Abstract
Background
Ileal pouch anal anastomosis (IPAA) to surgically manage ulcerative colitis may involve multiple separate surgical procedures, impacting treatment costs, length of stay in hospital, complication rates and patient outcomes, and there is currently no accepted standard of care regarding the number of stages that should be performed. The purpose of this study was to compare the practice patterns of Canadian and American colorectal surgeons regarding the surgical management of ulcerative colitis.
Methods
A questionnaire was mailed to all practisng fellows of the American Society of Colon and Rectal Surgeons (ASCRS) in Canada and the United States. Surgeons were asked to describe their typical practices for 3 clinical scenarios.
Results
Questionnaires were mailed to 40 Canadian and 873 American ASCRS fellows with response rates of 86% and 62%, respectively. In the case of a patient who has had a prior colectomy, who is not taking steroids and in whom a tension-free IPAA is possible, 44% of Canadian surgeons would perform IPAA alone and 56% would perform IPAA with a loop ileostomy. In contrast, only 26% of American surgeons would perform IPAA alone and 74% would perform IPAA with a loop ileostomy (p = 0.002). In the case of a patient who has not had previous surgery, who is taking 10 mg/day of prednisone and in whom a tension-free IPAA is possible, the majority of both Canadian and American surgeons would perform an IPAA with a loop ileostomy (93% and 89%, respectively, p = 0.06). In the case of a patient who has not had previous surgery, who is taking 40 mg/day of prednisone and in whom a tension-free IPAA is possible, 45% of Canadian surgeons would perform a subtotal colectomy with an end ileostomy compared with 14% of American surgeons (p < 0.001).
Conclusion
There are significant differences in the surgical management of ulcerative colitis between Canadian and American colorectal surgeons.
Abstract
Contexte
L’anastomose iléo-anale avec poche (AIAP) pour traiter chirurgicalement la colite ulcéreuse peut comporter de multiples interventions chirurgicales distinctes, ce qui a un effet sur les coûts du traitement, la durée du séjour à l’hôpital, les taux de complication et les résultats pour les patients. Il n’y a actuellement pas de norme de soins acceptée en ce qui a trait au nombre d’étapes à suivre. Cette étude visait à comparer les tendances de la pratique des spécialistes canadiens et américains de la chirurgie colorectale en ce qui a trait au traitement chirurgical de la colite ulcéreuse.
Méthodes
On a envoyé un questionnaire par la poste à tous les associés actifs de la Société américaine des chirurgiens du côlon et du rectum (American Society of Colon and Rectal Surgeons — ASCRS) au Canada et aux États-Unis. Les chirurgiens devaient décrire leur pratique habituelle dans 3 scénarios cliniques.
Résultats
Les questionnaires ont été envoyés par la poste à 40 associés canadiens et 873 associés américains de l’ASCRS et les taux de réponse ont atteint 86 % et 62 % respectivement. Dans le cas d’un patient qui a déjà subi une colectomie, qui ne prend pas de stéroïdes et qui peut subir une AIAP sans tension, 44 % des chirurgiens canadiens pratiqueraient une AIAP seulement et 56 % conjugueraient l’AIAP à une iléostomie en boucle. Par ailleurs, 26 % seulement des chirurgiens américains pratiqueraient une AIAP seulement et 74 % conjugueraient l’AIAP à l’iléostomie en boucle (p = 0,002). Dans le cas d’un patient qui n’a pas subi d’intervention chirurgicale auparavant, qui prend 10 mg/jour de prednisone et qui peut subir une AIAP sans tension, la majorité des chirurgiens canadiens et américains pratiqueraient une AIAP avec iléostomie en boucle (93 % et 89 % respectivement, p = 0,06). Dans le cas d’un patient qui n’a pas déjà subi d’intervention chirurgicale, qui prend 40 mg/jour de prednisone et qui peut subir une AIAP sans tension, 45 % des chirurgiens canadiens, comparativement à 14 % des chirurgiens américains (p < 0,001) pratiqueraient une colectomie partielle conjuguée à une iléostomie terminale.
Conclusion
Il existe des différences importantes entre les chirurgiens du côlon et du rectum du Canada et des États-Unis pour ce qui est du traitement chirurgical de la colite ulcéreuse.
