Abstract
Geriatric dentistry and its instruction are critical in a rapidly aging population. Japan is the world’s fastest-aging society, and thus geriatric dentistry education in Japan can serve as a global model for other countries that will soon encounter the issues that Japan has already confronted. This study aimed to evaluate geriatric dental education with respect to the overall dental education system, undergraduate geriatric dentistry curricula, mandatory internships, and graduate geriatric education of a selected dental school in Japan.
Bibliographic data and local information were collected. Descriptive and statistical analyses (Fisher and Chi-square test) were conducted.
Japanese dental schools teach geriatric dentistry in 10 geriatric dentistry departments as well as in prosthodontic departments. There was no significant differences found between the number of public and private dental schools with geriatric dentistry departments (p = 0.615). At Showa University School of Dentistry, there are more didactic hours than practical training hours; however, there is no significant didactic/practical hour distribution difference between the overall dental curriculum and fourth-year dental students’ geriatric dental education curriculum (p=0.077). Graduate geriatric education is unique because it is a four-year Ph.D. course of study; there is neither a Master’s degree program nor a certificate program in Geriatric Dentistry. Overall, both undergraduate and graduate geriatric dentistry curricula are multidisciplinary.
This study contributes to a better understanding of geriatric dental education in Japan; the implications of this study include developing a clinical/didactic curriculum, designing new national/international dental public health policies, and calibrating the competency of dentists in geriatric dentistry.
Keywords: geriatric dentistry, geriatric dental education, curriculum
Introduction
It is now widely recognized by dentists that they require a more comprehensive knowledge of the medical and dental problems that geriatric patients can pose, particularly those who are medically compromised (1–4). To better serve the increasing number of elderly patients, dentists must have reliable knowledge and skills to cope with their needs. However, geriatric dentistry is a relatively new component of dental education programs worldwide. The development of this area of study has been well documented in the U.S. since the early 1970s (5–7). By 1985, 100% of American dental schools reported that they offered geriatric dentistry as part of their academic curriculum (6). Significant growth in this area has become particularly evident since the mid-1980s with the creation of the Geriatric Oral Research section of the International Association for Dental Research. The European College of Gerodontology was founded in 1990, with members from 22 countries, even from outside of Europe.
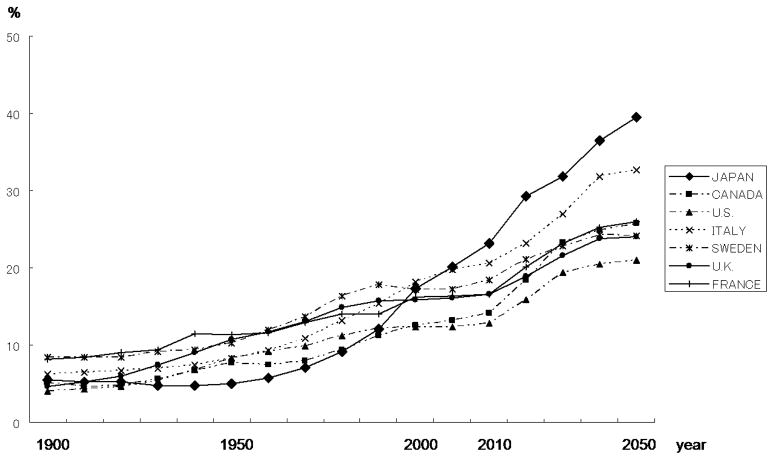
Although the general dental practitioner has historically been slow to accept the importance of treating the elderly (8), geriatric dentistry has become more visible in Japan due to the rapidly growing geriatric population; the most recent Japanese census indicates that 25 million, or 22.7%, of the approximately 120 million total population are elderly (over 65 years of age). Projections estimate that the elderly will account for 30.5% of the total population by 2025, increasing to 38.2% by 2045 and over 40.0% by 2055. Besides being the world’s fastest-aging society (Figure 1) (9), the Japanese population also has the longest life expectancy in the world (10). Therefore, there is a significant need for geriatric dental education to train dentists who will treat these patients.
Figure 1.
