Abstract
To date, only modest gains have been achieved in explaining adherence to medical regimens, limiting effective interventions. This is a particularly important issue for African Americans who are disproportionately affected by the HIV epidemic. Few studies have focused on intragroup variation among African Americans in adherence to ART. The aim of this study was to identify and describe the cultural rationales guiding African American patients' formulation and evaluation of adherence. Rationales are key features of purposeful human action. In-depth interviews with 80 seropositive African Americans were tape recorded, transcribed, and analyzed. Participant CD4, viral load and medical histories were collected at each data point. Analysis of four waves of panel data identified three types of adherence rationales: Authoritative Knowledge Rationale (AKR; n=29, 36.3%), Following Doctors' Orders Rationale (DOR; n=24, 30.0%) and Individualized Adherence Rationale (IAR; n=27, 33.8%). Differences in mean reported adherence between the rationale groups did not achieve statistical significance. However, the fraction reporting low adherence (<70%), although not different by rationale group at the first interview (T1), was significantly higher for the IAR group by the fourth interview (T4). Objective clinical markers (CD4 and viral load) improved over time (from T1 to T4) for AKR and DOR groups, but remained unchanged for the IAR group, yet self-reported adherence declined for all groups over the course of the four interviews.
Introduction
Although swallowing a pill is easily done by many, doing so consistently each day over a period of years is often a challenge. At least half of all patients fail to adhere to their medication regimens regardless of the disease or condition.1 To date, virtually no single characteristic of the individual, the treatment itself, or the system under which it is prescribed and administered can explain successful or failed adherence practices. However, a systematic review of three decades of adherence research2 across diverse medication regimens and over 200 variables identified three factors that were strongly associated with adherence rates: patient beliefs about medication in general, the past experiences of the patient or their family members, and social support. This article examines patient beliefs, conceptualized as rationales3 about taking antiretroviral therapy (ART) and their influence on adherence. Such personal rationales inform and powerfully pattern an individual's purposeful actions in adherence.
Low rates of adherence are a widespread problem but become exceptionally problematic when the medication is needed to sustain lives and limit morbidity as is the case for ART for HIV disease. Prior research on ART adherence4–9 shows that beliefs about medicine are strongly associated with adherence to treatment. This is a particularly important issue for seropositive African Americans who are disproportionally represented among people with HIV in the United States, with ten times the infection rate and higher morbidity and mortality rates than whites.10,11 Although accounting for less than 13% of the U.S. population, African Americans account for 49% of new HIV diagnoses.9 African Americans report poorer adherence than whites or Latinos,12 and are more likely to discontinue non-nucleoside reverse transcriptase inhibitors (NNRTIs) and protease inhibitors (PIs) after initiating therapy.13 Few research studies have focused exclusively on African American adherence to ART. Instead African Americans tend to be understood as a distinct, bounded racial group in comparison to whites and/or Latinos, an approach that makes it impossible to identify within-group variation.14 Studies specifically focusing on the HIV-related beliefs of African American have primarily documented the presence of conspiracy beliefs and the possible influence that those beliefs impose on their willingness to be tested15 and on ART adherence.16,17 Identifying the rationales African Americans hold concerning ART and describing the influence of these rationales on adherence will provide insight into how patients think about the medication and the need to adhere to their regimen, and may improve adherence by tailoring programs to patients' understandings of the illness and its treatment and by identifying counterproductive modes of reasoning. An appreciation of how rationales influence adherence may contribute to reducing disparities in HIV outcomes for African Americans.18
In this article, we utilize the construct of adherence rationales to capture the implicit models patients draw on in daily adherence practice. Our study extends and builds on the findings of Laws et al.19 who described how people use rationales to justify the way they have customized their ART regimens. These rationales are based on individual understandings of both ART adherence and HIV disease, which play a role in how patients define adherence to medication in the conduct of their everyday lives. We argue that studying the rationales that African Americans use to guide their ongoing ART adherence is a productive way to understand how beliefs influence daily adherence and to illuminate their potential contribution to understanding disparities in HIV outcomes.
People develop rationales that explain to themselves the necessity for taking medication, the manner in which it should be taken, and its impact on their bodies and their lives.19 Attention to rationales involves a focus on active decision making rather than the implied lack of intentionality in explanations that feature forgetting, absence from home, or the demands of work, often identified as causes for nonadherence.20–22 In its approach the research reported here is similar to studies of intentional nonadherence5,8,23,24 in that, rather than documenting the fact of nonadherence, it explores the rationales that patients develop to justify their individual approach to adhering to medication. Insight into rationales will allow us to move beyond the dichotomous understanding of ART adherence in which people are categorized as either adherent or nonadherent. Such a dichotomy fails to capture the range of behaviors involved in adherence or the rationales that justify these behaviors.25
Adherence rationales, derived from anthropological studies, are conceptualized as embodying individual cognitions and cultural beliefs along with explanations for the daily practices of adhering to a medical regimen. A rationale includes the patient's explanatory model of illness that is disease specific29 and is developed in response to specific episodes of illness within a naturally occurring clinical and life–world context.30 Anthropological research has shown that these adherence rationales are synergistically developed and reworked in the process of treatment,26,27 rather than operating as static factors as is posited, for example, with the Health Belief Model.28 Rationales give rise to a range of adherence practices, which are the behaviors people engage in when they adhere (or not) to treatment.1,31–36
Methods
Design
The design featured two groups to represent for observational study key natural situations in the course of ART therapy. The groups were: (1) individuals new to ART and with at most 30 days of experience (naive) and (2) veterans of ART with 12–30 months experience (long-term). The design provided theoretically meaningful experiential groupings attending to duration. It represented for extended 3-year case studies a wide range of the most salient socio-cultural and psychological conditions and experiences in the natural history of adherence understandings and practices. This design allowed us to sample the key issues of social and personal life reorganization attendant to initiating ART. The naive group consisted of individuals encountering the challenges and promises of taking and living with the medication for the first time. The long-term group consisted of patients who were already experienced with ART and who were confronting issues of long-term adherence as opposed to short-term adjustments in medication and daily routine. The study was conducted with the institutional review board approval from the university and the two hospitals' human investigation committees.
