Abstract
Background/Aims
Sleep disorder (SD) is associated with an increased risk of cardiovascular disease and is more prevalent among individuals with type 2 diabetes mellitus. These health problems not only frequently coexist but also exacerbate each other. We conducted a cross-sectional study to estimate the prevalence of SD among diabetic patients and to investigate the relationship between SD and cardiovascular risk among these patients.
Methods
We recruited 784 patients with type 2 diabetes and conducted a self-administered questionnaire. We assessed sleep quality using the Pittsburgh Sleep Quality Index and the risk of obstructive sleep apnea (OSA) using the Berlin Questionnaire. Additional information included blood pressure and metabolic profiles.
Results
Of the 784 diabetic patients, 301 (38.4%) patients had poor sleep quality, and 124 (15.8%) were at high risk for OSA. Patients at increased risk for OSA were more obese; they also had higher blood pressure, fasting plasma insulin levels, insulin resistance assessed by homeostasis model assessment (HOMA-IR), and serum triglycerides levels (p < 0.05). The frequency of risk for OSA was higher among obese patients compared with non-obese patients (34.8% vs. 9.4%, p < 0.05). Logistic regression analysis revealed that male sex and bone mass index were independent predictors of risk for OSA.
Conclusions
SD was prevalent among type 2 diabetic patients, and OSA could aggravate their risk for cardiovascular disease. Clinical treatment of these patients should include evaluation and intervention for SD.
Keywords: Cardiovascular diseases; Sleep apnea, obstructive; Diabetes mellitus, type 2
INTRODUCTION
Sleep disorder (SD) is a common chronic illness characterized by repetitive episodes of partial or complete cessation of breathing during sleep, which may affect up to 17% of middle-aged adults [1]. Chronic sleep fragmentation, sleep deprivation, and intermittent nocturnal hypoxemia associated with SD have been implicated in metabolic dysfunction, including altered glucose metabolism and adverse cardiovascular complications [2,3]. Common antecedent risks such as obesity, hypertension, endothelial dysfunction, inflammatory state, and oxidative stress appear among patients with diabetes mellitus and patients with SD. The association between diabetes mellitus and SD and its precise mechanism are not well understood. It is likely that chronic intermittent hypoxia and sleep fragmentation lead to pathogenic factors such as increased sympathetic activity, dysregulation of the hypothalamus-pituitary-adrenal axis, and activation of inflammatory pathways, resulting in abnormal glucose metabolism.
Large population studies have shown that SD is an independent risk factor for hypertension, cardiovascular disease (CVD) [4-8], and impaired glucose metabolism [9]. Self-reported history of snoring, a common symptom of SD, is independently associated with impaired glucose tolerance and type 2 diabetes mellitus (T2DM) [10,11].
Cross-sectional estimates from population studies have suggested that up to 40% of patients with obstructive sleep apnea (OSA) have T2DM [12,13]. Among patients who are known to have T2DM, the prevalence of OSA may be up to 23% [14], and the prevalence of some form of SD may be as high as 58% [15]. However, scanty documentation is available about the prevalence of SD among Asians. A community study of SD among middle-aged Chinese men and women in Hong Kong revealed 9% and 3.7% prevalence rates for SD and 4% and 2.1% for symptomatic OSA [16,17]. Because only limited studies have focused on the prevalence of SD in T2DM, especially among Asians, the goal of this study was to estimate the prevalence of SD among Korean diabetic patients and determine the association of CVD among these patients.
METHODS
Subjects
We consecutively recruited 784 patients with T2DM who attended the outpatient department of endocrinology at Ewha Womans University Hospital from January 2008 through December 2008. None of these patients used insulin injection or medications that would affect sleep, and none had serum creatinine levels greater than 1.4 mg/dL, serum transaminases levels more than three times the upper limit of normal value, severe painful peripheral neuropathy, and alcohol dependency. The Institutional Review Board of Ewha Womans University Mokdong Hospital approved this study. Written informed consent was obtained from each subject. Degree of obesity was classified based on the results of an Asia-Pacific study [18]: non-obese patients had a body mass index (BMI) < 25 kg/m2 and obese patients had a BMI ≥ 25 kg/m2.
