Abstract
Objectives
Hot flushes and night sweats (HF/NS) are experienced by 60–70% of menopausal women and are problematic for approximately 20–25%. Potential health risks associated with hormone-replacement therapy (HT) have led to a significant decline in HT use. There is therefore a need for safe, effective and evidence-based alternative treatments for menopausal symptoms. Previous exploratory work suggests that cognitive–behavioural therapy (CBT) is acceptable and effective for women with HF/NS during natural menopause and following breast-cancer treatment. This randomised controlled trial compares the effectiveness of Group CBT and Guided Self-Help CBT with no treatment control in reducing HF/NS Problem Rating and Frequency at post-treatment (main outcome) and at 6 months postrandomisation.
Methods and analysis
120 women, with 10 or more HF/NS a week for a month, are recruited from GP surgeries and the local community of South London. They are randomised to either 4 weeks of Group CBT, 4 weeks guided Self-Help CBT or no treatment control. Participants attend a clinical interview, and complete baseline questionnaire measures of HF/NS Problem Rating and Frequency (primary outcomes), mood, quality of life, self-esteem, hot-flush beliefs and behaviours, optimism and somatic amplification, and undergo 24 h sternal skin conductance monitoring (SCC—physiological measure of HF/NS) (secondary outcomes). Post-treatment measures (SSC, questionnaires and use of medical services) are collected 6–8 weeks later and follow-up measures (questionnaires and a use of medical services measure) at 6 months postrandomisation.
Ethics and dissemination
Ethical registration was granted by King's College London Research Ethics Committee (ref: PNM/08/09-42). All participants provide written informed consent. If treatment is successful, a Group CBT training manual and training sessions for health professionals, and a Self-Help CBT book will be published. Other CBT delivery options will also be examined (including Computerised Self-Help CBT and Group CBT workshops).
Clinical Trial Registration Number
ISRCTN57302613.
Keywords: Reproductive medicine, protocols & guidelines, clinical trials, psychology, breast tumours
Article summary
Article focus
There is a need for safe and effective, non-hormonal treatments for menopausal symptoms, that is hot flushes and night sweats.
This protocol paper outlines the design of a randomised controlled trial of self-management psychological interventions for menopausal hot flushes and night sweats.
The RCT aims to evaluate the effectiveness of Group Cognitive Behaviour Therapy (CBT) and Self-Help CBT versus no treatment control in managing frequency and problem rating of hot flushes and night sweats.
Key messages
This is a trial protocol.
The study is the first study to use both self-report and physiological measures to examine the effectiveness of two forms of CBT for menopausal symptoms.
If this treatment is successful, the interventions can be made widely available to women using manualised training sessions for health professionals, publication of the self-help book and educational sessions for women.
Strengths and limitations of this study
Strengths: the study uses both self-report and physiological outcome measures, and aims to recruit a diverse sample of menopausal women from a range of backgrounds.
Limitations: may recruit women with only very severe hot flushes, thereby reducing generalisability to menopausal women or the population as a whole.
Introduction
Menopausal symptoms—hot flushes and night sweats (HF/NS)—are experienced by 60–70% of women in Western cultures, and are troublesome for approximately 20–25% who seek medical help.1 Hormone-replacement therapy (HT) is an effective treatment for HF/NS, but there are concerns about its safety following the publication of prospective trials2 3 associating HT use with increased risks of breast cancer and stroke. As a result, HT use has fallen in the UK from 30 to 10% between 2002 and 2005.4 Many women prefer non-medical treatment options for these symptoms,5 and consequently there is an urgent need for the development of safe, acceptable and effective non-medical treatments to help women to manage menopausal symptoms.6
The aetiology of HF/NS is not clearly understood, but they appear to be associated with the rate of change in plasma oestrogen, which influences the thermoregulatory system via the hypothalamus.7 Hot flushes are also more prevalent following rapid withdrawal of oestrogen—for example, following surgical menopause or adjuvant chemotherapy for breast cancer.8 Alterations in oestrogen levels (but not absolute oestrogen levels) and neurotransmitters, such as norepinephrine and serotonin, and their subsequent impact on thermoregulatory homeostasis, have been widely implicated in the pathogenesis of HF/NS.9–11 Freedman12 proposes that there is a narrowed thermoneutral zone in women who have HF/NS, suggesting that small elevations in core body temperature such as changes in ambient temperature or other environmental triggers can activate HF/NS.13 14 There is some evidence that the thermoneutral zone is narrowed by elevated brain norepinephrine12 15 and general levels of stress.14 Hot flushes are often associated with social embarrassment, anxiety, discomfort and reduced health-related quality of life,16 whereas night sweats are associated with sleep problems and fatigue.
