Abstract
Background/Aims
We assessed changes in hemodynamic and arterial stiffness parameters following reductions of dialysate calcium concentrations in patients undergoing hemodialysis.
Methods
In this prospective study, 20 patients on maintenance hemodialysis (10 females, 10 males) with dialysate calcium concentrations of 1.75 mmol/L were enrolled. At the start of the study, the dialysate calcium level was lowered to 1.50 mmol/L. Serial changes in biochemical, hemodynamic, and arterial stiffness parameters, including pulse wave velocity (PWV) and augmentation index (AIx), were assessed every 2 months for 6 months. We also examined changes in the calcification-inhibitory protein, serum fetuin-A.
Results
During the 6-month study period, serum total calcium and ionized calcium decreased consistently (9.5 ± 1.0 to 9.0 ± 0.7, p = 0.002 vs. 1.3 ± 0.1 to 1.1 ± 0.1, p = 0.035). Although no apparent changes in blood pressure were observed, heart-femoral PWW (hf-PWV) and AIx showed significant improvement (p = 0.012, 0.043, respectively). Repeated-measures ANOVA indicated a significant effect of lowering dialysate calcium on hf-PWV (F = 4.58, p = 0.004) and AIx (F = 2.55, p = 0.049). Accompanying the change in serum calcium, serum fetuin-A levels significantly increased (95.8 ± 45.8 pmol/mL at baseline to 124.9 ± 82.2 pmol/mL at 6 months, p = 0.043).
Conclusions
Lowering dialysate calcium concentration significantly improved arterial stiffness parameters, which may have been associated with upregulation of serum fetuin-A.
Keywords: Arterial stiffness, Calcium, Dialysis solutions, Fetuin A, Hemodialysis
INTRODUCTION
Arterial stiffness and vascular calcification are common findings in patients with end-stage renal disease (ESRD), and they contribute to the development and progression of cardiovascular complications [1-3]. Although the precise pathophysiological mechanisms of arterial stiffness and vascular calcification are not yet fully understood, passive calcium deposition and active modification of osteotrophic regulators such as osteoprotegerin and fetuin-A are thought to play important roles in this process [4-6].
Because the diffusion of calcium during hemodialysis depends on the gradient between serum and dialysate calcium concentrations [7-9], understanding the effects of lowering dialysate calcium concentrations in patients undergoing hemodialysis is important. To date, several studies have examined the complex relationships among serum calcium levels, the degree of vascular calcification, and arterial stiffness in patients with ESRD, and low calcium dialysate has been reported to reduce serum calcium levels, which is helpful in improving arterial stiffness [10,11]. However, these studies were relatively short-term trials and did not demonstrate serial changes in arterial stiffness. Moreover, no reported study has evaluated the relationship between serum calcium concentrations and changes in serum fetuin-A, a calcification-inhibitory protein.
In this study, we prospectively evaluated changes in hemodynamic and arterial stiffness parameters, including pulse wave velocity (PWV) and augmentation index (AIx), after lowering dialysate calcium concentrations for 6 months in patients on hemodialysis. Changes in serum fetuin-A levels were also examined.
METHODS
This was a single-center, prospective observational study performed at Gangnam Severance Hospital in Seoul, Korea, from December 2008 to July 2009. The inclusion criteria were patients between 20 and 80 years of age who had been on regular hemodialysis (three or four times per week) with a high dialysate calcium concentration (1.75 mmol/L) for at least 6 months. We excluded patients with a history of recent hospitalization for cardiovascular events, acute or chronic inflammation, or parathyroidectomy. In total, 20 clinically stable patients on hemodialysis were enrolled.
The study was approved by the Institutional Review Board for Human Research at Yonsei University College of Medicine. Informed consent was obtained from all patients.