Survey assessment of sleep quality and risk for obstructive sleep apnea
Sleep quality was assessed using a self-administered questionnaire. The Pittsburgh Sleep Quality Index (SQI) was used to evaluate sleep quality, and the Berlin Questionnaire (BQ) was used to evaluate risk for OSA.
The SQI assesses sleep quality over the preceding month and differentiates 'good' sleepers from 'poor' sleepers [19]. Questionnaire responses involve seven components; each component is scored from 0 to 3, where a score of 3 represents the negative extreme. Component scores are summed to provide the SQI global score (range, 0 to 21); scores > 5 identify 'poor' sleepers [19].
The BQ includes five items on snoring (category 1, items 1-5), three items on daytime somnolence (category 2, items 6-8), and one item on the history of hypertension (category 3, item 9). The questionnaire also includes information about age, gender, height, and weight [20]. The overall score is based on the patient's responses to each of the three categories. The snoring or daytime somnolence categories are positive if responses indicate persistent symptoms (> 3 to 4 times a week) on the questionnaire items. A positive score for the third category requires a history of hypertension or a BMI ≥ 25 kg/m2. High risk for OSA is defined as a positive score for two or more of the three categories [21].
Anthropometric measurements and baseline sampling
The height and weight of each patient was measured, and BMI was calculated as body weight in kilograms divided by the square of height in meters (kg/m2). Blood pressure (BP) was measured once for each patient in the supine position with a mercury sphygmomanometer; systolic BP and diastolic BP were measured to the nearest 2 mmHg at Korotkoff sounds I and IV, respectively.
Venous blood was drawn from each patient after an overnight fast to obtain baseline measurements of glucose, HbA1c, total cholesterol, high-density lipoprotein cholesterol (HDL-C), and triglycerides (TG). Plasma glucose was measured using the glucose oxidase method (Beckman Model Glucose Analyzer 2, brea, ca , USA). Total cholesterol (TC), HDL-C, and TG were measured by enzymatic methods using a Hitachi 7150 autoanalyzer (Hitachi, Tokyo, Japan). LDL cholesterol (LDL-C) was calculated as follows: TC (mg/dL) - HDL-C (mg/dL) - TG/5 (mg/dL).
Statistical analysis
Data management and statistical analysis was conducted using SPSS version 16 (SPSS Inc., Chicago, IL, USA). The normality of distributions of the variables was analyzed using the Kolmogorov-Smirnov test. Data are expressed as means ± SD. Because TG and HDL-C exhibited skewed distribution, p values were based on logarithmic data, but mean values for untransformed data are presented.
Continuous variables were compared between subjects at high risk and those at low risk for OSA using an independent t test and analysis of covariance (ANCOVA). The χ2 test was used to assess differences in the frequency of sleep disturbance in each age group and sex. A logistic regression analysis was performed to determine which variables predicted high risk for OSA. All p values were two-tailed, and statistical significance was defined as p < 0.05.
RESULTS
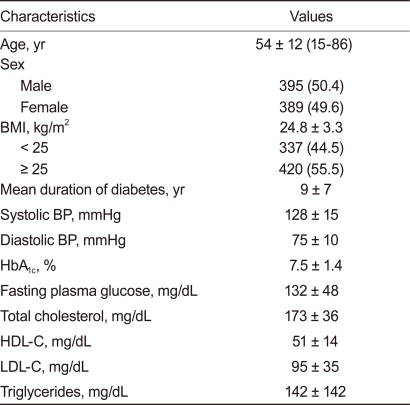
Table 1 lists the clinical and biochemical characteristics of all participants. The mean age was 54 ± 12 years, and 395 (50.4%) participants were male. The mean BMI value was 24.8 ± 3.3 kg/m2, mean duration of diabetes was 9 ± 7 years, and mean baseline HbA1c was 7.5 ± 1.4%.
Table 1.
Characteristics of 748 patients with type 2 diabetes
Values are presented as mean ± SD or number (%).
BMI, body mass index; BP, blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL, low-density lipoprotein cholesterol.