Percentage of total population over sixty-five years old
(Source: United nations, The Sex and Age Distribution of World Population: 2000)
Although the Japanese Society of Gerodontology was created in 1986 and Japan’s first department of geriatric dentistry was established at Nippon Dental University in 1987 (11), Hirai et al. reported that Japan’s geriatric education curriculum was still largely undeveloped, especially compared to the more established geriatric programs in U.S. and European dental schools (12). A recent reorganization of Japan’s dental schools at the beginning of the 21st century created ten new geriatric dentistry departments focusing on effective treatments for elderly patients whose anatomical and physiological changes, systemic handicaps, diseases, mental and psychological conditions, and social environments are quite different from those of younger people. Additionally, information on basic clinical medicine, incidence treatment, and emergency care are included in the dental curricula. For example, in Showa University’s geriatric dentistry department, the dental faculty teaches students and residents comprehensive care (caries care, treatment of periodontal disease, tooth extraction, denture adjusting, and denture repair) for elderly patients at dental hospitals, local clinics, and nursing homes.
Currently geriatric dentistry curricula in Japan may be considered at only a formative stage, but it may become a model for countries where the future geriatric population will be similar to that of Japan. While education depends on other conditions such as the cultural, legal and political circumstances, the practices developed in the Japanese geriatric dentistry programs may be applicable elsewhere.
Despite the importance of geriatric dentistry education, there is little published information on this topic. The purpose of this study, therefore, was to report on geriatric dentistry and geriatric education in a selected Japanese dental school (Showa University School of Dentistry). Other issues as well were explored: geriatric dental education with respect to the overall dental education system, undergraduate geriatric dentistry curricula and mandatory internship, and graduate geriatric education in Japan.
Materials and Methods
The data was analyzed to match selected parameters for obtaining critical information regarding dental education. In brief, the descriptive and statistical analyses were conducted as follows: the Fisher exact test was used to identify any distribution differences between the geriatric dentistry departments of public and private dental schools. Together with a breakdown of typical undergraduate geriatric dentistry study components, the chi square test was performed to examine any didactic/practical hour distribution differences between overall dental curricula and fourth-year dental student geriatric dental education curricula.
All analyses were performed using the PASW v.18. statistical package (SPSS Institute, Chicago, Illinois, USA); the significance level was set at 0.05.
Results
Geriatric Dental Education Regarding the Overall Dental Education System
Table 1 shows the distribution difference between the geriatric dentistry departments in public and private dental schools. There are twenty-nine dental schools in Japan; twelve of these are public, and seventeen are private. Ten dental schools have geriatric dentistry departments, four of which are public (Hokkaido University, Tohoku University, Tokyo Medical and Dental University, and Kyushu University), and the other six are private (Showa University, Tsurumi University, Asahi University, Aichi Gakuin University, Osaka Dental University, and Fukuoka Dental College). The other nineteen dental schools do not have geriatric dentistry departments, but prosthodontics departments are responsible for undergraduate and graduate geriatric curricula. Fisher’s exact test results indicate no significant differences between the number of public and private dental schools with geriatric dentistry departments (p = 0.615).
Table 1.
Dental Schools in Japan
| Department of Geriatric Dentistry of Dental Schools | No | Yes | Total |
|---|---|---|---|
| Governmental & Public Schools | 8 | 4 | 12 |
| Private Schools | 11 | 6 | 17 |
| Total | 19 | 10 | 29 |
Undergraduate Geriatric Dentistry Curriculum and Mandatory Internship
A typical geriatric dentistry curriculum is included in the Showa University syllabus. Japan’s dental educational system is a six-year DDS/DMD program that begins following high school graduation. The students engage in didactic and laboratory course work throughout the first four years; geriatric dentistry is taught to the fourth-year students (Table 2). There are twenty-six hours of didactic instruction, and seventeen practical training hours in the laboratory (Table 3). The chi square test reveals that there are more didactic hours than practical training hours, although there is no significant difference in the didactic/practical hour distribution between the overall dental curriculum and fourth-year dental students’ geriatric dental education curriculum (p=0.077).
Table 2.
Geriatric Dentistry Curriculum Outline (Showa University)
| Curriculum Hours | ||
| Didactic | 26 | |
| Practical | 17 | |
| Total | 43 | |
| Curriculum Outline | Contents | |
| Didactic | Public Health Issues | Demographics |
| Economic problems | ||
| Barriers to oral care | ||
| Oral health epidemiology | ||
| Aging | Physiology and pathology of aging | |
| Orofacial system of aging | ||
| Psychology of aging | ||
| Pharmacology in old age | ||
| Geriatric assessment | ||
| Diagnosis And Treatment Planning | ||
| Recording history | ||
| Patient-centred treatment planning | ||
| Oral/mucosal diseases | ||
| Salivary impairment | ||
| Xerostomia | ||
| Radiographical assessment | ||
| Caries risk assessment | ||
| Periodontal disease | ||
| Prosthodontic evaluation | ||
| Implantology for older persons | ||
| Theory of Therapy | Oral health education | |
| Oral hygiene measures and instructions for patients | ||
| Domiciliary care | ||
| Practical | Communication Skills | Active and respectful communication training |
| Communication with elderly adults | ||
| Evaluation | Take vital signs | |
| Laboratory Training | Denture repair | |
| Artificial tooth repair | ||
| Tissue conditioning | ||
Table 3.