Non-medical treatments such as complementary therapies are popular, but in many cases there is insufficient evidence to support their efficacy.17–19 Non-hormonal medical treatments such as Clonidine, Megace and Venlafaxine (SSRI) have been found to be effective but are associated with side-effects.20 21 In contrast, there is some evidence that relaxation therapy and paced breathing can reduce HF/NS.22 23 Anxiety and negative thoughts, associated with embarrassment, feeling out of control and being unable to cope, have also been associated with more frequent and problematic HF/NS.24 25 Hunter and Liao26 developed a four-session cognitive behavioural treatment (CBT), which included psycho-education, paced breathing and relaxation to reduce stress and cognitive behavioural therapy to help women manage HF/NS.5 26 In an initial study using a patient preference design (no treatment vs HT vs CBT), CBT and HT resulted in 50% reduction in hot-flush frequency, whereas there were no significant changes in the no-treatment group. These findings were replicated in a pilot study using CBT delivered in small groups27 and in a recent exploratory trial of Group CBT for breast-cancer-treatment-related menopausal symptoms.28 However, this form of CBT has not yet been evaluated for HF/NS. A recent systematic review of psychosocial interventions for HF/NS concluded that while psycho-educational interventions are acceptable for HF/NS, further evaluation of treatment effects in high-quality randomised controlled trials are required.29
The use of self-help methods can be a cost-effective way of delivering treatments that have limited availability.30 Guided self-help can also address some of the drawbacks previously fielded at self-help interventions (ie, lack of social context/social support and incorrectly completed tasks). In a recent systematic review, guided self-help treatments were found to be comparable with face-to-face treatments for depression and anxiety disorders.31
Evaluating treatment efficacy depends on valid and reliable measures of HF/NS. Self-report measures include daily diaries recording frequency and severity of HF/NS and validated scales such as the Hot Flush Rating Scale,32 or electronic event markers. Sternal skin conductance (SSC) monitoring is considered to be the most valid physiological index of HF/NS.33 The sweat response seen in HF/NS produces a sudden increase in skin conductivity which tails off (ie, like a swishy tail). The use of both subjective and physiological measures can increase our understanding of the impacts of interventions.34 CBT may influence physiological hot flushes, women's perceptions of hot flushes or both. Twenty-four-hour SSC hot-flush monitoring has not yet been used to evaluate menopausal treatments in the UK, but it has been piloted and is acceptable to women.35 36 Hunter and Mann34 developed a cognitive model of HF/NS that explains how cognitive and behavioural changes might impact on HF/NS. For example, stress and stimulants (such as caffeine) may potentiate HF/NS in symptomatic women, and HF/NS may be more distressing or interfering when they are associated with negative thoughts such as embarrassment, social anxiety and feeling out of control.34
Current study
This trial aims to evaluate the effectiveness of Group CBT and Self-Help CBT to alleviate HF/NS in women seeking help for menopausal symptoms. It will compare Group CBT with no treatment (control) and Self-Help CBT with no treatment (control) in a randomised controlled trial, with a 6-month follow-up. It is the first UK trial to evaluate menopause treatments using both physiological (SSC)35 36 and self-report measures of HF/NS.
Specific hypothesis include:
Group CBT and Self-Help CBT will be more effective than no treatment in reducing HF/NS Problem Rating (primary outcome) and Frequency at post-treatment.
Group CBT and Self-Help CBT will be more effective than no treatment in reducing HF/NS Problem Rating and Frequency at 6 months postrandomisation.
Group CBT and Self-Help CBT will be more effective than no treatment in reducing physiological HF/NS at post-treatment.
Additional analyses will examine the effects of Group CBT and Self-Help CBT on mood and quality of life and possible moderators (optimism and somatic amplification) and mediators (SSC, mood, beliefs and behaviours).
King's College London Research Ethics Committee approval has been granted (Psychiatry, Nursing and Midwifery Research Ethics Subcommittee, ref: PNM/08/09-42). The trial is registered with Current Controlled Trials (ISRCTN57302613).
Methods and analysis
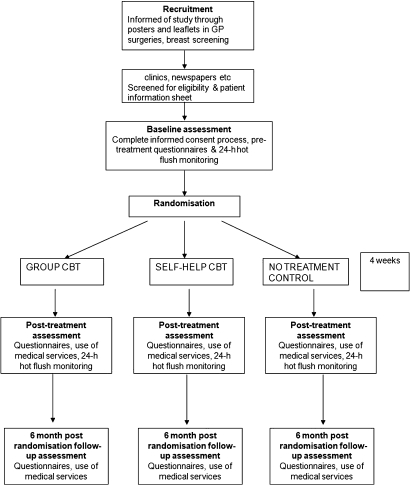
The study design and participant recruitment (completed May 2010) are shown in figure 1. Participants are block-randomised to receive either no treatment (access to GP support) or four weekly sessions of Group CBT (herein referred to Group CBT) or a 4-week guided Self-Help CBT Booklet (herein referred to as Self-Help CBT). The Group CBT was developed from previous work and an exploratory trial,26 28 and is specified in a treatment manual. Group CBT is delivered by a clinical psychologist but is designed to be delivered by appropriately trained and supervised health professionals. Post-treatment assessment is conducted 6–8 weeks postrandomisation (1–3 weeks after 4 weeks of treatment). Follow-up assessment is conducted 6 months postrandomisation. The primary outcome is Problem Rating of HF/NS (Hot Flush Rating Scale—HFRS)32 at post-treatment assessment.