SQI results revealed poor sleep quality (PSQ) in 301 (38.4%) of 784 diabetic patients, 132 (16.8%) of the 395 male patients, and 169 (21.6%) of the 389 female patients. No significant differences were observed by sex. BQ identified 124 (15.8%) of the 784 patients (44 [5.6%] of the 389 female patients and 80 [10.2%] of the 394 male patients) as being at high risk for OSA, revealing a significantly greater risk among male than female patients (p < 0.05).
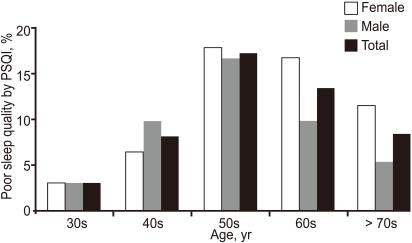
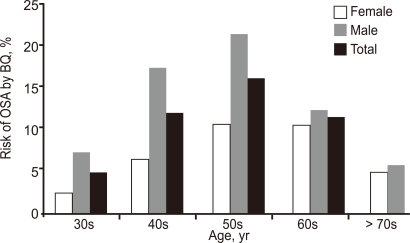
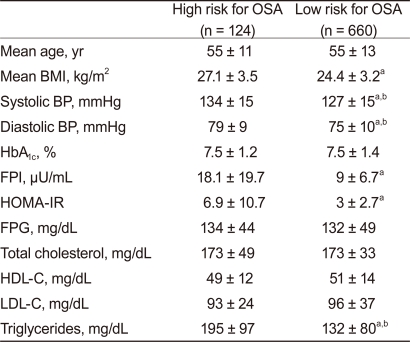
Fig. 1 presents the frequency of PSQ by age and sex. PSQ frequency increased for patients aged up to their 50s: 3% in patients in their 30s, 8.1% in patients in their 40s, and 17.2% in patients in their 50s; it then decreased to 13.3% in patients in their 60s and 8.4% in patients in their 70s and older. The frequency of PSQ in patients in their 40s and older was significantly higher than that in patients in their 30s for both sexes (p < 0.05). Similarly, the risk for OSA increased for patients aged up to their 50s: 4.9% in patients in their 30s, 12% in patients in their 40s, and 16.1% in their 50s; it then decreased to 11.6% in patients in their 60s and 5.4% in patients in their 70s and older (Fig. 2). The frequency of risk for OSA was significantly higher among patients in their 40s, 50s, and 60s than among those in their 30s (p < 0.05). The frequency of risk for OSA was significantly higher for males than females among patients in their 40s (17.4% vs. 6.6%, p < 0.05) and in their 50s (21.5% vs. 10.7%, p < 0.05) (Fig. 2). Patients at high risk for OSA had higher BMI, systolic and diastolic blood pressure, fasting plasma insulin, insulin resistance assessed by homeostasis model assessment (HOMA-IR), and triglyceride levels compared with those at low risk (Table 2). Significant differences appeared between the two groups in systolic and diastolic blood pressure and triglyceride levels after adjusting for BMI.
Figure 1.
Frequency of poor sleep quality by the Pittsburgh Sleep Quality Index (PSQI) according to age and sex.
Figure 2.
Frequency of high risk for obstructive sleep apnea (OSA) by the Berlin Questionnaire (BQ) according to age and sex.
Table 2.
Comparison of diabetic patients according to risk for OSA
OSA, obstructive sleep apnea; BMI, body mass index; BP, blood pressure; FPI, fasting plasma insulin; HOMA-IR, insulin resistance assessed by homeostasis model assessment; FPG, fasting plasma glucose; HDL-C, high-density lipoprotein cholesterol; LDc-c, low-density lipoprotein cholesterol.
ap < 0.05 vs. high risk.
bp < 0.05 after adjustment for BMI.
