Abstract:
Objectives
This article examines and evaluates the history of natural disasters in Oman and presents the health care response to cyclone Gonu, and highlights the health care lessons learnt from the Cyclone as narrated by frontline personnel and it puts forward some practical recommendations for health care policy makers in order to strengthen the health care disaster preparations to combat future natural and man-made disasters.
Methods
The lessons presented in this article are based on the reflections of frontline health care personnel who witnessed Cyclone Gonu. The reflections of experience collected as a part of a qualitative 17 semi-structured interviews conducted in Oman between December 2009 and January 2010.
Results
The study found that the lessons from passes events went by un-noticed and exposed some serious fragmentation in the coordination of different governmental sectors involved in emergency management and that there was no well-planned mechanism of alert and warning dissemination to people and communities.
Conclusion
Overall, the major lessons that learnt from Cyclone Gonu would have been very useful if they had been taken into consideration and implemented during the health care response to cyclone Phet.
Introduction
In June 2007, the Sultanate of Oman awoke to one of the worst natural disasters in its recent history. Cyclone Gonu, hit the country causing torrential rains and flash flood. The Cyclone claimed the lives of 49 people and left more than 20,000 others homeless. The infrastructure services of Oman were under unprecedented stress for days. Like all other services in the country, Gonu severely stretched health care services.
This article reviews the history of natural disasters in Oman and presents the health care response to cyclone Gonu. Furthermore, it documents the health care lessons learnt from Cyclone Gonu as narrated by frontline personnel and it puts forward some practical recommendations for health care policy makers in order to strengthen the health care disaster preparations to combat future natural or man-made disasters.
The literature of the history of natural disasters in Oman is very sparse, which is not uncommon among countries from the Arabian Peninsula.1 Arguably, the best record of international disasters comes from the International Disaster Database, Centre for Research on the Epidemiology of Disasters (CRED), School of Public Health of the Université Catholique de Louvain (UCL) in Brussels, Belgium. In 1980, the database became a well-established World Health Organization (WHO) project to compile and standardize the data collection of all international natural and man- made disasters. The history of natural disasters in the Sultanate of Oman documented in the CRED database is summarized in Table 1.2
Table 1. Natural disasters in the Sultanate of Oman from 1960 to 2010.
| Type of Disaster | Date | No killed | No affected | Cost in US $ |
|---|---|---|---|---|
| Storm | May 1977 | 105 | 5,048 | NA |
| Storm | June 1977 | 2 | 1.548 | NA |
| Storm | May 1981 | 26 | NA | NA |
| Storm | May 2002 | 7 | 83 | 50,000 3,900 |
| Storm | April 2003 | 30 | NA | 1000 |
| Storm | June 2007 | 76 | 20,000 | 3,900,000 |
| Storm | June 2010 | 24 | 10, 000 | NA |
*yet to be included in the CRED database*, NA = Not Available, *Note that the CRED database has a strict inclusion criteria.3
It is clear that storms are the most frequent natural disasters in the country. The worst storm in terms of fatality occurred in May 1977 in which 105 Omanis lost their lives. However, in terms of severity, number of people affected and the financial cost, Cyclone Gonu in 2007 topped the list. At the time of revising this article, Cyclone Phet struck the country, claiming 24 lives of which 21 were Omanis and three were expatriates.
A literature search using PubMed, Ovid search engines yielded no published studies about natural disasters in Oman. This emphasizes the issue that there is a severe scarcity of data on disasters and mass casualty incidents in Oman and other Arabian countries on this matter.1 Therefore, it is important to document health care response to disasters in order to learn from the precious experience.