Participants and setting
A sample of 80 seropositive African Americans on ART was recruited from infectious disease clinics at two inner city hospitals into the naïve and long-term study groups. At the public hospital 75% of its 1115 seropositive patients were African American, whereas the number of seropositive patients at the private hospital was 1800, of whom 65% were African American. For the combined clinic population, the median age was 34 and 30% were women. Overall, 28% were active substance users, 10% were alcohol abusers, 30% had hepatitis B, 25% hepatitis C, 20% were experiencing mental illness, and 5% were homeless. Approximately 80% of the clinic populations had prescriptions for ART.
Data collection
Data were collected as part of a longitudinal study of adherence to ART among African Americans. Study participants were interviewed 8 times over 3 years in their homes by trained interviewers. Interviews were conducted every 3 months in year 1 and every 6 months in years 2 and 3. The interviews were scheduled within 2 weeks before or after a clinic visit to facilitate collection of contemporaneous clinic data. The interviews lasted 1.5–2 h. In addition to in-depth open-ended interview questions, standardized assessments were administered and clinic outcome data (CD4 and viral load) were collected.
Measures
Three domains are relevant to this article: (1) adherence rationales, (2) self-reported levels of adherence, and (3) clinic data (CD4 and viral load counts).
Adherence rationales
Rationales were based on responses to in-depth questions that assessed the following topics identified by the literature as aspects of adherence rationales: (1) the patient's explanatory model describing how the medication and the disease interact38–43; (2) reasons for initiating treatment8,34; (3) discussions of self-initiated adjustments to their medication regimen30,37; and (4) metaphors used to describe adhering to treatment.44–46 Adherence rationales often represent beliefs and meanings beyond the specific act of pill taking, and reference higher order meanings embodied in one's personal philosophy, moral stance, or cultural values. These higher order meanings can potentially be seen in the metaphors that individuals associate with adherence.
Adherence—self-reports
We used the Medical Outcomes Study Adherence Scale (MOS)47 to assess self-reported adherence to antiretroviral medication. This scale consists of 5 questions each rated on a scale from 0 (none of the time) to 5 (all of the time): “I have a hard time doing what the doctor suggested I do,” “I find it easy to do the thing my doctor suggested I do,” “I was unable to do what was necessary to follow my doctor's treatment plans,” “I follow my doctor's suggestions exactly,” and “Generally speaking, how often during the past 4 weeks were you able to do what the doctor told you?” The first and third questions are reverse coded, then scaled to 100 to obtain a percent adherence. For purposes of analysis, we also trichotomized these data into low (<70%), medium (70–89%), and high (>90%) adherence.
Adherence outcome data
Research staff recorded CD4 and viral load from participant medical charts within 2 weeks before or after each interview.
Data analysis
The data for this article consisted of responses from a full year of interviews (T1–T4, every 3 months) to 12 questions (48 responses per participant) designed to assess aspects of adherence rationales identified by the literature.19 The topics of these questions included: (1) decision to initiate ART, (2) ART and HIV models, (3) adherence problem solving, and (4) adherence metaphors (Table 1). The data collection time frame allowed us to capture a full annual cycle of the ritual, celebratory, and “special” annual occurrences that could potentially impact adherence practice. The data set was divided randomly and approximately equally among the data analysis team (2 research assistants and 2 principal investigators) who summarized these responses to create an abstract (1–3 pages) of the data for each participant. These abstracts were then given to the interviewer assigned to each participant to verify that the abstracts captured the meaning of the original data set consistent with the interviewer's personal knowledge of the adherence rationale and practices of the participant gained through multiple interviews. The validated abstracts were returned to the analysis team.
Table 1.
Domains and Measures of the Adherence Rationale Construct
| Construct | Domain | Interview questions |
|---|---|---|
| Adherence rationale | Decision to initiate ART | Why did you decide to start taking HAART? |
| Has there been a “turning point” in your HIV experience—event or experience that changed the way you live with HIV? | ||
| Model of ART interaction with HIV | How does HIV work? | |
| How does ART work? | ||
| Do you believe that HIV's still there even if your viral load is low? | ||
| Have you ever given yourself a drug holiday? If so, why did you do this? | ||
| Do you need to take ART in the way your doctor told you to for it to work? Why or why not? | ||
| How often do you have to take your medication to be satisfied you are doing a good job? | ||
| Ongoing adherence problem solving | Is it OK to adjust your ART medication yourself? | |
| Does your body tell you when to take your medication? | ||
| Have you recently missed one or more doses of medication? How do you explain this? | ||
| Adherence metaphors | Sticking to my medication schedule is like…. |
ART, antiretroviral therapy; HAART, highly active antiretroviral therapy.