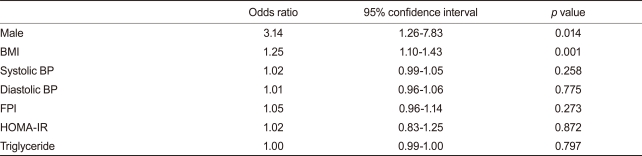
The frequency of risk for OSA was significantly higher among obese patients compared with non-obese patients (34.8% vs. 9.4%, p < 0.05). Logistic regression analysis revealed that male sex (odds ratio [OR], 3.14; confidence interval [CI], 1.26 to 7.83; p < 0.05) and BMI (OR, 1.25; CI, 1.10 to 1.43; p < 0.01) were independent predictors of risk for OSA (Table 3).
Table 3.
Factors associated with the risk for obstructive sleep apnea by logistic regression analysis
Regression model included age, sex, BMI, systolic and diastolic pressure, HbA1C, FPI, HOMA-IR, triglyceride, and total, HDL, and LDL cholesterol.
BMI, body mass index; BP, blood pressure; FPI, fasting plasma insulin; HOMA-IR, insulin resistance assessed by homeostasis model assessment; HDL, high-density lipoprotein cholesterol; LDL, low-density lipoprotein.
DISCUSSION
This study found that SD was more prevalent in patients with T2DM than in the general population, in which it appears in approximately 9% of women and 24% of men [1]. Of 784 diabetic patients, 301 (38.4%) patients had poor sleep quality according to the SQI, and 124 (15.8%) were at high risk for OSA according to the BQ. Reports from the International Diabetes Federation (IDF) taskforce on epidemiology and prevention [22] have also revealed a high prevalence of SD among patients with T2DM, suggesting a prevalence of SD as high as 58% and a prevalence of OSA as high as 23%. Several prospective studies have reported an association between sleeping disorders and the development of diabetes. Total sleep duration is known to be an independent risk factor for developing diabetes. The Nurses' Health Study, which examined sleep duration and diabetes, reported an increased risk of symptomatic incident diabetes over 10 years among those reporting sleep durations of 5 hours or less, even after controlling for many covariates [23]. A cross-sectional study of sleeping disorders among patients with T2DM using SQI reported that 48% of T2DM patients had poor sleep quality, and the poorest sleep quality was among patients who had been diagnosed more than 10 years earlier [24]. Many biological mechanisms have been proposed to explain how SD may lead to T2DM. One is the activation of the sympathetic nervous system, which plays a central role in the regulation of glucose and fat metabolism [25]. Repeated arousal from sleep after each obstructive breath exacerbates this effect [22]. Elevated cortisol levels [26], pro-inflammatory cytokines, and ghrelin levels may predispose an individual to insulin resistance, and decreased leptin levels may be the mechanism for increased prevalence of T2DM in SD [27].
Our results indicate that individuals at higher risk for OSA were more obese and had higher BP, fasting insulin levels, HOMA-IR, and triglyceride levels, suggesting that SD was associated with risk factors for CVD. Many prospective and cross-sectional studies have reported a link among OSA, CVD, and mortality [28-32]. Young et al. [33] reported that severe SD was associated with a three-fold increase in all-cause mortality compared with an absence of SD based on an 18-year follow-up prospective cohort study. Studies on the prevalence of CVD and OSA have reported that 50% of SD patients are hypertensive and that 11-37% experience heart failure [34]. One cross-sectional study reported that OSA was associated with a range of CVD manifestations such as stroke, heart failure, and ischemic heart disease [8]. There are several explanations for the development of CVD among patients with OSA. Patients with OSA exhibit repetitive hypoxemia, CO2 retention, consequent sympathetic activation, and marked blood pressure elevation during sleep [29]; additionally, adverse changes in the circulating levels of many vasoactive or inflammatory mediators including nitric oxide, interleukin-6, tumor necrosis factor, and c-reactive protein, as well as platelet activation and coagulation factors promote the development of CVD [35-39].