Figure 1.
Description of the overall trial design. CBT, cognitive–behavioural therapy.
Group and Self-Help CBT will be compared with the control group separately, based on identical assumptions. A total sample size of 120, 40 in each group, will have 90% power to detect a clinically relevant difference in a mean HF/NS Problem Rating of 2 points26 controlling for baseline value (estimated to have a mean of 5 and SD of 2.4), a correlation between baseline and post-treatment values of 0.4 (giving a correction factor of 0.84)37 and a 5% two-sided significance level.
Study sample and recruitment
One hundred and twenty participants will be recruited from posters and leaflets placed in South London GP surgeries, menopause and breast-screening clinics, a menopause website (Menopause Matters) and newspaper advertisements over an 18-month period from March 2009 to May 2010. Women opt into the study by returning a tear-off slip on the leaflet or through websites, phone or email.
Inclusion criteria:
English-speaking women;
aged 18+;
have had problematic HF/NS for at least 1 month (minimum frequency of 10 or more a week).
Women are excluded if they cannot understand English or if they are currently undergoing psychiatric treatment (ie, their psychiatric problem is the main issue for them at the time).
Procedure
Women who opt in to the study are contacted by telephone for a screening interview. A researcher conducts an eligibility check using the above criteria and explains the study, the three arms of the trial and the randomisation process. Those eligible are sent a participant information sheet, consent form, sociodemographic questionnaire and an appointment for the baseline assessment. The consent process is completed at the assessment appointment, whereby the researcher summarises the information in the participant information sheet and responds to questions about the study. Participants then provide written consent. The researcher then conducts a clinical interview covering medical history including mental health issues, menopause symptoms and treatments used, concomitant medication and therapy use, and current life concerns. Participants are given a questionnaire to complete, assessing HF/NS frequency and problem rating, beliefs about HF/NS, health-related quality of life, body-image satisfaction, self-esteem, stress, dispositional optimism and somatic amplification. After checking that the participant has no allergy to adhesive dressings (eg, plasters) and does not wear a pacemaker, the SSC hot flush monitor is fitted. Participants are given a magnet event marker, worn on a bracelet, and a 24 h hot-flush diary. They mark the experience of a HF/NS by passing the magnet over the monitor and noting the time and severity of the HF/NS in the diary. Participants wear the monitor for 24 h, carrying out their usual daily activities and removing the monitor only to shower or bathe.
Randomisation
Women are randomised in blocks of 18–30, when sufficient participants have been assessed at baseline to enable group sizes of six to 10 participants in each arm. Participant IDs are inputted into an internet randomisation site and individually randomised to the three treatment arms in the ratio 1:1:1 by the trial coordinator. Within 2 weeks of randomisation, participants are informed of their group allocation, and the clinical psychologist (who delivers the CBT treatment) arranges appointments to deliver the treatments. Assessments take place in the Health Psychology department of King's College London at Guy's Hospital. They are conducted by the trial coordinator and a research assistant who, for practical reasons, are not blind to group allocation. Analysis is conducted by the trial statistician, who is blind to group allocation.
Participants in the Group CBT treatment arm attend 2 h sessions of Group CBT, once a week for 4 weeks. Women in the Self-Help CBT arm attend one introductory session with the clinical psychologist (to receive the booklet and discuss the treatment), and complete the booklet over 4 weeks, receiving a ‘guiding’ telephone call from the clinical psychologist 2 weeks into treatment. Participants can also contact the psychologist for unscheduled guidance during the treatment phase. Women from all three arms attend post-treatment assessments in the 2 weeks following the treatment phase (see figure 1). All participants are interviewed about their use of health services and treatments, as well as any changes to lifestyle and health during the treatment phase. They complete post-treatment questionnaires and repeat 24 h SSC hot-flush monitoring. Six months after randomisation, all participants complete a follow-up questionnaire identical to the post-treatment questionnaire, plus use of health services and treatments, and changes in employment, lifestyle and health over the previous 4 months since post-treatment assessment.