The analysis team was blinded to the identity of the research participants. The question driving the analysis was: “What rationales did the study participants use to guide their adherence practice?” The abstracts were then subjected to a pile sort procedure.48 This involved:
Examining each abstract for evidence of adherence rationales.
Assigning each abstract to a “pile” based on the discussions in step 1. The resulting “piles” were developed inductively through reflection on the characteristics of each participant's rationale in comparison to those of other participants in the study.49,50 Abstracts with similar adherence rationales were placed in the same pile; those with different rationales were used to form new “piles.” Following this procedure resulted in five adherence rationales/“piles” being identified (medical model, doctor's orders, lifestyle, alternative model, different priority).
Analyzing each pile as a group and recording the characteristics that defined its rationale.
Resorting the entire set of abstracts based on the lists of characteristics identified in step 3. As a result of the re-sort, we determined that three of the initial piles (lifestyle, alternative model, different priority) belonged together. These were combined (individual adherence rationale) resulting in three “piles” of rationales.
Collecting and randomly mixing the set of abstracts and conducting a final confirmatory sort based on the characteristics identifying the three adherence rationales. In this final sort, inter-rater reliability ranged from 85% to 92%.
We examined the three resulting adherence rationales for demographic and length of time on ART (long-term and naive) patterns. We also investigated whether there was a relationship between adherence rationale and self-reported level of adherence, and between adherence rationale and clinic outcome data (CD4 and viral load).
For categorical variables, we used the χ2 test (e.g., testing the association between adherence rationale and study group). Since the medication adherence data and CD4 and viral load data were not normally distributed, we used the nonparametric Kruskal-Wallis test in examining the relationship between these variables and adherence rationales.
Results
Sample description
The study sample consisted of 80 seropositive African American adults with an active prescription for ART (Table 2).
Table 2.
Sample Description (n=80)
| |
Age |
Gender |
Employed |
Education |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean age (SD) | Men | Women | Yes | No | Missing | Grade school | High school | > High school | Missing | |
| ART-naive | 42.6 (42.9) | 15 (83%) | 3 (17%) | 7 (39%) | 10 (56%) | 1 (6%) | 2 (11%) | 10 (56%) | 5 (28%) | 1 (6%) |
| ART long-term | 41.1 (9.7) | 40 (65%) | 22 (35%) | 10 (16%) | 46 (74%) | 6 (10%) | 10 (16%) | 36 (58%) | 13 (21%) | 3 (5%) |
SD, standard deviation.
Analysis showed no statistically significant associations between demographic characteristics, time on ART (naive/long-term), and adherence rationales (all p>0.05)
Rationales
We identified three types of adherence rationales: the Authoritative Knowledge Rationale (AKR; n=29, 36.3%), the Follow Doctors Orders (DOR; n=24, 30.0%), and the Individualized Adherence Rationale (IAR; n=27, 33.8%).
Individuals exhibiting an AKR based their rationale of disease and treatment upon how it was defined by their physicians and stated they worked to adhere to the recommended regimen. However, they adopted their physician's recommendations only after individual evaluation and consideration of a range of sources of information. The DOR group accepted their physician's recommendations without much personal reflection, drawing on few external sources of knowledge and demonstrating little interest in thinking through the issues presented by adherence. People with an IAR drew information about ART from a range of sources that included their physicians, popular culture, the “street,” their own past experience and that of their relatives, alternative medical beliefs, and folk medicine. From these different sources, they developed their own rationale for adherence, rejecting the physician's authoritative knowledge.
In what follows, we describe the rationales in detail. Each rationale is illustrated with a case study selected as the best representation of the characteristics of the rationale being described.
Authoritative knowledge rationale
The AKR category represents an active engagement in the decision-making process. Patients professing an AKR tried to understand how ART worked, decided for themselves whether to start ART based on their knowledge of HIV, and then used this understanding to guide ongoing practice and to inform decision making concerning the challenges and dilemmas presented by long-term adherence.
Case example
R. is a former carnival worker and recovered substance abuser (alcohol and crack cocaine). He is functionally illiterate, and has a close and cordial relationship with his doctor. He firmly believes that it is his responsibility to ask questions and educate himself about his illness and treatment. He told his doctor, “Even though I don't know how to read all this you writing, give me a reason why you think it's time for me to take it (ART) and what the precaution is if I don't take it or if I do take it; I'll decide.”
A distinctive characteristic of this rationale was the patient's alliance with his or her physician.
I feel that the doctor knows what he's doing. I mean, provided the information that he's giving me about the medicine I've been taking, I agree with him. I've seen nothing but major improvement, so I can't not do what he's saying.—Long-Term AKR, male
In making the decision to initiate ART, AKR individuals indicated that although they had followed their physician's advice, the decision that they made had been their own.
The AKR does not imply a simple uncritical acceptance of the physician or the science used. However, the skepticism expressed by individuals was due to their understanding and appreciation for how science works, and not based on distrust of the medical system as a whole.