Our results revealed that obese diabetic patients are at higher risk for OSA, and logistic regression also demonstrated that BMI is an independent predictor of risk for OSA. A recent study of obese men (BMI ≥ 30 kg/m2) without major medical illnesses found that 60% of these men met the criteria for SD, and 27% had OSA [2]. The risk of having moderate to severe oSA over a 4-year period increases six-fold among individuals who gain 10% excess weight [40], suggesting that the high incidence of CV morbidity among patients with oSA is explained by the presence of obesity [41,42]. With the onset of OSA, individuals develop leptin resistance, which in turn contributes to further weight gain [28]. Inflammatory cytokines tumor necrosis factor (TNF)-α and interleukin (IL)-6, which are associated with daytime sleepiness, might also be involved in the causal pathway because they are elevated among obese patients with OSA [43].
Fasting plasma insulin levels and HOMA-IR were higher among patients at high risk for OSA. The mechanism underlying the relationship between SD and insulin resistance can be explained as follows [44]. Hypoxia and hypercapnia caused by sleep-disordered breathing provoke sympathetic nervous activity, releasing epinephrine, norepinephrine, and cortisol [45-47]. Sympathetic hyperactivity and increased catecholamine impair glucose homeostasis and induce insulin resistance by increasing glycogenolysis and gluconeogenesis [48,49]. Repetitive cycles of intermittent hypoxemia followed by reoxygenation may trigger the formation of reactive oxygen species, eliciting the release of inflammatory cytokines such as TNF-α and IL-6 [50,51]. Inflammatory cytokines play an important role in mediating peripheral insulin resistance by inhibiting glucose uptake by fat and muscle, increasing the level of counter-regulatory hormones and inducing the release of free fatty acids [52,53].
We found a higher frequency of risk for OSA among men, with logistic regression analysis revealing male sex to be an independent predictor. The higher prevalence of risk for OSA among men than women could be related to the greater tendency toward android fat distribution [54] and differences in upper airway muscle function during sleep [54]. Men have a greater increase in airway resistance and greater susceptibility to flow limitation during non-rapid eye movement (NREM) sleep than women do. During NREM sleep, women have a functional advantage over men that is protective against airway collapse, and this protective mechanism is lost with the transition to REM sleep [54].
This study had several limitations. First, its relatively small sample size limits the generalization of results. Large-scale long-term research will be needed in the future. Second, we did not consider the medications used by patients or the effects of hypoglycemia. We excluded patients who used insulin injection or medications that might affect sleep, but we did not consider hypoglycemic events, which might affect sleep patterns. Finally, the results might be affected by recall bias and the subjective nature of self-reported snoring and OSA. However, self-reported snoring and snoring reported by roommates were reasonably correlated in previous studies [55].
In conclusion, our data suggest that SD is prevalent among type 2 diabetic patients and that individuals at high risk for OSA are also at higher risk for CVD. OSA appears to aggravate the risk of CVD among type 2 diabetic patients. Therefore, early detection and treatment of SD among type 2 diabetic patients is essential to modulate the relationship between SD and risk for CVD.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165:1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 2.Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL. Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med. 2002;165:677–682. doi: 10.1164/ajrccm.165.5.2104087. [DOI] [PubMed] [Google Scholar]