Group CBT
Group CBT is interactive and psychoeducational, with a focus on helping participants to develop strategies to reduce stress, apply paced breathing, and cognitive and behavioural strategies during HF/NS (see Hunter et al,28 and Hunter and Mann34 for detailed descriptions of the components of CBT for HF/NS). Sessions include information and discussion, individual goal-setting and problem-solving, relaxation/paced-breathing practice (using a CD) and homework. Each session takes place at the Health Psychology department of King's College London at Guy's Hospital and is run according to a protocol set out in a treatment manual, including presentation slides and handouts. A clinical psychologist has been trained to deliver the treatment, and assistants also are trained to assist in the groups. Sessions are audio-taped, and an independent psychologist, experienced in cognitive behavioural therapy, rates 10% of the sessions for adherence to protocol using a coding sheet created for the purpose.
Self-Help CBT
Self-Help CBT comprises four weekly sessions of approximately 1 h. The approach and sessions are identical to that of Group CBT, with participants receiving a Self-Help CBT booklet and relaxation/paced breathing CD and the same homework tasks each week. The booklet includes interactive exercises with space for participants to write relevant information. A clinical psychologist trained in the delivery of the treatment provides an information session at the beginning of treatment. Participants are provided with the psychologist's contact details for assistance during the 4-week programme. Two weeks into treatment, participants receive a telephone call from the clinical psychologist to provide support and discuss their individual treatment goals.
Session 1 aims to engage participants by introducing them to the CBT model of HF/NS.34 They are informed about physiological, cognitive, behavioural and emotional components of HF/NS within an overall CBT model of menopausal symptoms and complete tasks on stressful thinking and problem-solving techniques. Full body relaxation and paced breathing (slow, deep and even breathing with attentional focus on the breath) are introduced, and participants practice relaxation for homework.
Session 2 introduces cognitive and behavioural aspects of hot flushes. Participants revisit the CBT model, and information about psychological processes contributing to distress during a hot flush is introduced. Participants complete tasks on thinking and behaviour during hot flushes and problem-solve their unhelpful thoughts. Paced breathing and cognitive behavioural strategies to alleviate HF are discussed.
Session 3 focuses on sleep and night sweats. Participants are taught the mechanisms of sleep and cognitive processes that influence subjective judgements of sleep to address unhelpful cognitions, behaviours and anxieties about sleep.
Session 4 reviews the overall model and goals of the previous 3 weeks. Participants write their individual maintenance plan.
No-treatment control
Control participants do not receive CBT treatment but have access to their GP and other healthcare options. Treatments and services accessed during the treatment phase are logged at post-treatment assessment. The control group are offered a form of CBT off-trial at the end of the trial.
Measures
Sociodemographics
Sociodemographic variables include age, height, weight, ethnicity, number of children, education, marital status, employment status, smoking, drinking and exercise. Menopausal status (as defined by the Stages of Reproductive Aging Workshop),38 use of treatments for menopause and concomitant medications and therapies are also recorded in table 1.
Table 1.
Study measures
| Phase | A0 baseline assessment | Treatment phase | A1 post-treatment assessment | A2 follow-up assessment |
| Interview measures | ||||
| Medical history, menopause symptoms, concomitant medications and therapies | X | |||
| Questionnaire measures | ||||
| Weekly diaries | X* | |||
| Demographics: age, BMI, ethnicity, parity, marital status, education, employment, smoking, drinking, exercise | X | |||
| Hot Flush Rating Scale | X | X* | X | X |
| Menopause representations questionnaire | X | X | X | |
| Hot Flush Beliefs Scale | X | X | X | |
| Women's health questionnaire | X | X | X | |
| Rosenberg's Self-Esteem Scale | X | X | X | |
| Multidimensional Body Self Relations Questionnaire | X | X | X | |
| Perceived Stress Scale | X | X | X | |
| Somatic Amplification Scale | X | X | X | |
| General Health Survey Short Form 36 | X | X | X | |
| Life Orientation Test | X | |||
| Use of services | X | X | ||
| CBT session evaluation | X* | |||
| 24 h monitoring | ||||
| Sternal skin conductance | X | X | ||
| 24 h diary | X | X | ||
Completed each week for 4 weeks by those randomised to group cognitive–behavioural therapy (CBT) and Self-Help CBT only.
Primary outcome: hot-flush problem-rating
Hot-flush problem-rating is a subscale of the Hot Flush Rating Scale,32 calculated as the mean of three items, each measured on a 10-point scale (low to high). Items include ‘To what extent do you regard your flushes/sweats as a problem?’; ‘How distressed do you feel about your hot flushes?’ and ‘How much do your hot flushes interfere with your daily routine?’
Secondary outcomes
Hot-flush frequency and severity are assessed using the following measures:
Hot Flush Rating Scale: frequency subscale
The frequency subscale of the HFRS is a retrospective recording of the number of HF/NS experienced in the previous week—for example, ‘How often have you had hot flushes in the past week?’ The average severity of HF/NS over the previous week is estimated for hot flushes and for night sweats separately (1=mild, 2=moderate and 3=severe).32
Twenty-four-hour hot-flush diary
Women monitor their HF/NS prospectively for 24 h. When they experience a hot flush or night sweat they note down the severity (1=mild, 2=moderate and 3=severe) and the time at which it occurred.