They ain't worked out all them bugs. It just is according to you, your doctor, your system, your body. You may not be able to take what I take, and you'll just have to work it out like you do a car. That's why they change a car every year, Chrysler wouldn't be in business if they just kept the first Chrysler they made. They kept changing it until they got better. Your doctor got to keep working with mixtures and cocktails and different meds and see what works best for your body.—Long-term AKR, male
The AKR acceptance of the medical scientific model of HIV and its treatment was seen in how rarely individuals with an AKR accord authority to embodied knowledge—“listening” to one's body is not factor in adherence to medication schedules. In this way, they were distinctly different from both the DOR and the IAR groups.
Individuals endorsing an AKR understood that ART would not cure HIV, but only control it, and appreciated the consequences of poor adherence, views consistent with those expressed by their physicians. They relied on these understandings in ongoing adherence decision-making. The CD4 and viral load of self-identified injection drug users who held an AKR confirmed the success of their practice.
The AKR acceptance of the medical model is reflected in the accounts people provided to explain why doses were missed and how these lapses would be corrected.
I overslept, left the house, didn't take it and got back it was too close to the next dose, so I don't play catch up and double up. I got enough in my bloodstream that should keep me up to catch back up.—Long-term AKR, male
Individuals with an AKR used metaphors that reflected an “active or “take charge” mentality that invoked a sense of personal responsibility and accountability.
Doctor's orders rationale
Study participants with the DOR took their medication because they were instructed by their physician to do so. These individuals considered few other sources of information and had few thoughts about the nature of HIV or ART when describing their adherence rationales. Their doubts were subsumed by their trust in their physician. (“He's the man; if he says do it, I do it.”) Their discussions often included talk that associated adherence with a moral duty. Using words like “should,” “must,” “have to,” individuals with the DOR signaled that they associated their adherence practice with the qualities of being a good person.
Case example
L. formerly worked as a day laborer and now lives on disability with his elderly mother. He believes the medications are keeping him healthy and says he is very adherent but occasionally forgets. At times medical insurance problems have interfered with his ability to get his medications. He sees these problems as beyond his control and, thus, does not “count” doses missed due to lack of insurance as really missed. He is now trying to be 100% adherent because he said his doctor told him that if he adhered completely, he would be able to discontinue the medications altogether.
Individuals with a DOR emphasized the role of their physician in the decision to initiate treatment. However, they often deviated from accepting the physician's authority when it came to embodied knowledge or the belief that the body could “tell” when it needed medication. Like the IAR group, but unlike the AKR group, some people with a DOR described how signals from their body acted as a countervailing influence to the physician's authority.
Individuals with a DOR were similar to those with an AKR in that both were emphatic that they were acting in accordance with physician's guidance, but differed in that individuals with a DOR could not clearly describe models for how HIV and ART worked, in contrast to the AKR group whose descriptions of the models were detailed and similar to those held by their physicians. Both groups were reluctant to self-adjust medication doses.
A distinctive feature of the DOR was an association of adherence with a sense of moral responsibility. A missed dose for individuals in this group reflected on their character and indicated that they were not meeting their adult responsibilities.
You want to feel that you did your part. It's not going to be because you didn't do some of the things you're supposed to do as far as taking your medication that something bad happens so I try.—Long-term DOR, woman
Despite this connection between adherence and moral responsibility, individuals with a DOR could justify missing doses when the circumstances were deemed to be beyond personal control. For example, four individuals with a DOR reported their adherence as 100% despite having missed several weeks of medication due to insurance problems, reasoning that they took 100% of their medications whenever they had them. “That [adherence interrupted by loss of insurance] wasn't my problem. I took all the pills I had when I could get them.” Since these missed doses were “not their fault,” their level of adherence was not impaired. This stance is a defining characteristic of the DOR and is not a feature of either the AKR or IAR.
The metaphors the DOR group associated with adherence reflect more habit, less volition, and little individual authority compared to the other two groups. Individuals with a DOR tended to say adherence is like drinking water, eating, or watching TV. These are relatively passive, habitual activities that are done with little effort or attention to detail and do not imply individual thought or decision making.
Individual adherence rationale
People with an IAR drew on multiple sources of authority, integrating ideas from popular culture, alternative medicine, “street” knowledge, and folk medicine into their own understanding of what it means to be adherent. Some based their adherence rationales on their own analysis of clinical research protocols. For example, three study participants followed self-designed structured treatment interruption programs modeled after their understanding of the SMART (Strategies for Management of Anti-Retroviral Therapy) study, a randomized controlled study that their clinics were participating in at the time of their interviews.
Individuals with an IAR had a personal understanding of ART adherence, which often resulted in an unwillingness or inability to assign the same high priority to adhering to treatment as their physician. For some, this meant accommodating ongoing substance use at the expense of regular adherence. Several people in this group were noteworthy for their distrust of their physician.
Case example
Ms. M is a retired LPN and former sex industry worker. She is on the board of several AIDS service organization as an advocate for African Americans with HIV, in particular women, and was a motivational speaker on living with HIV. She sometimes abused alcohol. She was largely nonadherent to ART. She distrusted physicians especially when they admonished her about the need to be adherent.
Like the AKR group, the IAR group challenged their physician's authority, but unlike those with an AKR, they did not seek to align themselves with their physician's view of adherence.
It's kinda hard to do what the doctor say all the time because you just don't feel like doing it; then it gotta be a certain time; you gotta be in the house all day to do it. Or I just don't have enough energy to do it; or you just get tired of doing what the damn doctor say to do, you just get pig-headed and wanna do what you wanna do.—Naive IAR, man.