Ileal pouch anal anastomosis (IPAA) is the procedure of choice for most patients with ulcerative colitis who require surgery. Depending on the indication for surgery, patient factors and surgeon preference, IPAA may involve 1, 2 or 3 separate surgical procedures. The number of procedures performed may have implications regarding overall treatment costs, length of stay in hospital, complication rates and patient outcomes.1–5 There are limited data available to indicate which treatment approach is optimal, and there is no accepted standard of care regarding the number of stages that should be performed. Previous studies have reported that there are differences in clinical practice between Canadian and American physicians.6–11 However, there are few data comparing general surgical practice patterns between the 2 countries. The purpose of this study was to compare the practice patterns of Canadian and American colorectal surgeons regarding the surgical management of ulcerative colitis.
Methods
We developed a questionnaire to examine surgical practice patterns for the management of ulcerative colitis. It was reviewed by colorectal surgeons from 2 Canadian centres for clarity and content. Several modifications were made to the survey instrument during this process. The questionnaire was mailed to all fellows of the American Society of Colon and Rectal Surgeons (ASCRS) in Canada and the United States. We mailed a second questionnaire to surgeons who did not respond after 6 weeks. We collected data on years in surgical practice, annual IPAA volume and practice setting (academic v. community). A community hospital was defined as a centre without a general surgery residency program or a colorectal surgery fellowship program. Annual IPAA volume was classified as high (> 15 patients/yr), medium (5–15 patients/yr) or low (< 5 patients/yr). Information on the location of colorectal surgery fellowship training was also obtained from the Canadian surgeons.
Surgeons were asked to describe their typical practices for 3 different clinical scenarios. The first clinical scenario described a 30-year-old patient who underwent subtotal colectomy with end ileostomy for ulcerative colitis 6 months previously. The patient had been off all steroids for 3 months, and at the time of surgery there were no intraoperative complications and there was no tension on the anastomosis. Surgeons were asked if they would perform an IPAA or an IPAA and loop ileostomy. The second clinical scenario described a 30-year-old patient with steroid-dependent ulcerative colitis taking 10 mg/day of prednisone. At the time of surgery, there were no intraoperative complications and a tension-free anastomosis was possible. Surgeons were asked which of the following 3 procedures they would perform: subtotal colectomy with end ileostomy and deferral of IPAA; total proctocolectomy, IPAA and loop ileostomy; or total proctocolectomy and IPAA. The third clinical scenario described a 30-year-old patient with steroid-dependent ulcerative colitis taking 40 mg/day of prednisone. At the time of surgery there were no intraoperative complications and a tension-free anastomosis was possible. Surgeons were asked which of the following 3 procedures they would perform: subtotal colectomy with end ileostomy and deferral of IPAA; total proctocolectomy, IPAA and loop ileostomy; or total proctocolectomy and IPAA.
To examine the potential impact of training environment (Canada v. United States) on practice patterns, we evaluated responses to clinical scenario 1 for 3 groups: Canadian colorectal surgeons with fellowship training in Canada, Canadian colorectal surgeons with fellowship training in the United States and American colorectal surgeons.
Statistical analysis
Data were entered into a computerized database. Statistical analysis of categorical variables was performed using the χ2 test. We compared continuous variables using the Student t test. Logistic regression analysis was used to determine univariate variables associated with surgeon responses to the clinical scenarios. Variables assessed included years in surgical practice, practice setting (academic v. community), surgeon volume (high, medium, low) and location of practice (Canada v. United States). To simplify the analysis of clinical scenarios 2 and 3, we collapsed the response choices into 2 groups: IPAA versus subtotal colectomy with end ileostomy. To control for confounding and interaction, we performed a multivariate logistic regression analysis, and all variables were forced into the model. All 2-way interaction terms were tested for inclusion in the regression model. We considered results to be significant at p < 0.05.
Results
We mailed questionnaires to 40 Canadian and 873 American ASCRS fellows with response rates of 88% and 62%, respectively. Of those who responded, 29 of 35 (83%) Canadian surgeons and 438 of 544 (81%) American surgeons perform IPAA for ulcerative colitis. There were significant differences in the number of years in clinical practice, practice setting and self-reported annual procedure volume between Canadian and American surgeons who perform IPAA (Table 1).