Twenty-four-hour ambulatory SSC and event marker
During the 24 h diary monitoring period, women wear an ambulatory SSC monitor.39 The monitor is approximately 6×6 cm, with two 8 cm electrodes attached to an adhesive electrode patch by press studs. This electrode patch is attached to the sternum, two inches below the sternal notch, and holds the monitor close to the body. Skin conductance is measured by passing a pulse through the electrodes every 5 s, indicated by a green flash of an LED on the monitor. A hot flush is defined by an increase in conductance of 2 mmhos or more in 30 s, occurring no less than 15 min since the last SSC-defined HF/NS (ie, a 15 min lock-out period).40 For each SSC-defined hot flush or night sweat, the SSC level and the time at which it occurred are extracted for analysis. Women indicate that they are experiencing an HF/NS by passing a magnet near to the monitor. The magnet is worn on a bracelet. The times at which the magnetic event marker is registered are summed to produce a 24 h HF/NS subjective frequency.
Health-related quality of life
General physical and mental health are indexed using the General Health Survey Short Form 36 (SF-36),41 a widely used 36-item health survey. Nine physical- and mental-health summary scales are constructed, with a possible range from 0 to 100, where higher scores indicate better health.42
Perceptions of physical and emotional symptoms are measured using the Women's Health Questionnaire,43 which is standardised on samples of mid-aged women. The WHQ contains 36 items, which are scored on four-point scales. Nine subscales are formed by counting the number of items scoring 2 or 3 and dividing by the number of items for each scale, resulting in scales from 0 to 1. The WHQ has been widely used to evaluate interventions for menopausal symptoms.44
Process measures
Beliefs about HF/NS
HF/NS beliefs were measured using the Hot Flush Beliefs Scale,25 a 27-item scale comprising three subscales including beliefs about HF in a social context, beliefs about ability to deal with HF, and beliefs about night sweats and sleep. An additional scale is included, assessing behavioural reactions to HF/NS (avoidance, safety behaviours and positive acceptance).
Perceived stress
The Perceived Stress Scale45 measures 14 items, on a scale from 0 (never) to 4 (very often). Items are summed to form a scale from 0 to 56, where 0 is low stress, and 56 is high stress.
Somatic amplification
Barsky, Grace and Klerman's Somatic Amplification Scale46 is a 10-item scale measuring a general tendency towards body focus, including items such as ‘When someone else coughs, it makes me cough, too’ (1=not like me to 5=very much like me). The mean for the items is calculated to give a five-point scale, where 5 is high somatic amplification.
Dispositional optimism
The Revised Life Orientation Test (LOT-R)47 measures dispositional optimism on an eight-item scale including ‘In uncertain times, I usually expect the best’ (0=strongly disagree to 4=strongly agree). Items are summed to give a total score ranging from 0 to 32, where high scores indicate higher dispositional optimism.
Self-esteem
Rosenberg's Self-Esteem Scale48 measures perceived self worth on a 10-item scale. Items are scored 1–4 in the direction of negative self-esteem, and scores are summed to give a total self-esteem score ranging from 10 to 40.
Body image
The Multi-Dimensional Body Self Relations Questionnaire—Appearance Subscale (MBSRQ-AS)49 is a 34-item measure which assesses attitudes towards ones body. It has five subscales—appearance orientation, appearance evaluation, overweight preoccupation, self-classified weight and the body areas satisfaction scale—and includes items such as ‘most people would consider me good-looking.’ Items are presented on a five-point scale, from 1=definitely disagree to 5=definitely agree, and means are calculated for the different subscales.
Menopause representation questionnaire
The Menopause Representations Questionnaire (MRQ)50 is a 37-item measure designed to assess women's cognitive representations (general beliefs) of the menopause with respect to identity, consequences, time-line and control/cure. Items are scored on a 5-point scale from strongly agree to strongly disagree (5–1). The identity subscale is scored from 0 to 2. The mean scores are calculated for the subscales.
Treatment evaluation
Participants randomised to Group CBT and Self-Help CBT are asked to rate the specific elements of the intervention and the sessions/booklet overall. Use of the relaxation CD, attendance and completion of homework are also being monitored for both treatment arms at each treatment week and through self-report on CBT evaluation forms. At follow-up, participants are interviewed by telephone or in person using open questions to ascertain their subjective evaluation of the treatments. This includes their perceptions of any symptom, cognitive or behavioural changes occurring during treatment or in the follow-up period, as well as their thoughts on the group sessions/self-help booklet and how well CBT treatment fits with their lifestyle. The interviews will be conducted, transcribed and analysed by an independent researcher using Interpretative Phenomenological Analysis.