Individuals with an IAR expressed clear ambivalence about the authority of scientific knowledge and were more likely than those with a DOR to accord authority to embodied knowledge; the need to “listen to my body” often appeared in their rationales.
All three rationale groups agreed that taking ART is necessary, but individuals with an IAR expressed considerable ambivalence and concern about the medication. Some study participants exhibited a clear pattern of cycling on and off the medication (taking “drug holidays”) because of these concerns.
You feel you need a break, so, you just stop, until you get sick. Or till you're not feeling well or something makes you think, maybe I better go back and start taking these medications. Then you go back.—Long-term IAR, man
This view stood in stark contrast to that of both AKR and DOR groups who believed that drug holidays were antithetical to treatment success.
These are the drugs for your life, so…ain't no holiday off-, ain't no such thing as a drug holiday when these are drugs for your life. So I mean…you, I mean me having this disease, why take chances.—Naive AKR, man
The IAR group held models of ART and HIV that were considerably different from those held by their physicians, and they were more confused regarding the precise effect of ART than the other rationale groups. This confusion is likely because their models combined knowledge from a number of sources that included the body, family members and popular media, which present conflicting views about the role of ART and its safety.
The metaphors individuals with an IAR used when asked about adherence to ART reflected a rejection of physician authority in their care and treatment.
Ongoing adherence practice
We analyzed self-rated adherence for each rationale group and found that at each of the first four interviews, the differences between the rationale groups were not statistically significant at p<0.05, except at T2 when those with an AKR rated themselves significantly more adherent (Kruskal-Wallis, p<0.01) than those who had an IAR. However, reported adherence for the entire sample declined over the 4 interviews (Wilcoxon signed ranks, p<0.001) and for the AKR and DOR groups separately (Wilcoxon signed ranks, p<0.01). The proportion of participants who reported low adherence (<70%) did not differ by rationale group at T1, but did so at T4 with a significantly higher proportion of individuals with an IAR reporting low adherence (χ2=5.3; p<0.05). CD4 counts improved significantly (Wilcoxon signed ranks, p<0.05) for the AKR and DOR groups between T1 and T4, whereas they remained statistically unchanged over this time period for the IAR group. Viral load was significantly higher for the IAR group at T4 compared to the other rationale groups (Kruskal-Wallis, p<0.05; Table 3).
Table 3.
Adherence Rationale by Reported Adherence and Clinical Outcomes at T1 and T4 (n=80)
| |
T1 |
T4 |
||||
|---|---|---|---|---|---|---|
| Reported adherence (mean %±SD) | Median CD4 (cells/μL) (min, max) | Median viral load (copies/mL) (min, max) | Reported adherence (mean %±SD) | Median CD4 (cells/μL) (min, max) | Median viral load (copies/mL) (min, max) | |
| Authoritative Knowledge Rationale (n=29) | 88.7±18.4a | 380a (5–992) | 694 (50–447k) | 76.0±23.8a | 450a (7–1029) | 400 (50–750k) |
| Doctor's Orders Rationale (n=24) | 84.5±16.4a | 339a (34–968) | 1974 (50–650k) | 76.5±20.7a | 440a (90–897) | 400 (50–30k) |
| Individual Adherence Rationale (n=27) | 79.9±21.5 | 242 (5–2500) | 725a (40–750k) | 66.4±21.5 | 315 (8–999) | 10,000a (50–750k) |
p<0.05 (comparisons between T1 and T4).
SD, standard deviation.
Discussion
This study identified a robust set of three rationales HIV-positive African Americans use to guide their adherence to ART. These rationales were unrelated to participant demographics or other characteristics and therefore are not proxies for these factors. The distinct adherence rationales identified in this study highlight heterogeneity among African Americans often underrecognized in the literature. Many studies on adherence to ART are designed to provide contrasts between groups—African Americans compared to whites or to Latinos—but may not adequately account for intragroup variation. The rationales we have identified may represent types of engagement with adherence to ART as a life practice, each of which entails different barriers, challenges, and rates of success.
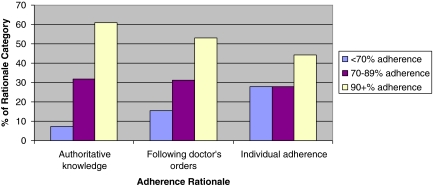
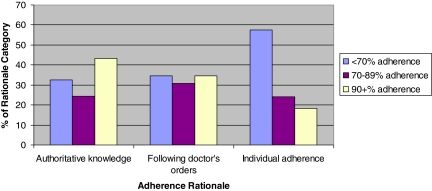
Most study participants intended to adhere to their treatment. To do so, they sought to integrate adherence into their daily lives. Attention to patient rationales for initiating and maintaining treatment helps in understanding adherence practices. Those with the AKR were similar to the participants in the Lewis et al.52 study of individuals who were 100% adherent. They established active partnerships with their physician and identified strongly with the health care team. Patients with the DOR trusted the authority of their physician to guide their adherence practice. However, while these individuals sought to be adherent in order to “please” their physician, they did not express an interest in being included in decision making or in acting as “partners” in their care. Those with the IAR developed rationales that in many cases competed with that of their physicians. For some, these were carefully constructed explanations of ART and its adherence requirements, but for others, they were a justification for integrating their adherence to ART into the demands of their lifestyle in a way that was most convenient for them (Figures 1 and 2).
FIG. 1.