- 3.Vgontzas AN, Bixler EO, Chrousos GP. Metabolic disturbances in obesity versus sleep apnoea: the importance of visceral obesity and insulin resistance. J Intern Med. 2003;254:32–44. doi: 10.1046/j.1365-2796.2003.01177.x. [DOI] [PubMed] [Google Scholar]
- 4.Punjabi NM, Ahmed MM, Polotsky VY, Beamer BA, O'Donnell CP. Sleep-disordered breathing, glucose intolerance, and insulin resistance. Respir Physiol Neurobiol. 2003;136:167–178. doi: 10.1016/s1569-9048(03)00079-x. [DOI] [PubMed] [Google Scholar]
- 5.Choi KM, Lee JS, Park HS, Baik SH, Choi DS, Kim SM. Relationship between sleep duration and the metabolic syndrome: Korean National Health and Nutrition Survey 2001. Int J Obes (Lond) 2008;32:1091–1097. doi: 10.1038/ijo.2008.62. [DOI] [PubMed] [Google Scholar]
- 6.Punjabi NM, Caffo BS, Goodwin JL, et al. Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med. 2009;6:e1000132. doi: 10.1371/journal.pmed.1000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342:1378–1384. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 8.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163:19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 9.Ybarra J, Planas F, Navarro-Lopez F, et al. Association between sleep-disordered breathing, aminoterminal pro-brain natriuretic peptide (NT-proBNP) levels and insulin resistance in morbidly obese young women. Eur J Intern Med. 2009;20:174–181. doi: 10.1016/j.ejim.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 10.Elmasry A, Janson C, Lindberg E, Gislason T, Tageldin MA, Boman G. The role of habitual snoring and obesity in the development of diabetes: a 10-year follow-up study in a male population. J Intern Med. 2000;248:13–20. doi: 10.1046/j.1365-2796.2000.00683.x. [DOI] [PubMed] [Google Scholar]
- 11.Al-Delaimy WK, Manson JE, Willett WC, Stampfer MJ, Hu FB. Snoring as a risk factor for type II diabetes mellitus: a prospective study. Am J Epidemiol. 2002;155:387–393. doi: 10.1093/aje/155.5.387. [DOI] [PubMed] [Google Scholar]
- 12.Meslier N, Gagnadoux F, Giraud P, et al. Impaired glucose-insulin metabolism in males with obstructive sleep apnoea syndrome. Eur Respir J. 2003;22:156–160. doi: 10.1183/09031936.03.00089902. [DOI] [PubMed] [Google Scholar]
- 13.Elmasry A, Lindberg E, Berne C, et al. Sleep-disordered breathing and glucose metabolism in hypertensive men: a population-based study. J Intern Med. 2001;249:153–161. doi: 10.1046/j.1365-2796.2001.00787.x. [DOI] [PubMed] [Google Scholar]
- 14.West SD, Nicoll DJ, Stradling JR. Prevalence of obstructive sleep apnoea in men with type 2 diabetes. Thorax. 2006;61:945–950. doi: 10.1136/thx.2005.057745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Resnick HE, Redline S, Shahar E, et al. Diabetes and sleep disturbances: findings from the Sleep Heart Health Study. Diabetes Care. 2003;26:702–709. doi: 10.2337/diacare.26.3.702. [DOI] [PubMed] [Google Scholar]
- 16.Ip MS, Lam B, Lauder IJ, et al. A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest. 2001;119:62–69. doi: 10.1378/chest.119.1.62. [DOI] [PubMed] [Google Scholar]
- 17.Ip MS, Lam B, Tang LC, Lauder IJ, Ip TY, Lam WK. A community study of sleep-disordered breathing in middle-aged Chinese women in Hong Kong: prevalence and gender differences. Chest. 2004;125:127–134. doi: 10.1378/chest.125.1.127. [DOI] [PubMed] [Google Scholar]
- 18.Cockram CS. Diabetes mellitus: perspective from the Asia-Pacific region. Diabetes Res Clin Pract. 2000;50(Suppl 2):S3–S7. doi: 10.1016/s0168-8227(00)00202-3. [DOI] [PubMed] [Google Scholar]
- 19.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 20.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–491. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 21.Ahmadi N, Chung SA, Gibbs A, Shapiro CM. The Berlin questionnaire for sleep apnea in a sleep clinic population: relationship to polysomnographic measurement of respiratory disturbance. Sleep Breath. 2008;12:39–45. doi: 10.1007/s11325-007-0125-y. [DOI] [PubMed] [Google Scholar]