Biochemical and hemodynamic data were obtained at baseline. Total calcium, ionized calcium, phosphorus, serum creatinine, albumin, intact parathyroid hormone (PTH), and C-reactive protein levels were checked under standardized fasting conditions immediately before the start of dialysis sessions. Using an automatic blood pressure monitor device, blood pressure was measured in the resting state before (pre-dialysis) and after (post-dialysis) each session. The mean value of three consecutive measurements was used. Arterial stiffness parameters (PWV, AIx) were measured after dialysis in the resting state. After the baseline measurement, the dialysate calcium concentration was lowered, from 1.75 to 1.5 mmol/L, and this change was maintained for 6 months. Blood samples were taken and arterial stiffness parameters were checked every 2 months. In total, four blood tests and arterial stiffness measurements were taken during the 6 months (T0, T2month, T4month, and T6month).
Blood samples were also obtained for assessment of serum fetuin-A levels. Serum fetuin-A levels were checked twice, at baseline and at the end of the study (T0 and T6month). To assess serum fetuin-A, the collected blood samples were immediately centrifuged (5,000 g, 10 minutes) and then stored at -70℃ until the assays were performed. A commercially available enzyme-linked immunosorbent assay (ELISA) kit (DuoSet ELISA Development kit, R&D Systems, Minneapolis, MN, USA) was used. Intra- and inter-assay coefficients of variation were less than 10%. In each subject, two sequences of measurements were performed and their mean value was used for the statistical analysis.
To assess additional calcium sources, a complete medication list, including calcium-containing phosphate binders and vitamin D agents, was reviewed. Adverse events, including hypotension and muscle cramps, were surveyed during the study period.
Assessment of arterial stiffness parameters
PWV and AIx were assessed using an automated device (VP-2000; Colin Co. Ltd., Komaki, Japan). Measurements were performed according to manufacturer instructions by the same physician 15 minutes after each midweek dialysis session with the patient in a resting, supine position.
The automatic device simultaneously obtains electrocardiograms, phonocardiograms, bilateral brachial and ankle blood pressures, and carotid and femoral arterial pulse waves. The PWV was determined from measurements of pulse transit time and the distance in the heart-femoral (hf) and brachial-ankle (ba) segments. The hf-PWV was considered to represent the central PWV. AIx was determined by automatic identification of the inflection point on the carotid pulse wave by applanation tonometry. It was calculated by dividing the augmented pressure amplitude (the difference between early and late systolic peaks) by the pulse pressure and expressed as a percentage. In younger subjects, aortic AIx is close to zero or may have a negative value. With aging, the aorta stiffens and the value becomes positive. The maximum value of AIx is approximately 50%.
Data analysis
Statistical analyses were performed using the SPSS version 15.0 (SPSS Inc., Chicago, IL, USA). All values are expressed as means ± standard deviation or as a percentage (%). Serial changes in each parameter during the 6-month follow-up were analyzed by Wilcoxon's signed-rank test and repeat-measure ANOVA. Because two patients were lost at 5 months (one died and one was transferred to a private clinic), final measurements for these patients were analyzed using last observation carried forward methods. Correlations among percentage change in serum calcium level, arterial stiffness parameters, and fetuin-A were determined by Spearman's correlation analysis. p values < 0.05 were considered to indicate statistical significance.
RESULTS
Baseline characteristics
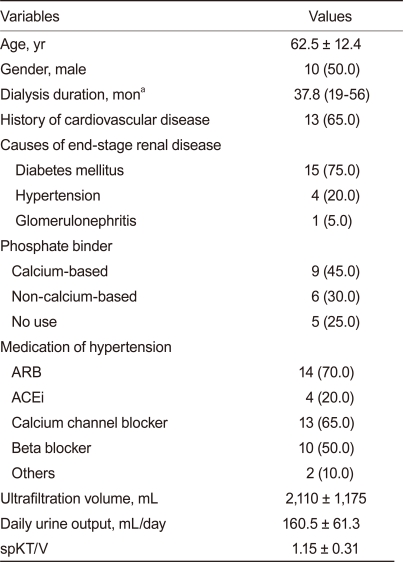
In total, 20 maintenance hemodialysis patients participated in this study. The baseline clinical characteristics of the patients are outlined in Table 1. The mean age was 62.5 ± 12.4 years and the median duration of hemodialysis was 37.8 months (range, 19 to 56). The patients consisted of 10 females and 10 males and the most common cause of ESRD was diabetes mellitus (n = 15, 75%). At the beginning of the study, 45% (n = 9) of patients were taking calcium-based phosphate binders (calcium acetate), 30% (n = 6) were taking non-calcium-based phosphate binders, and the remaining patients took no phosphate binder. No patient was on active vitamin D therapy. Antihypertensive medications at baseline included angiotensin-converting enzyme or angiotensin II receptor blockers in 90%, calcium channel blockers in 65%, β-blockers in 50%, and other medications in 10%.