Table 1.
Comparison of demographic and practice characteristics between Canadian and American colorectal surgeons
| Characteristic | Canadian surgeons | American surgeons | p value |
|---|---|---|---|
| Years in surgical practice, no. (SD) | 13.4 (8.14) | 16.4 (7.6) | 0.030 |
| Practice setting, no. (%) | 0.010 | ||
| Academic | 26 (90) | 280 (64) | |
| Community | 3 (10) | 158 (36) | |
| Annual IPAA volume, no. (%) | < 0.001 | ||
| Low (1–5 procedures) | 7 (24) | 219 (50) | |
| Medium (6–15 procedures) | 11 (38) | 162 (37) | |
| High (> 15 procedures) | 11 (38) | 57 (13) |
IPAA = ileal pouch anal anastomosis; SD = standard deviation.
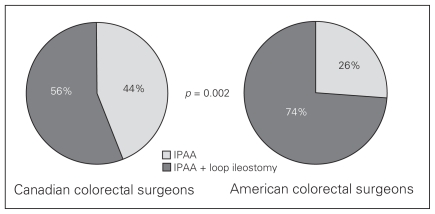
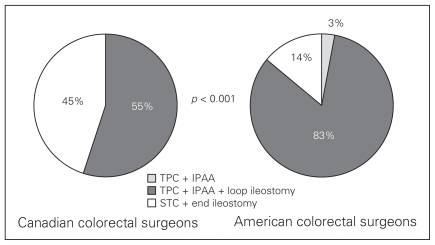
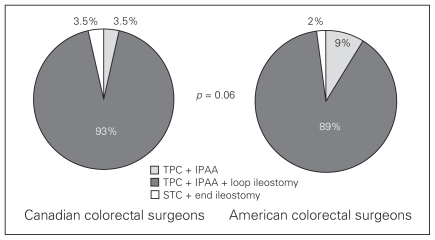
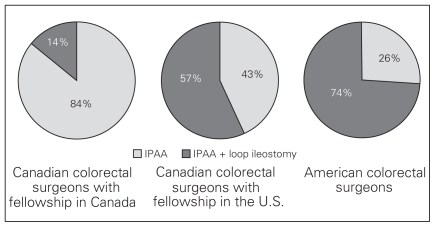
We compared practice patterns between Canadian and American colorectal surgeons for 3 different clinical scenarios (Figs. 1–3). Given a patient with ulcerative colitis who has had a prior subtotal colectomy and is off all steroids, Canadian colorectal surgeons were more likely to perform an IPAA procedure without an ileostomy compared with American colorectal surgeons (44% v. 26%, p = 0.002; Fig. 1). Given a patient with ulcerative colitis who has never had surgery and is taking low-dose steroids, both Canadian and American surgeons would perform an IPAA procedure with an ileostomy (93% and 89% respectively, p = 0.06; Fig. 2). Given a patient with ulcerative colitis who has never had surgery and is taking high-dose steroids, American colorectal surgeons were more likely to perform a pelvic pouch procedure compared with Canadian colorectal surgeons (83% v. 55%, respectively); Canadian surgeons were more likely than American surgeons to defer IPAA and perform a subtotal colectomy (45% v. 14%, respectively). The difference in practice patterns for scenario 3 was significant (p < 0.001; Fig. 3). On univariate analysis, there was no relation between clinical practice patterns and years in surgical practice, practice environment (academic v. community) or annual procedure volume for Canadian or American colorectal surgeons for any of the 3 clinical scenarios (Table 2). There was a significant association between location of practice (Canada v. United States) and practice patterns for clinical scenarios 1 and 3 on univariate analysis and on multivariate analysis after controlling for years in surgical practice, practice environment and annual procedure volume (Table 2, Table 3). For clinical scenario 1, Canadian surgeons who had fellowship training in the United States appeared to have practice patterns intermediate to the other 2 groups (Fig. 4). However, a statistically significant difference was not observed.
Fig. 1.
A comparison of surgical management between Canadian and American colorectal surgeons for a patient with ulcerative colitis who has had a prior subtotal colectomy with end ileostomy. The patient has been off all steroids for 3 months, and, at the time of surgery, a tension-free anastomosis is possible and there are no intraoperative complications.