- 22.Shaw JE, Punjabi NM, Wilding JP, Alberti KG, Zimmet PZ International Diabetes Federation Taskforce on Epidemiology and Prevention. Sleep-disordered breathing and type 2 diabetes: a report from the International Diabetes Federation Taskforce on Epidemiology and Prevention. Diabetes Res Clin Pract. 2008;81:2–12. doi: 10.1016/j.diabres.2008.04.025. [DOI] [PubMed] [Google Scholar]
- 23.Ayas NT, White DP, Al-Delaimy WK, et al. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes Care. 2003;26:380–384. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 24.Cunha MC, Zanetti ML, Hass VJ. Sleep quality in type 2 diabetics. Rev Lat Am Enfermagem. 2008;16:850–855. doi: 10.1590/s0104-11692008000500009. [DOI] [PubMed] [Google Scholar]
- 25.Nonogaki K. New insights into sympathetic regulation of glucose and fat metabolism. Diabetologia. 2000;43:533–549. doi: 10.1007/s001250051341. [DOI] [PubMed] [Google Scholar]
- 26.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29:657–661. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 27.Chaput JP, Despres JP, Bouchard C, Astrup A, Tremblay A. Sleep duration as a risk factor for the development of type 2 diabetes or impaired glucose tolerance: analyses of the Quebec Family Study. Sleep Med. 2009;10:919–924. doi: 10.1016/j.sleep.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 28.Jean-Louis G, Zizi F, Clark LT, Brown CD, McFarlane SI. Obstructive sleep apnea and cardiovascular disease: role of the metabolic syndrome and its components. J Clin Sleep Med. 2008;4:261–272. [PMC free article] [PubMed] [Google Scholar]
- 29.Reaven G. The metabolic syndrome or the insulin resistance syndrome? Different names, different concepts, and different goals. Endocrinol Metab Clin North Am. 2004;33:283–303. doi: 10.1016/j.ecl.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 30.Reaven G, Abbasi F, McLaughlin T. Obesity, insul in resistance, and cardiovascular disease. Recent Prog Horm Res. 2004;59:207–223. doi: 10.1210/rp.59.1.207. [DOI] [PubMed] [Google Scholar]
- 31.Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman MW, Grunstein RR. Sleep apnea as an independent risk factor for all-cause mortality: the Busselton Health Study. Sleep. 2008;31:1079–1085. [PMC free article] [PubMed] [Google Scholar]
- 32.Yumino D, Wang H, Floras JS, et al. Relationship between sleep apnoea and mortality in patients with ischaemic heart failure. Heart. 2009;95:819–824. doi: 10.1136/hrt.2008.160952. [DOI] [PubMed] [Google Scholar]
- 33.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep. 2008;31:1071–1078. [PMC free article] [PubMed] [Google Scholar]
- 34.Kato M, Adachi T, Koshino Y, Somers VK. Obstructive sleep apnea and cardiovascular disease. Circ J. 2009;73:1363–1370. doi: 10.1253/circj.cj-09-0364. [DOI] [PubMed] [Google Scholar]
- 35.Schulz R, Hummel C, Heinemann S, Seeger W, Grimminger F. Serum levels of vascular endothelial growth factor are elevated in patients with obstructive sleep apnea and severe nighttime hypoxia. Am J Respir Crit Care Med. 2002;165:67–70. doi: 10.1164/ajrccm.165.1.2101062. [DOI] [PubMed] [Google Scholar]
- 36.Schulz R, Flototto C, Jahn A, et al. Circulating adrenomedullin in obstructive sleep apnoea. J Sleep Res. 2006;15:89–95. doi: 10.1111/j.1365-2869.2006.00498.x. [DOI] [PubMed] [Google Scholar]
- 37.Riha RL, Brander P, Vennelle M, et al. Tumour necrosis factor-alpha (-308) gene polymorphism in obstructive sleep apnoea-hypopnoea syndrome. Eur Respir J. 2005;26:673–678. doi: 10.1183/09031936.05.00130804. [DOI] [PubMed] [Google Scholar]
- 38.Shamsuzzaman AS, Winnicki M, Lanfranchi P, et al. Elevated C-reactive protein in patients with obstructive sleep apnea. Circulation. 2002;105:2462–2464. doi: 10.1161/01.cir.0000018948.95175.03. [DOI] [PubMed] [Google Scholar]