Distribution of Curriculum (Showa University)
| Subject | Didactics | Practices | Total |
|---|---|---|---|
| Showa University all | 2091 (47%) | 2362 (53%) | 4453 (100%) |
| Geriatric Dentistry (4th year dental students) | 26 (60%) | 17 (40%) | 43 (100%) |
| Total | 2117 | 2379 | 2379 |
Note: The practical training hours in the 4th year dental students refers to laboratory training only. Direct patient care, which will be conducted druing the 5th year, is excluded.
Discussion
According to the report by Mohammad et al. in 2001, 63% of U.S. dental schools had a geriatric program director or a chairman of a geriatric department, and 67% of schools included clinical components with this instruction (13). Geriatric dental education in Europe varies considerably (14). Our results show that 35% of the dental schools have geriatric dentistry departments offer formal graduate level training exclusively (Table 1). However, where there are no geriatric dentistry departments, the prosthodontic department teaches a geriatric dentistry component instead.
An establishment of a geriatric dentistry department does not require the elimination of other traditional departments in Japan. Geriatric dentistry, prosthodontic, and restorative dentistry departments co-exist and help each other. Therefore, basic skills and knowledge necessary for geriatric dentistry have already covered by these departments for dental students. Table 2 indicates that the curriculum contents are very diverse because there is a demand for more sophisticated dental care with an aging society and changes in disease structures. Some other Japanese schools teach geriatric dentistry with a multidisciplinary perspective, including departments such as prosthodontics, oral implantology, oral surgery, endodontics, periodontics, dental pharmacology, and basic sciences. Communication skills are critical in geriatric dentistry and are therefore included in the curriculum. In addition to hearing impairments as people age, the generation gap and use of dialect by elderly patients are challenges for dental students.
By using published reports on geriatric dentistry education in the United States (13, 15, 16) and in Europe (4, 14, 17–19), geriatric dentistry curricula in the US and in Europe were compared to those at Showa University. While no reports presented specific curriculum hours, curriculum content was well described. Curriculum guidelines for geriatric dentistry in the United States (15) included ➀ cultural and ethnic diversity, and ➁ dietary/food selection. At Showa University, these components are not included in the curriculum, possibly due to the fact that Japan is not ethnically diverse and most people are Buddhist. Japanese, especially the elderly population, prefer fish, steamed rice, and soup. These soft foods facilitate mastication and digestion and are usually prepared by the family members. Kossioni and Karkazis (14) reported the development of a new geriatric dentistry course in Athens, Greece. The European College of Gerodontology published undergraduate curriculum guidelines including the curriculum outline, the related competences, and the structure of training and facilities (4).
Nitschke et al. pointed out that it is important to examine which traditional specialties are covered in the undergraduate geriatric dentistry curriculum (18). The Department of Geriatric Dentistry at Showa University has several faculty members, including the department chair, who are prosthodontic specialists focusing on complete and removal dentures. The availability of this expertise might influence the uniqueness of the curriculum.
Table 3 shows that forty three curriculum hours were assigned to the fourth-year undergraduate geriatric dentistry curricula. There are twenty-six hours of didactic instruction, and seventeen practical training hours in the laboratory. The fifth-year-students will divide their time between direct clinical patient care and preparation for the National Examination for Dentistry (NED), which they take after their sixth year in order to receive their license. Prior to a dental student’s clinical clerkship, there are two common achievement tests: the computer-based test (CBT) and the objective standard clinical examination (OSCE), both implemented in 2006. In preparation for these tests, students observe the clinical treatment of elderly patients in a dental school hospital/clinic setting. Fifth-year students are assigned ninety clinic hours exclusively for geriatric dentistry. Also, dental students learn basics from prosthodontic and restorative dentistry department faculty members. While the exact calculation is difficult due to unclear cut-offs of subjects taught, total training hours in relation to geriatric dentistry will be around 10% of the curriculum.