Fig. 3.
A comparison of surgical management between Canadian and American colorectal surgeons for a patient with ulcerative colitis who is taking 40 mg/day of prednisone. At the time of surgery, a tension-free anastomosis is possible, and there are no intraoperative complications. STC = subtotal colectomy; TPC = total proctocolectomy.
Fig. 2.
A comparison of surgical management between Canadian and American colorectal surgeons for a patient with ulcerative colitis who is taking 10 mg/day of prednisone. At the time of surgery, a tension-free anastomosis is possible, and there are no intra-operative complications. STC = subtotal colectomy; TPC = total proctocolectomy.
Table 2.
Univariate logistic regression analysis for 3 clinical scenarios* involving patients with ulcerative colitis
| Variable | Clinical scenario; odds ratio (95% CI) | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Surgeon volume | |||
| Low | 0.72 (0.4–1.3) | 0.38 (0.1–1.7) | 0.61 (0.3–1.2) |
| Medium | 0.66 (0.4–1.2) | 0.37 (0.1–1.9) | 0.60 (0.3–1.2) |
| High | 1.0 | 1.0 | 1.0 |
| Practice setting | |||
| Academic | 1.0 | 1.0 | 1.0 |
| Community | 0.77 (0.5–1.2) | 0.82 (0.2–3.2) | 1.09 (0.6–1.8) |
| Years in practice | 1.01 (0.9–1.1) | 1.01 (0.9–1.1) | 0.99 (0.9–1.0) |
| Country | |||
| Canada | 3.60 (1.2–10.6) | 2.5 (0.3–18.6) | 10.42 (3.4–32.1) |
| United States | 1.0 | 1.0 | 1.0 |
CI = confidence interval.
In scenarios 1 and 2 the probablility of ileal pouch anal anastomosis is modelled, in scenario 3 the probability of a subtotal colectomy with end ileostomy is modelled.
Table 3.
Multivariate logistic regression analysis for 3 clinical scenarios* involving patients with ulcerative colitis
| Variable | Clinical scenario; odds ratio (95% CI) | ||
|---|---|---|---|
| 1 | 2 | 3 | |
| Surgeon volume | |||
| Low | 0.85 (0.4–1.6) | 0.4 (0.1–1.7) | 0.73 (0.3–1.5) |
| Medium | 0.75 (0.4–1.4) | 0.4 (0.1–2.1) | 0.66 (0.3–1.4) |
| High | 1.0 | 1.0 | 1.0 |
| Practice setting | |||
| Academic | 1.0 | 1.0 | 1.0 |
| Community | 0.81 (0.5–1.3) | 0.96 (0.2–4.0) | 1.26 (0.7–2.2) |
| Years in practice | 1.01 (0.9–1.1) | 1.01 (0.9–1.1) | 0.98 (0.9–1.0) |
| Country | |||
| Canada | 3.23 (1.1–9.7) | 1.3 (0.1–11.6) | 10.6 (3.3–33.9) |
| United States | 1.0 | 1.0 | 1.0 |
CI = confidence interval.
In scenarios 1 and 2 the probablility of ileal pouch anal anastomosis is modelled, in scenario 3 the probability of a subtotal colectomy with end ileostomy is modelled.
Fig. 4.
A comparison of surgical management for a patient with ulcerative colitis who has had a prior subtotal colectomy with end ileostomy according to surgeon location of practice and fellowship training. The patient has been off all steroids for 3 months, and, at the time of surgery, a tension-free anastomosis is possible and there are no intraoperative complications.
Discussion
In the present study, a number of differences were observed between Canadian and American colorectal surgeons. Canadian colorectal surgeons were more likely to practice in academic institutions and report high annual procedure volumes compared with American colorectal surgeons, who were more likely to practice in a community setting and reported low annual procedure volumes. These differences likely reflect the lower number of specialists per capita practising in Canada. Differences were also observed in the surgical practice patterns between Canadian and American colorectal surgeons for patients with ulcerative colitis. These differences are in keeping with the findings of previous survey research and clinical studies that have compared medical and surgical practice patterns between Canadian and American surgeons.6–11 These studies have consistently reported that American surgeons and physicians are more likely to order diagnostic tests and recommend surgery and interventional procedures compared with their Canadian counterparts. To our knowledge, no previous studies have specifically compared gastrointestinal surgery practice patterns between the 2 countries.