- 39.Robinson GV, Pepperell JC, Segal HC, Davies RJ, Stradling JR. Circulating cardiovascular risk factors in obstructive sleep apnoea: data from randomized controlled trials. Thorax. 2004;59:777–782. doi: 10.1136/thx.2003.018739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Makinodan K, Yoshikawa M, Fukuoka A, et al. Effect of serum leptin levels on hypercapnic ventilator response in obstructive sleep apnea. Respiration. 2008;75:257–264. doi: 10.1159/000112471. [DOI] [PubMed] [Google Scholar]
- 41.Vgontzas AN, Papanicolaou DA, Bixler EO, et al. Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab. 2000;85:1151–1158. doi: 10.1210/jcem.85.3.6484. [DOI] [PubMed] [Google Scholar]
- 42.Coughlin SR, Mawdsley L, Mugarza JA, Calverley PM, Wilding JP. Obstructive sleep apnoea is independently associated with an increased prevalence of metabolic syndrome. Eur Heart J. 2004;25:735–741. doi: 10.1016/j.ehj.2004.02.021. [DOI] [PubMed] [Google Scholar]
- 43.Hu FB, Willett WC, Colditz GA, et al. Prospective study of snoring and risk of hypertension in women. Am J Epidemiol. 1999;150:806–816. doi: 10.1093/oxfordjournals.aje.a010085. [DOI] [PubMed] [Google Scholar]
- 44.Joo S, Lee S, Choi HA, et al. Habitual snoring is associated with elevated hemoglobin A1c levels in non-obese middle-aged adults. J Sleep Res. 2006;15:437–444. doi: 10.1111/j.1365-2869.2006.00556.x. [DOI] [PubMed] [Google Scholar]
- 45.Fletcher EC. Sympathetic activity and blood pressure in the sleep apnea syndrome. Respiration. 1997;64(Suppl 1):22–28. doi: 10.1159/000196732. [DOI] [PubMed] [Google Scholar]
- 46.Fletcher EC. Sympathetic over activity in the etiology of hypertension of obstructive sleep apnea. Sleep. 2003;26:15–19. doi: 10.1093/sleep/26.1.15. [DOI] [PubMed] [Google Scholar]
- 47.Somers VK, Dyken ME, Clary MP, Abboud FM. Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest. 1995;96:1897–1904. doi: 10.1172/JCI118235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hjalmarsen A, Aasebø U, Birkeland K, Sager G, Jorde R. Impaired glucose tolerance in patients with chronic hypoxic pulmonary disease. Diabetes Metab. 1996;22:37–42. [PubMed] [Google Scholar]
- 49.Marshall S, Garvey WT, Traxinger RR. New insights into the metabolic regulation of insulin action and insulin resistance: role of glucose and amino acids. FASEB J. 1991;5:3031–3036. doi: 10.1096/fasebj.5.15.1743436. [DOI] [PubMed] [Google Scholar]
- 50.Dyugovskaya L, Lavie P, Lavie L. Increased adhesion molecules expression and production of reactive oxygen species in leukocytes of sleep apnea patients. Am J Respir Crit Care Med. 2002;165:934–939. doi: 10.1164/ajrccm.165.7.2104126. [DOI] [PubMed] [Google Scholar]
- 51.Schulz R, Mahmoudi S, Hattar K, et al. Enhanced release of superoxide from polymorphonuclear neutrophils in obstructive sleep apnea: impact of continuous positive airway pressure therapy. Am J Respir Crit Care Med. 2000;162(2 Pt 1):566–570. doi: 10.1164/ajrccm.162.2.9908091. [DOI] [PubMed] [Google Scholar]
- 52.Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science. 1993;259:87–91. doi: 10.1126/science.7678183. [DOI] [PubMed] [Google Scholar]
- 53.Stumvoll M, Haring H. Insulin resistance and insulin sensitizers. Horm Res. 2001;55(Suppl 2):3–13. doi: 10.1159/000063466. [DOI] [PubMed] [Google Scholar]
- 54.O'Connor C, Thornley KS, Hanly PJ. Gender differences in the polysomnographic features of obstructive sleep apnea. Am J Respir Crit Care Med. 2000;161:1465–1472. doi: 10.1164/ajrccm.161.5.9904121. [DOI] [PubMed] [Google Scholar]
- 55.Enright PL, Newman AB, Wahl PW, Manolio TA, Haponik EF, Boyle PJ. Prevalence and correlates of snoring and observed apneas in 5,201 older adults. Sleep. 1996;19:531–538. doi: 10.1093/sleep/19.7.531. [DOI] [PubMed] [Google Scholar]