Analysis
An analysis plan has been agreed (ie, prior to completion of data collection). A trial statistician carries out primary and secondary data analysis, and is blind to group allocation. Unless indicated, scales are calculated according to published scoring algorithms. All statistical tests are two-sided (level of significance=0.05). The outcome analyses are performed using the statistical software SPSS version 15.0. An intention-to-treat analysis of difference in Problem Rating HFRS between intervention and control groups (Group CBT vs no treatment or Self-Help CBT vs no treatment) is conducted using a linear mixed model, utilising fixed and random effects, allowing for the baseline measurements to control for pretreatment differences and clinically relevant covariates. Secondary outcomes at post-treatment are analysed similarly. Follow-up data at 6 months are also explored through linear mixed models utilising repeated-measures analyses, allowing simultaneous modelling of the two outcome time points. Mediation of treatment effects by hot-flush beliefs and behaviours, mood, self-esteem, body satisfaction, stress, quality of life and frequency of HF/NS defined by skin-conductance rises will be explored using a two-stage least-squares method.51 Moderation by optimism and somatisation is also tested using multiple-group modelling.52
Ethics and dissemination
Ethical and safety considerations: some women consider the menopause a taboo subject and may be embarrassed about the topic of the questionnaires and CBT sessions (menopause, hot flushes, night sweats, etc). However, we ensure that all potential participants are fully informed about study materials prior to obtaining consent and that they are given the opportunity to withdraw from the study, should they feel uncomfortable. Women will also be randomised into three groups, two active treatment groups and one no-treatment group. Some participants may be disappointed that they are not receiving a potentially helpful treatment. However, we offer all no-treatment participants a form of the CBT intervention at the end of the trial. We also ensure that all participants are fully aware of the randomisation procedure prior to obtaining informed consent.
The SSC monitor is attached to the skin with an adhesive electrode patch and operates with an event marker (a magnet on a bracelet). The adhesive electrode patch may cause irritation to those with skin allergies, and the magnet may interfere with a pacemaker. Participants will be asked if they have any skin allergies or a pacemaker prior to wearing the monitor. Those who do will not be asked to wear the monitor, and this will not exclude them from the study.
We hope to disseminate the study through conferences and journal publications. If the treatment is successful, we plan to produce a Group CBT training manual and training sessions for health professionals, publish the Self-Help CBT as a book and design a further study using a computerised version of Self-Help CBT, and hope to examine other delivery options for the intervention (guided vs unguided Self-Help CBT, workshops and 1 day, 2-day versions of Group CBT). If effective, these interventions will enable menopausal women with problematic HF/NS to easily access acceptable, safe alternative treatment options. These CBT-based interventions can also be used to enable women to stop using HT when this is indicated.
Supplementary Material
Acknowledgments
We would like to thank the NIHR Biomedical Research Centre for Mental Health, South London and Maudsley NHS Foundation Trust and the Institute of Psychiatry, King's College London for their support in this research.
Footnotes
To cite: Ayers B, Mann E, Hunter MS. A randomised controlled trial of cognitive-behavioural therapy for women with problematic menopausal hot flushes: MENOS 2 trial protocol. BMJ Open 2011;1:e000047. doi:10.1136/bmjopen-2010-000047
Funding: This work was supported by the NIHR Biomedical Research Centre for Mental Health, South London and Maudsley NHS Foundation Trust and the Institute of Psychiatry, King's College London: grant number PAXKAYT-BRC-PAXKAZI.
Competing interests: None.
Ethics approval: Ethics approval was provided by the King's College London Research Ethics Committee (Psychiatry, Nursing and Midwifery Research Ethics Subcommittee, ref: PNM/08/09-42).