The reasons for the differences in practice patterns between Canadian and American surgeons observed in the present study and previous studies are unclear. The organization of the health care systems in the 2 countries is quite different. Universal health care is provided in Canada by a publicly funded single payer as compared with the American system, which has both private and public health care with multiple payers. Exactly how these delivery systems may impact surgical practice patterns is unclear. There are differences in resource availability and the medicolegal systems between the 2 countries. In Canada, there are financial consequences for plaintiffs who are not successful with their legal actions, damages for pain and suffering are capped, and it is uncommon for malpractice suits to be heard by a jury. American physicians are 7 times more likely than Canadian surgeons to be named in medical liability claims, and this may influence clinical practice.12 Previous studies have reported that American physicians and surgeons commonly alter their clinical management because of the threat of malpractice liability.13,14 Physicians reported restricting their practices by eliminating procedures that had high complication rates and avoiding patients with complex medical problems.
Concern about postoperative complications may explain our finding that American colorectal surgeons were less likely to perform IPAA without a proximal diverting ileostomy for a patient who has had a previous subtotal colectomy and end ileostomy and is off all steroids. Given this scenario, 45% of Canadian surgeons reported that they would perform an IPAA without a diverting ileostomy compared with only 26% of American surgeons. However, American colorectal surgeons did not consistently select the most conservative surgical approach for all of the clinical scenarios in the present study. Given a patient with ulcerative colitis who is taking 40 mg/day of prednisone, Most American colorectal surgeons (83%) indicated that they would perform a total proctocolectomy, IPAA and diverting loop ileostomy. In contrast, only 55% of Canadian colorectal surgeons indicated that they would perform this procedure, whereas the remaining 45% would be more conservative and perform a subtotal colectomy and end ilestomy with deferral of IPAA. The explanation for the more aggressive approach taken by American surgeons for the patient taking high-dose steroids is not clear. Research has suggested that patients who are taking high-dose steroids (≥ 40 mg of prednisone/d) are at increased risk of anastomotic leak after IPAA.15,16 Although there is literature to suggest that a proximal loop ileostomy may mitigate the consequences of an anastomotic leak after IPAA,17 it is not clear to what extent this holds true in patients taking high-dose steroids.
Differences in resource availability could explain some of the variation in practice patterns between the 2 countries. With many more specialists per capita in the United States and a for-profit competitive system, wait times for consultation and surgery are significantly shorter compared with wait times in Canada.18–20 The implication is that Canadian patients with steroid-dependent ulcerative colitis may be taking high-dose steroids for a longer duration by the time they undergo surgery compared with American patients. Therefore, Canadian surgeons may have greater concern about effects of steroids on tissue healing, leading them to select a more conservative surgical approach in a patient with ulcerative colitis who is taking high-dose steroids. Limited resources and long wait lists could also influence Canadian surgeons to omit an ileostomy in a low-risk patient with ulcerative colitis who is not taking steroids. This avoids the need for a second operation and frees operating room time for other patients.
We examined the impact of fellowship training location (Canada v. United States) on practice patterns in a subgroup analysis. Canadian surgeons who completed their colorectal fellowship training in Canada appeared to have a very different approach with a low-risk patient with ulcerative colitis compared with American surgeons. Interestingly, surgeons who practise in Canada but completed their fellowship training in the United States reported an intermediate approach to clinical practice. The differences were not statistically significant, and the number of Canadian surgeons included in the analysis was small, making it difficult to draw firm conclusions. However, these data suggest, not surprisingly, that both training and practice environment contribute to surgical decision-making. It should be noted that the Canadian surgeons who received fellowship training in Canada all trained at the same centre, as there was only 1 fellowship program in the country at the time.