The name Gonu is thought to originate from the language of the people of the Maldives and it means "a bag made from palm leaves." A tropical cyclone is formed by a combination of high temperature on the sea surface over 25ºC (77 F), high humidity and low spiralling winds with other divergent stronger winds. At the mature stage, the cyclone extends for hundreds of thousands of kilometres with a depressurized centre where an eye is formed which is surrounded by heavy clouds that cause torrential rains accompanied by strong gusty winds.4
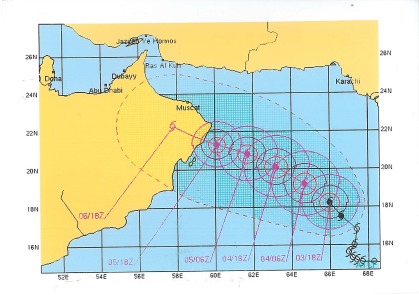
On the 27th of May 2007, satellite images showed a widespread convection which persisted in the south eastern of the Arabian sea and gradually intensified into a deep depression and later transformed into a cyclonic storm by June 2nd. By June 4th, the cyclone was in category five. The Cyclone, moved to the eastern coastline of Oman with wind speed of 260 km/hr and gust of 315 km/hr, with an estimated central pressure of 920 mBar while located about 285 km away from land at latitude 210 N and longitude 830 E. On June the 5th, it was downgraded to category four after maintaining peak winds for 9 hours. The cyclone hit the land later on June the 5th and after 24 hours the inner core of the cyclone weakened to a wind intensity of 95 km/hr. On June the 6th, it hit the eastern coastline of Oman as the strongest tropical cyclone ever to strike the Arabian Peninsula.5 The following diagram shows the route of the cyclone. (Fig. 1)
Figure 1.
Route of Cyclone Gonu, (with permission from Directorate General of Civil Aviation and Meteorology, Ministry of Transport and communications, Oman
The effect of cyclone Gonu began before the arrival of the actual cyclone. Seven hours before the centre of the cyclone hit the north-eastern coastline, the country was already experiencing the impact of rough winds, torrential rain falls reaching 24 inches (average 3.9 inch per annum) near the coastline leaving many areas flooded. Strong winds knocked down power lines and communication poles across the coastline of the country leaving thousands stranded and isolated. The most effected cities were Sur and the Capital City of Muscat where infrastructure facilities were severely damaged in the early hours of the event. (Fig. 1)
Muscat suffered loss of power cuts and communication for two days. There was a shortage of clean water supply. Table 2 summarizes the impact of Cyclone Gonu in Muscat.
Table 2. Estimated Impact of the Cyclone Gonu in Muscat6.
| Impact | Day 1 of Cyclone | Day 2 of Cyclone |
|---|---|---|
| Sheltered people | 67,120 people in 139 shelters | 2650 people in 4 shelters |
| Affected roads | 90% of all roads | 20% of all roads |
| Electricity cuts | 27% of the capital w/out power | 4% of the capital w/out power |
| Water supply | 23% of the capital | 7% of the capital w/out water |
| Affected (tel.) | 35% of network | 1% of network |
| Affected (mobiles) | 30% of network | 3% of network |
| Fatalities | 49 confirmed dead | 14 still missing |
49 people lost their lives directly due to the cyclone. The majority were expatriates from Indian sub-continent regions. They were mainly workers living in low-areas of the city which were subjected to flash flooding hours before the centre of the cyclone arrived. However, it is important to note that, this number of fatality does not take into account other people who died from exacerbation of chronic disease and could not get to health care facilities. Although the communication lines were not 100% affected during the event, the networks were all overwhelmed and inaccessible. Roads and bridges were washed out and major sites in the capital area were totally isolated and inaccessible for days. More than 2,000 people were airlifted from damaged areas and water was delivered by fishing boats to isolated towns near the coastline. Like all other public infrastructures, hospitals were flooded and cut off because of damaged roads. The Omani authorities have estimated the direct cost of the event to be US$ 4 billion. Despite the wonderful resilience of the Omani community and the heroic rebuilding after the cyclone, there are many lessons to be learnt.
Methods
The lessons presented in this article are based on the reflections of frontline health care personnel who witnessed Cyclone Gonu. The reflections of experience collected as a part of a qualitative 17 semi-structured interviews conducted in Oman between December 2009 and January 2010. The interviewees included a selected mix of acute care providers from Emergency Departments, Intensive Care Units from all secondary and tertiary level hospitals in Oman and from frontline personnel from the Royal Oman Police EMS system. The interviews were audio-recorded and fully transcribed. The transcripts were sent back to interviewees for approval and editing.
This article presents only the experience and lessons learnt from Cyclone Gonu as reflected from the interviewees answers to this question: "what are the lessons learnt from Cyclone Gonu in 2007?" The answers were qualitatively analyzed and categorized into seven common themes "lessons" using NVivo 8 © QRS International Pty Limited, MA, USA. Then for each lesson learnt, a recommendation was suggested by the interviewees.