Contributors: BA is the trial coordinator on the study and generated the first draft of this manuscript based on the study protocol; EM is the trial statistician and contributed to the analysis aspect of the protocol; MSH is the principal investigator of this study and wrote the original protocol and supervised the intervention.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Rymer J, Wilson R, Ballard K. Making decisions about hormone replacement therapy. BMJ 2003;326:322–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rossouw JE, Anderson GL, Prentice RL, et al. Writing Group for the Women's Health Initiative Investigators. Risks and benefits of oestrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomised controlled trial. JAMA 2002;288:321–33 [DOI] [PubMed] [Google Scholar]
- 3.Manson JE, Hsia J, Johnson KC, et al. Women's Health Initiative Investigators. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med 2003;349:523–34 [DOI] [PubMed] [Google Scholar]
- 4.Menon U, Burnell M, Sharma A, et al. UKCTOCS Group Decline in women using hormone replacement therapy at recruitment to a large screening trial in the United Kingdom. Menopause 2007;14:462–7 [DOI] [PubMed] [Google Scholar]
- 5.Hunter MS. Cognitive behavioural interventions for premenstrual and menopausal problems. J Reprod Infant Psychol 2003;21:183–94 [Google Scholar]
- 6.Utian WH. Psychosocial and socioeconomic burden of vasomotor symptoms in menopause: a comprehensive review. Health Qual Life Outcomes 2005;3:47–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ginsberg H, Hardiman P, O'Reily B. Peripheral blood flow in menopausal women who have hot flushes and those who do not. BMJ 1989;298:1488–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kronenberg F. Hot flashes: epidemiology and physiology. Ann N Y Acad Sci 1990;592:52–86; discussion 123–33. [DOI] [PubMed] [Google Scholar]
- 9.Berendsen HHG. Hot flushes and serotonin. Menopause Inter 2002;8:30–4 [Google Scholar]
- 10.Freedman RR. Pathophysiology and treatment of menopausal hot flashes: a contemporary approach to the menopause. Semin Reprod Med 2005;23:117–25 [DOI] [PubMed] [Google Scholar]
- 11.Mom CH, Buijs C, Willemse PH, et al. Hot flushes in breast cancer patients. Crit Rev Oncol Hematol 2006;57:63–77 [DOI] [PubMed] [Google Scholar]
- 12.Freedman RR. Hot flashes: behavioral treatments, mechanisms, and relation to sleep. Am J Med 2005;118(Suppl 12B):124–30 [DOI] [PubMed] [Google Scholar]
- 13.Gannon L, Hansel S, Goodwin J. Correlates of menopausal hot flushes. J Behav Med 1987;10:277–85 [DOI] [PubMed] [Google Scholar]
- 14.Swartzman LC, Edelberg R, Kemmann E. Impact of stress on objectively recorded menopausal hot flushes and on hot flush report bias. Health Psychol 1990;9:529–45 [DOI] [PubMed] [Google Scholar]
- 15.Freedman RR, Krell W. Reduced thermoregulatory null zone in postmenopausal women with hot flashes. Am J Obstet Gynecol 1999;181:66–70 [DOI] [PubMed] [Google Scholar]
- 16.Gupta P, Sturdee DW, Hunter MS. Mid-age health in women from the Indian subcontinent (MAHWIS): general health and the experience of menopause in women. Climacteric 2006;9:13–22 [DOI] [PubMed] [Google Scholar]
- 17.Kronenberg F, Fugh-Berman A. Complementary and alternative medicine for menopausal symptoms: a review of randomised controlled trials. Ann Intern Med 2002;137:806–13 [DOI] [PubMed] [Google Scholar]
- 18.Carroll DG. Nonhormonal therapies for hot flushes in menopause. Am Fam Physician 2006;73:457–64 [PubMed] [Google Scholar]
- 19.Borrelli F, Ernst E. Alternative and complementary therapies for the menopause. Maturitas 2010;66:333–43 [DOI] [PubMed] [Google Scholar]
- 20.Pandya KJ, Raubertas RF, Flynn PJ, et al. Oral Clonidine in postmenopausal patients with breast cancer experiencing tamoxifen-induced hot flashes: a University of Rochester Cancer Center Community Clinical Oncology Program study. Ann Intern Med 2000;132:788–93 [DOI] [PubMed] [Google Scholar]
- 21.Loprinzi CL, Michalak JC, Quella SK, et al. Megestrol acetate for the prevention of hot flushes. N Engl J Med 1994;331:347–52 [DOI] [PubMed] [Google Scholar]
- 22.Freedman R, Woodward S. Behavioral treatment of menopausal hot flushes: evaluation by ambulatory monitoring. Am J Obstet Gynecol 1992;167:436–9 [DOI] [PubMed] [Google Scholar]
- 23.Nedstrand E, Wijma K, Wyon Y. Applied relaxation and oral estrodiol treatment of vasomotor symptoms in postmenopausal women. Maturtitas 2005;51:154–62 [DOI] [PubMed] [Google Scholar]
- 24.Hunter MS, Rendall M. Bio-psycho-socio-cultural perspectives on menopause. Best Pract Res Clin Obstet Gynaecol 2007;21:261–74 [DOI] [PubMed] [Google Scholar]