The present study has demonstrated a significant difference in practice patterns between Canadian and American colorectal surgeons. Importantly, it has also demonstrated substantial differences in practice patterns within each country for the management of patients with ulcerative colitis. Whereas IPAA remains the procedure of choice for most patients with ulcerative colitis, there appears to be no standard of care with regards to the number of stages needed to achieve the desired treatment outcome. As the number of procedures to complete an IPAA increases, the overall costs, length of recovery and time off work for the patient also increases.1 Each additional procedure is also associated with morbidity and mortality. These costs and risks may be justified if the outcome for IPAA is improved (i.e., lower leak rate, lower failure rate) with a multistage approach. However, there are very limited data available to guide clinical practice.1–5 Previous studies are all retrospective and have included heterogeneous groups of patients with ulcerative colitis. It is likely that the optimal surgical approach is different for patients with ulcerative colitis taking high-dose steroids compared with those who are relatively well and who are not taking steroids.
There are a number of limitations associated with the present study that need to be considered. A low response rate may limit the conclusions that can be drawn from survey research. However, we achieved an overall response rate of 63%, which exceeds the generally acceptable threshold for this type of research. Response bias is a consideration with all survey research. No information was available for the nonresponders in this study. Reporting bias may also have occurred with respondents reporting what they perceived to be the correct responses as opposed to their actual clinical practices. However, a previous study has suggested that physician practice patterns measured using a clinical vignette are similar to actual clinical practice.21 Practice patterns were not collected for a clinical scenario involving a patient with ulcerative colitis who is clinically well but requires surgery owing to long duration of disease and associated cancer risk. However, it is likely that the management approach for this type of patient would have been similar to clinical scenario 1, in which the patient was clinically well and not taking steroids. To keep the survey short and simple, other factors that may contribute to surgical decision-making, such as nutritional status and preoperative duration of steroid treatment, were not included. Finally this research has not linked practice patterns to clinical outcomes.
Conclusion
There is variation in the surgical approach to ulcerative colitis between Canadian and American colorectal surgeons. The reasons for these differences remain unclear. Ideally, clinical management should be guided by medical evidence to provide patients with optimal outcomes balanced against morbidity, mortality and direct and indirect costs associated with care. In the absence of good evidence, care may be influenced by nonmedical factors and lead to unnecessary patient suffering and costs. Currently, there is no accepted standard of care for the surgical approach to IPAA in patients with ulcerative colitis. There is clearly a need for prospective studies to address this issue.
Footnotes
Presented at the Canadian Surgery Forum, Toronto, Ont., Sept. 6–9, 2007
Competing interests: This research was supported by a grant from the Capitol Health Research Fund. Otherwise, none declared.
Contributors: Drs. Richardson and Johnson designed the study, analyzed the data and wrote the article. Drs. Richardson and deMontbrun acquired the data. All authors reviewed the article and approved its publication.
References
- 1.Swenson BR, Hollenbeak CS, Poritz LS, et al. Modified two stage ileal pouch-anal anastomosis: equivalent outcomes with less resource utilization. Dis Colon Rectum. 2005;48:256–61. doi: 10.1007/s10350-004-0848-9. [DOI] [PubMed] [Google Scholar]
- 2.Kaidar-Person O, Person B, Wexner SD. Complications of construction and closure of temporary loop ileostomy. J Am Coll Surg. 2005;201:759–73. doi: 10.1016/j.jamcollsurg.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 3.MacLean AR, Cohen Z, MacRae HM, et al. Risk of small bowel obstruction after the ileal pouch-anal anastomosis. Ann Surg. 2002;235:200–6. doi: 10.1097/00000658-200202000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swenson BR, Hollenbeak CS, Koltun WA. Factors affecting cost and length of stay associated with ileal pouch-anal anastomosis. Dis Colon Rectum. 2003;46:754–61. doi: 10.1007/s10350-004-6653-7. [DOI] [PubMed] [Google Scholar]