Results
History is a dynamic and cyclical process and disasters are somewhat repeatable. On the 14th April 2003, the south of Oman was flooded by a tropical cyclone causing wide spread destruction of infrastructure and claimed the lives of 30 people.2 The lessons from that event passed by unnoticed. After the cyclone, people returned to their normal lives as if nothing had happened or will ever happen again. Looking at the disaster timeline in Oman, it seems that the country is hit by a strong cyclonic storm once in five years, however, the lessons learnt have not been taken into account and proper preparation measures are still lacking. This may be because of the widely accepted attitude of "what Allah (God) wishes to happen, will happen anyway." Ignoring the lessons that should be learnt from the history of disasters will be costly and render all preparation measures to be reactive rather than proactive. An emergency physician expressing the frustration stated the following: "I guess it is never thought of as something important. Although, we have had a history of a few major natural incidents but we seem not to learn from what we should have learnt. So our response will always be a reactive rather than a proactive, unless we consider the lessons learnt by our own disaster history." Another Intensive Care doctor said: "From Gonu, there are a lot of lessons we should learn, basically taking things seriously, and learning from our history in order to be well-prepared for the worse in the future." Cyclone Gonu exposed some serious fragmentation in the coordination of different governmental sectors involved in emergency management. Although, the National Civil Defence Committee was activated, it was a mere reactive move to an imminent cyclone.
The committee is a national-level committee which includes 16 members from different ministries in the government. They rarely meet other than when there is an imminent national disaster. Disasters require planning and proactive coordination. It is incomprehensible to expect different parties to work as a team during a crisis if they have never met each other beforehand. On a local level, there is still no effort to coordinate disaster preparatory activities across different community sectors and the situation is left to the affected community to deal with as the disaster unfolds. Cyclone Gonu has emphasized the need for robust communication and coordination between all key agencies of the emergency management team and more importantly, the coordination should take place during non-disaster times rather than on the day of the disaster starting from a local to regional to national level in a coordinated and graded pattern.
An executive director of one hospital reiterated the need for better coordination between health care providers and other agencies during emergency planning by stating:
"We should have a close liaison with ROP and civil defence and all other agencies who are involved in the mass casualty management with the objective of streamlining and strengthening the entire system in totality and gaps / lacunas if any identified should be corrected with appropriate feasible remedial measures for effective and efficient services."
One emergency doctor stated: "We did not know what to do when the Cyclone came here. We have no idea what doctors and nurses have to do and the families, and the community have to do. It was a total failure in terms of functional regional command. There was one regional command but was not functional on grass root level."
Also, the National warning system was active days before the cyclone arrived, however the dissemination of warning alerts to local people in remote villages and cities was inefficient. In some cities, the local people only realized there was something serious happening when the evacuation helicopter landed in their area to pick them up. Doctors in many peripheral hospitals were not alerted of the coming cyclone and the potential impact. An Emergency doctor stated that: "We did not receive any official news that the Cyclone will come here. Even if we did, I am not sure what I’m supposed to do." Therefore, there has to be a well-planned mechanism of alert and warning dissemination to people and communities.
During cyclone Gonu, hospitals were cut off and flooded. The national trauma centre was not accessible as were all other hospitals in the affected area. Also, a day before the cyclone, most health care facilities were stockpiling medications and expanding bed capacity in Emergency Departments and Intensive Care Units while neglected a fundamental understanding of the nature of flooding disasters and their health impact. Floods, as such, do not create a high number of injured victims, rather the majority of victims require basic needs such as shelter, food and clean drinkable water which many hospitals in Oman have failed to appreciate in preparation for the cyclone.7
An Executive director of one major hospital in Oman expressed how a fundamental hazard assessment before the building of the hospital was not conducted properly. The first floor of the hospital was underwater and not functional for 8 days following the cyclone. "One of the things we discovered during the cyclone is that the level of the hospital was planned to be higher than it is right now and also there has not been a proper risk assessment study before building the hospital."
Many interviewees indicated that their preparation was based on an invalid assumption that the cyclone will create a high volume of critically ill patients which was not the case. "So we were expecting a major inflow of patients. But actually luckily, that did not happen...." Stated an ICU doctor. "Number two, management of the staff, themselves, was poor and based on shaky assumptions. In a sense we posted all the staff at one time in to the Emergency Department, hoping that patients will come. Patients never turned up" commented an Emergency doctor.