Table 1.
Baseline demographic and clinical characteristics of the subjects (n = 20)
Values are presented as mean ± SD, number (%) or median (range). ARB, angiotensin II receptor blocker; ACEi, angiotensin-converting enzyme inhibitor.
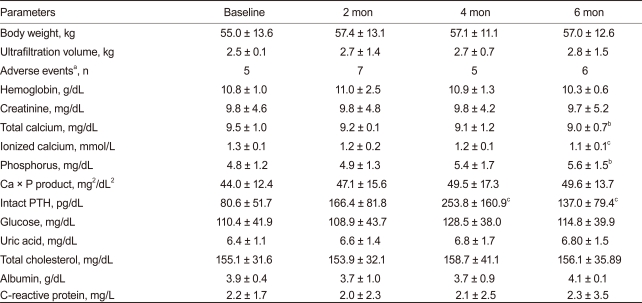
Changes in clinical and biochemical parameters during 6 months
The effects of reducing dialysate calcium on clinical and biochemical parameters are listed in Table 2. No significant change occurred in body weight, ultrafiltration rate, or adverse event rate during hemodialysis. After lowering dialysate calcium, serum total calcium levels decreased significantly, from 9.5 ± 1.0 mg/dL at baseline to 9.0 ± 0.7 mg/dL at 6 months (p = 0.031), and serum ionized calcium levels also decreased, from 1.3 ± 0.1 mmol/L to 1.1 ± 0.1 mmol/L (p = 0.001). Serum phosphorus levels increased significantly (4.8 ± 1.2 at baseline vs. 5.6 ± 1.5 at 6 months; p = 0.025), and serum intact PTH levels increased gradually, from 80.6 ± 51.7 pg/mL at baseline to a maximum of 253.8 ± 160.9 pg/mL at 4 months (p < 0.001). At this point, active vitamin D treatment was administered to five patients to prevent secondary hyperparathyroidism and the intact PTH level decreased thereafter to 137.0 ± 79.4 pg/mL at 6 months; however, the difference was still significant (p = 0.001). No significant change was observed in hemoglobin, calcium-phosphorus product, glucose, uric acid, total cholesterol, or C-reactive protein levels over the study period.
Table 2.
Clinical and biochemical data at baseline and 6 months after reducing dialysate calcium concentration (1.75 → 1.5 mmol/L)
Ca, calcium; P, phosphorus; PTH, parathyroid hormone.
aAdverse events include intradialytic hypotension, muscle cramps, dizziness, nausea, vomiting, and headache.
bp < 0.05, cp < 0.01, vs. baseline by Wilcoxon's signed-rank test.