Just before graduation, the sixth-year Japanese dental students are eligible to take the Japan National Examination for Dentists (NED) (20, 21); it is a multiple-choice, two-day written exam containing questions regarding the knowledge and techniques required for all aspects of dental practice, including geriatric dentistry. The NED results are reported on a pass/fail basis with scores; in March 2010, 3,465 Japanese dental students took the NED, with a 69.5% pass rate (2,408 students). The NED is currently very competitive; however, no renewal of licensure is required.
After passing the NED, a dentist is eligible to practice anywhere in Japan after a minimum one-year mandatory internship in a post-graduate clinical training course. This internship differs from those completed in each university. Showa University’s course consists of three programs:
Six months in a hospital faculty of dentistry, and six months in an out-of-hospital dental office performing clinical rotations
Six months in a hospital faculty of dentistry, and six months in the dental education center performing clinical rotations
One year of clinical training in the dental education center. Geriatric dentistry is also taught in these programs.
Graduate geriatric education is unique because it is a four-year Ph.D. course; there is neither a Master’s degree program nor a certificate program in Geriatric Dentistry. The curricula are different for each dental school. Ph.D. students must submit a doctoral thesis, complete the required credits, and pass a final examination. To enter graduate school, the applicants must take two examinations: one is an English proficiency test, and the other is a written test in the geriatric dentistry discipline. In addition, the chair and professor of each department usually interview the applicants, who must have a dental license to practice in Japan (except for foreign trained dentists). The tuition for graduate school varies according to each dental school; at Showa University for example, the annual graduate tuition is approximately $5,000 (U.S.).
The main research areas of study at Showa University’s Department of Geriatric Dentistry are the effect of dental treatment, biomechanics of the prosthesis, and implant prosthetics on elderly quality of life (QOL). The effect of dental treatment consists of QOL evaluation method, Evidence-Based prosthesis evaluation, and a study of dry mouth and oral malodor. The biomechanics of the prosthesis include a biomechanical evaluation of the denture-supporting tissues, the biomechanics of the over-denture, and an analysis of the properties of artificial saliva that cure dry mouth. The implant prosthetics include the production of the superstructure design with three-dimensional mechanics analysis, functional reconstruction by implant treatment of a cleft palate patient, and the biomechanics in an implant surface and bone interface. In the clinic, graduate students work for elderly patients at dental hospitals, local clinics, long-term care facilities, and nursing homes. The cross-training in geriatric dental research and clinical dentistry is unique to Showa University’s Department of Geriatric Dentistry. The goal is to educate the clinician scientist not only to ask scientific questions derived from actual clinical experiences, but also to translate scientific data into clinically relevant standards.
Conclusion
Japanese dental schools teach geriatric dentistry in ten geriatric dentistry departments as well as in prosthodontic departments; overall, undergraduate and graduate geriatric dentistry curricula are multidisciplinary. Very little data regarding geriatric dental education has been published by dental associations and government agencies. There are no curriculum guidelines for geriatric dentistry in Japan. In addition to bibliographic data, the information for this study was collected by the authors with support from the Showa University School of Dentistry. Collecting the limited amount of information regarding the other Japanese dental schools was a challenge in this study. However, the information gained about a selected dental school in Japan will serve as a model for other Japanese dental schools with developing a clinical/didactic curriculum, designing new national dental public health policies, and calibrating the competency level of dentists with respect to geriatric dentistry. The results of this study will also be helpful to countries where the geriatric population will soon be similar to that in Japan.
Acknowledgments
The authors thank Ms. Jeanne Santa Cruz (Texas A&M Health Science Center Baylor College of Dentistry) for the critical editing of this paper. They also thank Dr. Chul Ahn (University of Texas Southwestern Medical Center at Dallas) for statistical advice.
This work has been supported by NIH KL2RR024983 (TK) and UL1 RR024982, entitled, “North and Central Texas Clinical and Translational Science Initiative” from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research, and its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/. Information on Reengineering the Clinical Research Enterprise can be obtained from http://nihroadmap.nih.gov/clinicalresearch/overview-translational.asp.