An EMS personnel thought that "even with Gonu we had a lot of preparations but we did not have a lot of casualties per se. We were prepared and we had a lot of things that we could offer and do but we did not have the real disaster like injuries and things."
On the other hand, during the cyclone, many health care personnel were stranded inside hospitals and health clinics leaving their families at home. Communications were out of order for at least three days. Many doctors and nurses were not able to contact their families while they were on duty providing health care to victims of the cyclone. This situation along with the lack of planning to look after health care providers and their families led to a harsh conditions which many health care personnel found traumatizing.
An emergency doctor who spent three days stranded in hospital described the situation as follows: "We did not take much care of the doctors themselves or their families. The staff had to manage their own problems. There were no adequate supplies of food, water for the staff themselves, both in the hospital and in the campus. Sadly, there was nobody to care for that." Another ICU doctor stated, "I think there was a lot of psychological trauma for the staff, the doctors and everybody else, because we have never seen such a thing like the hospital getting flooded. We always thought of hospitals as very safe places."
Furthermore, the critical care services in most hospitals in Oman run on a high occupancy rate on a daily basis. Thus, any increase in patient influx will quickly lead to an activation of a disaster mode. This over-stretched situation of critical care services reduces the surge capability of the system very dramatically.
An ICU consultant expressed his concerns about the high occupancy rate of ICU services, "So we are usually in our occupancy on 90% rate, so we don’t need a disaster we are already in a crisis situation." Another ICU doctor said; "Our occupancy rate is about 70% most of the time, we have limited capacity and we currently have no plan on who we should discharge if things get tight." When asked how critical care services in Oman can expand their capacity, an Emergency Physician proposed to have an electronic national map of resources. "We should learn how much we have and we should map our resources, along the country. We should know what we have, and the capabilities of facilities."
Additonally, the country currently lacked a medical assistance team that could respond to disasters and Mass Casualty Incidents inside or outside the country.
Discussion
The study showed that past experiences went unnoticed and proper preparation measures were not implemented and are still lacking. The recommendation for this is to form a task force committee to conduct a comprehensive review of all the natural events in the country and the lessons learnt from each event. Ground-zero personnel have to be consulted about lessons learnt from their experiences. The Committee should have the authority to follow the implementations of the lessons to a satisfactory level.
Cyclone Gonu also exposed some serious disintegration between different governmental sectors involved in emergency management. Disasters of such scale require planning and proactive coordination. Disasters are unique situations in which many agencies play a role. Thus, unless the activities of each agency is coordinated by an overall executive authority then the efforts will be rendered ineffective. Clear lines of responsibility for each agency should be defined well in advance before the disaster strikes. Many of the doctors interviewed were concerned that there were no guidelines on what responsibilities to expect from each person during a disaster.
Since disasters are local events to start with, there must be a coordinating body on a local-level. This body must function during calm periods as well as during disaster situations. They must bring together different local agencies such as schools, hospitals, local civil defence, local police and local business owners. The local body should strive to adopt an active approach to disaster preparations rather than a reactive one. All local agencies should have clear delineated roles and responsibilities on what to do during a disaster.
In terms of the National Warning System, it is critical to involve the local leadership in the process of establishing alert mechanisms, as this will give extra weight and authority when the mechanism is activated. People in local communities have to be responsible for what they should do during an alert and this can be established by prior planning with local authorities.
The Ministry of Health emergency operation centre should have a list of all doctors and nurses working in all the hospitals so a mass alert can be initiated using modern technology such as text messages (SMS) or emails.
The impact of the cyclone has proven that the infrastructure of most health care facilities in Oman is vulnerable. Therefore, hazard vulnerability assessment has to be undertaken before embarking into the establishment of any health care facility in Oman. The local and environmental factors have to be factored into any planning. Also, a comprehensive hazard assessment for all existing hospitals will be valuable. The Ministry of Health has conducted a sample analysis using the World Health Organisation "Safer Hospitals" project. This move can be extended to all health care facilities in the country.
Basic understanding of the pattern of natural and man-made disasters is critical in order to base the planning process on a robust science rather than invalid assumptions. Planners and policy makers should consider the nature of the disaster, the local needs, and the available capabilities. It is essential to secure the basic needs first such as food, shelter and clean water rather than focusing entirely on high technology medical and surgical items. Disaster preparation is about securing basic and critical needs.