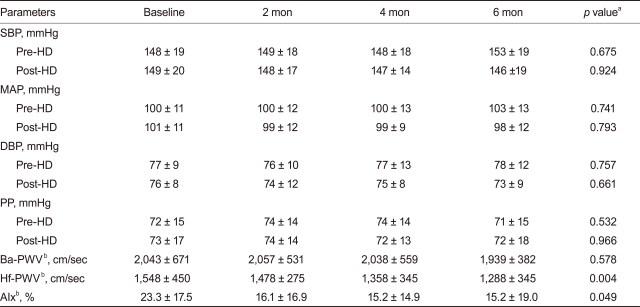
Changes in hemodynamic and arterial stiffness parameters and fetuin-A
No apparent change was detected in systolic, diastolic, mean arterial blood pressure, or pulse pressure during follow-up (Table 3). However, hf-PWV and heart rate-adjusted AIx showed significant improvements (1,548 ± 450 cm/sec, 23.3 ± 17.5%, at baseline vs. 1,288 ± 345 cm/sec, 15.2 ± 19.0% at 6 months; p = 0.012, 0.043, respectively).
Table 3.
Changes in hemodynamic and arterial stiffness parameters over 6 months
SBP, systolic blood pressure; HD, hemodialysis; MAP, mean arterial pressure; DBP, diastolic blood pressure; PP, pulse pressure; ba-PWV, brachial-ankle pulse wave velocity; hf-PWV, heart-femoral pulse wave velocity; AIx, augmentation index.
ap value by repeated-measures ANOVA.
bMeasured post-hemodialysis.
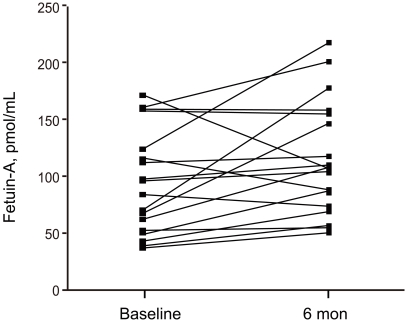
Moreover, accompanying the changes in serum calcium levels, serum fetuin-A levels increased significantly, from 95.8 ± 45.8 pmol/mL at baseline to 124.9 ± 82.2 pmol/mL at 6 months (p = 0.043; Fig 1). A negative and significant correlation was detected between serum calcium and fetuin-A level (r = -0.52, p = 0.027 at 6 months).
Figure 1.
Changes in serum fetuin-A levels after reducing dialysate calcium concentration. The serum fetuin-A level increased significantly after 6 months (95.8 ± 45.8 pmol/mL at baseline vs. 124.9 ± 82.2 pmol/mL at 6 months, p = 0.043).
Reduction in serum calcium and its relationship with arterial stiffness markers
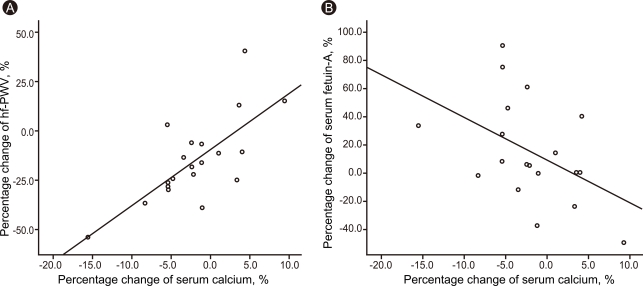
The percentage change in serum calcium level (Δserum calcium, %) was significantly correlated with the change in post-dialysis hf-PWV (Δhf-PWV, r = 0.721, p < 0.001) and the serum fetuin-A level (Δfetuin-A; r = -0.463, p = 0.046; Fig. 2). Further analysis, using repeated-measures ANOVA, confirmed the significant effect of lowering dialysate calcium on hf-PWV (F = 4.58, p = 0.004) and heart rate-adjusted AIx (F = 2.55, p = 0.049).
Figure 2.
Correlation between Δserum calcium level and post-dialysis Δheart-femoral pulse wave velocity (Δhf-PWV) (A) and Δfetuin-A (B). Percentage change in serum calcium level was significantly associated with the change in post-dialysis hf-PWV (r = 0.721, p < 0.001) and the change in fetuin-A (r = -0.463, p = 0.046).
