA. 1993;270:835–840. [PubMed] [Google Scholar]
- 28.Sciamanna CN. Nicholson RA. Lofland JH. Manocchia M. Mui S. Hartmann CW. Effects of a website designed to improve the management of migraines. Headache. 2006;46:92–100. doi: 10.1111/j.1526-4610.2006.00312.x. [DOI] [PubMed] [Google Scholar]
- 29.Stone E. Morton S. Hulscher M. Maglione MA. Roth EA. Grimshaw JM. Mittman BS. Rubenstein LV. Rubenstein LZ. Shekelle PG. Interventions that increase use of adult immunization and cancer screening services: A meta-analysis. Ann Intern Med. 2002;136:641–651. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 30.Rakowski W. The potential variances of tailoring in health behavior interventions. Ann Behav Med. 1999;21(4):284–289. doi: 10.1007/BF02895959. [DOI] [PubMed] [Google Scholar]
- 31.Strecher V. Kreuter M. Den Boer D. Kobrin S. Hospers H. Skinner C. The effects of computer-tailored smoking cessation messages in family practice settings. J Fam Pract. 1994;39(3):262–270. [PubMed] [Google Scholar]
- 32.Hartmann CW. Sciamanna CN. Blanch DC. Mui S. Lawless H. Manocchia M. Rosen RK. Pietropaoli A. A website to improve asthma care by suggesting patient questions for physicians: Qualitative analysis of user experiences. J Med Internet Res. 2007;9(1):e3. doi: 10.2196/jmir.9.1.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sciamanna CN. Clark MA. Diaz JA. Newton S. Filling the gaps in physician communication: The role of the Internet among primary care patients. Int J Med Inform. 2003;72:1–8. doi: 10.1016/j.ijmedinf.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 34.Stange KC. Zyzanski SJ. Smith TF. Kelly R. Langa DM. FLocke SA. Jaen CR. How valid are medical records and patient questionnaires for physician profiling and health services research? A comparison with direct observation of patients visits. Med Care. 1998;36:851–867. doi: 10.1097/00005650-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 35.Tisnado DM. Adams JL. Liu H. Damberg CL. Chen WP. Hu FA. Carlisle DM. Mangione CM. Kahn KL. What is the concordance between the medical record and patient self-report as data sources for ambulatory care? Med Care. 2006;44:132–140. doi: 10.1097/01.mlr.0000196952.15921.bf. [DOI] [PubMed] [Google Scholar]
- 36.Tarn D. Heritage J. Paterniti D. Hays R. Kravitz R. Wenger N. Physician communication when prescribing new medications. Arch Intern Med. 2006;166:1855–1862. doi: 10.1001/archinte.166.17.1855. [DOI] [PubMed] [Google Scholar]
- 37.Rosenthal M. Hsuan C. Milstein A. A report card on the freshman class of consumer-directed health plans. Health Aff(Milwood). 2005;24:1592–1600. doi: 10.1377/hlthaff.24.6.1592. [DOI] [PubMed] [Google Scholar]