- 5.Heuschen UA, Allemeyer EH, Lucas M, et al. One- or two-stage procedure for restorative proctocolectomy: rationale for a surgical strategy in ulcerative colitis. Ann Surg. 2001;234:788–94. doi: 10.1097/00000658-200112000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung D, Hersey K, Fleshner N. Differences between urologists in United States and Canada in approach to bladder cancer. Urology. 2005;65:919–25. doi: 10.1016/j.urology.2004.11.028. [DOI] [PubMed] [Google Scholar]
- 7.Fleshner N, Rakovitch E, Klotz L. Differences between urologists in the United States and Canada in the approach to prostate cancer. J Urol. 2000;163:1461–6. [PubMed] [Google Scholar]
- 8.O’Hara GE, Charbonneau L, Chandler M, et al. Comparison of management patterns and clinical outcomes inpatients with atrial fibrillation in Canada and the United States (from the analysis of the atrial fibrillation follow-up investigation of rhythm management (AFFIRM) database. Am J Cardiol. 2005;96:815–21. doi: 10.1016/j.amjcard.2005.05.027. [DOI] [PubMed] [Google Scholar]
- 9.Groome PA, O’Sullivan B, Irish J, et al. Management and outcome differences in supraglottic cancer between Ontario, Canada and the surveillance, epidemiology, and end results areas of the United States. J Clin Oncol. 2003;21:496–505. doi: 10.1200/JCO.2003.10.106. [DOI] [PubMed] [Google Scholar]
- 10.Tu JV, Pashos C, Naylor D, et al. Use of cardiac procedures and outcomes in elderly patients with myocardial infarction in the United States and Canada. N Engl J Med. 1997;336:1500–5. doi: 10.1056/NEJM199705223362106. [DOI] [PubMed] [Google Scholar]
- 11.Katz SJ, McMahon LF, Manning WG. Comparing the use of diagnostic tests in Canadian and US hospitals. Med Care. 1996;34:117–25. doi: 10.1097/00005650-199602000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Korcok M. CMPA not alone in pursuing huge reserves, CMAJ survey of US firms reveals. CMAJ. 1996;154:1891–4. [PMC free article] [PubMed] [Google Scholar]
- 13.Sobel DL, Loughlin KR, Coogan CL. Medical malpractice liability in clinical urology: a survey of practicing urologists. J Urol. 2006;175:1847–51. doi: 10.1016/S0022-5347(05)01021-9. [DOI] [PubMed] [Google Scholar]
- 14.Elmore JG, Taplin SH, Barlow WE, et al. Does litigation influence medical practice? The influence of community radiologists’ medical malpractice perceptions and experience on screening mammography. Radiology. 2005;236:37–46. doi: 10.1148/radiol.2361040512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heuschen UA, Hinz U, Allemeyer EH, et al. Risk factors for ileoanal J pouch-related septic complications in ulcerative colitis and familial adenomatous polyposis. Ann Surg. 2002;235:207–16. doi: 10.1097/00000658-200202000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lim M, Sagar P, Abdulgader A, et al. The impact of preoperative immunomodulation on pouch-related septic complications after ileal pouch-anal anastomosis. Dis Colon Rectum. 2007;50:943–51. doi: 10.1007/s10350-007-0246-1. [DOI] [PubMed] [Google Scholar]
- 17.Williamson ME, Lewis WG, Sagar PM, et al. One-stage restorative proctocolectomy without temporary ileostomy for ulcerative colitis: a note of caution. Dis Colon Rectum. 1997;40:1019–22. doi: 10.1007/BF02050922. [DOI] [PubMed] [Google Scholar]
- 18.Coyte PC, Wright JG, Hawker GA, et al. Waiting times for knee-replacement surgery in the United States and Ontario. N Engl J Med. 1994;331:1068–71. doi: 10.1056/NEJM199410203311607. [DOI] [PubMed] [Google Scholar]
- 19.Blendon RJ, Schoen C, DesRoches, et al. Inequities in health care: a five country survey. Health Aff (Millwood) 2002;21:182–91. doi: 10.1377/hlthaff.21.3.182. [DOI] [PubMed] [Google Scholar]
- 20.Chen LE, Zamakhshary M, Foglia RP, et al. Impact of wait time on outcome for inguinal hernia surgery repair in infants. Pediatr Surg Int. 2009;25:223–7. doi: 10.1007/s00383-008-2306-6. [DOI] [PubMed] [Google Scholar]
- 21.Peabody JW, Luck J, Glassman P, et al. Comparison of vignettes, standardized patients, and chart abstraction. A prospective validation study of 3 methods for measuring quality. JAMA. 2000;283:1715–22. doi: 10.1001/jama.283.13.1715. [DOI] [PubMed] [Google Scholar]