Adherence level at interview #1 by rationale. (Color image can be found at www.liebertonline.com/apc)
FIG. 2.
Adherence level at interview #4 by rationale. p<0.05. (Color image can be found at www.liebertonline.com/apc)
All self-reported adherence declined over time as measured by the MOS adherence scale. However, the decline was most significant for the IAR group who were more likely to report low adherence at the fourth interview compared to the other groups. In addition, their CD4 counts did not increase as they did for the other groups and their viral load was markedly worse at T4 compared to the AKR and DOR groups.
An examination of the metaphors participants used when describing their treatment adherence provided a window into the relatively neglected area of interactions between current adherence practices and deep-seated value orientations. For example, a life-long tendency to challenge authority was clear in some adherence metaphors used by individuals with an IAR and a passive stance toward responsibility was evident in metaphors of the DOR group. Identifying how the range of values reflected in adherence metaphors contributes to adherence practices among HIV-positive African Americans will advance research regarding health disparities and move us toward a more nuanced understanding of the African American health care experience.
Limitations
The study has several limitations. The sample population used is clinic based and nonrandom. In addition, the rationales held by people who drop out of treatment or have never started treatment remain unknown. Since the study participants were exclusively African Americans, the findings of this study cannot be generalized to non-African American groups. Also, the low sample size implies that the power to detect differences in variables such as CD4 and viral load across rationale groups is limited. Assuming a “medium” effect size as defined by Cohen,53 we obtained a power of only approximately 50%.
Study findings emphasize the importance of understanding the patient's model of the disease, the treatment, and the interaction of the two. Each adherence rationale presented a different set of self-identified barriers, clinical challenges, and opportunities for adherence interventions. The IAR created treatment challenges because people with this rationale resisted their physician's directions. For clinicians it may be possible to identify the problems that individuals with an IAR face and offer appropriate interventions. A positive feature is that those with an IAR were trying to integrate ART into their lives and were open and explicit about the problems they faced.
Individuals with the AKR and the DOR rationales seemed less clearly willing to disclose the various types of adherence problems that they encountered. This constitutes a problem for interventions because these rationales may not readily provide direct insight into the particular personal issues people face when trying to adhere to prescribed treatment protocols. For the AKR group, we suggest that clinicians focus on the need to improve the patient's confidence in their own interpretation of what is required in adherence practice, and therefore instill a greater level of confidence in their own treatment.
The willingness of individuals with a DOR to follow authority suggests that more regular, even brief, contact with clinicians will enhance adherence. However, the reliance of those with a DOR on the clinician suggests that adverse events like side effects could result in disillusionment and dropping out of therapy. Increasing the patient's understanding and appreciation of their own responsibility for both adherence and the clinic outcomes it produces could circumvent this problem from occurring.
In order to contribute directly to improving adherence, a clear way of identifying which rationale guides patient adherence needs to be developed. This would allow clinicians to tailor interventions to address the challenges posed by the different rationales. Adherence problems created by a patient's rejection of medical authority are different from those where a patient cuts down on therapeutic doses due to toxicity fears.
Overall, an understanding of individual adherence rationales offers useful avenues for targeted interventions based on patient beliefs and values, as opposed to personal characteristics, and provides the opportunity to develop interventions that will improve the prospects of long-term adherence to ART.
Acknowledgment
This research was supported by National Institute of Allergy and Infectious Disease grant # AI 49113.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Horne R. Adherence to medication: A review of existing research. In: Myers LB, editor; Midence K, editor. Adherence to Treatment in Medical Conditions. Amsterdam: Overseas Publishers Assoc.; 1998. pp. 285–311. [Google Scholar]
- 2.Vermeire E. Hearnshaw H. Van Royen P. Denekens J. Patient adherence to treatment: Three decades of research. A comprehensive review. J Clin Pharm Ther. 2001;26:331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 3.McMullen K. Luborsky M. Self-rated health as cultural and identity appraisal process: African-American elders' health evaluative rationales. Gerontologist. 2006;46:431–438. doi: 10.1093/geront/46.4.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spire B. Duran S. Souville M. Adherence to highly active antiretroviral therapies (ART) in HIV-infected patients: From a predictive to a dynamic approach. Soc Sci Med. 2002;54:1481–1496. doi: 10.1016/s0277-9536(01)00125-3. [DOI] [PubMed] [Google Scholar]