DISCUSSION
Arterial stiffness is an important manifestation of vascular calcification. Although vascular calcification is thought to result from old age and atherosclerosis, not all vascular calcification occurs in the presence of atherosclerosis. Previously, physicochemical factors alone, such as calcium-phosphate derangement and alkaline pH, were thought to regulate the development of vascular calcification. However, recent studies have demonstrated that it is an elaborately regulated process, involving bone morphogenic proteins including osteoprotegerin and fetuin-A, and metabolic disorders such as uremia [12-15].
Because serum calcium levels depend on the diffusion rate between the dialysate and serum calcium concentration gradient, special attention is paid to the dialysate calcium level [7,8]. In this study, we investigated the effect of reduced dialysate calcium on arterial stiffness parameters and serum fetuin-A levels. Our results demonstrated that lowering the dialysate calcium concentration, from 1.75 to 1.5 mmol/L, for 6 months lowered serum total and ionized calcium levels significantly and this change was associated with definite improvements in central PWV and AIx. With the change in serum total calcium, the serum ionized calcium level was reduced, by 15.3%, and central PWV was lowered, by 16.7%. Moreover, these changes were accompanied by a significant increase in serum fetuin-A levels.
Our results are consistent with previously reported data indicating that dialysate calcium directly affects aortic stiffness in patients undergoing dialysis. The first description of the relationship in humans was by Marchais et al. [16] in 1989. They reported that hemodialysis with a dialysate calcium of 1.75 mmol/L led to a significant increase in both central and brachial PWV, but that a concentration of 1.5 mmol/L did not [16]. Recently, LeBeouf et al. [11] also investigated the impact of acute modification of the dialysate calcium level on serum ionized calcium and central PWV. Using a crossover study with three different dialysate calcium levels, they found a linear, positive relationship between dialysate calcium concentrations and central PWV, and they suggested that even an acute decrease in serum calcium levels from reduced dialysate calcium can lead to a detectable improvement in central PWV. A longer study was conducted by Demirci et al. [3] with patients on peritoneal dialysis. They used higher dialysate calcium over 6 months and found a significant worsening of brachial PWV, but the change was not detected with low dialysate calcium treatment. These results are similar to our data, except that we assessed central PWV, not brachial ankle PWV. Although ba-PWV is used as a convenient and accurate method to assess central arterial stiffness [10], unlike hf-PWV, ba-PWV includes peripheral stiffness with the measurements of peripheral artery velocity [17]. Generally, the correlation between central and peripheral PWV is not definite, suggesting that arterial stiffening does not occur equally, especially in patients with renal dysfunction. In fact, the increase in PWV is most significant in the hf (central) segment compared with the femoral-ankle (peripheral) segment in these patients. Similarly in patients with ischemic heart disease (IHD), the positive association between IHD and PWV was significant only in the hf segment, when an adjustment was made for other confounding factors [18]. We thought that because of the relatively short duration of our study, only a change in hf-PWV was observed. However, with longer term follow-up, we think that improvement in ba-PWV would also occur.
Several previous studies reported that the serum phosphate level decreased with reduced dialysate calcium concentrations [19,20]. In contrast to previous studies, the serum phosphate level in our patients actually increased, from a pretreatment value of 4.8 ± 1.2 to 5.6 ± 1.5 mg/dL at 6 months after the treatment (p < 0.05). This finding may be explained by changes in the phosphate binder. Initially, approximately 30% of patients (6/20) used non-calcium-based phosphate binders, such as sevelamer hydrochloride or lanthanum carbonate, which have stronger phosphate-binding capacity without hypercalcemia. However, as serum calcium levels decreased, many of our patients changed phosphate binders, to equivalent doses of the calcium-based phosphate binder, calcium acetate (PhosLo; each dose of sevelamer 800 mg or lanthanum 500 mg was changed to calcium acetate 667 mg). Although the dose of the calcium-based phosphate binder was similar to that of the non-calcium-based phosphate binder, serum phosphate levels in our patient group seemed to rise, probably due to the lower efficacy of the calcium-based phosphate binder. Additionally, five patients received active vitamin D treatment after 4 months, which may also have contributed to the increased serum phosphate level. With those five patients, the baseline serum phosphate level was 4.98 ± 1.41 mg/dL, but the level increased to 5.59 ± 1.60 and 5.76 ± 1.75 mg/dL at 4 and 6 months, respectively.