- 25.Rendall MJ, Simonds LM, Hunter MS. The Hot Flush Beliefs Scale: a tool for assessing thoughts and beliefs associated with the experience of menopausal hot flushes and night sweats. Maturitas 2008;60:158–69 [DOI] [PubMed] [Google Scholar]
- 26.Hunter MS, Liao KLM. An evaluation of a four-session cognitive behavioural intervention for menopausal hot flushes. Br J Health Psychol 1996;1:113–25 [Google Scholar]
- 27.Keefer L, Blanchard EB. A behavioral group treatment program for menopausal hot flashes: results of a pilot study. Appl Psychophysiol Biofeedback 2005;30:21–30 [DOI] [PubMed] [Google Scholar]
- 28.Hunter MS, Coventry S, Hamed H, et al. Evaluation of a group cognitive behavioural intervention for women suffering from menopausal symptoms following breast cancer treatment. Psychooncology 2009;18:560–3 [DOI] [PubMed] [Google Scholar]
- 29.Tremblay A, Sheeran L, Aranda SK. Psychoeducational interventions to alleviate hot flashes: a systematic review. Menopause 2008;15:193–202 [DOI] [PubMed] [Google Scholar]
- 30.Gould RA, Clum GA. A meta-analysis of self-help treatment approaches. Clin Psychol Rev 1993;13:169–86 [Google Scholar]
- 31.Cuijpers P, Donker T, van Straten A, et al. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med 2010;40:1943–57 [DOI] [PubMed] [Google Scholar]
- 32.Hunter MS, Liao KL. A psychological analysis of menopausal hot flushes. Br J Clin Psychol 1995;34:589–99 [DOI] [PubMed] [Google Scholar]
- 33.Miller HG, Li RM. Measuring hot flashes: summary of a National Institutes of Health workshop. Mayo Clin Proc 2004;79:777–81 [DOI] [PubMed] [Google Scholar]
- 34.Hunter MS, Mann E. A cognitive model of menopausal hot flushes and night sweats. J Psychosom Res 2010;69:491–501 [DOI] [PubMed] [Google Scholar]
- 35.Hunter MS, Haqqani J. An investigation of subjective perceptions and physiological measures of hot flushes and night sweats. Climacteric. Published Online First: 2010. doi: 10.3109/13697131003735585 [Google Scholar]
- 36.Dormire SL, Carpenter JS. An alternative to Unibase/glycol as an effective nonhydrating electrolyte medium for the measurement of electrodermal activity. Psychophysiology 2002;39:423–6 [DOI] [PubMed] [Google Scholar]
- 37.Machin D, Fayers P, Pinol A. Sample Size Tables for Clinical Studies. Oxford: Blackwell Science, 1997 [Google Scholar]
- 38.Soules MR, Sherman S, Parrott E, et al. Executive summary: Stages of Reproductive Aging Workshop (STRAW). Climacteric 2001;4:267–72 [PubMed] [Google Scholar]
- 39.Webster J, Bahr D, Shults M, et al. A miniature sternal skin-attached hot flash recorder. In: Ibrahim F, Abu Osman JA, Usmann J, et al., eds. 3rd Kuala Lumpur International Conference on Biomedical Engineering. Berlin, Heidelberg: Springer, 2006:550–3 [Google Scholar]
- 40.Carpenter JS, Monahan PO, Azzouz F. Accuracy of subjective hot flush reports compared with continuous sternal skin conductance monitoring. Obstet Gynecol 2004;104:1322–6 [DOI] [PubMed] [Google Scholar]
- 41.Ware J, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Lincoln, RI: QualityMetric Incorporated, 1993:2000 [Google Scholar]
- 42.Ware J, Kosinski M. Sf-36 Physical & Mental Health Summary Scales: A Manual for Users of Version 1. 2nd edn Lincoln, RI: QualityMetric Incorporated, 2001 [Google Scholar]
- 43.Hunter MS. The Women's Health Questionnaire: a measure of mid-aged women's perceptions of their emotional and physical health. Psychol Health 1992;7:45–54 [Google Scholar]
- 44.Hunter MS. The Women's Health Questionnaire (WHQ): frequently asked questions (FAQ). Health Qual Life Outcomes 2003;1:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385–96 [PubMed] [Google Scholar]
- 46.Barsky AJ, Wyshak G, Klerman GL. The somatosensory amplification scale and its relationship to hypochondriasis. J Psychiatr Res 1990;24:323–34 [DOI] [PubMed] [Google Scholar]
- 47.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neurotiscism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol 1994;67:1063–78 [DOI] [PubMed] [Google Scholar]
- 48.Rosenberg M. Society and the Adolescent Self-Image (Reprint Edition). Middletown, CT: Wesleyan University Press, 1989 [Google Scholar]
- 49.Cash TF. Multidimensional Body Self Relations Questionnaire (MBSRQ). MBSRQ Users' Manual (Third Revision), 2000 [Google Scholar]
- 50.Hunter MS, O'Dea I. Development of the menopause representations questionnaire. Psychol Health Med 2001;6:65–76 [Google Scholar]
- 51.Emsley R, Dunn G, White IR. Mediation and moderation of treatment effects in randomised controlled trials of complex interventions. Stat Methods Med Res 2010;19:237–70 [DOI] [PubMed] [Google Scholar]
- 52.Byrne B. Structural Equation Modelling with AMOS: Basic Concepts, Applications, and Programming. Mahwah, NJ: Lawrence Erlbaum Associates, 2001 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.