- 5.Preau M. Vincent E. Spire B, et al. Health-related quality of life and health locus of control beliefs among HIV-infected treated patients. J Psychosom Res. 2005;59:407–413. doi: 10.1016/j.jpsychores.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Reimen R. Hirky AE. Johnson MO. Weinhardt LS. Whittier D. Lee GM. Adherence to medication treatment: A qualitative study of facilitators and barriers among a diverse sample of HIV+ men and women in four U.S cites. AIDS Behav. 2003;7:61–72. doi: 10.1023/a:1022513507669. [DOI] [PubMed] [Google Scholar]
- 7.Sankar A. Wunderlich T. Neufeld S. Luborsky M. Sero-positive African American beliefs about alcohol and impact on antiretroviral adherence. AIDS Behav. 2006;10:1–9. doi: 10.1007/s10461-006-9144-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horne R. Buick D. Fisher M. Leake H. Cooper V. Weinman J. Doubts about necessity and concerns about adverse effects: Identifying the types of beliefs that are associated with non-adherence to HAART. Int J STD AIDS. 2004;15:38–44. doi: 10.1258/095646204322637245. [DOI] [PubMed] [Google Scholar]
- 9.Pound P. Britten N. Morgan M, et al. Resisting medicines: A synthesis of qualitative studies of medicine taking. Soc Sci Med. 2005;61:133–155. doi: 10.1016/j.socscimed.2004.11.063. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease and Prevention. Fact Sheet: HIV/AIDS among African Americans, CDC 2008. Rev ed. Atlanta: Centers for Disease Control and Prevention; 2008. [Google Scholar]
- 11.Jain S. Schwarcz S. Katz M. Gulati R. McFarland W. Elevated risk of death for African Americans with AIDS, San Francisco, 1996–2002. J Health Care Poor Underserv. 2006;17:493–503. doi: 10.1353/hpu.2006.0106. [DOI] [PubMed] [Google Scholar]
- 12.Giordano TP. Bartsch G. Zhang Y, et al. Disparities in outcomes for African American and Latino subjects in the Flexible Initial Retrovirus Suppressive Therapies (FIRST) Trail. AIDS Patient Care STDs. 2010;24:287–295. doi: 10.1089/apc.2009.0332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asad S. Hulgan T. Raffanti SP. Daugherty J. Ray W. Sterling TR. Socio-demographic factors predict early discontinuation of HIV non-nucleoside reverse transcriptase inhibitors and protease inhibitors. J Natl Med Assoc. 2008;100:1417–1424. doi: 10.1016/s0027-9684(15)31541-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weidle PJ. Ganea CE. Irwin KL. Adherence to antiretroviral medications in an inner-city population. J Acquir Immune Defic Syndr. 1999;22:498–502. doi: 10.1097/00126334-199912150-00011. [DOI] [PubMed] [Google Scholar]
- 15.Bohnert AS. Latkin CA. HIV testing and conspiracy beliefs regarding the origins of HIV among African Americans. AIDS Patient Care STDs. 2009;23:759–763. doi: 10.1089/apc.2009.0061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bogart L. Thorburn S. Are HIV/AIDS conspiracy beliefs a barrier to HIV prevention among African Americans? J Acquir Immune Defic Syndr. 2005;38:213–218. doi: 10.1097/00126334-200502010-00014. [DOI] [PubMed] [Google Scholar]
- 17.Oh DL. Sarafian F. Silvestre A, et al. Evaluation of adherence and factors affecting adherence to combination antiretroviral therapy among white Hispanic and Black men in the MACS cohort. J Acquir Immune Defic Syndr. 2009;52:290–293. doi: 10.1097/QAI.0b013e3181ab6d48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saha S. Jacobs EA. Moore RD. Beach MC. Trust in physicians and racial disparities in HIV care. AIDS Patient Care STDs. 2010;24:415–420. doi: 10.1089/apc.2009.0288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laws MB. Wilson IB. Bowser D. Keer SE. Taking antiretroviral therapy for HIV infection: Learning from patients' stories. J Gen Intern Med. 2000;15:848–858. doi: 10.1046/j.1525-1497.2000.90732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reynolds N. Testa MA. Marc LG, et al. Factors influencing medication adherence beliefs and self-efficacy in persons new to antiretroviral therapy: A multicenter, cross-sectional study. AIDS Behav. 2004;8:141–150. doi: 10.1023/B:AIBE.0000030245.52406.bb. [DOI] [PubMed] [Google Scholar]
- 21.Golin CE. Liu H. Hays RD, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J Gen Intern Med. 2002;17:756–765. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Walsh JC. Horne R. Dalton M. Burgess AP. Gazzard BG. Reasons for non-adherence to antiretroviral therapy: Patients' perspectives provide evidence of multiple causes. AIDS Care. 2001;13:709–720. doi: 10.1080/09540120120076878. [DOI] [PubMed] [Google Scholar]
- 23.Wong WKT. Ussher J. How do subjectively-constructed meanings ascribed to anti-HIV treatments affect treatment-adherent patients? Qual Health Res. 2008;18:458–468. doi: 10.1177/1049732308314852. [DOI] [PubMed] [Google Scholar]
- 24.Stevens PE. Hildebrandt E. Pill taking from the perspective of HIV-infected women who are vulnerable to antiretroviral treatment failure. Qual Health Res. 2009;19:593–604. doi: 10.1177/1049732309333272. [DOI] [PubMed] [Google Scholar]
- 25.Donovan JL. Patient decision making. The missing ingredient in compliance research. Int J Technol Assess Health Care. 1995;11:443–455. doi: 10.1017/s0266462300008667. [DOI] [PubMed] [Google Scholar]