Another finding was that the marked improvements in arterial stiffness parameters were independent of blood pressure. During the study period, despite the use of the same doses of antihypertensive drugs, no significant change occurred in blood pressure. Systolic, diastolic, mean arterial pressure, and pulse pressure remained unchanged, while the markers of arterial stiffness showed significant improvements. These findings somewhat contradict those in the report by Argiles et al. [21]. They studied the long-term hemodynamic effects of dialysate calcium reductions from 1.5 mmol/L to 1.25 mmol/L in seven patients for 1 year. At the end of the study, 24-hour blood pressure monitoring showed significantly decreased diastolic blood pressure and heart rate. These seemingly conflicting results are likely due to differences in the baseline characteristics of the patients. Compared to our study, none of their patients had a history of hypertension and none received antihypertensive drugs. That the PWV and AIx improvements in our study were independent of blood pressure may suggest that the decrease in serum calcium concentrations affects arterial stiffness by a mechanism other than blood pressure control.
Another finding in this study is the significant rise in the serum fetuin-A level accompanying the improvement in central PWV. Fetuin-A, an abundant serum protein produced in the liver, forms calcioprotein particles and thereby prevents aggregation of calcium phosphate into insoluble mineral crystals [22]. It is also expressed in bone, accumulates at sites of vascular calcification, and plays a role in skeletal mineralization, possibly through the inhibition of calcification [5,23]. In in vitro studies, fetuin-A contributes about 50% of the calcification-inhibitory capacity of human plasma [22]. Recently, several studies have reported a protective role of fetuin-A against arterial stiffness and cardiovascular mortality in patients with ESRD; our results are consistent with these findings [24-27].
A cohort study of 258 patients with ESRD starting renal replacement therapy showed that a low fetuin-A level was associated with increased cardiovascular and all-cause mortality [25]. Shroff et al. [24] also reported that fetuin-A level increased in patients on dialysis compared to healthy controls, and that fetuin-A levels were negatively correlated with dialysis duration, PWV, and vascular calcification. In our study, after reducing the level of dialysate calcium, serum fetuin-A levels increased significantly and correlation analysis showed a negative association between percentage change of serum calcium and fetuin-A levels during the whole study period, suggesting a possible role of fetuin-A in improving arterial stiffness via upregulation. Although our study could not show a significant direct correlation between fetuin-A level and PWV or AIx, this may have been due to the small sample size.
Our study had several limitations. The generalizability of our findings may be limited because our sample size was relatively small and we did not include a control group, which may have reduced statistical power. However, to minimize the confounding factors, we fixed the medication list, such as antihypertensive and lipid-lowering agents, and controlled dry weight to maintain euvolemic status. Although vitamin D treatment in five patients may have been a confounding factor, vitamin D analogs were used after 4 months in all patients. Thus, improvements in PWV and AIx at 2 and 4 months were most likely due to reduced dialysate calcium concentrations, and was not a vitamin D effect. However, a randomized controlled trial with more subjects is necessary, and further long-term follow-up is needed to establish the long-term effects of lowering the dialysate calcium concentration.
In conclusion, lowering the dialysate calcium concentration induced a blood pressure-independent, favorable effect in arterial stiffness parameters, as indicated by improved AIx and central PWV. These findings may be associated with the upregulation of serum fetuin-A.