References
- 1.Preshaw PM, Mohammad AR. Geriatric dentistry education in European dental schools. Eur J Dent Educ. 2005;9:73–77. doi: 10.1111/j.1600-0579.2004.00357.x. [DOI] [PubMed] [Google Scholar]
- 2.Shah N. Geriatric dentistry: the need for a new specialty in India. Natl Med J India. 2005;18:37–38. [PubMed] [Google Scholar]
- 3.Tanaka K, Honda T, Kitamura K. Dentistry in Japan should become a specialty of medicine with dentists educated as oral physicians. J Dent Educ. 2008;72:1077–1083. [PubMed] [Google Scholar]
- 4.Kossioni A, Vanobbergen J, Newton J, Muller F, Heath R. European College of Gerodontology: undergraduate curriculum guidelines in gerodontology. Gerodontology. 2009;26:165–171. doi: 10.1111/j.1741-2358.2009.00296.x. [DOI] [PubMed] [Google Scholar]
- 5.Ettinger R, Beck JD, Jakobsen J. The development of teaching programs in geriatric dentistry in the United States from 1974 to 1979. Spec Care Dentist. 1981;5:221–224. doi: 10.1111/j.1754-4505.1981.tb01257.x. [DOI] [PubMed] [Google Scholar]
- 6.Beck JD, Ettinger RL. The development of geriatric curricula in U.S. dental schools, 1979–1984. J Dent Educ. 1987;51:523–527. [PubMed] [Google Scholar]
- 7.Saunders RH, Yellowitz JA, Dolan TA, Smith BJ. Trends in predoctoral education in geriatric dentistry. J Dent Educ. 1998;62:314–318. [PubMed] [Google Scholar]
- 8.Meskin L. The changing face of dentistry -the future of gerodontology- Bull Tokyo Dent Coll. 1998;39:1–5. [PubMed] [Google Scholar]
- 9.United Nations. The Sex and Age Distribution of World Population. 2000. [Google Scholar]
- 10.Population Statistics of Japan 2008. National Institute of Population and Social Security Research; Tokyo, Japan: 2008. pp. 12–16. [Google Scholar]
- 11.Inaba S. Geriatric dentistry in the Nippon Dental University. Japanese journal of gerodontology. 1988;2:74–76. [Google Scholar]
- 12.Hirai T, Endoho J, Ogura H. Status of geriatric education in Japanese dental schools. Gerodontics. 1988;4:232–234. [PubMed] [Google Scholar]
- 13.Mohammad AR, Preshaw PM, Ettinger RL. Current status of predoctoral geriatric education in U.S. dental schools. J Dent Educ. 2003;67:509–514. [PubMed] [Google Scholar]
- 14.Kossioni AE, Karkazis HC. Development of a Gerodontology course in Athens: a pilot study. Eur J Dent Educ. 2006;10:131–136. doi: 10.1111/j.1600-0579.2006.00402.x. [DOI] [PubMed] [Google Scholar]
- 15.Curiculum Guidelines for Geriatric Dentistry. J Dent Res. 1989;53:313–316. [PubMed] [Google Scholar]
- 16.Dolan TA, Berkey DB, Mulligan R, Saunders MJ. Geriatric dental education and training in the United States: 1995 White Paper findings. Gerodontology. 1996;13:94–109. doi: 10.1111/j.1741-2358.1996.tb00161.x. [DOI] [PubMed] [Google Scholar]
- 17.Shanley DB. Dental education and dentistry in Europe. J Am Coll Dent. 2007;74(2):4–8. [PubMed] [Google Scholar]
- 18.Nitschke Ina, Müller Frauke, Ilgner Alexander, Reiber Thomas. Undergraduate teaching in gerodontology in Austria, Switzerland and Germany. Gerodontology. 2004;3:123–129. doi: 10.1111/j.1741-2358.2004.00031.x. [DOI] [PubMed] [Google Scholar]
- 19.Nitschke Ina, Bernhard A, Sobotta J, Reiber Thomas. Undergraduate education in gerodontology in Germany: the Leipzig Programme. Gerodontology. 2008;3:135–141. doi: 10.1111/j.1741-2358.2008.00222.x. [DOI] [PubMed] [Google Scholar]
- 20.Heo SM, Kim KJ, Kawamura M, Komabayashi T. Comparison of the dental education systems in Korea and Japan. Int Dent J. 2004;54:70–72. doi: 10.1111/j.1875-595x.2004.tb00257.x. [DOI] [PubMed] [Google Scholar]
- 21.Komabayashi T, Bird WF. Comparison of written examinations required for dental licensure in Japan and the United States: contents, cognitive levels, and cultural implications. J Dent Educ. 2005;69:930–936. [PubMed] [Google Scholar]