- 26.Anderson J. Wiggens S. Rajwani R. Holbrook A. Blue C. Ng M. Living with a chronic illness: Chinese-Canadian and Euro-Canadian women with diabetes—Exploring factors that influence management. Soc Sci Med. 1995;41:181–195. doi: 10.1016/0277-9536(94)00324-m. [DOI] [PubMed] [Google Scholar]
- 27.Anderson R. Donnely M. David W. Controversial beliefs about diabetes and its care. Diabetes Care. 1992;15:859–863. doi: 10.2337/diacare.15.7.859. [DOI] [PubMed] [Google Scholar]
- 28.Rosenstock I. The health belief model and preventative behavior. Health Educ Monogr. 1974;2:354–386. [Google Scholar]
- 29.Baer H. The emergence of integrative medicine in Australia: The growing interest of biomedicine and nursing in complementary medicine in a southern developed society. Med Anthropol Q. 2008;22:52–67. doi: 10.1111/j.1548-1387.2008.00003.x. [DOI] [PubMed] [Google Scholar]
- 30.Hunt L. Arar N. An analytical framework for contrasting patient and provider views of the process of chronic disease management. Med Anthropol Q. 2001;15:1–21. doi: 10.1525/maq.2001.15.3.347. [DOI] [PubMed] [Google Scholar]
- 31.Leventhal H. Meyer D. Nerenz D. The common sense representation of illness danger. In: Rachman S, editor. Contributions to Medical Psychology. Vol. 2. Oxford: Pergamon Press; 1980. pp. 7–30. [Google Scholar]
- 32.Leventhal H. Diefenbach M. Leventhal EA. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cogn Ther Res. 1992;16:143–163. [Google Scholar]
- 33.Horne R. Buick D. Fisher M. Leake H. Cooper V. Weinman J. Doubts about necessity and concerns about adverse effects: Identifying the types of beliefs that are associated with non-adherence to ART. Int J STD AIDS. 2004;15:38. doi: 10.1258/095646204322637245. [DOI] [PubMed] [Google Scholar]
- 34.Horne R. Weinman J. Patient beliefs about prescribed medications and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;46:555–567. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 35.Trostle J. Hauser A. Susser I. The logic of noncompliance: Management of epilepsy from the patient's point of view. J Clin Pharm Ther. 1983;26:331–342. doi: 10.1007/BF00249998. [DOI] [PubMed] [Google Scholar]
- 36.Murray LK. Semrau K. McCurley E, et al. Barriers to acceptance and adherenece of antiretroviral therapy in urban Zambian women: A qualitative study. AIDS Care. 2009;21:78–86. doi: 10.1080/09540120802032643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sankar A. Luborsky M. Schuman P. Roberts G. Adherence discourse among HIV+ African American women taking high acting anti-retroviral therapy. AIDS Care. 2002;14:203–218. doi: 10.1080/09540120220104712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kleinman A. Berkeley: University of California Press; 1980. Patients and Healers in the Context of Culture. [Google Scholar]
- 39.Garro L. Explaining high blood pressure: Variation in knowledge about illness. Am Anthropol. 1988;15:98–119. [Google Scholar]
- 40.Garro L. Individual or societal responsibility? Explanations of diabetes in an Anishinaabe (Ojibway) Community. Soc Sci Med. 1995;40:37–46. doi: 10.1016/0277-9536(94)00125-d. [DOI] [PubMed] [Google Scholar]
- 41.Hernandez C. The experience of living with Insulin-dependent diabetes: Lessons for the diabetes educator. Diabetes Educ. 1995;21:33–37. doi: 10.1177/014572179502100106. [DOI] [PubMed] [Google Scholar]
- 42.Becker G. Disrupted Lives: How People Create Meaning in a Chaotic World. Berkeley: University of California Press; 1997. [Google Scholar]
- 43.Meiwald C. Is awareness enough? The contradictions of self-care in a chronic disease clinic. Hum Organ. 1997;56:353–363. [Google Scholar]
- 44.Good MJ. Good B. Schaffer C. Lind S. American oncology and the discourse of hope. Cult Med Psych. 1990;14:59–79. doi: 10.1007/BF00046704. [DOI] [PubMed] [Google Scholar]
- 45.Lakoff G. Johnson M. Metaphors We Live. Chicago: University of Chicago Press; 1980. [Google Scholar]
- 46.Scheer J. Luborsky M. Cultural context of polio biographies. Orthopedics. 1991;14:1173–1181. doi: 10.3928/0147-7447-19911101-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hays R. Kravitz R. Mazel R. Sherbourne C. The impact of patient adherence on health outcomes for patients with chronic disease in the Medical Outcomes Study. J Behav Med. 1994;17:347–360. doi: 10.1007/BF01858007. [DOI] [PubMed] [Google Scholar]
- 48.Bernard HR. Research Methods in Anthropology: Qualitative and Quantitative Approaches. Oxford: Altimira; 2001. [Google Scholar]
- 49.Ezzy D. Lived experience and interpretation in narrative theory: Experiences of living with HIV/AIDS. Qual Sociol. 1998;21:169–179. [Google Scholar]
- 50.Ezzy D. Illness narratives: Time, hope and HIV. Soc Sci Med. 2000;50:605–617. doi: 10.1016/s0277-9536(99)00306-8. [DOI] [PubMed] [Google Scholar]
- 51.The Strategies for Management of Antiretroviral Therapy (SMART) Study Group. CD4+ count-guided interruption of antiretroviral treatment. N Engl J Med. 2006;355:2283–2296. doi: 10.1056/NEJMoa062360. [DOI] [PubMed] [Google Scholar]
- 52.Lewis MP. Colbert A. Erlen J. Meyers M. A qualitative study of persons who are 100% adherent to antiretroviral therapy. AIDS Care. 2006;18:140–148. doi: 10.1080/09540120500161835. [DOI] [PubMed] [Google Scholar]
- 53.Cohen J. Hillsdale NJ: Earlbaum; 1988. Statistical Power Analysis for the Social Sciences. [Google Scholar]