Acknowledgments
This work was supported by a Gangnam Severance Hospital Internal Medicine Research Grant in 2008.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Kundhal K, Lok CE. Clinical epidemiology of cardiovascular disease in chronic kidney disease. Nephron Clin Pract. 2005;101:c47–c52. doi: 10.1159/000086221. [DOI] [PubMed] [Google Scholar]
- 2.Sigrist MK, Levin A, Er L, McIntyre CW. Elevated osteoprotegerin is associated with all-cause mortality in CKD stage 4 and 5 patients in addition to vascular calcification. Nephrol Dial Transplant. 2009;24:3157–3162. doi: 10.1093/ndt/gfp253. [DOI] [PubMed] [Google Scholar]
- 3.Demirci MS, Ozkahya M, Asci G, et al. The influence of dialysate calcium on progression of arterial stiffness in peritoneal dialysis patients. Perit Dial Int. 2009;29(Suppl 2):S15–S17. [PubMed] [Google Scholar]
- 4.Essalihi R, Zandvliet ML, Moreau S, et al. Distinct effects of amlodipine treatment on vascular elastocalcinosis and stiffness in a rat model of isolated systolic hypertension. J Hypertens. 2007;25:1879–1886. doi: 10.1097/HJH.0b013e328255e906. [DOI] [PubMed] [Google Scholar]
- 5.Speer G, Fekete BC, El Hadj Othmane T, et al. Serum osteoprotegerin level, carotid-femoral pulse wave velocity and cardiovascular survival in haemodialysis patients. Nephrol Dial Transplant. 2008;23:3256–3262. doi: 10.1093/ndt/gfn242. [DOI] [PubMed] [Google Scholar]
- 6.Nakamura U, Iwase M, Nohara S, Kanai H, Ichikawa K, Iida M. Usefulness of brachial-ankle pulse wave velocity measurement: correlation with abdominal aortic calcification. Hypertens Res. 2003;26:163–167. doi: 10.1291/hypres.26.163. [DOI] [PubMed] [Google Scholar]
- 7.Giachelli CM. Vascular calcification mechanisms. J Am Soc Nephrol. 2004;15:2959–2964. doi: 10.1097/01.ASN.0000145894.57533.C4. [DOI] [PubMed] [Google Scholar]
- 8.Yoo SJ, Oh DJ, Yu SH. The effects of low calcium dialysate on arterial compliance and vasoactive substances in patients with hemodialysis. Korean J Intern Med. 2004;19:27–32. doi: 10.3904/kjim.2004.19.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gotch F, Levin NW, Kotanko P. Calcium balance in dialysis is best managed by adjusting dialysate calcium guided by kinetic modeling of the interrelationship between calcium intake, dose of vitamin D analogues and the dialysate calcium concentration. Blood Purif. 2010;29:163–176. doi: 10.1159/000245924. [DOI] [PubMed] [Google Scholar]
- 10.Kyriazis J, Katsipi I, Stylianou K, Jenakis N, Karida A, Daphnis E. Arterial stiffness alterations during hemodialysis: the role of dialysate calcium. Nephron Clin Pract. 2007;106:c34–c42. doi: 10.1159/000101482. [DOI] [PubMed] [Google Scholar]
- 11.LeBeouf A, Mac-Way F, Utescu MS, et al. Effects of acute variation of dialysate calcium concentrations on arterial stif fness and aor tic pressure waveform. Nephrol Dial Transplant. 2009;24:3788–3794. doi: 10.1093/ndt/gfp351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goldsmith D, Ritz E, Covic A. Vascular calcification: a stiff challenge for the nephrologist: does preventing bone disease cause arterial disease? Kidney Int. 2004;66:1315–1333. doi: 10.1111/j.1523-1755.2004.00895.x. [DOI] [PubMed] [Google Scholar]
- 13.Shroff RC, Shanahan CM. The vascular biology of calcification. Semin Dial. 2007;20:103–109. doi: 10.1111/j.1525-139X.2007.00255.x. [DOI] [PubMed] [Google Scholar]