The results showed that many doctors and nurses were traumatized during the cyclone as they were cut-off from their families and were stranded in hospitals. Consequently, it is essential to develop a comprehensive plan to look after the welfare of health personnel during a disaster. There is an ethical and moral obligation of "reciprocal care" in which a health care system looks after the frontline personnel in order for them to provide the best possible care for victims. This was basically neglected in the current planning in Oman. This component has to be included in every hospital plan in the country so the health care personnel feel looked after as they look after the victims of disasters.
There was also no process to increase the national capacity of critical care services. A special funding process should be established to increase the capacity and capability of critical care services in Oman to cope with increased influx of victims during a disaster. At a local-level, each critical care facility should have measures in place to increase capacity such as a disaster discharge policy, and disaster admission criteria protocols.
Another neglected source of capacity in Oman was the private health care sector. All private sector organizations have to be included in disaster preparation measures especially as a source of critical equipment and space.
Additionally, the concept of an Omani Medical Assistance Team (OMAT) would be a valuable investment for the country. There is a search and rescue team under the Civil Defence, but the current team has limited scope of actual medical management of victims. Thus, OMAT will be a valuable asset for the medical community to expand its operations outside the premises of hospitals during a disaster as many hospitals were rendered inaccessible during Gonu.
Accordingly, an Omani Medical Assistance Team should be urgently formed. The ideal team should include a doctor, a nurse, a paramedic and a logistician. Members of the team should be intensively trained in disaster medicine and Mass Casualty Incident management. The team should be self-sufficient with all equipment (shelter, power, food, water, medical supplies and communications). Finally, a government agency such as the Ministry of Health or the Armed Forces services should take the initiative to form Oman Medical Assistance Team units.
Conclusion
Oman has a history of frequent tropical storms. Cyclone Gonu was the most devastating cyclone which claimed the lives of 49 people. Three years after the cyclone, we still have some lessons to learn and areas for further development in health care disaster management and preparation. At the time of revising this manuscript for publication, another tropical storm "Cyclone Phet" struck the country. It would have been useful if the lessons from Gonu had been taken into consideration during the health care response to Phet.
Overall, the major lessons learnt from Cyclone Gonu include; learning from past experiences, delineated responsibilities of local agencies during a disaster, forming strong and robust risk communication and alert dissemination, acquiring basic understanding of disasters and vulnerability assessments, developing mechanisms to look after health care personnel in th e aftermath of disasters, creating innovative new mechanisms to increase the surge capability of critical care services in Oman and finally, forming Oman Medical Assistance Team to respond to disaster situations nationally and internationally.
An emergency physician talking about the need for preparedness in acute care services stated "we have to be prepared. True disasters are rare but that does not justify not being prepared. So we better care before we cry."
Acknowledgments
This article is in memory of all those people whose their lives were cut short because of Cyclone Gonu. I would like to express my gratitude to all the doctors and paramedics who shared their experiences with me. There were no conflict of interest and no funding was received on this work.
References
- 1.Al-Madhari A, Elberier M. Trends and fatality of natural disasters in the Arab world. Disaster Prevention and Management 1996;5(2):27-35 . 10.1108/09653569610112899 [DOI] [Google Scholar]
- 2.Porfile C. Natural Disasters. Centre for Research on the Epidemiology of Disasters. [Database on the Internet] Brusseles, Beligum [1st April 2010]; Available from: http://www.emdat.be/country-profile.
- 3.International Disaster Database, Centre for Research on the Epidemiology of Disasters (CRED). [1st April 2010]; Available from: http://www.emdat.be/.
- 4.Fritz H, Blount C, Albusaidi F, Al-Harthy A. Cyclone Gonu Storm Surge in the Gulf of Oman. Indian Ocean Tropical Cyclones and Climate Change: 255-63.
- 5.Health Mo. Confronting Tropical Cyclone "Gonu". April-June 2007 ed. Sultanate of Oman: Ministry of Health; 2007.
- 6.Building National infrastructure in response to disasters "the Omani experience." Ret. Col Azhar Al-Kindi; 2008.
- 7.Briggs S, Brinsfield K. Advanced Disaster Medical Response Manual for Providers, Harvard Medical International Trauma & Disaster Institute. Boston: University Press; 2003. [Google Scholar]