- 14.Adragao T, Frazao JM. Cardiovascular risk in dialysis patients: an X-ray vision on vascular calcifications. Kidney Int. 2008;74:1505–1507. doi: 10.1038/ki.2008.503. [DOI] [PubMed] [Google Scholar]
- 15.London GM, Marchais SJ, Guerin AP, Metivier F, Adda H. Arterial structure and function in end-stage renal disease. Nephrol Dial Transplant. 2002;17:1713–1724. doi: 10.1093/ndt/17.10.1713. [DOI] [PubMed] [Google Scholar]
- 16.Marchais S, Guerin A, Safar M, London G. Arterial compliance in uraemia. J Hypertens Suppl. 1989;7:S84–S85. doi: 10.1097/00004872-198900076-00038. [DOI] [PubMed] [Google Scholar]
- 17.Ogawa O, Onuma T, Kubo S, Mitsuhashi N, Muramatsu C, Kawamori R. Brachial-ankle pulse wave velocity and symptomatic cerebral infarction in patients with type 2 diabetes: a cross-sectional study. Cardiovasc Diabetol. 2003;2:10. doi: 10.1186/1475-2840-2-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hatsuda S, Shoji T, Shinohara K, et al. Regional arterial stiffness associated with ischemic heart disease in type 2 diabetes mellitus. J Atheroscler Thromb. 2006;13:114–121. doi: 10.5551/jat.13.114. [DOI] [PubMed] [Google Scholar]
- 19.Cheng IK, Lu HB, Chan CY, et al. The requirement of low calcium dialysate in patients on continuous ambulatory peritoneal dialysis receiving calcium carbonate as a phosphate binder. Clin Nephrol. 1993;40:100–105. [PubMed] [Google Scholar]
- 20.Lezaic V, Pejanovic S, Kostic S, et al. Effects of lowering dialysate calcium concentration on mineral metabolism and parathyroid hormone secretion: a multicentric study. Ther Apher Dial. 2007;11:121–130. doi: 10.1111/j.1744-9987.2007.00419.x. [DOI] [PubMed] [Google Scholar]
- 21.Argiles A, Kerr PG, Canaud B, Flavier JL, Mion C. Calcium kinetics and the long-term effects of lowering dialysate calcium concentration. Kidney Int. 1993;43:630–640. doi: 10.1038/ki.1993.92. [DOI] [PubMed] [Google Scholar]
- 22.Sage AP, Tintut Y, Demer LL. Regulatory mechanisms in vascular calcification. Nat Rev Cardiol. 2010;7:528–536. doi: 10.1038/nrcardio.2010.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lebreton JP, Joisel F, Raoult JP, Lannuzel B, Rogez JP, Humbert G. Serum concentration of human alpha 2 HS glycoprotein during the inflammatory process: evidence that alpha 2 HS glycoprotein is a negative acute-phase reactant. J Clin Invest. 1979;64:1118–1129. doi: 10.1172/JCI109551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shroff RC, Shah V, Hiorns MP, et al. The circulating calcification inhibitors, fetuin-A and osteoprotegerin, but not matrix Gla protein, are associated with vascular stiffness and calcification in children on dialysis. Nephrol Dial Transplant. 2008;23:3263–3271. doi: 10.1093/ndt/gfn226. [DOI] [PubMed] [Google Scholar]
- 25.Stenvinkel P, Wang K, Qureshi AR, et al. Low fetuin-A levels are associated with cardiovascular death: impact of variations in the gene encoding fetuin. Kidney Int. 2005;67:2383–2392. doi: 10.1111/j.1523-1755.2005.00345.x. [DOI] [PubMed] [Google Scholar]
- 26.Mori K, Emoto M, Araki T, et al. Association of serum fetuin-A with carotid arterial stiffness. Clin Endocrinol (Oxf) 2007;66:246–250. doi: 10.1111/j.1365-2265.2006.02716.x. [DOI] [PubMed] [Google Scholar]
- 27.Ketteler M, Bongartz P, Westenfeld R, et al. Association of low fetuin-A (AHSG) concentrations in serum with cardiovascular mortality in patients on dialysis: a cross-sectional study. Lancet. 2003;361:827–833. doi: 10.1016/S0140-6736(03)12710-9. [DOI] [PubMed] [Google Scholar]